Abstract
STUDY QUESTION
Are male factor infertility or remaining childless risk factors for unipolar depression among men in assisted reproductive technology (ART) treatment?
SUMMARY ANSWER
Male factor infertility was not associated with a significantly increased risk of unipolar depression and men remaining childless did not have a significantly increased risk of developing unipolar depression compared to men in ART treatment who became fathers.
WHAT IS KNOWN ALREADY
Men in medically assisted reproduction due to male factor infertility are more distressed and have more negative emotions such as feelings of loss, stigma and low self-esteem compared to men in fertility treatment due to other infertility diagnosis. Stress is in general a risk factor for depression. However, previous studies show conflicting results whether male factor infertility is a risk factor for depression.
STUDY DESIGN, SIZE, DURATION
This national, register-based cohort study consisted of 37 913 cohabitant male partners of women in ART treatment recorded in the Danish IVF register (1994–2009). Via a national register, the men’s personal identification number data were linked to the Danish Psychiatric Central Research Register (PCRR) (1969–2009) which records psychiatric diagnoses including unipolar depression, based on the ICD-8 and ICD-10 classification system.
PARTICIPANTS/MATERIALS, SETTING, METHODS
The full cohort of male partners (n = 37 913) was included in the initial analysis on prevalence of unipolar depression before or after ART treatment initiation. The association between male factor infertility and unipolar depression diagnosis after initiating ART treatment was analysed with Cox regression analysis in a sub-study population of men with the exclusion of men having a depression prior to ART treatment or not having full data on educational level and infertility diagnosis (n = 34 817).
MAIN RESULTS AND THE ROLE OF CHANCE
Overall, 1.2% (n = 446) of the men were diagnosed with unipolar depression either before initiating ART treatment (n = 146) or during follow-up (n = 300). In all, 76.0% of men with depression prior to or after ART treatment achieved fatherhood compared to 82.3% of men without depression (P < 0.001). In the sub-study population (n = 34 817, which included 266 men with a unipolar depression diagnosis), male factor infertility was not associated a significantly increased risk of depression (adjusted hazard ratio (aHR) = 1.04, 95% CI: 0.79–1.36, P = 0.804), and ART-treated men who remained childless did not have a significantly increased risk of developing depression compared to ART treated men who became fathers (aHR = 1.13, 95% CI: 0.87–1.48, P = 0.355).
LIMITATIONS, REASONS FOR CAUTIONS
Only severe cases of depression are recorded and included in this national register-based study given that only men with clinically diagnosed unipolar depression recorded in a psychiatric hospital (in-patient and out-patient) are included in the Danish PCRR. It is difficult to completely rule out an association between the exposures and depression as this outcome is so rare, and therefore the results are still statistically uncertain despite a large cohort. Furthermore, only men in ART treatment were included in this study, and caution should be taken in generalising findings to the total population of men in all areas of medically assisted reproduction or infertile men who have not sought treatment.
WIDER IMPLICATIONS OT THE FINDINGS
This large national cohort study suggests that despite evidence showing that male factor infertility is a potential severe stressor for men, which can increase psychological distress and negative emotions, infertile men in ART treatment and men remaining childless after ART are not at a significantly increased risk of developing clinically diagnosed unipolar depression.
STUDY FUNDING/COMPETING INTERESTS
C.S.S. was funded by unrestricted research grants received by Lone Schmidt from The Danish Health Insurance Foundation (J.nr. 2008B105) and Merck Sharp & Dohme (MSD). The sponsors had no influence on how data were retrieved and analysed or on the conclusions of the study. C.S.S. and L.S. have declared conflicts of interests; the remaining co-authors have no conflicts of interests to declare.
TRIAL REGISTRATION NUMBER
Not applicable.
Keywords: ART treatment , cohort study , fatherhood , male factor infertility , register-based research , unipolar depression
WHAT DOES THIS MEAN FOR PATIENTS?
This study measured the rate of depression in men in fertility treatment and whether male fertility problems and childlessness were connected to a higher risk of depression. In our study, we used data from large national registers in Denmark. Nearly 40 000 men cohabiting with/married to women having had fertility (ART) treatment during 1994–2009 were identified and included in this study. Depression diagnoses were taken from the Danish national psychiatric register, which records severe depression diagnoses given by a psychiatrist in an in- or out-patient hospital setting. Overall, 1.2% of the men had a depression diagnosis. Men with a depression diagnosis before or after ART treatment were less likely to become fathers. Men with poor semen quality (male factor infertility) had no increased risk of developing depression compared to men with other infertility diagnoses. Men who did not become fathers after ART did not have a higher risk of developing depression than men who did become fathers.
Introduction
Male factor infertility is the sole or contributing factor for at least half of couples experiencing infertility (Keihani et al., 2019). Since the 1990s, qualitative studies among men seeking medically assisted reproduction (MAR) treatment have found that male factor infertility is a severe stressor and associated with a sense of reduced masculinity (Greil, 1991; Schmidt, 1996; Tjørnhøj-Thomsen, 2009; Dolan et al., 2017; Sylvest et al., 2018). These results have been confirmed through studies using data collected from self-reported questionnaires (e.g. Nacthigall et al., 1992; Schick et al., 2016; Warchol-Biedermann, 2019). Additional studies have reported higher levels of depressive symptoms among infertile men compared to fertile men in MAR treatment (Droszdol et al., 2009; Volgsten et al., 2010; Warchol-Biedermann, 2019). A recent register-based study from the USA showed a higher risk of developing depression (HR = 1.19, 95% CI: 1.04–1.36) among men diagnosed with infertility compared to all men tested for infertility (Eisenberg et al., 2016). In contrast, a review on psychosocial and social aspects of infertility concluded that rates of clinically significant mental health problems in infertile men and in the general population were similar (Fisher and Hammarberg, 2012).
