Abstract
Low testosterone (T) is frequent in men with chronic illnesses. The clinical features of T deficiency (TD) overlap with those of chronic diseases. The aim of this study is to evaluate the relative contribution of chronic disease score (CDS) and low T to the presence of TD symptoms. A consecutive series of 3862 men (aged 52.1 ± 13.1 years) consulting for sexual dysfunction were studied. Several clinical and biochemical parameters were collected, including the structured interview, ANDROTEST, for the assessment of TD symptoms. Penile color Doppler ultrasound (PCDU) was also performed. Based on the medications taken, the CDS was calculated. For a subset of 1687 men, information on mortality was collected (follow-up of 4.3 ± 2.6 years). Higher CDS was associated with lower free and total T (TT) as well as with higher ANDROTEST score. When introducing CDS and TT in multivariable models adjusted for age, severe erectile dysfunction and impaired morning erections were associated with both CDS (odds ratio and 95% confidence interaval, OR [95% CI] = 1.25 [1.13; 1.37] and 1.38 [1.29; 1.48], respectively) and low TT (OR [95% CI] = 1.11 [1.00; 1.23] and 1.13 [1.06; 1.21], respectively). Similar results were obtained for PCDU parameters. Hypoactive sexual desire was associated with low TT (OR [95% CI] = 1.21 [1.13; 1.30]), whereas it was inversely related with CDS (OR [95% CI] = 0.91 [0.84; 0.97]). When considering mortality for major cardiovascular events, TT <8 nmol l−1, but not CDS, was a significant predictor (hazard ratio [95% CI] = 5.57 [1.51; 20.63]). Chronic illnesses are associated with an overt TD. Both chronic diseases and low T can be involved in determining symptoms present in subjects complaining for sexual dysfunction. This should be considered in the diagnostic workup for TD.
Keywords: chronic diseases, erectile dysfunction, sexual symptoms, testosterone deficiency
INTRODUCTION
Testosterone (T) deficiency (TD) occurring during adulthood (i.e., late-onset hypogonadism, LOH) is a common condition, representing the main endocrine concern in the aging male. In fact, up to 14% of the European subjects older than 40 years show low T (total T <10.5 nmol l−1 or <300 ng dl−1), according to the European Male Ageing Study (EMAS) survey.1 Of them, the large majority (11.8%) have inappropriately low luteinizing hormone (LH) (LH ≤9.4 U l−1, secondary hypogonadism) and only 2% elevated LH (primary hypogonadism).1 Hence, TD is a pandemic condition. However, there is universal agreement that the biochemical demonstration of TD is not enough to define the clinical condition of LOH, the presence of specific symptoms being an essential requirement.2,3,4
Symptoms of LOH encompass a wide range of domains including psychological, physical, and sexual disturbances. According to the EMAS studies, only those related to the sexual domain (i.e., reduced libido and reduced spontaneous or sexual-related erections) show a syndromic association with TD, and, therefore, they could represent a useful correlate to define a symptomatic LOH.3,5,6,7 By restricting the construct of LOH to those having both TD and the aforementioned sexual symptoms, the figure of its representation in Europe is dramatically reduced, i.e., 2.1% of the European general population older than 40 years.3
The presence of a specific association between sexual symptoms and TD is not enough to establish the direction of the relationship; in fact, it is possible that TD is responsible for causing the symptoms or the other way around. Longitudinal extensions of the EMAS studies clarified that the development of both primary and secondary hypogonadism predicts the occurrence or worsening of sexual symptoms at follow-up.5,8 On the other hand, the incidence or worsening of these symptoms is not negligible – although lower than in men developing primary or secondary hypogonadism – even among men who remain eugonadal during the follow-up.5,8 This suggests that factors other than TD play a role in determining sexual symptoms compatible with those of LOH.
Intervention studies are useful in defining causality in the relationship between TD and sexual symptoms. In particular, it is important to understand whether treating TD might improve sexual symptoms. Several results of the Testosterone Trials (T Trials) have been published during the last few years.9 T Trials are placebo-controlled trials conducted at 12 sites across the US in 790 men aged 65 years or older with unequivocally low levels of T (total T <9.54 nmol l−1 or 275 ng dl−1) and symptoms to which TD might contribute. Interestingly, men having health conditions comorbid with TD were included in these trials with few exceptions, such as prostate cancer. The results of the Sexual Function Trial indicate a mild increase of more than 2.5 points in the erection domain of the International Index of Erectile Function (IIEF) and an increase of libido with an effect size of 0.44, indicating a moderate effect.9 A recently published meta-analysis of all the controlled trials with T therapy (TTh) involving TD subjects and employing IIEF provided similar results.10 In addition, the meta-regression analysis indicates that the magnitude of the effect was lower in the presence of metabolic derangements, such as diabetes and obesity.10 This is tantamount to say that the presence of comorbidities could dampen the effectiveness of TTh on sexual symptoms, because these comorbidities per se are responsible for their appearance.
The Chronic Disease Score (CDS) is a widely accepted measure of comorbidities.11,12 It is based on the aggregate number and complexity of prescribed medications for the selected chronic conditions (categorized by the Anatomical Therapeutic Chemical [ATC] and classification codes) and contains 25 categories. Weights are given to these disease categories and summed to obtain a numeric score ranging 0–35, with higher scores associated with a greater complexity of the comorbidity status.11,12
Although it is generally accepted that sexual symptoms are the hallmark of TD in adults, this might not be the case in patients with a high complexity of chronic conditions, as suggested by the high prevalence (20%–25%) of sexual symptoms found in the European general population irrespectively of T levels.5,8,13 Hence, the aim of this study is to evaluate the relative contribution of CDS and low T to the presence of putative TD-related symptoms in the setting of a Sexual Medicine Outpatient Clinic. Because the role of low T occurring in unhealthy men toward the development of cardiovascular (CV) adverse outcomes or CV mortality is at present still debated, a secondary aim of this study is to assess the relative contribution of CDS and low T to CV morbidity and mortality employing longitudinally collected data on major adverse CV events (MACE).
PATIENTS AND METHODS
Cross-sectional study interviews
A consecutive series of 3862 patients consulting the Sexual Medicine and Andrology Unit of the University of Florence (Florence, Italy) for sexual dysfunction between 2000 and 2015 were studied. The characteristics of the population are reported in Table 1. According to our routine clinical practice, each patient underwent a standard diagnostic protocol, which has been approved by our Hospital with the reference ID# L99-A08 292/2014. Informed consent for collecting these data was obtained from each patient. All the procedures are in accordance with the Code of Ethics of the World Medical Association. Before starting any diagnostic or therapeutic procedure, all patients were interviewed using the Structured Interview on Erectile Dysfunction (SIEDY) and ANDROTEST. SIEDY is a validated 13-item structured interview evaluating the pathogenic components of erectile dysfunction (ED).14 ANDROTEST is a validated 12-item structured interview for the screening of hypogonadism in patients with sexual dysfunction.15 In both the interviews, answers to each question are arranged on a Likert scale. The algebraic sum of the questions included in the ANDROTEST provides a total score, which is higher as the probability of having hypogonadism increases.15 ED was investigated by question #5 of ANDROTEST “Describe what happens during sexual intercourse: how often do you have lack of an erection?” Rating 0 = sometimes (<25% of cases), 1 = quite often (25%–50% of cases), 2 = often (50%–75% of cases), and 3 = always (≥75% of cases). Reduced spontaneous morning erections were assessed by question #6 of ANDROTEST “Do you ever wake up with an erection?” Rating 0 = yes, regularly (no reduction), 1 = less frequently than in the past (mild reduction), 2 = only occasionally (moderate reduction), and 3 = never (severe reduction). Reduced sexual desire was investigated by question #14 of SIEDY “Did you have more or less desire to make love in the last three months?” Rating 0 = unmodified or increased desire (no reduction), 1 = desire present but moderately reduced (mild reduction), 2 = desire remarkably reduced (moderate reduction), and 3 = desire never present (severely reduced).
