Abstract
Purpose:
All women diagnosed with breast cancer (BC) ≤ age 50 should be referred for genetic counseling (GC) and testing. We sought to compare differences in provider practices and access across a racially and ethnically diverse population of young BC survivors.
Methods:
A registry-based sample of women diagnosed with invasive BC ≤ age 50 from 2009 to 2012 was recruited through the Florida Cancer Registry, and completed a questionnaire and medical record release. Differences were compared across those tested with or without the involvement of a board-certified or credentialed genetics health professional (GHP) in 1) clinical and demographic variables; and 2) pre-test GC elements.
Results:
Of 1622 participants, there were 440 Blacks, 285 Hispanics, and 897 Non-Hispanic Whites. Of 831 participants with medical record verification of testing provider, 170 (20%) had documentation of GHP involvement. Among the 613 who recalled a pre-test discussion and had GC elements collected, those with GHP involvement were significantly more likely to recall the seven recognized GC elements.
Conclusion:
GHP involvement was associated with adherence to nationally recommended best practices. With the expanding importance of identifying inherited cancers, it is critical to ensure equitable access to best practices across all populations.
Keywords: Hereditary breast cancer, Genetic Testing, Genetic Counseling, Genetics Health Professional
Introduction
Breast cancer is the most common cancer among women worldwide, with 2 million new cases diagnosed in 2018.1 Hereditary breast cancer (HBC) accounts for approximately 5–10% of all breast cancer cases, most commonly due to pathogenic/likely pathogenic (P/LP) variants in the BRCA1 and BRCA2 (BRCA) genes.2 Female BRCA carriers have a 60–70% lifetime risk of developing breast cancer compared to 12% in the general population,2 and up to a 50% or greater risk of developing a second primary breast cancer.3–7 Evidence-based interventions such as risk-reducing surgery and breast cancer screening exist for cancer prevention and early diagnosis among BRCA carriers.8–10 Moreover, in addition to the personal impact of identifying HBC, this information may be shared with at-risk family members to amplify the benefits of testing and subsequent care among those at high risk.
National practice guidelines, developed and updated at least annually through the National Comprehensive Cancer Network (NCCN), recommend identification and referral for genetic counseling (GC) and consideration of testing of all women diagnosed with breast cancer at or below age 50.11 These practice guidelines also set forth recommendations for content and elements that should be discussed during the pre-test GC session which may be directed by a board-certified or credentialed genetics health professional (GHP) or a health professional without formal certification in genetics (non-GHP). The NCCN guidelines are aligned with pre-test GC discussion elements set forth by the National Society of Genetic Counselors (NSGC) and the American Society of Clinical Oncology (ASCO).11–13
The national shortage of GHPs14 coupled with particularly limited access in rural areas,15,16 certain states,17 and community oncology practices,18 has resulted in most testing in the United States being performed without the inclusion of a GHP.19–21 Further challenges may include lack of referral to genetic counseling services, either in person or through telehealth, among providers with limited proficiency in genetics, as well as reimbursement challenges with the Center for Medicare and Medicaid (CMS) not currently recognizing genetic counselors as billing providers. Consequently, there is great variability in adherence to pre-test GC practices as defined by national practice guidelines. Adding to the logistical complexities of testing and in the face of GHP shortages, there are policies that mandate pre-test GC be conducted with involvement of a GHP which may disproportionately reduce testing rates among minority and underserved populations.22,23 To our knowledge, no prior population-based efforts have evaluated delivery of hereditary cancer services based on patient-reported GC elements covered by the ordering provider across a diverse population of young breast cancer survivors. Through the proposed study, we sought to compare a population-based sample of young Black, Hispanic, and Non-Hispanic White (NHW) female breast cancer survivors for differences across those tested with or without GHP involvement in: 1) clinical and demographic variables and; 2) content of pre-test GC discussion.
Methods
Eligible patients were women diagnosed with invasive breast cancer ≤ age 50 between 2009–2012, living within Florida at the time of diagnosis, and alive at the time of recruitment. Information was obtained on all eligible participants from the Florida Cancer Registry (FCR) after obtaining approval from the Institutional Review Boards at the University of South Florida and the Florida Department of Health, as previously described.24
Participants were recruited using previously described state-mandated recruitment methods,25,26 which consisted of two separate mailings sent at least three weeks apart, which included a “telephone response card” to give potential participants the option to either express interest in participation with follow-up by a study team member or decline to participate (i.e., indicate they did not wish to be contacted by phone or future mailings).27 If no response was received within three weeks of the second mailing, a member of the study team attempted to contact the potential participant by telephone to explain the study and determine interest in participation. For those willing to participate, informed consent was secured, and a baseline study questionnaire was requested.