The International Classification of Diseases, ICD-10 defines unipolar depression as the presence of several symptoms simultaneously (World Health Organization, 2008), hereafter referred to as ‘depression’. In general, stressful life events are risk factors for developing unipolar depression, when this definition of depression is used (Kessler, 1997; Kendler et al., 1999). The unfulfilled wish for a child is a major life stressor regardless of the source of infertility. One review, based on studies among men in MAR treatment, showed that unsuccessful treatment was a risk factor for psychological maladjustment 1 year after treatment initiation (Martins et al., 2016). Other studies have shown that for men, treatment termination without having achieved fatherhood is a risk factor for increased depressive symptoms and lower quality of life compared to men having achieved fatherhood (Johansson et al., 2010). A cohort study based on structured diagnostic interviews reported that 15.3% of men with unsuccessful MAR treatment met the criteria for major depressive disorder/depression at one point during an 18-month period after MAR treatment initiation (Holley et al., 2015).
In a review by Martins et al. (2016), the authors concluded that very few prospective studies on mental health consequences of MAR focus on men. The aim of this longitudinal register-based cohort study was to investigate the prevalence and timing of depression diagnosis in men undergoing assisted reproductive technology (ART) treatment (i.e. IVF and/or ICSI cycles followed by fresh or frozen/thawed embryo transfer) and to determine whether male factor infertility or remaining childless after ART were risk factors for developing depression.
Materials and Methods
Setting
In the Danish public healthcare system, women or couples with no shared children are offered reimbursement for up to three ART cycles with fresh embryo transfer, and an unlimited number of frozen/thawed embryo transfer cycles (FET) and insemination cycles, up until the woman turns 41. About half of all MAR treatments are provided in the public system. In the private healthcare system, MAR treatment is offered as a fee-for service to women under 46. The Danish law restricts fertility treatment to women after age 46, but no such limit exists for the male partner.
Study population and data
The present study is a part of the Copenhagen Multi-centre Psychosocial Infertility (COMPI) Research Programme (Schmidt, 2006). The first Danish National ART-Couple I (DANAC I) Cohort (Schmidt et al., 2013) included all women registered in the Danish IVF Register from its start 1 January 1994 to 30 September 2009 (n = 42 915, see Fig. 1). Both public and private clinics must report all ART cycles (i.e. in vitro fertilisation (IVF), intracytoplasmic sperm injection (ICSI), FET and oocyte recipient cycles). Since 2007, all intrauterine insemination (IUI) cycles are also reported in the Danish IVF Register. However, the DANAC I cohort only includes ART cycles. The IVF Register also covers data on infertility diagnoses. For the purposes of this study, data on infertility diagnosis was retrieved and, for the primary analyses, dichotomised into (i) male factor infertility and (ii) other infertility diagnoses consisting of all diagnoses other than male factor infertility.
Figure 1.
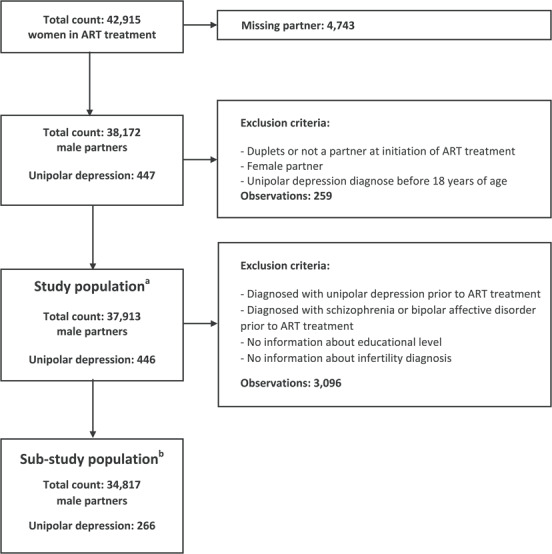
Flow diagram including the exclusion criteria for the two study populations of the Danish National ART-Couple I (DANAC I) Cohort. aThe study population is used in the comparison of men with depression before and after initiating ART treatment and men with and without depression. bThe sub-study population is used in the Cox regression analyses. Abbreviation: ART, assisted reproductive technology.
All residents in Denmark are provided with a personal identification number immediately after birth or immigration. This number is used in all healthcare registers and socio-demographic registers and ensures precise linkages between registers providing researchers with a large and comprehensive data source in which to explore their variable of interest.
The male cohabiting/married partner of each of the women in the DANAC I Cohort was identified based on the socio-demographic registers from Statistics Denmark. In Denmark, on average during the last 30 years, almost 40% of cohabiting heterosexual couples in the reproductive age groups are not married (Statistics Denmark, 2020). Hence, in this study a male partner of the unmarried woman was defined as (i) the cohabiting male, who was father of a common child; (ii) the cohabiting male with an age difference of ~15 years and no close relation; or (iii) the cohabiting male closest to the woman’s age in the case of more than one adult male residing at the same address. If a woman lived with more than one man over the time period that fulfilled the criteria, the man she lived with at the time of initiation of ART treatment was included in the study.
