Abstract
Introduction and Objectives
Low serum testosterone (T) is common and increasingly prevalent with increased age. Recent studies report an “epidemic” of T prescribing and concern about unnecessary T-treatment. The only approved indication for T treatment is repeated low-T levels plus symptoms of hypogonadism. We investigated trends in serum T testing, prevalence of low-serum T among those tested, and initiation of T-treatment among those with low T in Veterans.
Methods
We identified male Veterans, aged 40 years and older in the Pacific Northwest who underwent T testing from 2002 to 2011. We excluded men with prostate or breast cancer or T treatment within the year prior to the T-test. Treatment initiation was defined as the first prescription for T within a year following a low T test.
Results
From 2002–2011, the number of men treated yearly at Northwest VA medical centers increased from 129,247 to 163,572 and annual serum-T testing more than doubled from 4,078 to 9,452. The proportion of men tested yearly increased by 83% from 3.2% to 5.8%. The proportion of those tested with low T increased from 35% to 47%. The absolute number of men who were treated with T increased; however, the proportion of men with low T who were T-treated remained essentially the same from 31% to 28%.
Conclusions
Despite increases in the absolute number and proportion of men who were T-tested and had low T levels, the proportion of men with low T levels who were T-treated yearly decreased since 2002. This contrasts to the escalating T-treatment trends noted in other studies.
Introduction
Low serum testosterone (T) levels in men are common and are increasingly prevalent with increased age(1–3). Low testosterone is associated with a number of comorbid conditions, e.g., chronic illness, obesity, and diabetes mellitus (DM). Furthermore, T levels may be transiently low with acute illness, malnutrition, and use of certain medications(4). Multiple studies suggest a significant increase in the prevalence of men with low T levels over the last decade although the prevalence of true hypogonadism—defined as low T levels plus signs and symptoms—is much lower. Because the signs and symptoms of hypogonadism lack specificity, there is increased likelihood of over diagnosis and subsequent T treatment in middle-age and older men who may have comorbid medical conditions that may mimic symptoms of hypogonadism(5, 6).
Several studies have reported increasing prescription rates of T in community-based populations throughout the world over the last decade(7). These increases have occurred in association with the introduction of transdermal T-formulations (patches and gels), studies suggesting that low T levels was associated with adverse effects, and increases in direct-to-consumer advertising for T-treatment in the US, UK, Australia, and Europe(8).
Prior reports of increasing T prescription rates were derived from pharmacy claims of commercially insured individuals(7–9). However, it is unclear whether the increased prescriptions for T are the result of increased T testing, increased identification of low serum T levels, or both. Furthermore, it is not clear whether similar trends may be found in more managed care populations.
The aim of the present study was to characterize the prevalence of T testing, low T, and T treatment in an integrated Veterans Affairs (VA) health care system in which there were formulary restrictions in the use transdermal T formulations. We examined yearly proportions of men tested for T, found to have low T levels, and subsequently treated with T in male Veterans from 2002 to 2011.
Materials and Methods
Setting
The VA Health Care System provides longitudinal health care to a large population of aging men, as well as maintaining a well-developed and comprehensive electronic health record database. In addition to extensive data on testosterone prescriptions and pharmacy dispensation, the VA database contains comprehensive clinical information on all enrolled patients, including demographic data, outpatient and inpatient clinical care, and laboratory testing.
Cohort identification
We identified all men aged 40 to 89 years who used any VA health care in a single Veterans Integrated Service Network (VISN) in the Pacific Northwest (VISN 20) from January 2002 to December 2011. For men to be included in the study, they needed to demonstrate utilization of the VA healthcare system by presenting for care at a VA clinic on at least one occasion during the year prior to the first T test obtained during the study period 2002–2011. We excluded men with a history of prostate or breast cancer, or a T treatment in the VA in the year prior to the T test. The absolute number of men age 40 to 89 years who utilized the VA healthcare system in each year was used to determine the proportion of men annually who were tested for T in the VA system.
Laboratory evaluation
In each year, we identified the absolute number of men who were first recognized as having a low serum T level, as defined by an abnormally low-flag for total T, free T or bioavailable T, performed in local and regional VA laboratories within the VISN or sent to reference laboratories. T tests were identified in the data using Logical Observation Identifiers Names and Codes (LOINC.)