Age at diagnosis, racial/ethnic group, and primary insurance payer at diagnosis on all potential participants were obtained from the FCR. Participants were categorized through self-reported race/ethnicity into Black, Hispanic, and NHW groups. Additional information obtained through the baseline questionnaire included college education, income, insurance status, marital status, and family history of breast and ovarian cancer.
The FCR provided the stage at diagnosis, histologic subtype, and tumor receptor status on all participants. Participants were asked to complete an authorization for release of medical records for verification of clinical information and genetic testing. Participants were further categorized into groups based on those who received GC and/or testing by a GHP. GHPs were defined as genetic counselors or medical geneticists and non-GHPs were defined as any other healthcare provider, which included physicians, physician assistants, nurse practitioners or nurses. Women who recalled having pre-test GC were then asked a multi-part question about whether they recalled seven pre-test GC elements recommended per national guidelines,11–13 as listed in Table 2.
Table 2:
Patient recall of nationally-recommended genetic counseling elements by provider type
| Genetics Health Professional N = 144 | Non-Genetics Health Professional N = 469 | ||||
|---|---|---|---|---|---|
| n | % | n | % | ||
| Test results (positive, negative, inconclusive) | 125 | 87% | 347 | 74% | 0.001 |
| Laws against health insurance discrimination | 69 | 48% | 108 | 23% | <0.001 |
| Issues related to life and disability insurance | 46 | 32% | 60 | 13% | <0.001 |
| Management recommendations | 72 | 50% | 191 | 41% | 0.04 |
| Other hereditary cancers | 65 | 45% | 136 | 29% | <0.001 |
| Family implications | 123 | 85% | 365 | 78% | 0.04 |
| Pedigree completed | 124 | 86% | 225 | 48% | <0.001 |
| Summary letter received | 89 | 62% | 122 | 26% | <0.001 |
Two-sided Chi-square test was used to calculate the p-values
Clinical and demographic variables for all eligible participants were summarized by involvement of GHP using descriptive statistics. Using multiple logistic regression, we assessed if the following variables were associated with GHP involvement: 1) socioeconomic status (i.e., income, college education, and private insurance); 2) racial/ethnic group (Black, Hispanic, and NHW); and 3) clinical factors (i.e., age at diagnosis and family history of breast or ovarian cancer).
Women tested through a GHP were compared using Pearson chi-squared tests to those tested through a non-GHP based on: 1) recall of pre-test discussion; and 2) seven pre-test GC elements controlling the familywise type 1 error using an alpha of 0.05 and Holm step-down procedure. We also used a two-tailed, independent samples T-test to evaluate if there was a statistically significant difference in the sum of elements recalled between the GHP and non-GHP groups.
Results
There were a total of 1622 participants, including 440 Blacks, 285 Hispanics, and 897 NHW (Figure 1). Of these, four participants were excluded as GC and/or testing information was missing. Of the remaining 1618 study participants, 831 had genetic testing and provider information verified. GHP involvement (either through consultation and/or test ordering) was reported in 170 women (20%) whereas the remaining 661 women (80%) had no documentation of GHP involvement.