Data on depression diagnoses were retrieved from the Danish Psychiatric Central Research Register (PCRR) established in 1969. This register includes data on all psychiatric hospital admissions and, from 1995, all out-patient treatments and emergency room contacts (Mors et al., 2011) along with psychiatric diagnoses using ICD-8 and ICD-10. Visits to, and diagnoses assigned by, general practitioners or psychiatrists outside the hospital setting are not included in this register. These non-hospital depression diagnoses constitute the vast majority of the medically treated individuals, up to 85–90%, aged 15–44-year-old men and women. However, about one-quarter of these individuals will initially or within a 5-year window of the medical treatment also receive hospital care (Musliner et al., 2019).
For this study, the following ICD codes were included: depression ICD-8 (296.0, 296.2) and ICD-10 (F32, F33); schizophrenia ICD-8 (295.0–295.3, 295.5–295.9, 297.0–297.1, 297.9, 298.0–298.3, 298.8–298.9, 299.0) and ICD-10 (F20–F29); and bipolar affective disorder ICD-8 (296.1, 296.3, 296.8, 296.9) and ICD-10 (F30, F31). The psychiatric diagnoses were determined by the date of the first admission or the first outpatient contact. A diagnosis of schizophrenia or bipolar affective disorder was used to establish the study population for the Cox regression analyses, where we excluded men with a depression, schizophrenia or bipolar affective disorder diagnosis prior to ART treatment. The diagnoses were dichotomised (yes/no).
The Fertility Database supplied information about the study sample’s children. This register contains information from 1980 and onward about all births in Denmark. The register includes date of birth, parity, singleton or multiple birth, stillbirth and death of child (Blenstrup and Knudsen, 2011). In this study, only the first live birth was included (single/multiple births). Unfortunately, it was not possible to determine the source of conception (i.e. spontaneous conception or treatment-related conception).
The National Socio-Demographic registers (established in 1995) supplied information on age, educational level and migration. In the analyses, we used the highest obtained education level at the time of the man’s first ART treatment. As no information on the highest obtained educational level was available for men with their first ART treatment in 1994, the highest obtained educational level for 1995 was used in its place. The International Standard Classification of Education (ISCED) system was used to categorise the educational level: (i) low (up to 10 years of education), (ii) medium (upper secondary education, vocational education and academy profession), (iii) high (professional bachelor programs) and (iv) highest (Bachelor and Master’s programs and PhD).
The Danish Register of Causes of Death was used to determine whether individuals in the study population were now deceased.
Our study population consisted of n = 37 913 men. Men with depression diagnosed before the age of 18 years were excluded from the study population. Additionally, we constructed a sub-study population to investigate, with the use of survival analyses, the risk of depression with regards to male factor infertility and staying childless. Here, we excluded 3096 men who were diagnosed with depression, schizophrenia or bipolar affective disorder prior to ART treatment or had missing information about educational level or infertility diagnosis. In total, 34 817 men were eligible for the survival analyses. Study and sub-study populations are depicted in the flow chart in Fig. 1.
Ethical approval
This project was approved by the Danish Data Protection Agency (J.nr. 2008-41-2076), the National Board of Health (J.nr. 7-505-29-1658/1), the Danish Medical Agency and Statistics Denmark (J.nr. 703481). The project follows the Helsinki II Declaration. According to the Danish law, register-based studies are not required to receive approval from a scientific ethical committee, as these studies do not involve direct contact with participants.
Statistical analysis
The statistical analyses were conducted in SAS version 9.3 (SAS Institute Inc., Cary, NC, USA).
First, we explored for the full study population: (i) the timing of the most recent depression for men with a diagnosis prior to initiating ART treatment and (ii) the timing of the first depression for men with their first diagnosis after ART treatment.
Second, crude comparisons between men with their first depression diagnosis prior to versus after ART treatment were made with regard to infertility diagnosis, highest obtained educational level, and fatherhood (χ2 tests), age at onset of depression and age at first ART treatment (Student t tests). The same descriptive factors were compared for men with and without a depression diagnosis. Further, men with male factor infertility were compared to men with other infertility diagnoses with regard to fatherhood status, highest obtained educational level, and reason of censoring (see below) (χ2 tests), age at onset of depression and age at first ART treatment (t test).
Third, multiple Cox regression analyses were conducted to investigate the risk of depression in relation to male factor infertility (male factor infertility versus other infertility diagnosis (reference group)), becoming a father (time-dependent exposure; no, yes (reference group)), and with male age as the underlying time scale. Time at risk was defined as the age interval from initiation of ART treatment until a first diagnosis of depression, schizophrenia or bipolar affective disorder, migration, death or end of study (30 September 2009), whichever came first. Three different age-adjusted models were analysed. In Model 1, the effects of male factor infertility and childlessness were investigated separately with adjustment for year of initiating ART treatment. In Model 2, the two separate analyses were further adjusted for highest obtained educational level. Model 3 included mutual adjustment between the two exposures, otherwise adjusted as Model 2.
Fourth, sub-group analyses (Models 1 and 2) were conducted to investigate the association between male factor infertility and depression in two groups: (i) men who were childless and (ii) men who were already fathers before initiating ART. In the former analysis, Model 3 including male factor infertility and no fatherhood was also conducted. In all analyses in the former sub-group, men were censored when they achieved fatherhood.