Table 1.
Characteristics of the patients in the cross-sectional sample and longitudinal subset
| Characteristic | Cross-sectional sample (n=3862) | Longitudinal sample (n=1685) |
|---|---|---|
| Age (year), mean±s.d. | 52.1±13.1 | 52.8±12.6 |
| Education (%) | ||
| Primary | 13.3 | 16.8 |
| Secondary | 33.1 | 29.3 |
| Higher | 34.7 | 33.8 |
| University | 18.9 | 20.1 |
| Current smoker (%) | 29.4 | 33.7 |
| Alcohol intake >4 drinks daily (%) | 3.5 | 3.7 |
| Severe ED (>25% of cases) (%) | 13.4 | 13.9 |
| Reduced spontaneous erections (any degree) (%) | 66.6 | 61.9 |
| Hypoactive sexual desire (any degree) (%) | 37.6 | 34.4 |
| ANDROTEST score, mean±s.d. | 7.7±3.6 | 7.7±3.3 |
| Body mass index (kg m−2), mean±s.d. | 26.7±4.2 | 26.4±3.9 |
| Systolic blood pressure (mmHg), median (interquartile range) | 130.0 (120.0–140.0) | 140.0 (130.0–155.0) |
| Diastolic blood pressure (mmHg), median (interquartile range) | 80.0 (80.0–90.0) | 85.0 (80.0–95.0) |
| Mean testis volume (ml), mean±s.d. | 19.0±4.6 | 19.8±4.2 |
| Luteinizing hormone (U l−1), median (interquartile range) | 3.8 (2.6–5.6) | 3.9 (2.6–5.5) |
| Follicle-stimulating hormone (U l−1), median (interquartile range) | 4.6 (3.0–7.8) | 4.5 (3.0–6.9) |
| Total testosterone (nmol l−1), mean±s.d. | 15.5±6.4 | 16.5±6.1 |
| Sex hormone binding globulin (nmol l−1), mean±s.d. | 35.8±18.1 | 36.8±16.8 |
| Calculated free testosterone (pmol l−1), mean±s.d. | 302.1±131.5 | 322.3±126.3 |
| Penile color Doppler ultrasound, mean±s.d. | ||
| Flaccid peak systolic velocity (cm s−1) | 17.1±6.2 | 15.5±5.6 |
| Flaccid acceleration (m s−2) | 2.8±1.4 | 2.8±1.3 |
| Dynamic peak systolic velocity (cm s−1) | 51.1±19.5 | 52.4±20.3 |
| Middlesex Hospital Questionnaire subscales, mean±s.d. | ||
| Free floating anxiety | 5.4±3.6 | 6.0±3.5 |
| Phobic anxiety | 4.3±2.7 | 5.2±2.4 |
| Obsessive symptoms | 5.7±3.8 | 6.9±3.3 |
| Somatized anxiety | 3.5±2.8 | 4.1±2.8 |
| Depressive symptoms | 4.6±3.3 | 5.5±3.1 |
| Hysterical traits | 4.7±3.2 | 5.7±2.9 |
| Total score | 28.1±15.1 | 33.4±12.6 |
Data are reported as mean±s.d. if normally distributed, or median (interquartile range) when nonnormally distributed. ED: erectile dysfunction; s.d.: standard deviation
Algorithm for comorbidity burden assessment (Chronic Disease Score)
All patients were also asked to report all their comorbidities and drugs used. The systematic collection of information on medications used is part of our routine clinical practice. During the visit at the Outpatient Clinic, the physicians ask each patient to report any medication used and these are registered in the patient's medical records. The collection of these data by a clinician minimizes the risk of mistake and misclassification, thus allowing to calculate the CDS reliably. The CDS is an aggregate comorbidity measure based on the current medication use.11,12 It was originally created by a panel of health professionals who included 25 classes of medications, which are weighted in the total score to correspond to disease complexity and severity.11,12 The CDS was originally validated for use as a predictor of physician-rated disease status, self-rated health status, hospitalization, and mortality.11 CDS potentially ranges between 0 and 35, with higher values corresponding to more complicated comorbidity status.
Physical examination, blood and ecocolor Doppler tests
All patients underwent a complete physical examination, with measurement of blood pressure (mean of three measurements is 5 min apart, in a sitting position, with a standard sphygmomanometer), height, weight, and testis volume (using Prader orchidometer, ESP Models, Rustington, UK). For the purpose of the study, we considered the mean testis volume as the mean value of the left and right testes. Blood samples were drawn in the morning, after an overnight fast, for the determination of total testosterone (TT), LH, follicle-stimulating hormone (FSH), and sex hormone-binding globulin (SHBG). Blood sample analyses were performed in the central laboratory of the Careggi Teaching Hospital (University of Florence, Florence, Italy). TT was measured by immunoassay. Free T was calculated (calculated free T [cFT]) according to the Vermeulen formula in a subset of 1988 men who had TT and SHBG available.16
Penile blood flows were assessed by penile color Doppler ultrasound (PCDU) after an intracavernosal injection of 10 μg of prostaglandin E1 (dynamic evaluation), as previously reported,17 and it was available for 2341 men.
Questionnaire for psychological symptoms
The Middlesex Hospital Questionnaire (MHQ)18 was administered to each patient in order to quantify the psychological symptoms. The MHQ is a brief self-reported questionnaire for the screening of the symptoms of mental disorders in nonpsychiatric settings, which provides scores for free-floating anxiety (MHQ-A), phobic anxiety (MHQ-P), obsessive–compulsive traits and symptoms (MHQ-O), somatization (MHQ-S), depressive symptoms (MHQ-D), and histrionic/hysterical symptoms (MHQ-H).