Figure 1:
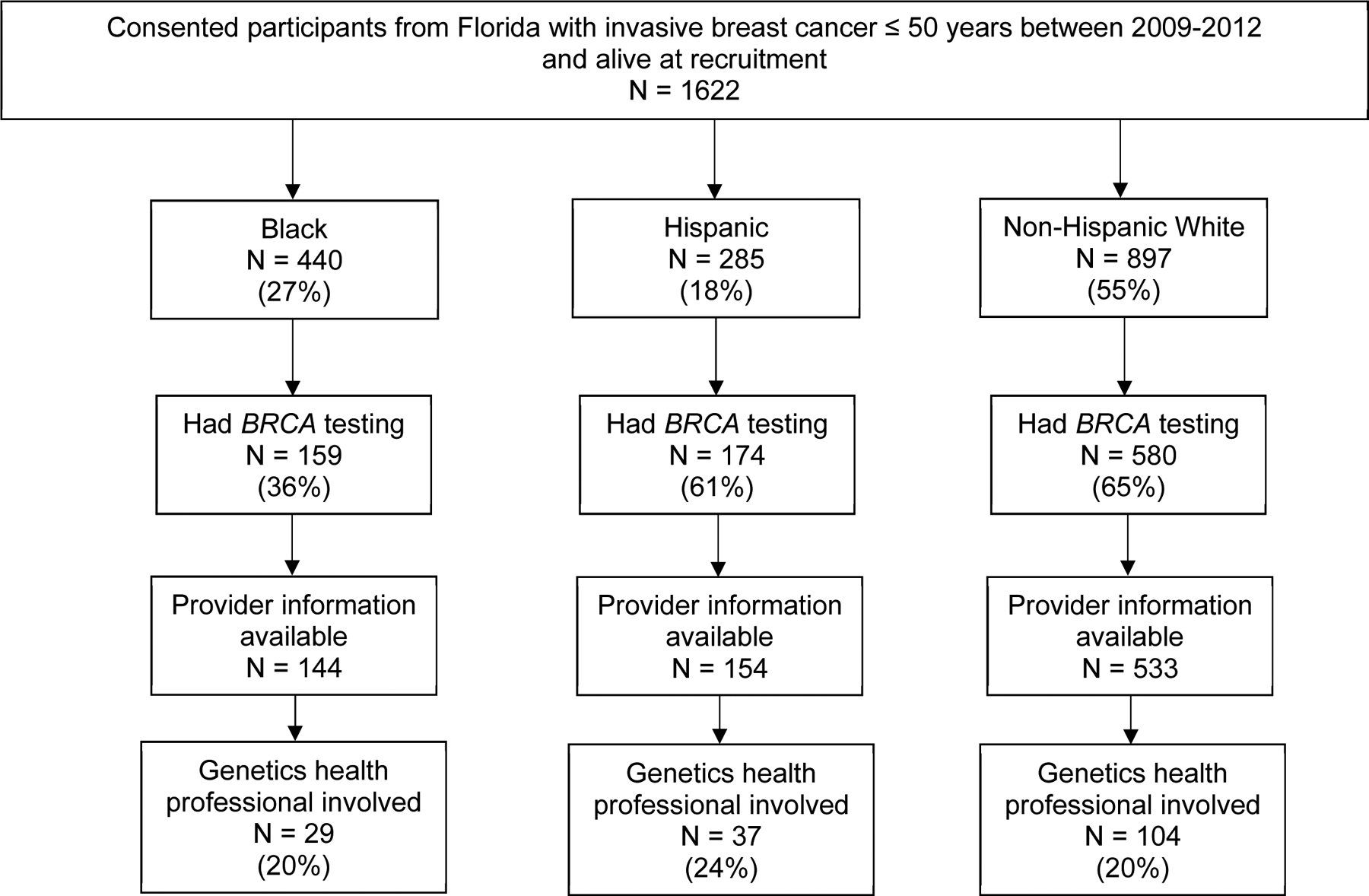
Recruitment from the Florida Cancer Registry
Of the participants that had genetic testing, there was no significant differences in GHP involvement based on participant age at diagnosis, family history of breast or ovarian cancer, college education and annual household income ≥ $50,000. Compared to NHW, Blacks and Hispanics had similar rates of GHP involvement. Based on the results of the multiple logistic regression model, private insurance was the only variable inversely associated with GHP involvement (OR = 0.60, 95% CI: 0.39–0.93, p=0.02) (Table 1).
