Abstract
Objective
Despite huge global, national, and local preventive measures including travel restriction, social distancing, and quarantines, the outbreak of novel severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) develops the coronavirus disease 2019 (COVID-19) worldwide pandemic. SARS-CoV-2 emerging from Wuhan, China, took only three months to cover >200 countries worldwide by infecting more than 2.4 million people and killing more than 150,000 people. Although this infection at the early stage creates seasonal flu-like symptoms with a higher illness, it eventually causes a higher mortality. Epidemiological studies not only find the causes of many health issues but also suggest preventive measures. This study aimed to see the link between environment temperature and COVID-19 cases.
Study design
The monthly average environment temperature (MAET) and various COVID-19 cases of a country were collected and analyzed to see the relationship between these parameters.
Methods
Univariate analysis and statistical modeling were used to determine the relationship between environment temperature and different COVID-19 cases.
Results
This study found that the majorities of the countries having higher COVID-19 cases are located in the higher latitude (colder region) in the globe. As of 20th April data available, statistical analyses by various methods have found that strong negative correlations with statistical significance exist between MAET and several COVID-19 cases including total cases, active cases, and cases per million of a country (Spearman correlation coefficients were −0.45, −0.42, and −0.50 for total cases, active cases, and cases/per million, respectively). Analysis by the statistical log-linear regression model further supports that the chance of patients to contract COVID-19 is less in warmer countries than in colder countries.
Conclusion
This pilot study proposes that cold environment may be an additional risk factor for COVID-19 cases.
Keywords: COVID-19, Coronavirus, SARS-CoV-2, Temperature, Cold environment
Highlights
-
•
Majority countries having higher COVID-19 cases situated in higher latitude/cold region.
-
•
Negative relationship exists between environment temperature and COVID-19 cases.
-
•
The chance of COVID-19 cases in warmer countries is fewer than in colder countries.
-
•
Cold environment may be an additional risk factor for SARS-CoV-2 infection.
Introduction
Within three months from emerging of the novel coronavirus at Wuhan city, China, in December 2019, this pandemic outbreak has spread largely across the world. On February 12, the World Health Organization has named the disease caused by novel coronavirus as coronavirus disease 2019 (COVID-19). Virologists have named this virus as severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). The results of genome sequencing obtained from the infected patients revealed that this novel virus belongs to coronavirus clusters and is closely related to other bat-derived coronaviruses, bat-SL-CoVZC45 and bat-SL-CoVZXC21, but this new coronavirus is somewhat related to SARS-CoV and MERS-CoV.1 However, the origin of this virus is yet to be confirmed. In this stage, it may not be concluded that this virus has originated from animals (such as bats) or a chimeric virus.2 , 3 It might be the case that bat coronaviruses after specific mutations can gain the ability to affect human beings.3 A few recent studies have found that COVID-19 can develop faster in old age individuals, but the infection rate may or may not vary with age, gender, ethnicities, and races.4 , 5 In general, this novel coronavirus infection develops symptoms such as those of seasonal flu including fever, cough, expectoration, myalgia, sore throat, and fatigue, but the severity of the illness could be more than that of influenza. Some patients may develop shortness of breath, pneumonia, severe acute respiratory distress syndromes, and multiorgan failure.4 , 6 Accumulating evidence indicated that people having various diseases such as diabetes, hypertension, and cardiovascular diseases experience serious complication if they are infected with the SARS-CoV-2. The outbreak of the SARS-CoV-2 pandemic might be even more fatal than the most devastating influenza (Spanish flu) pandemic outbreak in 1918 that occurred a century ago because almost 2.4 million COVID-19 confirmed cases with more than 150,000 deaths have been reported from 200 countries within only three months of the evolving of this viral infection. Because seasonal flu is comparatively low in the summer as compared with winter, the general population along with various researchers think that the summer might drop the novel coronavirus infection rate.
Thus, this present study was aimed to see the link between temperature and COVID-19 cases. The results from our statistical analysis suggested that a negative relationship exists between various COVID-19 cases including total confirmed cases, active cases, and cases per million of the countries with the monthly average environmental temperature. This study suggests that a cold environment might be an additional risk factor for COVID-19 cases.
Methods
Data collection
The data of COVID-19 cases for each country were collected throughout time from 25th March to 18th April, 2020, from the website worldometers.info. The values of various COVID-19 cases were highly dynamic and changed rapidly in every day. Thus, in this study, we had analyzed separately the data of different dates, collected every six days intervals (25th March, 30th March, 6th April, 12th April, and 18th April, 2020) to see the consistency of the statistical results. In this study, we had included total cases and active cases because values of these two variables were there for all the countries throughout the study period and are gradually increased by the changed values of every day. The absolute values of total and active cases may depend on population density. Thus, we have also considered population adjusted data, that is, cases/million. Monthly average environment temperature (MAET) was obtained by making the average of average highest and lowest temperature of a specific month of the capital of a country, collected from the website climatestotravel.com.
Geographic location of countries
The locations of various countries were pointed in a world map by using world map maker ArcGIS software described previously.7 The top countries having at least 1000 coronavirus infection cases were marked in the world map.