Testosterone treatment
T treatment initiation was defined as the first prescription for T following the first low T test. T prescriptions were identified in the data by using VA National Drug Internal Entry Numbers for various T formulations. The absolute number and proportion of men who had low T levels that were treated with T and the T formulations used were determined. To insure that calculation of T treatment proportions represented data within a given year only, the index testosterone prescription needed to occur within 12 calendar-months of the index low T value. The results presented were descriptive only. Men were characterized by 10-year age categories and by calendar year of T testing.
Results
Serum testosterone testing
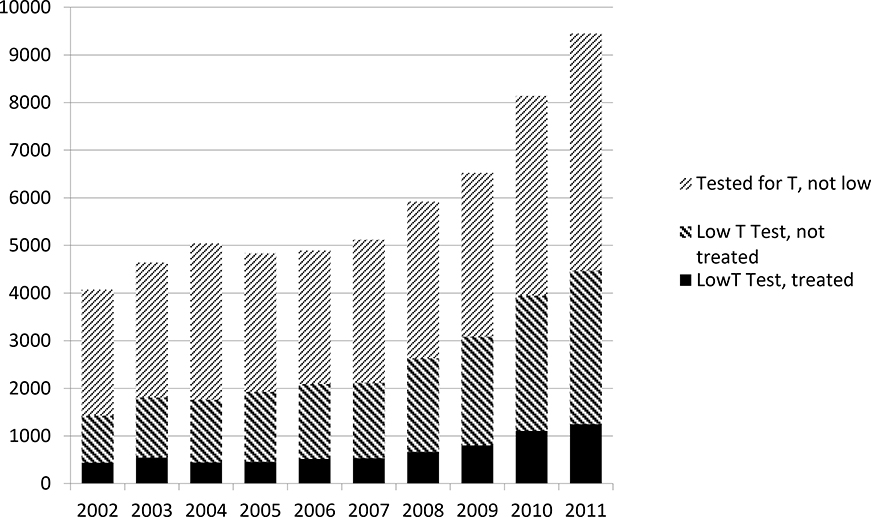
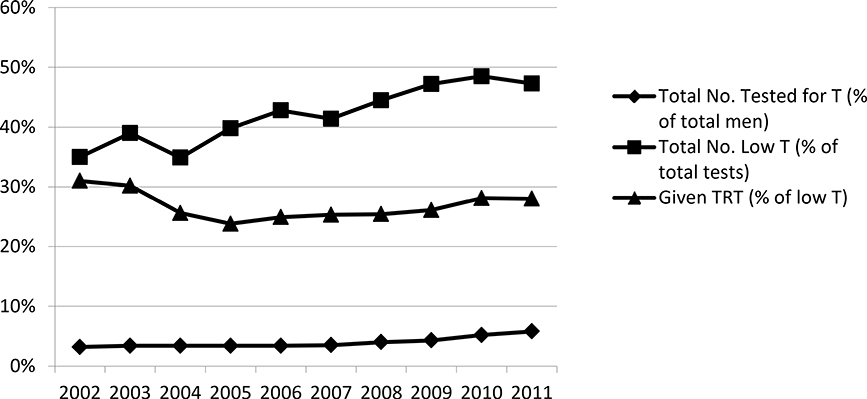
The number of men in the VISN each year increased from 129,247 in 2002 to 163,572 in 2011 (Table 1). During this decade, the number of men undergoing serum T testing yearly more than doubled from 4,078 in 2002 to 9,452 in 2011 (Figure 1). The proportion of men being tested annually increased from 3.2% to 5.8% of all men (Figure 2). The observed increase in testing primarily occurred between 2007 and 2011, where the proportion tested yearly increased from 3.4% to 5.8%.
Table 1.