Table 1:
Results of multiple logistic regression showing associations with Genetics Health Professional Involvement
| Genetics Health Professional N=170 | Non-Genetics Health Professional N=661 | ||||||
|---|---|---|---|---|---|---|---|
| n | % | n | % | ||||
| Non-Hispanic White a | 104 | 61% | 429 | 65% | |||
| Black | 29 | 17% | 115 | 17% | 1.05 | 0.64–1.70 | 0.85 |
| Hispanic | 37 | 22% | 117 | 18% | 1.22 | 0.80–1.85 | 0.36 |
| Age at diagnosis < 45 | 108 | 64% | 417 | 63% | 0.99 | 0.70–1.40 | 0.97 |
| Family History of Breast Cancer | 108 | 64% | 390 | 59% | 1.23 | 0.87–1.73 | 0.24 |
| Family History of Ovarian Cancer | 27 | 16% | 93 | 14% | 1.14 | 0.70–1.83 | 0.60 |
| Private Insurance | 123 | 72% | 531 | 80% | 0.60 | 0.39–0.93 | 0.02 |
| College Education | 95 | 56% | 411 | 62% | 0.86 | 0.61–1.22 | 0.40 |
| Annual household income ≥ $50,000 | 133 | 78% | 566 | 86% | 0.88 | 0.60–1.28 | 0.49 |
Non-Hispanic White is the reference group
Among tested participants with GHP involvement, 84.7% recalled having a pre-test discussion compared to 71.3% without GHP involvement (p<0.001). Among the subset of 613 participants who recalled a pre-test discussion and had GC elements collected, those with GHP involvement were more likely to recall specific GC elements and these differences were statistically significant for all elements analyzed, including the seven endorsed by ASCO (Table 2). In addition, the mean number of items recalled when a GHP was involved was 4.80 compared to 3.06 when a GHP was not involved. The mean difference between the GHP and non-GHP groups was statistically significant (1.74 [95% CI: 1.38 – 2.09]).
Discussion
To our knowledge, this is amongst the first population-based studies to evaluate the impact of GHP involvement in the delivery and quality of pre-test hereditary cancer GC and testing services across a racially and ethnically diverse population of young breast cancer survivors. Our results indicate that 20% of young breast cancer survivors are tested through a GHP. Furthermore, women with private insurance were less likely to receive care through a GHP after controlling for other clinical and socioeconomic variables. Finally, GHPs were more likely to conduct pre-test GC and cover more pre-test GC discussion elements based on national practice guidelines, compared to other providers without certification in genetics.
In our study, only 20% of women had genetic testing services provided by a GHP. Although survey data on patients tested for HBC by ordering provider is limited, a prior study surveyed 666 patients with early-stage breast cancer on the type of healthcare provider that ordered the genetic test (surgeon, medical oncologist, primary care provider, genetic counselor, or other).28 Similar to our findings, approximately 21% of patients who received genetic testing reported that a genetic counselor ordered their genetic test.28 Demand and indications for testing have continued to rise and outpace the supply of GHPs.14,17,18 Consequently, it has become critical to develop strategies to promote best practices for delivering GC and testing services, improve proficiency in genetics, and promote partnerships to improve overall gene-based care provided to patients among non-GHPs to address several unmet needs.29
Our study is the first to evaluate the impact of socioeconomic and clinical factors on GHP involvement in a patient’s care. Prior studies to evaluate the impact of sociodemographic factors (e.g. race, age, education and insurance status) on the receipt of GC suggest that Black women are less likely to receive GC than White women.30–32 It is well established that insured populations with higher SES-related indicators are over-represented among populations who utilize GC and testing for hereditary cancer through a GHP.27,33 Furthermore, prior studies have reported that women with higher SES indicators are more likely to receive care through a GHP compared to women with public or no insurance.33,34 Yet women with private insurance in our study, were more likely to receive care without the involvement of a GHP. This is surprising given hereditary cancer GC and testing through a GHP is a covered service among most private insurers, with some insurers making this a requirement in order for testing to be covered.35 It is possible that some providers refer patients to a GHP in instances where coverage may be a challenge, given that GHPs may be more familiar with coverage options for some of these patients, particularly among underinsured or uninsured populations.
In our racially, ethnically, and socioeconomically diverse population, our findings suggest that GHPs (compared to non-GHPs) were more likely to conduct pre-test GC (86.5% versus 75.7%; p<0.001) and cover more pre-test GC discussion elements based on national practice guidelines (4.80 versus 3.06, (1.74 [95% CI: 1.38 – 2.09])). These findings are consistent with our prior study comparing pre-test discussion of standard pre-test GC elements among a primarily NHW sample of insured patients who received BRCA testing across diverse providers and settings.24 Results from this prior study indicated that GHP involvement was associated with conduct of pre-test GC, as well as with higher adherence to discussion of specific nationally-recommended pre-test GC elements. Pre-test GC through a GHP has also been associated with increased recall about the implications of testing and the laws in place to prohibit insurance companies from denying coverage on the basis of the genetic test result.36 Consequently, with expansion of gene-based care for those at risk for inherited cancer, these gaps highlight the need to standardize the delivery of pre-test GC to improve care across diverse populations and healthcare settings.