Fifth, sensitivity analyses were conducted to investigate whether the categorisation of infertility diagnoses influenced the results. Four different categorisations were investigated: (i) a dichotomised exposure comparing male factor and mixed infertility (female and male) to other infertility diagnoses; (ii) a trichotomised exposure of male factor, mixed (female and male), and other infertility diagnoses; (iii) a trichotomised exposure of male factor, unexplained and other infertility diagnoses (including mixed); and (iv) a four group exposure of male factor, mixed (female and male), unexplained and female infertility. The four different categorisations were analysed with Models 1 to 3.
Results
Depression diagnosis and timing of ART treatment
Among the 37 913 men, who received ART treatment, 446 (1.2%) were diagnosed with a depression during the study period, and 146 (32.7%) of these were diagnosed prior to initiation of ART treatment. Among these 146 men, we detected the following cumulative proportion with the most recent depression within four periods, 1-, 2-, 5- and 10-year period, before ART treatment of 11.6, 26.0, 59.6 and 94.5%, respectively (Fig. 2). The mean age at the most recent depression before ART treatment was 32.9 years (SD ± 7.2 years).
Figure 2.
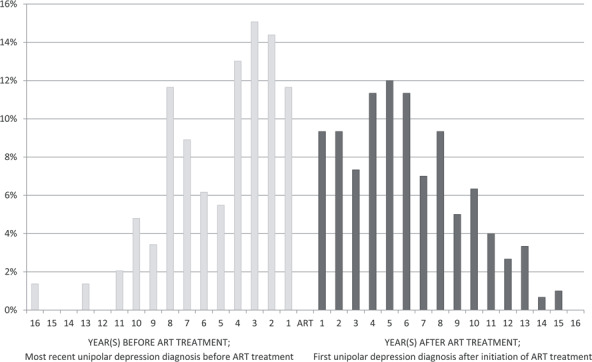
Men and unipolar depression diagnosis—time of unipolar depression diagnosis in relation to the date of the first assisted reproductive technology (ART) treatment. LEFT: the most recent depression diagnosis prior to ART treatment among men having a first depression prior to ART (n = 146) RIGHT: the first depression diagnosis after initiating ART treatment among men having a first depression after ART (n = 300) Abbreviation: ART, assisted reproductive technology.
Of the men with their first depression diagnosis after initiation of ART treatment (N = 300), 9.3% were diagnosed within 1 year (Fig. 2) and 18.7, 49.3 and 88.3% within a 2-, 5- and 10-year period after initiation of ART treatment, respectively.
Overall, significantly fewer men with a depression diagnosis, either prior to or after initiation of ART treatment, experienced fatherhood (group III), only 76.0% compared to 82.3% of men without depression (group IV; P < 0.001) (Table I). Men with a prior depression (Group I) were 1.6 years older at the start of ART treatment compared to men with their first depression diagnosis after ART treatment initiation (Group II). Furthermore, men with their first depression prior to ART treatment were more likely to be diagnosed with male factor infertility compared to the men with their first depression diagnosis after ART treatment initiation (46.0 vs. 27.8%; P < 0.001). No difference was found between men with and without a depression diagnosis in relation to the type/cause of infertility (P = 0.186).
Table I.
Comparisons of men according to time of unipolar depression diagnosis and ART treatment.
| Men with their first unipolar depression diagnosis prior ART treatment (I) | Men with their first unipolar depression diagnosis after ART treatment (II) | P value comparing I vs. II | All men with a unipolar depression diagnosis (III) | Comparison group, men without a unipolar depression diagnosis (IV) | P value comparing III vs. IV | |
|---|---|---|---|---|---|---|
| Men, n | 146 | 300 | - | 446 | 37 467 | - |
| Age at onset of unipolar depression (years), mean (±SD) | 32.4 (±7.3) | 41.3 (±7.3) | < 0.001 | 38.4 (±8.4) | - | - |
| Age at first ART treatment (years), mean (±SD) | 37.5 (±7.3) | 35.9 (±6.4) | 0.016 | 36.4 (±6.7) | 35.1 (±5.6) | <0.001 |
| Age range at first ART treatment (years) | 23.8–62.8 | 19.9–69.1 | - | 19.9–69.1 | 19.4–77.6 | - |
| Infertility diagnosis, N (%)a | <0.001b | 0.186b | ||||
| Male factor infertility | 64 (46.0) | 80 (27.8) | 144 (33.7) | 11 231 (31.8) | ||
| Mixed female and male factor | 8 (5.8) | 28 (9.7) | 36 (8.4) | 3135 (8.9) | ||
| Ovulation disorder | 12 (8.6) | 9 (3.1) | 21 (4.9) | 2273 (6.4) | ||
| Tubal pathology | 30 (21.6) | 108 (37.5) | 138 (32.3) | 9966 (28.2) | ||
| Other female factor | 6 (4.3) | 15 (5.2) | 21 (4.9) | 1938 (5.5) | ||
| Unexplained | 19 (13.7) | 48 (16.7) | 67 (15.7) | 6765 (19.2) | ||
| Highest obtained educational level | 0.565 | <0.001 | ||||
| I Low | 33 (22.6) | 84 (28.0) | 117 (26.2) | 6056 (16.2) | ||
| II Medium | 72 (49.3) | 148 (49.3) | 220 (49.3) | 20 714 (55.3) | ||
| III High | 18 (12.3) | 33 (11.0) | 51 (11.4) | 4632 (12.4) | ||
| IV Highest | 16 (11.0) | 27 (9.0) | 43 (9.6) | 5386 (14.4) | ||
| Unknown | 7 (4.8) | 8 (2.7) | 15 (3.4) | 679 (1.8) | ||
| Live birth | 0.995 | <0.001 | ||||
| Yes | 111 (76.0) | 228 (76.0) | 339 (76.0) | 30 847 (82.3) | ||
| No | 35 (24.0) | 72 (24.0) | 107 (24.0) | 6620 (17.7) |
Comparisons of men with a unipolar depression diagnosis prior to ART treatment (I) to men with a unipolar depression diagnosis after initiation of ART treatment (II). Comparisons of men in ART treatment with a unipolar depression diagnosis at any point in time (III) to men without a unipolar depression diagnosis (IV)
aIn total, 2178 individuals are lacking information on infertility diagnosis; of men with a unipolar depression diagnosis prior to ART treatment n = 7; of men with a unipolar depression diagnosis after ART treatment n = 12; of men in the comparison group of men without a unipolar depression diagnosis n = 2159.