VISN 20 Men aged 40–89 who underwent testosterone testing, who have low T, and who were treated with T, 2002 to 2011
| Year | Total VISN 20 men (age ≥40) | Total no. tested for T (% of total men) | Total no. low T (% of total tests) | Given TRT* (% of low T) |
|---|---|---|---|---|
| 2002 | 129247 | 4078 (3.2%) | 1428 (35.0%) | 443 (31.0%) |
| 2003 | 135325 | 4646 (3.4%) | 1813 (39.0%) | 548 (30.2%) |
| 2004 | 146250 | 5044 (3.4%) | 1761 (34.9%) | 451 (25.6%) |
| 2005 | 143657 | 4841 (3.4%) | 1928 (39.8%) | 459 (23.8%) |
| 2006 | 144912 | 4894 (3.4%) | 2093 (42.8%) | 521 (24.9%) |
| 2007 | 144552 | 5124 (3.5%) | 2121 (41.4%) | 536 (25.3%) |
| 2008 | 147266 | 5919 (4.0%) | 2635 (44.5%) | 668 (25.4%) |
| 2009 | 152398 | 6527 (4.3%) | 3084 (47.2%) | 805 (26.1%) |
| 2010 | 157454 | 8143 (5.2%) | 3949 (48.5%) | 1110 (28.1%) |
| 2011 | 163572 | 9452 (5.8%) | 4472 (47.3%) | 1251 (28.0%) |
Within one year of low T measurement
Figure 1.
Total Testosterone Tests Performed and No. of Hypogonadal Men by Year
Figure 2.
Percentage of Men Receiving Testosterone Tests and Percentage of Low T Tests by Year
In men ages 40–49 years, the increase in annual T testing was more substantial over the period of study compared to other decade-age groups. Among this age group, testing yearly increased from 2.6% in 2002 to 6.6% in 2011 (Supplemental Table 1). Similar to men of all ages, the observed increase in annual testing occurred primarily between 2007 and 2011, during which the proportion tested yearly increased from 3.0% to 6.6%.
In men age 70 years and older, T testing yearly was proportionately less and increased minimally during the study period compared to other age groups. The proportion of men tested annually in this age group was 0.7% between 2002 and 2006 and rose to 0.9% in 2011 (Supplemental Table 1).
Among all men who underwent serum T testing, the proportion with a diagnosis of diabetes mellitus (DM) was 13.7% (Table 2). Among men who were tested, the proportion with DM was lowest among men ages 40–49 (9.2%) and highest among men ages 60–69 (16.1%) (Data not shown). The proportion of men who were obese (BMI >= 30) was 41.8% . The average body mass index (BMI) among tested men was 29 kg /m2, was stable over the period of study, and demonstrated little variation among different decade-age groups.
Table 2:
Prevalence of Diabetes and Average BMI among VISN 20 men aged 40–89 who underwent testosterone testing, who have low T, and who were treated with T, 2002 to 2011
| Men 40–89 years | 2002–2011 |
|---|---|
| Total VISN 20 Men | 351421 |
| Total No. Tested for T (% of total men) | 44762 (12.7%)a |
| # Diabetes ICD9 Code (%) | 6213 (13.9%) |
| BMI (Mean (SD)) | 29.3 (5.4) |
| Obese (BMI>=30) | 18725 (41.8%) |
| Total No. Low T (% of total tests) | 17546 (39.2%)b |
| # Diabetes ICD9 Code | 3858 (22.0%) |
| BMI (Mean (SD)) | 31.9 (6.9)_ |
| Obese (BMI>=30) | 9920 (56.5%) |
| Given TRT (% of low T) | 6792 (38.7%)c |
| # Diabetes ICD9 Code | 2801 (41.2%) |
| BMI (Mean (SD)) | 32.8 (6.6) |
| Obese (BMI>=30) | 4172 (61.4%) |
Missing BMI
2343
1417
360
Men with low testosterone
Among all men who underwent T testing, there was a 2.3-fold increase over the study period in the number of men with initial low T levels in each year (Table 1, Figure 1), but relatively less increase over time in the proportion of men found to have low T levels yearly, from 35.0% of men tested in 2002 to 47.3% in 2011 (Figure 2). While a rise in the proportion of men with low T annually was seen in all decade-age groups, it was most substantial in the youngest men and least in the oldest men, with 66%, 58%, 25% and 9% increases in the proportion of men with low T in the 40–49, 50–59, 60–69 and 70+ age groups, respectively.
Twenty-five percent of men of all ages with low T had diabetes mellitus (Table 2). Among men with low T, the proportion with DM increased with increasing decade-age group, where 16%, 23%, 28% and 30% of men with low T had DM in the 40–49, 50–59, 60–69, and 70+ age groups respectively. The proportion of men who obese was 56.5%. The average BMI of men with low T was 32 kg/m2 (Table 2). This value was stable over the period of study, and was similar among different decade-age groups. Men who underwent serum testosterone testing and were found to have low T were, on average, obese and a significant proportion of these men had a diagnosis of diabetes mellitus.