Longitudinal study
All patients attending the clinic between 2000 and 2007 (n = 1687) were enrolled in a longitudinal study, and for 1685 of these, CDS was available. Their characteristics are summarized in Table 1. Cardiovascular events were identified through the regional hospital discharge system and the City of Florence Registry Office. Information on mortality up to December 31, 2007, including causes of death, was obtained from the City of Florence Registry Office, which contains complete and updated records of all persons living within city boundaries. For those who had moved away, queries were sent to the Registry Office of the new city of residence. Nonfatal cases of MACE requiring hospitalization were identified through the regional hospital discharge system. Following the International Classification of Diseases, fatal and nonfatal MACE were coded as 410–414 (ischemic heart disease), 420–429 (other heart diseases), or 798–799 (sudden death) for cardiac diseases; 430–434 or 436–438 for cerebrovascular disease; and 440 for peripheral arterial disease. The data set of the regional hospital discharge system, which is used for administrative (reimbursement) purposes, contains complete data on all hospital admissions of subjects residing within the borders of the local health district. Compilation in the register of causes of death is completed for any deceased subjects. Therefore, these sources of data allow a complete retrieval of information on all subjects, with no loss at follow-up.
Statistical analyses
Data are reported as mean ± standard deviation (s.d.) when normally distributed and as median (interquartile range) when nonnormally distributed. Linear regressions and ordinal logistic regressions have been used for evaluating the unadjusted and adjusted associations between variables, when the dependent parameter was continuous or categorical, respectively. The results from linear regressions or ordinal logistic regressions were reported as odds ratio (OR) or unstandardized β coefficients, respectively, along with their 95% confidence interval (CI). For graphical purpose, linear associations have been shown using percentiles of the independent variable (deciles or quintile based on the range of the possible values). The results of the linear regression using the independent variable as continuous have been introduced as inset in each panel. For the adjusted comparisons between groups, the multivariate analysis of covariance (ANCOVA) has been used.
RESULTS
Cross-sectional results
In the analytical population, as expected, CDS was significantly associated with aging (β [95% CI] = 1.12 [1.05; 1.19]; P < 0.001); hence, all the following analyses have been adjusted for age. Figure 1 shows, depicted as deciles of the independent variables, the results from the age-adjusted linear regressions for the association between CDS and hormones as well as for other androgen-dependent physical and symptomatic parameters. Independently of age, lower total or cFT was correlated with a higher CDS (Figure 1a and 1b). According to the relationship with T levels, higher CDS is associated with a smaller testicular volume and with higher FSH levels (Figure 1d and 1e).Figure 1c shows a similar association with LH (r = 0.105; P < 0.0001), which, however, did not retain statistical significance after adjusting for age (P = 0.327). In addition, higher CDS was associated with more symptoms of hypogonadism, as detected by a higher ANDROTEST score (Figure 1f). In particular, higher CDS was associated, independently of age, with more severely reduced spontaneous erections (question #6 of ANDROTEST) and with a more frequent occurrence of lack of erections during the intercourse (question #5 of ANDROTEST) (Figure 2a and 2b). Conversely, higher CDS was associated with a less frequent report of hypoactive sexual desire (question #14 of SIEDY) (Figure 2c). Concerning objective measures of erectile function, a higher CDS was associated with more impaired penile blood flows, as assessed by lower flaccid and dynamic peak systolic velocity (PSV) and by lower flaccid acceleration (Figure 2d–2f).
Figure 1.
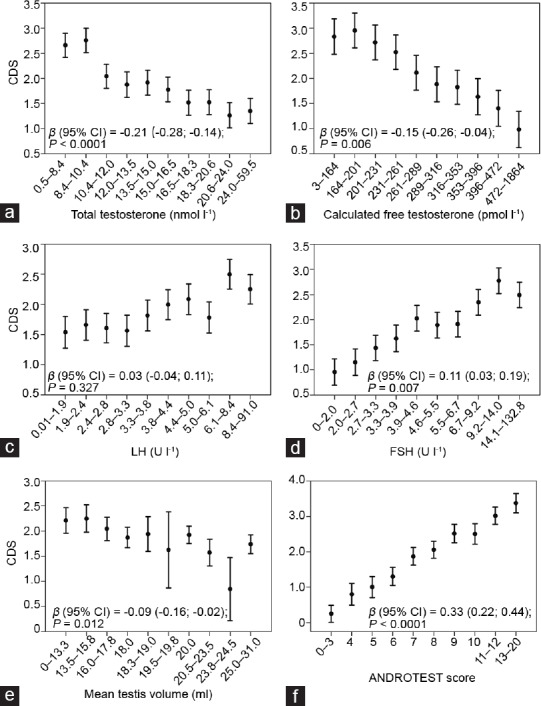
CDS according to hormone levels and clinical features of hypogonadism. Levels of CDS according to (a) total testosterone, (b) calculated free testosterone, gonadotropins ([c] LH and [d] FSH), (e) testis volume, or (f) androgen deficiency symptoms, as assessed by the ANDROTEST score. For a graphical purpose, the data are represented as mean and 95% confidence interval of the dependent variable, according to deciles of the independent variable. Statistics reported in each panel are derived from age-adjusted linear regressions using both the dependent (CDS) and the independent variables as continuous parameters. LH: luteinizing hormone; FSH: follicle-stimulating hormone; CDS: chronic disease score.
Figure 2.
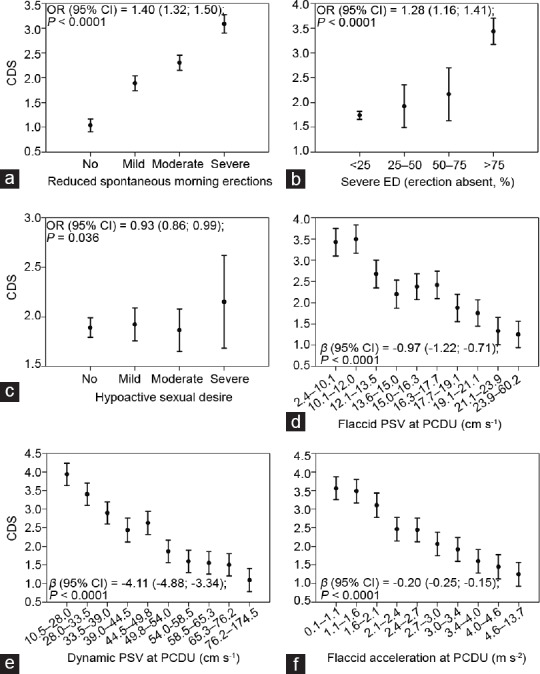
CDS according to sexual symptoms and penile blood flow. Levels of CDS according to the severity of (a) reduction of spontaneous erections, (b) ED, and (c) hypoactive sexual desire and according to the levels of (d) flaccid PSV, (e) dynamic PSV, and (f) flaccid acceleration. For a graphical purpose, the data are represented as mean and 95% confidence interval of the dependent variable, according to deciles of the independent variable. Statistics reported in each panel are derived from age-adjusted (a–c) ordinal regressions or (d–f) linear regressions. CDS: chronic disease score; ED: erectile dysfunction; PSV: peak systolic velocity; PCDU: penile color Doppler ultrasound; OR: odds ratio.