The current study has several strengths including being the first registry-based study to systematically compare associations between socioeconomic and clinical factors and access to GHP among an ethnically and racially diverse sample of young breast cancer survivors treated across multiple healthcare settings, enhancing the generalizability of our findings. Furthermore, our estimates of provider discussion and genetic testing across diverse populations provides updated and novel data, compared to prior efforts with more limited minority representation32,36,37 or older cohorts.31,38 Despite these strengths, there remain some limitations, including that although participants were diagnosed within the same four years and eligibility criteria were the same, the Blacks and non-Blacks were recruited under separate protocols, which could contribute to recall bias across populations. However, systemic verification of all available medical records was conducted to confirm self-reported baseline questionnaire data and minimize the impact of recall bias. It is also possible that our definition of a GHP, limited to healthcare providers board-certified in genetics, may have led to underestimating the magnitude of the differences between those healthcare providers without expertise or additional training in genetics. This is because there are many other healthcare providers without board certification in genetics who have robust expertise in this content area.
With the tremendous advances in genetic testing for use across the cancer prevention and control continuum, including importance in guiding personalized treatments,39 we expect the demand for testing to continue to rise rapidly. These factors highlight the need to develop strategies that promote robust partnerships across GHPs and non-GHPs while also supporting educational efforts to improve overall proficiency in genetics across the entire healthcare workforce. This is absolutely essential to improve the provision of guideline-adherent GC services for hereditary cancer predisposition across populations, and broadly promote identification of high-risk populations and GC, as recently highlighted by the United States Preventive Services Task Force (USPTSF).40 Given that most hereditary cancer GC and testing is provided by those without formal certification or training in genetics, promoting strategies for them to partner with GHPs to assist them in providing guideline-adherent service is critical.29 Standardizing the quality of genetic services provided to all racial and ethnic groups is paramount with the expanding importance of gene-based care.
In summary, this is the first population-based study across a racially and ethnically diverse population to demonstrate that GHPs were more likely to discuss GC elements, as recommended per national practice guidelines, which have potential legal, psychosocial and cultural implications. Our findings also suggest that women with private insurance were less likely to be tested through a GHP which is considered the gold standard and is a covered service by most private insurers. Taken together, the key differences among those in whom testing was conducted with and without the involvement of a GHP can be used to identify important implementation strategies to enhance guideline-adherent care when conducting genetic testing for HBC across diverse populations and settings.
Acknowledgements
This work was supported by grants through the Bankhead Coley Granting agency (4BB15 and IBG10-34199), the National Cancer Institute (R01 CA204819), and in part by the Ingram Professorship, and the Kleberg Foundation, and Vanderbilt Genetic Institute departmental funds (TP). Support for Sonya Reid’s time was provided by a NCI T32 training grant awarded to Vanderbilt University (T32 CA160056).