Testosterone treatment
The total number of men treated with T annually nearly tripled from 443 in 2002 to 1251 in 2011 (Table 1, Figure 1). However, there was no increase in the proportion of all men with low T in each year who were treated with T, with 31% of men with low T treated in 2002 and 28% treated in 2011 (Figure 2). Among men with low T, a small decline in the proportion treated yearly was seen in every decade-age group. Approximately 30% of men with low T were treated annually with T, with the exception of men aged 70+, in which 20% were treated yearly with T. Among treated men, 41% had DM (Table 2) and the proportion with DM generally increased slightly with increasing decade-age group, where 30%, 40%, 47% and 41% of men with low T who were treated had a diagnosis of DM in the 40–49, 50–59, 60–69, and 70+ age groups respectively (data not shown). The proportion of men who were obese was 61.4%. The average BMI of men treated with T was 33 kg/m2, was unchanged over the period of study, demonstrated little variation among different decade-age groups and was only slightly higher than that of all men with low T. Men who were found to have low T and underwent testosterone treatment were, on average, obese and a significant proportion of these men had a diagnosis of diabetes mellitus.
Throughout the period of study, most men were treated with injectable T (81.4%), as compared to T patches (13.2%) and T gels (5.4%). The use of all treatment modalities increased over the period of study.
Discussion
We found that the number and proportion of men undergoing serum T testing yearly in the Pacific Northwest VA Healthcare system nearly doubled over the last three years. With this rise, there was a concomitant rise in the proportion of men with low T in each year, suggesting that testing may have been more targeted in later years.
Although the absolute number of men treated annually with T doubled, the proportion of men with low T levels who were treated with T yearly remained relatively unchanged from 2002–2011. This contrasts to several other studies that reported a substantial increase in T-prescriptions over the past several years.
Specifically, our data differs from a recent work by Layton and colleagues, who reported testosterone prescribing patterns in the U.S. from the MarketScan Commercial Claims database and in the U.K. from the Clinical Practice Research Datalink(7). Although this study found an increase in T prescription over 10 years, this increase occurred despite a decline in the proportion of men with low T levels. Authors concluded that testosterone testing in the U.S. population may be less targeted to symptoms, and more driven by direct to consumer marketing of testosterone replacement pharmaceuticals. Layton noted that the percentage of men tested with low T remained near 20% from 2007 to 2011 in the U.S., while the percentage of men with low T rose from less than 10% to nearly 30% among men tested in the U.K. While trends in the VA appear more similar to those reported for the U.K., testing appears even more targeted in the VA population, with the percentage of men with low T rising from 35% to nearly 50% in this healthcare setting.
Work by Baillargeon and colleagues described increased testosterone utilization from 2001 to 2011 using data from the Clinformatics DataMart, one of the largest U.S. commercial health insurance populations(9). The authors noted that the percentage of male subscribers aged 40 years and over rose from 0.54% in 2001 to 2.29% in 2011. While suggesting a significant and more than 4-fold rise in T utilization in this population, the interpretation of these data is limited by the lack of concomitant information on T testing and the proportion of men with low T. Among male subscribers in the Northwest VA population, rise in T utilization as a proportion of the total number of eligible men was far more modest, with 0.34% of the total receiving T in 2002 and 0.76% of the total receiving T in 2011.
Handelsman described global testosterone prescribing from 2000 to 2011 for 41 different countries(8). Data from IMS Heal was used to calculate number of T doses per month per 1000 of the eligible population, and suggests that T prescribing in the U.S. rose by more than 10-fold over the period of study. However, given that T utilization overall rose just over 2-fold from 2002 to 2011 in the VISN 20 population, it seems that the trends described by Handelsman are not reflected in Veterans in the VISN 20 Health Network.