Because hypogonadal symptoms, including the sexual ones, and penile blood flows are known to be affected by T levels, we evaluated the relative weight and mutual effect of CDS and total T on these associations. Table 2 shows the results from age-adjusted ordinal logistic regressions or linear regressions using CDS (increasing levels) and total T (decreasing levels) transformed into Z-values (number of standard deviations from the mean value) in order to make the results comparable. The introduction of total T into the models did not substantially affect the strength of the previously reported associations between CDS and sexual or vascular parameters. However, the relationships between total T and the aforementioned parameters were overall 2–3 folds weaker than those observed with CDS. The only exception was hypoactive sexual desire, which showed a stronger, positive relationship with total T and a weaker, negative association with CDS (Table 2). Similar results were obtained when substituting free for total T (Table 2).
Table 2.
Relationship between chronic disease score and low total or free testosterone with sexual and psychological symptoms and with penile color Doppler parameters
| Symptom | Total patients | Patients with TT and SHBG available | ||
|---|---|---|---|---|
| Effect size (n=3862) | P | Effect size (n=1988) | P | |
| Reduced spontaneous erections, OR (95% CI) | ||||
| CDS score | 1.38 (1.29; 1.48) | <0.0001 | 1.37 (1.25; 1.50) | <0.0001 |
| Total testosterone | 1.13 (1.06; 1.21) | <0.0001 | NI | NI |
| Free testosterone | NI | NI | 1.12 (1.03; 1.23) | 0.020 |
| Severe ED, OR (95% CI) | ||||
| CDS score | 1.25 (1.13; 1.37) | <0.0001 | 1.29 (1.13; 1.46) | <0.0001 |
| Total testosterone | 1.11 (1.00; 1.23) | 0.047 | NI | NI |
| Free testosterone | NI | NI | 1.26 (1.06; 1.48) | 0.007 |
| Hypoactive sexual desire, OR (95% CI) | ||||
| CDS score | 0.91 (0.84; 0.97) | 0.008 | 0.84 (0.77; 0.93) | 0.001 |
| Total testosterone | 1.21 (1.13; 1.30) | <0.0001 | NI | NI |
| Free testosterone | NI | NI | 1.24 (1.12; 1.37) | <0.0001 |
| Flaccid PSV, β (95% CI) | ||||
| CDS score | −0.91 (−1.18; −0.65) | <0.0001 | −0.90 (−1.20; −0.61) | <0.0001 |
| Total testosterone | −0.28 (−0.54; −0.02) | 0.033 | NI | NI |
| Free testosterone | NI | NI | −0.40 (−0.74; −0.05) | 0.024 |
| Dynamic PSV, β (95% CI) | ||||
| CDS score | −3.85 (−4.64; −3.06) | <0.0001 | −4.15 (−5.11; −3.20) | <0.0001 |
| Total testosterone | −1.39 (−2.17; −0.61) | 0.001 | NI | NI |
| Free testosterone | NI | NI | −1.46 (−2.55; −0.36) | 0.009 |
| Flaccid acceleration, β (95% CI) | ||||
| CDS score | −0.19 (−0.25; −0.14) | <0.0001 | −0.21 (−0.27; −0.14) | <0.0001 |
| Total testosterone | −0.07 (−0.13; −0.01) | 0.016 | NI | NI |
| Free testosterone | NI | NI | −0.09 (−0.17; −0.02) | 0.014 |
| Phobic anxiety (MHQ-P), β (95% CI) | ||||
| CDS score | 0.23 (0.12; 0.34) | <0.0001 | 0.08 (−0.05; 0.21) | 0.225 |
| Total testosterone | 0.09 (−0.01; 0.19) | 0.066 | NI | NI |
| Free testosterone | NI | NI | 0.03 (−0.10; 0.16) | 0.674 |
| Obsessive symptoms (MHQ-O), β (95% CI) | ||||
| CDS score | 0.18 (0.02; 0.33) | 0.028 | −0.08 (−0.27; 0.10) | 0.368 |
| Total testosterone | −0.02 (−0.16; 0.12) | 0.797 | NI | NI |
| Free testosterone | NI | NI | −0.12 (−0.30; 0.06) | 0.195 |
| Somatized anxiety (MHQ-S), β (95% CI) | ||||
| CDS score | 0.25 (0.14; 0.37) | <0.0001 | 0.16 (0.01; 0.32) | 0.034 |
| Total testosterone | 0.11 (0; 0.22) | 0.042 | NI | NI |
| Free testosterone | NI | NI | 0.13 (−0.02; 0.28) | 0.099 |
| Depressive symptoms (MHQ-D), β (95% CI) | ||||
| CDS score | 0.12 (−0.02; 0.26) | 0.083 | −0.06 (−0.23; 0.11) | 0.487 |
| Total testosterone | 0.13 (0.01; 0.26) | 0.036 | NI | NI |
| Free testosterone | NI | NI | 0.05 (−0.12; 0.22) | 0.529 |
Data are derived from age-adjusted ordinal logistic regressions or linear regressions using CDS (increasing levels) and total or free testosterone (decreasing levels) transformed into Z values (number of s.d. from the mean value) in order to make the results comparable. TT: total testosterone; SHBG: sex hormone-binding globulin; NI: not introduced in the model as covariate; CDS: chronic disease score; ED: erectile dysfunction; PSV: peak systolic velocity; OR: odds ratio; CI: confidence interval; MHQ: Middlesex Hospital Questionnaire; P: phobic anxiety; O: obsessive symptoms; S: somatization; D: depressive symptoms; s.d.: standard deviations
In order to further analyze the relationship between T, chronic illnesses, and sexual symptoms, we categorized the population according to TT and CDS (using the commonly accepted threshold of 10.4 nmol l−1 and CDS = 0 or ≥1), and we evaluated the scores for sexual symptoms in the resulting four groups. Figure 3a shows that the most severe impairment in morning erections was found in hypogonadic men with chronic conditions, whereas healthy men with low TT, as compared with the eugonadal ones with chronic diseases, had a lower impairment. There were no significant differences in ED between healthy hypogonadal men and unhealthy eugonadal ones (P = 0.356), whereas those hypogonadal with chronic conditions had the worst erectile function, although not achieving the full statistical significance for the comparison with the hypogonadal healthy men (P = 0.150; (Figure 3b). Finally, eugonadal men with chronic diseases had the lowest scoring on hypoactive sexual desire, whereas hypogonadal men with or without chronic diseases reported similar scores (P = 0.334; Figure 3c). Similar findings were derived from the categorization according to CDS and free T above and below the commonly accepted threshold of 225 pmol l−1 (Figure 3d-3f).
Figure 3.