References
- 1.Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA: a cancer journal for clinicians. 2018;68(6):394–424. [DOI] [PubMed] [Google Scholar]
- 2.Felix GES, Zheng Y, Olopade OI. Mutations in context: implications of BRCA testing in diverse populations. Familial cancer. 2018;17(4):471–483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Yedjou CG, Sims JN, Miele L, et al. Health and Racial Disparity in Breast Cancer In: Ahmad A, ed. Breast Cancer Metastasis and Drug Resistance: Challenges and Progress. Cham: Springer International Publishing; 2019:31–49. [Google Scholar]
- 4.Metcalfe K, Gershman S, Lynch HT, et al. Predictors of contralateral breast cancer in BRCA1 and BRCA2 mutation carriers. Br J Cancer. 2011;104(9):1384–1392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Pierce LJ, Phillips K-A, Griffith KA, et al. Local therapy in BRCA1 and BRCA2 mutation carriers with operable breast cancer: comparison of breast conservation and mastectomy. Breast cancer research and treatment. 2010;121(2):389–398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Menes TS, Terry MB, Goldgar D, et al. Second primary breast cancer in BRCA1 and BRCA2 mutation carriers: 10-year cumulative incidence in the Breast Cancer Family Registry. Breast cancer research and treatment. 2015;151(3):653–660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Malone KE, Begg CB, Haile RW, et al. Population-based study of the risk of second primary contralateral breast cancer associated with carrying a mutation in BRCA1 or BRCA2. Journal of clinical oncology : official journal of the American Society of Clinical Oncology. 2010;28(14):2404–2410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Salhab M, Bismohun S, Mokbel K. Risk-reducing strategies for women carrying BRCA1/2 mutations with a focus on prophylactic surgery. BMC Womens Health. 2010;10:28–28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Warner E. Screening BRCA1 and BRCA2 Mutation Carriers for Breast Cancer. Cancers (Basel). 2018;10(12):477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Carbine NE, Lostumbo L, Wallace J, Ko H. Risk-reducing mastectomy for the prevention of primary breast cancer. Cochrane Database Syst Rev. 2018;4(4):CD002748–CD002748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Network. NCC. Genetic/Familial High-Risk Assessment: Breast, Ovarian and Pancreatic. (Version1.2020). [Accessed December 5, 2019]. Available from: https://www-nccn-org.proxy.library.vanderbilt.edu/. 2019.
- 12.Riley BD, Culver JO, Skrzynia C, et al. Essential Elements of Genetic Cancer Risk Assessment, Counseling, and Testing: Updated Recommendations of the National Society of Genetic Counselors. J Genet Couns. 2012;21(2):151–161. [DOI] [PubMed] [Google Scholar]
- 13.Robson ME, Bradbury AR, Arun B, et al. American Society of Clinical Oncology Policy Statement Update: Genetic and Genomic Testing for Cancer Susceptibility. Journal of clinical oncology : official journal of the American Society of Clinical Oncology. 2015;33(31):3660–3667. [DOI] [PubMed] [Google Scholar]
- 14.Penon-Portmann M, Chang J, Cheng M, Shieh JT. Genetics workforce: distribution of genetics services and challenges to health care in California. Genetics in Medicine. 2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bookman T. More People Seek Genetic Testing, But There Aren’t Enough Counselors. Shots: Health News from NPR Web site. http://www.npr.org/sections/health-shots/2016/04/18/473066953/more-people-seek-genetic-testing-but-there-arent-enough-counselors. Published 2016. Accessed Oct 11, 2016.
- 16.Occupational Employment Statistics: Occupational Employment and Wages, May 2015: 29–902 Genetic Counselors. In: Bureau of Labor Statistics; 2016. [Google Scholar]
- 17.Villegas C, Haga SB. Access to Genetic Counselors in the Southern United States. J Pers Med. 2019;9(3). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hoskovec JM, Bennett RL, Carey ME, et al. Projecting the Supply and Demand for Certified Genetic Counselors: a Workforce Study. J Genet Couns. 2018;27(1):16–20. [DOI] [PubMed] [Google Scholar]
- 19.Acheson LS, Stange KC, Zyzanski S. Clinical genetics issues encountered by family physicians. Genetics in medicine : official journal of the American College of Medical Genetics. 2005;7(7):501–508. [DOI] [PubMed] [Google Scholar]
- 20.Vig HS, Armstrong J, Egleston BL, et al. Cancer genetic risk assessment and referral patterns in primary care. Genetic testing and molecular biomarkers. 2009;13(6):735–741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Radford C, Prince A, Lewis K, Pal T. Factors which impact the delivery of genetic risk assessment services focused on inherited cancer genomics: expanding the role and reach of certified genetics professionals. Journal of genetic counseling. 2014;23(4):522–530. [DOI] [PubMed] [Google Scholar]