Hall and colleagues described changes in T utilization in the province of Saskatchewan, Canada from 1976 to 2008(10). Similar to our results, these authors reported much more modest T utilization and change over the entire period of study, with 0.15% of men in 1976 rising to a peak of ~0.45% of men in 2000 receiving T. Unlike our results and those from others, this work suggests a decline in T utilization from 2000 onward, with only ~0.25% of men receiving T in 2008. Given greater prescribing constraints that may accompany a nationalized healthcare system, comparison of these data to ours is intriguing; however, such a comparison is limited given that Hall considered eligible men to be 18 and older and, like others, they do not provide information on men who are tested and found to have low T.
Other factors that may explain why annual T treatment did not increase as markedly in the VA setting as in other practice settings is that there may be greater adherence to clinical guidelines which may related to local practice patterns. In addition, the limited availability of transdermal T due to formulary restrictions is also likely to impact decisions for T treatment. Finally, the VA patient population has a high degree of medical comorbidity that may affect the patient and provider’s decision to initiate T treatment.
While providing novel information on a unique population, our data do have limitations as we were unable to ascertain if treated men had signs and symptoms of hypogonadism. Thus, despite detailed laboratory data prior to treatment, we are unable to determine which men are treated in accordance with The Endocrine Society guidelines.
In summary, this is the first report to place T treatment in the context of men having T levels tested, and of men found to have low T. Our results suggest that the number of men age 40 to 89 years who are undergoing T testing yearly has increased modestly, as has the proportion of those with low T yearly. However, the proportion of men with low T who are treated annually has not increased. This may reflect specific local clinical practice patterns and/or the impact of a more restricted pharmacy formulary that limits initial T- treatment to IM testosterone.
Supplementary Material
References
- 1.Araujo AB, O’Donnell AB, Brambilla DJ, Simpson WB, Longcope C, Matsumoto AM, et al. Prevalence and incidence of androgen deficiency in middle-aged and older men: estimates from the Massachusetts Male Aging Study. J Clin Endocrinol Metab. 2004;89(12):5920–6. [DOI] [PubMed] [Google Scholar]
- 2.Araujo AB, Esche GR, Kupelian V, O’Donnell AB, Travison TG, Williams RE, et al. Prevalence of symptomatic androgen deficiency in men. J Clin Endocrinol Metab. 2007;92(11):4241–7. [DOI] [PubMed] [Google Scholar]
- 3.Harman SM, Metter EJ, Tobin JD, Pearson J, Blackman MR, Baltimore Longitudinal Study of A. Longitudinal effects of aging on serum total and free testosterone levels in healthy men. Baltimore Longitudinal Study of Aging. J Clin Endocrinol Metab. 2001;86(2):724–31. [DOI] [PubMed] [Google Scholar]
- 4.Bhasin S, Cunningham GR, Hayes FJ, Matsumoto AM, Snyder PJ, Swerdloff RS, et al. Testosterone therapy in men with androgen deficiency syndromes: an Endocrine Society clinical practice guideline. J Clin Endocrinol Metab. 2010;95(6):2536–59. [DOI] [PubMed] [Google Scholar]
- 5.Wu FC, Tajar A, Beynon JM, Pye SR, Silman AJ, Finn JD, et al. Identification of late-onset hypogonadism in middle-aged and elderly men. N Engl J Med. 2010;363(2):123–35. [DOI] [PubMed] [Google Scholar]
- 6.Anawalt BD, Hotaling JM, Walsh TJ, Matsumoto AM. Performance of total testosterone measurement to predict free testosterone for the biochemical evaluation of male hypogonadism. J Urol. 2012;187(4):1369–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Layton JB, Li D, Meier CR, Sharpless J, Sturmer T, Jick SS, et al. Testosterone Lab Testing and Initiation in the United Kingdom and the United States, 2000–2011. J Clin Endocrinol Metab. 2014:jc20133570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Handelsman DJ. Global trends in testosterone prescribing, 2000–2011: expanding the spectrum of prescription drug misuse. Med J Aust. 2013;199(8):548–51. [DOI] [PubMed] [Google Scholar]
- 9.Baillargeon J, Urban RJ, Ottenbacher KJ, Pierson KS, Goodwin JS. Trends in androgen prescribing in the United States, 2001 to 2011. JAMA Intern Med. 2013;173(15):1465–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hall SA, Ranganathan G, Tinsley LJ, Lund JL, Kupelian V, Wittert GA, et al. Population-based patterns of prescription androgen use, 1976–2008. Pharmacoepidemiol Drug Saf. 2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.