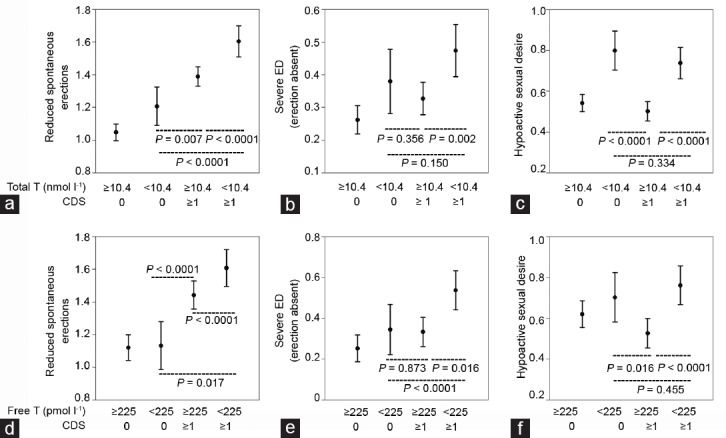
Relationship of sexual symptoms with CDS and testosterone categories. Severity of (a) reduction of spontaneous erections, (b) ED, and (c) hypoactive sexual desire according to categories of CDS (0 or ≥1) and total T (≥10.4 nmol l-1 or <10.4 nmol l-1). Severity of (d) reduction of spontaneous erections, (e) ED, and (f) hypoactive sexual desire according to categories of CDS (0 or ≥1) and free T (≥225 pmol l-1 or <225 pmol l-1). Sexual symptoms were assessed by questions (a) #5 and (b) #6 of ANDROTEST ([a and d] spontaneous morning erection and [b and e] ED) and #14 of SIEDY ([c and f] hypoactive sexual desire) and a higher score denotes a greater severity of the symptom. Data are represented as estimates with 95% confidence interval. Statistics are derived from age-adjusted multivariate analysis of covariance. ED: erectile dysfunction; T: testosterone; CDS: chronic disease score; SIEDY: Structured Interview on Erectile Dysfunction.
In age-adjusted models, a higher CDS was positively associated with several psychological symptoms, including phobic and somatized anxiety, obsessive, and depressive symptoms (Figure 4), whereas no association was found with free-floating anxiety and histrionic traits (data not shown). The aforementioned positive relationships with the exception of depressive symptoms were confirmed after introducing total T in the models as a further covariate. The use of free T instead of TT did not yield any significant result (Table 2).
Figure 4.
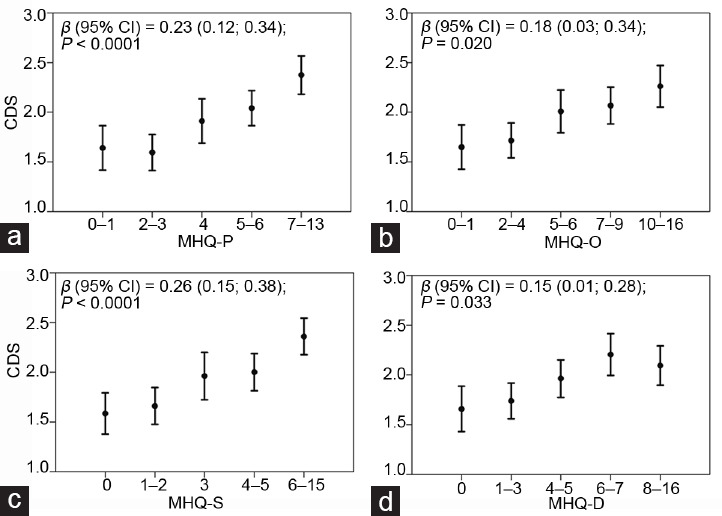
CDS according to psychological symptoms. Levels of CDS according to MHQ score ([a] P: phobic anxiety; [b] O: obsessive symptoms; [c] S: somatization; and [d] D: depressive symptoms). For a graphical purpose, the data are represented as mean and 95% confidence interval of the dependent variable, according to quintiles of the independent variable. Statistics reported in each panel are derived from age-adjusted linear regressions using both the dependent (CDS) and the independent variables as continuous parameters. CDS: chronic disease score; MHQ: Middlesex Hospital Questionnaire.
Longitudinal results
Among men who had follow-up data (n = 1685), during a mean of 4.3 ± 2.6 years, 138 had a MACE, of which 15 were fatal. Of the occurred MACE, 84 were ischemic heart diseases, 40 were cerebral events (stroke or transient ischemic attack), and 14 were peripheral artery diseases.
Figure 5 shows that men with a baseline CDS above 0 (corresponding to the median value of the population) had a higher risk of developing a MACE during follow-up (Figure 5a) and a higher MACE mortality (Figure 5b). The predictive role of CDS toward the incidence of MACE was confirmed after adjusting for severe TD (total T <8 nmol l−1) and age (hazard ratio [HR] [95% CI] = 2.37 [1.56; 3.60]; P < 0.001). Conversely, when considering age and severe TD as covariates, CDS did not retain statistical significance for MACE mortality (HR [95 % CI] = 1.37 [0.41; 4.59]; P = 0.610) whereas severe TD was a significant predictor of MACE mortality (HR [95 % CI] = 5.57 [1.51; 20.63]; P = 0.010) independently of age and CDS.
Figure 5.
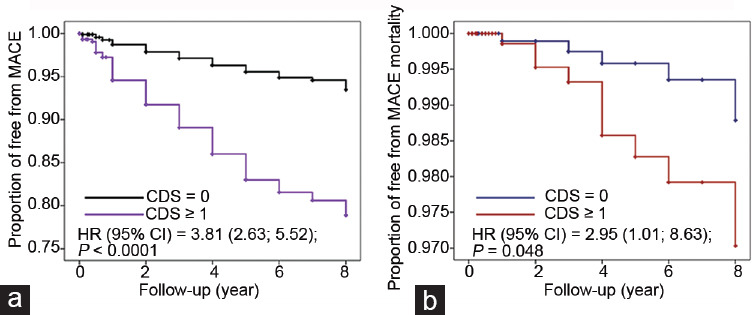
Baseline CDS in relation to incident MACE and MACE mortality. Kaplan–Meier curves for the risk of (a) incident MACE and (b) mortality for MACE according to the median value of CDS. CDS: chronic disease score; MACE: major adverse cardiovascular events; HR: hazard ratio.
DISCUSSION
This study shows that some clinical characteristics of chronic illnesses, as measured by CDS, are associated, independently of aging, with the presence of several sexual and psychological features widely overlapping with the clinical characteristics suggestive for TD. In addition, the comorbidity burden is also related with an impaired gonadal status; indeed, our results show that a condition of primary testicular dysfunction (lower total and free T and high gonadotropins), as well as its related symptoms (higher ANDROTEST score), is often present in subjects scoring higher in CDS.
The association of CDS with low T and with putative TD symptoms arises questions on whether the clinical features associated with an ill-health status are primarily due to a concomitant TD or whether they could be directly attributed to the unhealthy general condition. In order to unravel this point, we evaluated the independence of the association between CDS and the aforementioned symptoms and signs of TD. We therefore conducted a series of multivariate analyses introducing T levels as a possible predictor. The analyses confirmed that both CDS and T are independently associated with sexual symptoms and their psychological burden, although at a different extent. In fact, overall, the comorbidity burden is more strongly related than total T with the investigated parameters.