bThe P value is calculated on behalf of information on infertility diagnosis without the individuals with missing information on infertility diagnosis. Abbreviations: ART, assisted reproductive technology; SD, standard deviation.
Male factor infertility and remaining childless
The remaining results are based on the sub-study population consisting of 34 817 men (exclusion: diagnosis of depression/schizophrenia/bipolar affective disorder prior ART treatment, lack of information on education or infertility diagnosis). Of these, 266 men developed depression after initiation of ART treatment (Fig. 1). Men with and without a male factor infertility diagnosis were very similar in relation to the co-variables presented in Table II.
Table II.
Men in assisted reproductive technology (ART) treatment.
| Male factor infertility diagnosis | Other infertility diagnosis a | P value | |||
|---|---|---|---|---|---|
| Men, n (% of total population) | 11 052 | (31.7) | 23 765 | (68.3) | - |
| Person-years of follow-up | 72 508 | 195 379 | - | ||
| Unipolar depression diagnosis, n (%) | 73 | (27.4) | 193 | (72.6) | - |
| Censoring/end of study, n (%) | 0.018 | ||||
| End of study | 10 522 | (95.8) | 22 497 | (95.4) | |
| Migration | 322 | (2.9) | 824 | (3.5) | |
| Schizophrenia | 12 | (0.1) | 27 | (0.2) | |
| Bipolar affective disorder | 7 | (0.1) | 13 | (0.1) | |
| Mortality | 116 | (1.1) | 201 | (0.9) | |
| Mean age at first ART treatment (years), mean (±SD) | 35.0 | (±5.9) | 35.0 | (±5.4) | 0.783 |
| Mean age at unipolar depression diagnosis (years), mean (±SD) | 40.9 | (±7.3) | 40.9 | (±6.8) | 0.965 |
| Highest obtained educational level, n (%) | 0.011 | ||||
| I Low | 1785 | (16.2) | 4002 | (16.8) | |
| II Middle | 6329 | (57.3) | 13 257 | (55.8) | |
| III High | 1399 | (12.7) | 2947 | (12.4) | |
| IV Highest | 1539 | (13.9) | 3559 | (15.0) | |
| Live birth | 0.054 | ||||
| Yes | 8667 | (78.4) | 18 851 | (79.3) | |
| No | 2385 | (21.6) | 4914 | (20.7) | |
Descriptive analysis for the sub-study population of the men (n = 34 817) included in the Cox regression analysis
aOther infertility diagnosis includes mixed female and male factor, ovulation disorder, tubal pathology, other female factor, or unexplained infertility. Abbreviations: SD, standard deviation.
In the Cox regression analyses, we found no evidence that ‘no child’ (i.e. remaining childless) or ‘male factor infertility’ per se increased the risk of depression in men following ART treatment (Table III). Adjustment for educational level (Model 2) did not change the risk estimates. In Model 3, which included ‘no child’ and ‘male factor infertility’ with mutual adjustment, the results were similar. The sensitivity analyses including four categorisations of infertility diagnosis (described in the Statistical analysis section) confirmed the findings of the main analyses.
Table III.
Results from the Cox regression analyses.
| Model 1 a | Model 2 b | Model 3 c | |||||||
|---|---|---|---|---|---|---|---|---|---|
| HR | 95% CI | P value | HR | 95% CI | P value | HR | 95% CI | P value | |
| Unipolar depression diagnosis by fatherhood status | |||||||||
| No child | 1.15 | 0.88–1.50 | 0.305 | 1.13 | 0.87–1.48 | 0.357 | 1.13 | 0.87–1.48 | 0.355 |
| Child | 1 (ref) | 1 (ref) | 1 (ref) | ||||||
| Unipolar depression diagnosis by infertility diagnosis | |||||||||
| Male factor infertility | 1.03 | 0.79–1.35 | 0.816 | 1.03 | 0.79–1.35 | 0.816 | 1.04 | 0.79–1.36 | 0.804 |
| Other infertility diagnosis’d | 1 (ref) | 1 (ref) | 1 (ref) | ||||||
Unipolar depression diagnosis by fatherhood status and infertility diagnosis among n = 34 817 men from the Danish National ART-Couple I (DANAC I) Cohort
aModel 1 = no fatherhood or male factor infertility diagnosis adjusted for age and ART treatment year.
bModel 2 = no fatherhood or male factor infertility diagnosis adjusted for age, ART treatment year and highest obtained educational level.
bModel 3 = mutually adjusted for no fatherhood and male factor infertility diagnosis; otherwise, adjusted as described in model 2.
dOther infertility diagnosis includes mixed female and male factor, ovulation disorder, tubal pathology, other female factor, or unexplained infertility. Abbreviations: 95% CI, 95% confidence interval; HR, hazard ratio.