Statistical methods
Univariate analysis
The Spearman and Kendall methods for univariate analysis were used to test the null hypothesis between two variables described previously.8 , 9 These methods provide the coefficient of correlation for observations which are not in linear relationship (mentioned as coefficient in tables). Both negative and positive correlations were denoted by negative and positive coefficients. Here, significant differences were considered for P < 0.05. In this statistical analysis, we had included all data available in the website worldometers.info.
Statistical modeling
In this study, we have considered three response variables as follows: (i) cases per million, (ii) total cases, and (iii) active cases. By simple graphs, it can be seen that there does not exist any linear relationship between temperature and COVID-19 considered variables. Therefore, we purpose a log-linear model to fit the COVID-19 case data with temperature. A log-linear model can be defined by the following equation:
where and are the parameters of the model and n denotes the number of countries considered under study. The parameter gives the intercept on y-axis. The parameter is of more interest and can be interpreted as the t-unit increment in X is to multiply the expected value of Y by .
In this model, x i is an independent variable denoting the average temperature of a month of the ith country, whereas the response variable Y ij denotes the value of jth case for the ith country at the considered day. Here, j will be 1, 2, and 3 for cases per million, total cases, and active cases, respectively. In particular, we can write the log-linear model for j=1, 2, and 3 as follows:
An objective of giving a log-linear model is to show a trend in between temperature and other variables. It is expected that the outcomes from models will support our hypothesis under study based on univariate correlation coefficients.
Results
Geographical distribution of countries having higher COVID-19 cases
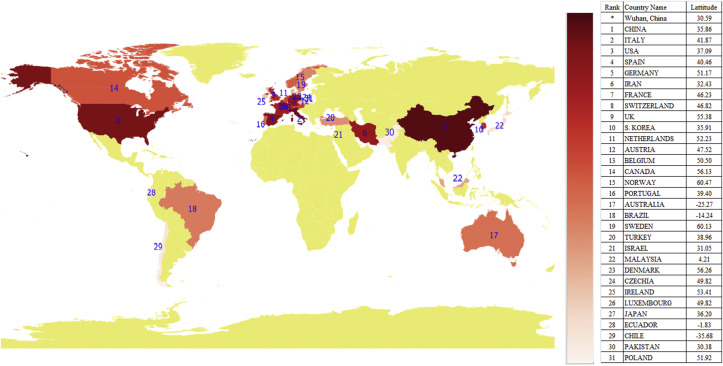
The outbreak of novel coronavirus (SARS-CoV-2) was first reported in Wuhan, China, at the end of December 2019. In January 2020, a few individuals of other countries had also been infected with the coronavirus. However, by mid January 2020, the number of confirmed COVID-19 cases became more than 200. By March 25, 2020, almost 200 countries reported coronavirus infected cases, where thirty one countries were badly affected with more than 1000 confirmed cases. It was noticed that majority of the severely affected countries (27 of 31) are geographically situated on the similar latitude as Wuhan (30.59 0N) or located toward the North Pole (Fig. 1). Except Ecuador, none of these twenty countries belong to the equatorial zone. Three countries of the Southern hemisphere (Australia, Brazil, and Chile) are located near by the Tropic of Capricorn. All these are relatively cold countries because of their geographical location. It was noticed that Hong Kong (22.31 0N) and Taiwan (23.69 0N), the territory/country neighboring China which are located away from Wuhan toward the equatorial side, had reported at least 10 COVID-19 confirmed cases by the end of January 2020. But till 25th March, 2020, the infected individuals were less than 500 in these two countries. Besides many reasons for spreading infection, cold environmental temperature could be an underestimated additional risk factor for COVID-19 cases.
Fig. 1.
Geographical distribution of the top countries having at least 1000 COVID-19 confirmed cases as of 25th of March, 2020. Table shows the list of 31 countries with their latitudes. Here, minus value latitude depicts the country of Southern hemisphere. COVID-19, coronavirus disease 2019.
Association between environment temperature and COVID-19 cases of a country
The aforementioned initial observations had attracted our attention to see the link between environment temperature and the novel coronavirus infection cases of a country. Firstly, univariate analysis was performed between MAET and coronavirus infected cases of a country, taking all the available data present in the website mentioned in method section. This website updates data every day for all countries. As per the data available in this website on 25th March 2020, coronavirus confirmed cases were reported from ∼200 countries. Spearman statistical analysis found a negative correlation between MAET and coronavirus confirmed cases of a country (correlation coefficient: −0.54 and P value: <0.0001). Furthermore, this analysis found negative correlation between MAET and total active cases (Table 1 ). Our analysis also noticed a presence of a significant correlation between cases per million population and MAET (correlation coefficient: −0.47 and P value: <0.0001) (Table 1). All these statistical results indicated that a negative link might exist between COVID-19 cases and environment temperature of a country. Just to verify all these results, we had further analyzed all the data by the Kendall univariate method. Similar to the Spearman method, Kendall analysis also found the negative association between environment temperature and various COVID-19 cases mentioned earlier. The observed values were highly dynamic, and thus, we have further analyzed the data of every six days intervals (30th March, 6th April, 12th April, and 18th April, 2020) to see the consistency of the statistical results among the data of different days. It was noticed that all these results from the analysis of these days’ data found similar results to the data of 25th March 2020 (Table 1). All these findings suggest that cold environment temperature might be sensitive to novel coronavirus (SAAR-CoV-2) infection.