Sexual symptoms are deemed as the most specifically related to androgen deficiency3,5,6 constituting, besides low serum T levels, one pillar of the diagnostic criteria for LOH.2,4 However, the present results suggest that the weighted effect of CDS versus total T is 2–3 times higher, as denoted by all the PCDU parameters (basal and dynamic peak systolic velocity and acceleration). Even the relative risk of having impaired erection, either spontaneous or sex related, seems to be more affected by high CDS than by low total T. It is well known that erectile function is deeply affected by CV risk factors, which produce, in penile arteries, similar damages than in all the other vascular beds. Considering that, in CDS, a high weight is attributed to heart conditions and CV risk factors (hypertension, diabetes mellitus, dyslipidemia, and hyperuricemia), it is not surprising that scoring higher in CDS is associated with symptoms and signs of arteriogenic ED. Accordingly, we previously showed that dynamic PSV, independently of T, is impaired in obese men.19 Other chronic conditions, such as hypertriglyceridemia,20 impaired fasting glucose or overt diabetes mellitus,17 and hypertension,17 are associated with reduced PCDU parameters. Hence, this tight relationship between ED and cardiometabolic derangements should be taken into account when a man is under evaluation for a putative diagnosis of TD. In fact, a reduced erectile function, either spontaneous or during sexual intercourse, could be due to a metabolically induced vascular damage which dampens its significance as a specific symptom of TD. These considerations are also supported by intervention studies. In fact, all the meta-analyses of the randomized controlled trials (RCTs) on this topic10 consistently show that TTh in TD men is associated with a small, although clinically significant,21 improvement in erectile function, which averages two-three points of IIEF-erectile function domain (EFD).10 However, meta-regression analysis of the same data indicates that, for clinically overt obese subjects (body mass index [BMI] >30) or in the population enriched by diabetic subjects (>75%), the effect of TTh is almost null.10 This is most probably because the metabolic derangements have buried the effect of TD.
Based on the results here presented, it is reasonable to hypothesize that the best therapeutic approach for ED occurring in men with chronic disorders and with TD is to treat not only the TD but also the chronic medical condition by specific treatments or by lifestyle modifications. So far, only few trials compared the combination of lifestyle modifications and TTh with any of the two. In a recent RCT,22 82 obese men with moderately reduced T levels and mild-to-moderate clinical symptoms were treated with a very-low-energy diet. After 46 weeks of weight loss maintenance, they were randomly assigned to intramuscular T undecanoate or placebo. At the end of the 56 weeks of follow-up, TTh yielded a significantly greater improvement in androgen-deficiency symptoms and in erectile function than placebo.22 In a RCT involving 70 sedentary, community dwelling, and elderly men randomized to TTh and/or physical exercise or none of these,23 men receiving the combination therapy for 12 weeks experienced an improvement in quality of life as compared with the inactive arm and the arms with only one of the two treatments. In addition, as shown by a recent meta-analysis, TTh on top of lifestyle demonstrated a significant advantage on metabolic parameters and body composition as compared with lifestyle alone,24 thus suggesting that the two approaches are synergic in producing their benefits.
Reduced sexual desire is one of the three sexual symptoms proposed by the EMAS as the most specific correlates of TD.3 In the present study, the association of hypoactive sexual desire with lower T levels is confirmed. However, in contrast with ED, scoring higher in CDS is not associated with a worse sexual desire but even the reverse. This is even more evident when comparing sexual desire in healthy hypogonadal men with that reported by unhealthy ones with normal or low TT. In fact, hypoactive sexual desire is more severe in hypogonadal groups irrespective of the health status, thus strengthening the concept that sexual desire is dependent on T with limited influence of chronic conditions. This, most probably, because chronic diseases could impair sexual functioning but do not affect sexual motivation, as TD does. This could represent a useful information in the assessment of patients consulting for sexual dysfunction. In fact, when TD is suspected in men with chronic illnesses, the presence of hypoactive sexual desire could be of help to outline an androgen deficiency-related clinical phenotype. Accordingly, in the European general population, the development of secondary hypogonadism, among the sexual symptoms, has the strongest correlation with the decline in sexual desire.5 This is also evident in a population consulting for sexual dysfunction where the difference in total and free T levels between men reporting or not hypoactive sexual desire was largely greater than that found in men with or without ED or impaired morning erections.6
In the present study, among psychological traits, depressive symptoms were the most specific to low T, being associated with it independently of comorbidities. The association between low T and depression has been previously reported in men from either the general population25 or specialty medical settings.26,27 In addition, a recent network meta-analysis, aimed to evaluate several outcomes of TTh, showed an improvement in depression in TTh, as compared with placebo.28 Similarly, a meta-analysis, specifically focusing on the effects of TTh on mood, found an improvement in T-treated men, which was maintained independently of the presence of a chronic condition, such as HIV infection.29 Here, we also found that lower T levels are also associated with more severe somatic symptoms. We previously described this association in a population of men with sexual dysfunction,30 and we showed that patients with more somatic symptoms were characterized by a symptomatic secondary hypogonadism (low T with inappropriately normal LH), independently of lifestyle, BMI, and psychiatric conditions. Here, we confirm this association, which was retained even after the adjustment for CDS. Interestingly, in our previous study,30 despite unhealthier behaviors, we failed to show any associations between somatic symptoms and adverse glycolipid profile, prevalence of diabetes mellitus or metabolic syndrome. In addition, patients with severe somatic symptoms were even characterized by a lower estimated CV risk.30 The apparent inconsistency with the present findings could be explained by the medication-based nature of the CDS. It could be hypothesized that the “mind focused on the body” behavior (which characterizes patients with somatic symptoms) leads them to frequently consult practitioners for recurring physical complaints and that this could result in unnecessary prescriptions and even in self-medications.
Not surprisingly, our longitudinal data show that a heavier comorbidity burden is associated with a greater risk of forthcoming MACE in an age- and T-independent manner. However, when considering the mortality from MACE, the relationship with the baseline burden of comorbidities, as observed at Kaplan–Meier curves, was overwhelmed by the adjustment for severe TD, which appeared as an independent predictor of mortality. These findings are in keeping with several previous reports.31–33 Furthermore, the lack of association between low T and incident MACE was previously reported.31,34–36 Altogether, these observations suggest that low T is not a major risk factor for MACE, but, more likely, it represents a marker of frailty. In fact, the independence of the association between low T and MACE mortality from the comorbidity burden hints that low T could explain a part of frailty, which is not covered by the most common chronic diseases.
The study presents a number of limitations. The data are derived from a cohort of men seeking medical care for sexual dysfunction at a Sexual Medicine Clinic, and they could be different from men in the general population or different specialty settings. Most of the results are obtained from a cross-sectional study, which does not allow inferring a cause–effect relationship for the associations found. In addition, the study relies on structured interviews (SIEDY and ANDROTEST), self-administered questionnaires (MHQ), and a comorbidity measure based on medications used (CDS), which, although validated, present limitations. Hence, the present results should be considered also in light of this and a replication in different clinical or research settings with a longitudinal approach being advocated. In particular, the assessment of sexual and TD-related symptoms is a sensitive issue because any instrument validated so far is limited by relatively low accuracy.2,37 In fact, an objective measurement of symptoms is not feasible and their assessment is based on case-history tools, which are liable to mistakes, although minimized in studies enrolling a large sample, as the present one. Structured interviews, as compared with self-reported questionnaires, have a more limited risk of misinterpretations of questions and replies or mistakes in classifying the answers because a well-trained clinician assists the patient by modulating the language and providing explanations, whenever necessary. Accordingly, a recent review37 has shown that, among several available case-history instruments for the identification of TD, ANDROTEST has the most favorable positive and negative likelihood ratio. In addition, the agreement of the observations on erectile function, as derived from SIEDY, with objective measures derived from PCDU assessment, further reassures on the reliability of our instruments. As a further source of confidence, SIEDY and ANDROTEST have been used in multicenter studies38,39 providing consistent results.