Discussion
Overall, 1.2% of the men in ART treatment were diagnosed with depression, and of these most were diagnosed with depression after initiation of ART treatment. Neither male factor infertility nor remaining childless was associated with a significantly increased risk of depression diagnosis. To our knowledge, this is the first large-scale study among men in ART treatment using a national psychiatric register to measure depression prevalence. Two previous large register-based studies have investigated the association between fatherhood and psychiatric episodes in a cohort of men in ART treatment (Agerbo et al., 2013; Munk-Olsen and Agerbo, 2015). However, these studies did not differentiate between different types of psychiatric disorders, and as such the prevalence of those with depression is unknown. In these studies, no association was found between fatherhood and any psychiatric disorder (Agerbo et al., 2013). Furthermore, there was no association between fatherhood and development of a psychiatric disorder after childbirth (Munk-Olsen and Agerbo, 2015). Our results and the previous findings support the theory that men in ART treatment are not at risk of developing a psychiatric disorder including depression if fatherhood is not obtained.
Previous studies on male factor infertility and depression have mainly been based on qualitative studies or self-reported questionnaires (Greil, 1997) frequently measuring less severe depression/depressive symptoms, whereas in our study depression was defined by a diagnosis by a psychiatrist in a hospital setting (in-patient/out-patient). This information was accessed through a large-scale health-based register that includes all Danish citizens.
Previous studies indicate that male factor infertility is a stressor (Greil, 1997) and that having low sperm quality may be associated with depressive symptoms (Zorn et al., 2008). Volgsten et al. (2010) reported an association between male factor infertility and increased risk of depressive and/or anxiety disorders among 320 men in ART treatment. However, the authors emphasise that this finding should be interpreted with caution due to the small sample size. A more recent register-based study among 13 027 men with male factor infertility found, in line with Volgsten and colleagues (2010), a slight but significantly increased risk of developing depression after being diagnosed with male factor infertility compared with vasectomised men (Eisenberg et al., 2016), which is in contrast to our findings.
Men diagnosed with depression prior to or after ART treatment had a significantly lower chance of achieving fatherhood compared to men without depression prior to or after ART. These results are consistent with a Danish population-based register study investigating the likelihood of becoming a parent after a depression diagnosis (Laursen and Munk-Olsen, 2010). Little is known about this association; however, one may speculate that in our study population, vulnerable men might be more likely to discontinue ART treatment and therefore have a lower chance of fatherhood.
A smaller proportion of men (1.2%) were diagnosed with depression in comparison to the women in the DANAC I cohort (2.6%) (Sejbaek et al., 2013). This is consistent with the general population, where men are also less likely to be diagnosed with depression. A Danish study of randomly selected men and women showed an overall prevalence of depression of 3.1% in men versus 4.9% in women (Olsen et al., 2004). These percentages are based on a self-reported questionnaire that includes symptoms for mild to severe depression; hence, direct comparison to our study is not possible. One explanation for gender differences in depression rates could be that the diagnostic criteria used for the depression diagnosis might not be adequate for men. When including alternative symptoms more likely to be seen in males with depression (anger attacks/aggression and risk-taking behaviour) in combination with traditional symptoms of depression, similar numbers of men and women are diagnosed with depression (Martin et al., 2013). In fact, when a Male Symptoms Scale was used for a depression diagnosis, men were more likely to be diagnosed with depression than women (Martin et al., 2013). This indicates that studies in general, as well as this study, underestimate the prevalence of depression in men.
Study strengths and limitations
The strengths of this study include the use of national registers, which have shown to have acceptable validity (Blenstrup and Knudsen, 2011; Mors et al., 2011). Denmark offers a unique and important research context given access to comprehensive and longitudinal personal and health-based data of its citizens through large registers that can be linked using a personal identification number. This eliminates self-selection biases present in many other studies. The data in this study is based on one of the largest national population of men in ART treatment worldwide. The follow-up time was on average 7.7 years (range 0 to 15.7). Only live births are recorded, thus adopted children are not included. All depression diagnoses were registered in a hospital setting by a psychiatrist and including both in- and out-patient contact, whereas most previous studies used depressive symptoms from self-administered questionnaires. In addition, sensitivity analyses were conducted to validate the main findings.
Despite the strength of this large data source, the registered-based design of the study has three main limitations. First, there is room for small error in the assignment of male partners to women who share the same address but are not partnered. However, this proportion is minimal and we assume equal in the whole study population regardless of exposure or outcome.
Second, the PCRR only records diagnoses that are assigned whilst receiving treatment in a psychiatric hospital setting (in- and out-patient contact). Hence, only the most severe cases of depression are included. Those with mild to moderate depression may be treated by their general physician and/or psychiatrist or remain untreated. None of these depression episodes are tracked in the PCRR. As such, it is likely that our prevalence data are underestimated for depression in general, of various severities.