- 22.Whitworth P, Beitsch P, Arnell C, et al. Impact of Payer Constraints on Access to Genetic Testing. Journal of oncology practice. 2017;13(1):e47–e56. [DOI] [PubMed] [Google Scholar]
- 23.Stenehjem DD, Au T, Sainski AM, et al. Impact of a genetic counseling requirement prior to genetic testing. BMC health services research. 2018;18(1):165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Cragun D, Camperlengo L, Robinson E, et al. Differences in BRCA counseling and testing practices based on ordering provider type. Genet Med. 2015;17(1):51–57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Pal T, Rocchio E, Garcia A, Rivers D, Vadaparampil S. Recruitment of Black Women for a Study of Inherited Breast Cancer Using a Cancer Registry–Based Approach. Genetic Testing and Molecular Biomarkers. 2010;15(1–2):69–77. [DOI] [PubMed] [Google Scholar]
- 26.Bonner D, Pal T, Tallo C, Vadaparampil ST. Abstract A33: The utility of a state-wide cancer registry in recruiting a clinically representative population-based sample of young black women diagnosed with early-onset breast cancer. Cancer Epidemiology Biomarkers & Prevention. 2012;21(10 Supplement):A33–A33. [Google Scholar]
- 27.Cragun D, Weidner A, Lewis C, et al. Racial disparities in BRCA testing and cancer risk management across a population-based sample of young breast cancer survivors. Cancer. 2017;123(13):2497–2505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Kurian AW, Li Y, Hamilton AS, et al. Gaps in Incorporating Germline Genetic Testing Into Treatment Decision-Making for Early-Stage Breast Cancer. Journal of Clinical Oncology. 2017;35(20):2232–2239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Pal T, Radford C, Weidner A, Tezak AL, Cragun D, Wiesner GL. The Inherited Cancer Registry (ICARE) Initiative: An Academic-Community Partnership for Patients and Providers. Oncology Issues. 2018;33(6):54–63. [Google Scholar]
- 30.Bellcross CA, Leadbetter S, Alford SH, Peipins LA. Prevalence and healthcare actions of women in a large health system with a family history meeting the 2005 USPSTF recommendation for BRCA genetic counseling referral. Cancer epidemiology, biomarkers & prevention : a publication of the American Association for Cancer Research, cosponsored by the American Society of Preventive Oncology. 2013;22(4):728–735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Hall M, Olopade OI. Confronting Genetic Testing DisparitiesKnowledge Is Power. Jama. 2005;293(14):1783–1785. [DOI] [PubMed] [Google Scholar]
- 32.Levy DE, Byfield SD, Comstock CB, et al. Underutilization of BRCA1/2 testing to guide breast cancer treatment: Black and Hispanic women particularly at risk. Genetics in Medicine. 2011;13(4):349–355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Katz SJ, Ward KC, Hamilton AS, et al. Gaps in Receipt of Clinically Indicated Genetic Counseling After Diagnosis of Breast Cancer. Journal of clinical oncology : official journal of the American Society of Clinical Oncology. 2018;36(12):1218–1224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Hull LE, Haas JS, Simon SR. Provider Discussions of Genetic Tests With U.S. Women at Risk for a BRCA Mutation. American Journal of Preventive Medicine. 2018;54(2):221–228. [DOI] [PubMed] [Google Scholar]
- 35.2016 C. Genetic Testing and Counseling Resources. https://wwwcignacom/health-care-providers/resources/genetic-testing-and-counseling-program.
- 36.Scott D, Friedman S, Telli ML, Kurian AW. Decision Making About Genetic Testing Among Women With a Personal and Family History of Breast Cancer. Journal of Oncology Practice. 2019:JOP.19.00221. [DOI] [PubMed] [Google Scholar]
- 37.Barcenas CH, Shafaee MN, Sinha AK, et al. Genetic Counseling Referral Rates in Long-Term Survivors of Triple-Negative Breast Cancer. J Natl Compr Canc Netw. 2018;16(5):518–524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Armstrong K, Micco E, Carney A, Stopfer J, Putt M. Racial differences in the use of BRCA1/2 testing among women with a family history of breast or ovarian cancer. Jama. 2005;293(14):1729–1736. [DOI] [PubMed] [Google Scholar]
- 39.Robson M, Im S-A, Senkus E, et al. Olaparib for Metastatic Breast Cancer in Patients with a Germline BRCA Mutation. New England Journal of Medicine. 2017;377(6):523–533. [DOI] [PubMed] [Google Scholar]
- 40.Force UPST. Risk Assessment, Genetic Counseling, and Genetic Testing for BRCA-Related Cancer: US Preventive Services Task Force Recommendation Statement. Jama. 2019;322(7):652–665. [DOI] [PubMed] [Google Scholar]