CONCLUSIONS
Chronic illnesses and TD can be considered overlapping conditions, often sharing the same phenotype and hormonal alterations. In fact, an increasing complexity of chronic disease is associated “per se” with TD, and symptoms of TD might be entirely due to a concomitant chronic condition. Among TD clinical features, loss of sexual desire appears as the most genuine hallmark of TD. Particular attention should be paid to ED, because the contribution of chronic morbidities to this complaint, as well as to the impairment in penile blood flows, seems to be stronger than that played by low T. Although the present results need to be replicated in different clinical settings and to be confirmed in studies with a longitudinal design, they should encourage clinicians to cautiously take into account the overlap of TD and chronic conditions when performing the diagnostic workup for hypogonadism.
AUTHOR CONTRIBUTIONS
GR and MM conceived the study, designed the methodology, and performed the analysis; GR and GC collected the data; GR drafted the article; and GR, GC, and MM revised and edited the final article. All authors read and approved the final manuscript.
COMPETING INTERESTS
All authors declared no competing interests.
REFERENCES
- 1.Tajar A, Forti G, O'Neill TW, Lee DM, Silman AJ, et al. Characteristics of secondary, primary, and compensated hypogonadism in aging men: evidence from the European Male Ageing Study. J Clin Endocrinol Metab. 2010;95:1810–8. doi: 10.1210/jc.2009-1796. [DOI] [PubMed] [Google Scholar]
- 2.Wang C, Nieschlag E, Swerdloff R, Behre HM, Hellstrom WJ, et al. Investigation, treatment, and monitoring of late-onset hypogonadism in males: ISA, ISSAM, EAU, EAA, and ASA recommendations. Eur Urol. 2009;55:121–30. doi: 10.1016/j.eururo.2008.08.033. [DOI] [PubMed] [Google Scholar]
- 3.Wu FC, Tajar A, Beynon JM, Pye SR, Silman AJ, et al. Identification of late-onset hypogonadism in middle-aged and elderly men. N Engl J Med. 2010;363:123–35. doi: 10.1056/NEJMoa0911101. [DOI] [PubMed] [Google Scholar]
- 4.Bhasin S, Brito JP, Cunningham GR, Hayes FJ, Hodis HN, et al. Testosterone therapy in men with hypogonadism: an endocrine society clinical practice guideline. J Clin Endocrinol Metab. 2018;103:1715–44. doi: 10.1210/jc.2018-00229. [DOI] [PubMed] [Google Scholar]
- 5.Rastrelli G, Carter EL, Ahern T, Finn JD, Antonio L, et al. Development of and recovery from secondary hypogonadism in aging men: prospective results from the EMAS. J Clin Endocrinol Metab. 2015;100:3172–82. doi: 10.1210/jc.2015-1571. [DOI] [PubMed] [Google Scholar]
- 6.Rastrelli G, Corona G, Tarocchi M, Mannucci E, Maggi M. How to define hypogonadism? Results from a population of men consulting for sexual dysfunction. J Endocrinol Invest. 2016;39:473–84. doi: 10.1007/s40618-015-0425-1. [DOI] [PubMed] [Google Scholar]
- 7.Rastrelli G, O'Neill TW, Ahern T, Bártfai G, Casanueva FF, et al. Symptomatic androgen deficiency develops only when both total and free testosterone decline in obese men who may have incident biochemical secondary hypogonadism: prospective results from the EMAS. Clin Endocrinol (Oxf) 2018;89:459–69. doi: 10.1111/cen.13756. [DOI] [PubMed] [Google Scholar]
- 8.Ahern T, Swiecicka A, Eendebak RJ, Carter EL, Finn JD, et al. Natural history, risk factors and clinical features of primary hypogonadism in ageing men: longitudinal data from the European Male Ageing Study. Clin Endocrinol (Oxf) 2016;85:891–901. doi: 10.1111/cen.13152. [DOI] [PubMed] [Google Scholar]
- 9.Snyder PJ, Bhasin S, Cunningham GR, Matsumoto AM, Stephens-Shields AJ, et al. Lessons from the testosterone trials. Endocr Rev. 2018;39:369–86. doi: 10.1210/er.2017-00234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Corona G, Rastrelli G, Morgentaler A, Sforza A, Mannucci E, et al. Meta-analysis of results of testosterone therapy on sexual function based on international index of erectile function scores. Eur Urol. 2017;72:1000–11. doi: 10.1016/j.eururo.2017.03.032. [DOI] [PubMed] [Google Scholar]
- 11.Von Korff M, Wagner EH, Saunders K. A chronic disease score from automated pharmacy data. J Clin Epidemiol. 1992;45:197–203. doi: 10.1016/0895-4356(92)90016-g. [DOI] [PubMed] [Google Scholar]
- 12.McGregor JC, Kim PW, Perencevich EN, Bradham DD, Furuno JP, et al. Utility of the chronic disease score and Charlson comorbidity index as comorbidity measures for use in epidemiologic studies of antibiotic-resistant organisms. Am J Epidemiol. 2005;161:483–93. doi: 10.1093/aje/kwi068. [DOI] [PubMed] [Google Scholar]
- 13.Wu FC, Tajar A, Pye SR, Silman AJ, Finn JD, et al. Hypothalamic-pituitary-testicular axis disruptions in older men are differentially linked to age and modifiable risk factors: the European Male Aging Study. J Clin Endocrinol Metab. 2008;93:2737–45. doi: 10.1210/jc.2007-1972. [DOI] [PubMed] [Google Scholar]
- 14.Petrone L, Mannucci E, Corona G, Bartolini M, Forti G, et al. Structured interview on erectile dysfunction (SIEDY©): a new, multidimensional instrument for quantification of pathogenetic issues on erectile dysfunction. Int J Impot Res. 2003;15:210–20. doi: 10.1038/sj.ijir.3901006. [DOI] [PubMed] [Google Scholar]
- 15.Corona G, Mannucci E, Petrone L, Balercia G, Fisher AD, et al. ANDROTEST©: a structured interview for the screening of hypogonadism in patients with sexual dysfunction. J Sex Med. 2011;3:706–15. doi: 10.1111/j.1743-6109.2006.00262.x. [DOI] [PubMed] [Google Scholar]
- 16.Vermeulen A, Verdonck L, Kaufman JM. A critical evaluation of simple methods for the estimation of free testosterone in serum. J Clin Endocrinol Metab. 1999;84:3666–72. doi: 10.1210/jcem.84.10.6079. [DOI] [PubMed] [Google Scholar]