Finally, the DANAC I cohort was limited to those who are undergoing ART treatment; as a result they do not represent all men in infertile couples. Some will have undergone other MAR treatments not captured in the IVF register. As such, caution should therefore be taken in generalising these findings to the total population of infertile men.
Clinical implications
Previous studies showed that male factor infertility is a potential severe stressor among men in MAR treatment (Fisher and Hammarberg, 2012). However, this large national cohort study did not find that male factor infertility represents a risk factor of a depression diagnosis after ART treatment when compared to men in couples with other infertility diagnoses. Overall, the diagnosis of depression in relation to men still needs to be addressed as mentioned. We do not know the distribution of depression relative to type of infertility. However, for the moment, the results from this study are reassuring for men in ART and for healthcare professionals. However, our results suggest that men who were previously diagnosed with depression prior to ART treatment may need additional support whilst trying to achieve their family building goals.
In conclusion, overall 1.2% of the male population in ART treatment were diagnosed with depression prior to ART treatment or during the follow-up period. Men with male factor infertility are not at a significantly increased risk of being diagnosed with depression compared to men in ART treatment due to other causes of infertility. Furthermore, men in ART treatment who did not achieve fatherhood had a similar risk of developing depression after ART treatment compared to men who became fathers to a live-born child. However, men with a depression diagnosis were less likely to achieve fatherhood compared to men with no depression diagnosis.
Acknowledgements
This study is part of the Copenhagen Multi-centre Psychosocial Infertility (COMPI) Research Programme initiated by L. Schmidt, University of Copenhagen, 2000. The authors wish to give thanks to Gurli Pilgaard Perto (the Danish Psychiatric Central Research Register), Jørn Korsbø Petersen (Statistics Denmark) and Steen Rasmussen (prior employed at the National Board of Health) for their efforts in extracting and linking register data for this project.
Authors’ roles
All authors contributed to the concept and the design of the study. A.P. and L.S. obtained the data. C.S.S. performed the data analysis with help from J.L.F. C.S.S. drafted the article with help from A.M.S.S. All co-authors contributed in the data interpretation, critical revision of the article and final approval of the manuscript.
Funding
C.S.S. was funded by unrestricted research grants received by Lone Schmidt from the Danish Health Insurance Foundation (J.nr. 2008B105) and Merck Sharp & Dohme (MSD).
Conflict of interest
C.S.S. was funded by unrestricted research grants received by Lone Schmidt from the Danish Health Insurance Foundation (J.nr. 2008B105) and Merck Sharp & Dohme (MSD). The sponsors had no influence on how data were retrieved and analysed or on the conclusions of the study. The remaining co-authors have no conflicts of interest to declare with regards to this work.
References
- Agerbo E, Mortensen PB, Munk-Olsen T. Childlessness, parental mortality and psychiatric illness: a natural experiment based on in vitro fertility treatment and adoption. J Epidemiol Community Health 2013;67:374–376. [DOI] [PubMed] [Google Scholar]
- Blenstrup LT, Knudsen LB. Danish registers on aspects of reproduction. Scand J Public Health 2011;39:79–82. [DOI] [PubMed] [Google Scholar]
- Dolan A, Lomas T, Ghobara T, Hartshorne G. ‘It’s like taking a bit masculinity away from you’: towards a theoretical understanding of men’s experiences of infertility. Soc Health Illness 2017;39:878–892. [DOI] [PubMed] [Google Scholar]
- Drosdzol A, Skrzypulec V. Depression and anxiety among Polish infertile couples - an evaluative prevalence study. J Psychosom Obstet Gynaecol 2009;30:11–20. [DOI] [PubMed] [Google Scholar]
- Eisenberg ML, Shufeng L, Cullen MR, Baker LC. Increased risk of incident chronic medical conditions in infertile men: analysis of Inited states claims data. Fertil Steril 2016;105:629–636. [DOI] [PubMed] [Google Scholar]
- Fisher JR, Hammarberg K. Psychological and social aspects of infertility in men: an overview of the evidence and implications for psychologically informed clinical care and future research. Asian J Androl 2012;14:121–129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greil AL. Not yet pregnant In: Infertile couples in Contemporary America. New Brunswick: Ruthers University Press, 1991. [Google Scholar]
- Greil AL. Infertility and psychological distress: a critical review of the literature. Soc Sci Med 1997;45:1679–1704. [DOI] [PubMed] [Google Scholar]
- Holley SR, Pasch LA, Bleil ME, Gregorich S, Katz PK, Adler NE. Prevalence and predictors of major depressive disorder for fertility treatment patients and their partners. Fertil Steril 2015;103:1332–1339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johansson M, Adolfsson A, Berg M, Francis J, Hogstrom L, Janson PO, Sogn J, Hellstrom AL. Gender perspective on quality of life, comparisons between groups 4-5.5 years after unsuccessful or successful IVF treatment. Acta Obstet Gynecol Scand 2010;89:683–691. [DOI] [PubMed] [Google Scholar]
- Keihani S, Hanson B, Hotaling JM. Male factor infertility; an opportunity to investigate individual and family health. BJOG 2019;126:149–151. [DOI] [PubMed] [Google Scholar]
- Kendler KS, Karkowski LM, Prescott CA. Causal relationship between stressful life events and onset of major depression. Am J Psychiatry 1999;156:837–841. [DOI] [PubMed] [Google Scholar]
- Kessler RC. The effects of stressful life events on depression. Annu Rev Psychol 1997;48:191–214. [DOI] [PubMed] [Google Scholar]
- Laursen TM, Munk-Olsen T. Reproductive patterns in psychotic patients. Schizophr Res 2010;121:234–240. [DOI] [PubMed] [Google Scholar]
- Martin LA, Neighbors HW, Griffith DM. The experience of symptoms of depression in men vs women: analysis of the National Comorbidity Survey Replication. JAMA Psychiat 2013;70:1100–1106. [DOI] [PubMed] [Google Scholar]
- Martins MV, Basto-Pereira M, Pedro J, Peterson B, Almeida V, Schmidt L, Costa ME. Male psychological adaptation to unsuccessful medically assisted reproduction treatments: a systematic review. Hum Reprod Update 2016;22:466–478. [DOI] [PubMed] [Google Scholar]
- Mors O, Perto GP, Mortensen PB. The Danish psychiatric central research register. Scand J Public Health 2011;39:54–57. [DOI] [PubMed] [Google Scholar]
- Munk-Olsen T, Agerbo E. Does childbirth cause psychiatric disorders? A population-based study paralleling a natural experiment. Epidemiology 2015;26:79–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Musliner KL, Liu X, Gasse C, Christensen KS, Wimberley T, Munk-Olsen T. Incidence of medically treated depression in Denmark among individuals 15-44 years old: a comprehensive overview based on population registers. Acta Psychiat Scand 2019;39:548–557. [DOI] [PubMed] [Google Scholar]
- Nachtigall RD, Becker G, Wozny M. The effects of gender-specific diagnosis on men’s and women’s response to infertility. Fertil Steril 1992;57:113–121. [PubMed] [Google Scholar]
- Olsen LR, Mortensen EL, Bech P. Prevalence of major depression and stress indicators in the Danish general population. Acta Psychiatr Scand 2004;109:96–103. [DOI] [PubMed] [Google Scholar]
- Schick M, Rösner S, Toth B, Strowotzki T, Jank A, Kentenich H, Thöne C, Wischmann T. Effects of medical causes, role concepts and treatment stages on quality if life in involuntary childless men. Andrologia 2016;48:937–942. [DOI] [PubMed] [Google Scholar]
- Schmidt L. Psykosociale konsekvenser af infertilitet og behandling [Psychosocial consequences’of infertility and treatment, in Danish] [PhD Dissertation]. Copenhagen, Denmark: FADL Publishers; 1996. [Google Scholar]
- Schmidt L. Infertility and assisted reproduction in Denmark. Epidemiology and psychosocial consequences. Dan Med Bull 2006;53:390–417. [PubMed] [Google Scholar]
- Schmidt L, Hageman I, Hougaard CO, Sejbaek CS, Assens M, Ebdrup NH, Pinborg A. Psychiatric disorders among women and men in assisted reproductive technology (ART) treatment. The Danish National ART-Couple (DANAC) cohort: protocol for a longitudinal, national register-based cohort study. BMJ Open 2013;3:1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sejbaek CS, Hageman I, Pinborg A, Hougaard CO, Schmidt L. Incidence of depression and influence of depression on the number of treatment cycles and births in a national cohort of 42,880 women treated with ART. Hum Reprod 2013;28:1100–1109. [DOI] [PubMed] [Google Scholar]
- Denmark Statistics. Statistikbanken: Befolkning og valg [Statbank Denmark: Population and option]. https://www.statistikbanken.dk/statbank5a/default.asp?w=1536 (3 March 2020, date last accessed).
- Sylvest R, Fürbringer JK, Pinborg A, Koert E, Bogstad J, Loessl K, Praetorius L, Schmidt L. Low semen quality and experiences of masculinity and family building. Acta Obstet Gynaecol Scand 2018;97:727–737. [DOI] [PubMed] [Google Scholar]
- Tjørnhøj-Thomsen T. It’s a bit unmanly in a way: men and infertility in Denmark In: Inhorn MC, Tjørnhøj-Thomsen T, Goldberg H, MLC M (eds). Reconceiving the Second Sex - Men, Masculinity, and Reproduction. New York: Berghahn Books, 2009,226–252. [Google Scholar]
- Volgsten H, Ekselius L, Poromaa IS, Svanberg AS. Personality traits associated with depressive and anxiety disorders in infertile women and men undergoing in vitro fertilization treatment. Acta Obstet Gynecol Scand 2010;89:27–34. [DOI] [PubMed] [Google Scholar]
- Warchol-Biedermann K. The risk of psychiatric morbidity and course of distress in males undergoing inferitlity evaluation is affected by their factor of infertility. Am J Mens Health 2019;13:1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization International Classification of Diseases and Related Health Problems 10th revision: ICD-10 Version 2008.https://icd.who.int/browse10/2008/en#/ (2 December 2019, date last accessed).
- Zorn B, Auger J, Velikonja V, Kolbezen M, Meden-Vrtovec H. Psychological factors in male partners of infertile couples: relationship with semen quality and early miscarriage. Int J Androl 2008;31:557–564. [DOI] [PubMed] [Google Scholar]