- 17.Rastrelli G, Corona G, Lotti F, Aversa A, Bartolini M, et al. Flaccid penile acceleration as a marker of cardiovascular risk in men without classical risk factors. J Sex Med. 2014;11:173–86. doi: 10.1111/jsm.12342. [DOI] [PubMed] [Google Scholar]
- 18.Crown S, Crisp AH. A short clinical diagnostic self-rating scale for psychoneurotic patients The Middlesex Hospital Questionnaire (MHQ) Br J Psychiatry. 1966;112:917–23. doi: 10.1192/bjp.112.490.917. [DOI] [PubMed] [Google Scholar]
- 19.Corona G, Rastrelli G, Filippi S, Vignozzi L, Mannucci E, et al. Erectile dysfunction and central obesity: an Italian perspective. Asian J Androl. 2014;16:581–91. doi: 10.4103/1008-682X.126386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Corona G, Cipriani S, Rastrelli G, Sforza A, Mannucci E, et al. High triglycerides predicts arteriogenic erectile dysfunction and major adverse cardiovascular events in subjects with sexual dysfunction. J Sex Med. 2016;13:1347–58. doi: 10.1016/j.jsxm.2016.07.004. [DOI] [PubMed] [Google Scholar]
- 21.Rosen RC, Allen KR, Ni X, Araujo AB. Minimal clinically important differences in the erectile function domain of the international index of erectile function scale. Eur Urol. 2011;60:1010–6. doi: 10.1016/j.eururo.2011.07.053. [DOI] [PubMed] [Google Scholar]
- 22.Ng Tang Fui M, Hoermann R, Grossmann M. Effect of testosterone treatment on adipokines and gut hormones in obese men on a hypocaloric diet. J Endocr Soc. 2017;1:302–12. doi: 10.1210/js.2017-00062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Katznelson L, Robinson MW, Coyle CL, Lee H, Farrell CE. Effects of modest testosterone supplementation and exercise for 12 weeks on body composition and quality of life in elderly men. Eur J Endocrinol. 2006;155:86775. doi: 10.1530/eje.1.02291. [DOI] [PubMed] [Google Scholar]
- 24.Corona G, Vignozzi L, Sforza A, Mannucci E, Maggi M. Obesity and late-onset hypogonadism. Mol Cell Endocrinol. 2015;418:120–33. doi: 10.1016/j.mce.2015.06.031. [DOI] [PubMed] [Google Scholar]
- 25.Hintikka J, Niskanen L, Koivumaa-Honkanen H, Tolmunen T, Honkalampi K, et al. Hypogonadism, decreased sexual desire, and long-term depression in middle-aged men. J Sex Med. 2009;6:2049–57. doi: 10.1111/j.1743-6109.2009.01299.x. [DOI] [PubMed] [Google Scholar]
- 26.Westley CJ, Amdur RL, Irwig MS. High rates of depression and depressive symptoms among men referred for borderline testosterone levels. J Sex Med. 2015;12:1753–60. doi: 10.1111/jsm.12937. [DOI] [PubMed] [Google Scholar]
- 27.Corona G, Ricca V, Bandini E, Mannucci E, Petrone L, et al. Association between psychiatric symptoms and erectile dysfunction. J Sex Med. 2008;5:458–68. doi: 10.1111/j.1743-6109.2007.00663.x. [DOI] [PubMed] [Google Scholar]
- 28.Elliott J, Kelly SE, Millar AC, Peterson J, Chen L, et al. Testosterone therapy in hypogonadal men: a systematic review and network meta-analysis. BMJ Open. 2017;7:e015284. doi: 10.1136/bmjopen-2016-015284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Amanatkar HR, Chibnall JT, Seo BW, Manepalli JN, Grossberg GT. Impact of exogenous testosterone on mood: a systematic review and meta-analysis of randomized placebo-controlled trials. Ann Clin Psychiatry. 2014;26:19–32. [PubMed] [Google Scholar]
- 30.Fanni E, Castellini G, Corona G, Boddi V, Ricca V, et al. The role of somatic symptoms in sexual medicine: somatization as important contextual factor in male sexual dysfunction. J Sex Med. 2016;13:1395–407. doi: 10.1016/j.jsxm.2016.07.002. [DOI] [PubMed] [Google Scholar]
- 31.Corona G, Rastrelli G, Monami M, Guay A, Buvat J, et al. Hypogonadism as a risk factor for cardiovascular mortality in men: a meta-analytic study. Eur J Endocrinol. 2011;165:687–701. doi: 10.1530/EJE-11-0447. [DOI] [PubMed] [Google Scholar]
- 32.Araujo AB, Dixon JM, Suarez EA, Murad MH, Guey LT, et al. Endogenous testosterone and mortality in men: a systematic review and meta-analysis. J Clin Endocrinol Metab. 2011;96:3007–19. doi: 10.1210/jc.2011-1137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Pye SR, Huhtaniemi IT, Finn JD, Lee DM, O'Neill TW, et al. Late-onset hypogonadism and mortality in aging men. J Clin Endocrinol Metab. 2014;99:1357–66. doi: 10.1210/jc.2013-2052. [DOI] [PubMed] [Google Scholar]
- 34.Contoreggi CS, Blackman MR, Andres R, Muller DC, Lakatta EG, et al. Plasma levels of estradiol, testosterone, and DHEAS do not predict risk of coronary artery disease in men. J Androl. 1990;11:460–70. [PubMed] [Google Scholar]
- 35.Arnlöv J, Pencina MJ, Amin S, Nam BH, Benjamin EJ, et al. Endogenous sex hormones and cardiovascular disease incidence in men. Ann Intern Med. 2006;145:176–84. doi: 10.7326/0003-4819-145-3-200608010-00005. [DOI] [PubMed] [Google Scholar]
- 36.Vikan T, Schirmer H, Njølstad I, Svartberg J. Endogenous sex hormones and the prospective association with cardiovascular disease and mortality in men: the Tromsø study. Eur J Endocrinol. 2009;161:435–42. doi: 10.1530/EJE-09-0284. [DOI] [PubMed] [Google Scholar]
- 37.Millar AC, Lau AN, Tomlinson G, Kraguljac A, Simel DL, et al. Predicting low testosterone in aging men: a systematic review. CMAJ. 2016;188:E321–30. doi: 10.1503/cmaj.150262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Lotti F, Rochira V, Pivonello R, Santi D, Galdiero M, et al. Erectile dysfunction is common among men with acromegaly and is associated with morbidities related to the disease. J Sex Med. 2015;12:1184–93. doi: 10.1111/jsm.12859. [DOI] [PubMed] [Google Scholar]
- 39.Rastrelli G, Giovannini L, Calogero AE, Gianfrilli D, Serra E, et al. Predictors and clinical consequences of starting androgen therapy in men with low testosterone: results from the SIAMO-NOI registry. J Endocrinol Invest. 2016;39:695–708. doi: 10.1007/s40618-016-0461-5. [DOI] [PubMed] [Google Scholar]