Table 1.
Univariate analysis between monthly average environment temperature and COVID-19 cases: countrywise analysis, as of 25th March to 18th April, 2020.
| Method | Cases per million | Total cases | Active cases |
|---|---|---|---|
| 25th March, 2020 | |||
| Total country | 198 | 198 | 198 |
| Spearman | −0.47 | −0.54 | −0.54 |
| Kendall | −0.32 | −0.37 | −0.37 |
| 30th March, 2020 | |||
| Total country | 200 | 200 | 200 |
| Spearman | −0.49 | −0.54 | −0.55 |
| Kendall | −0.34 | −0.37 | −0.37 |
| 6th April, 2020 | |||
| Total country | 200 | 200 | 200 |
| Spearman | −0.50 | −0.49 | −0.49 |
| Kendall | −0.34 | −0.33 | −0.33 |
| 12th April, 2020 | |||
| Total country | 200 | 200 | 200 |
| Spearman | −0.50 | −0.46 | −0.44 |
| Kendall | −0.34 | −0.31 | −0.31 |
| 18th April, 2020 | |||
| Total country | 200 | 200 | 200 |
| Spearman | −0.50 | −0.45 | −0.42 |
| Kendall | −0.34 | −0.31 | −0.30 |
Note: P value corresponding to each test statistic is ∗P < 0.001. We have considered those countries having COVID-19 cases on at least 30th March, 2020 or before. COVID-19, coronavirus disease 2019.
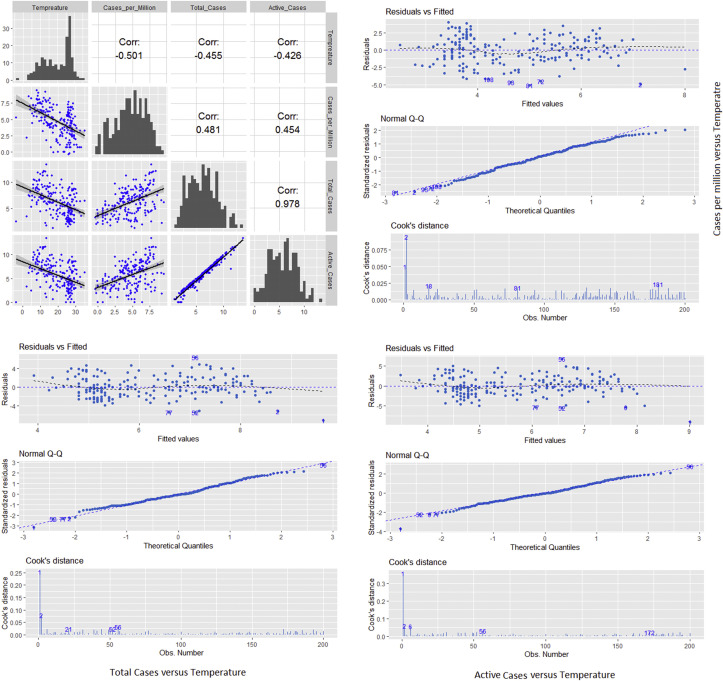
Log-linear model fit study for finding the relationship between temperature and COVID-19 cases
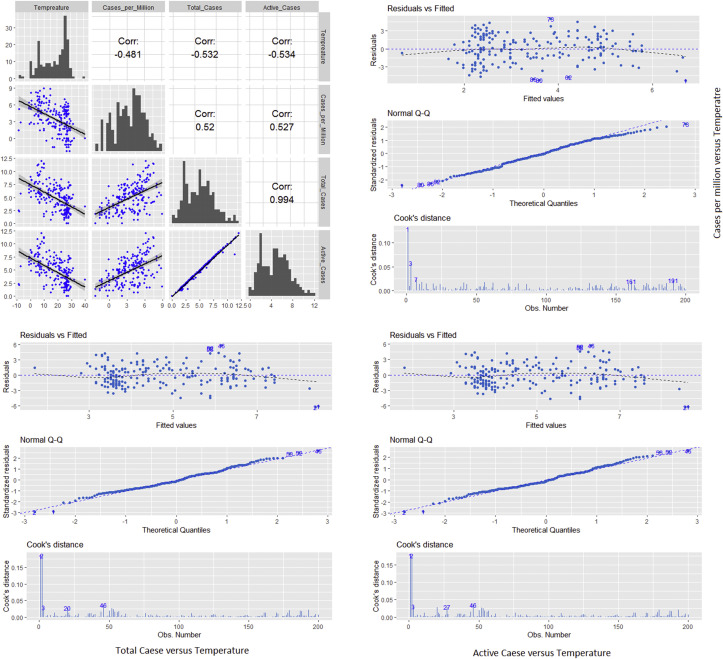
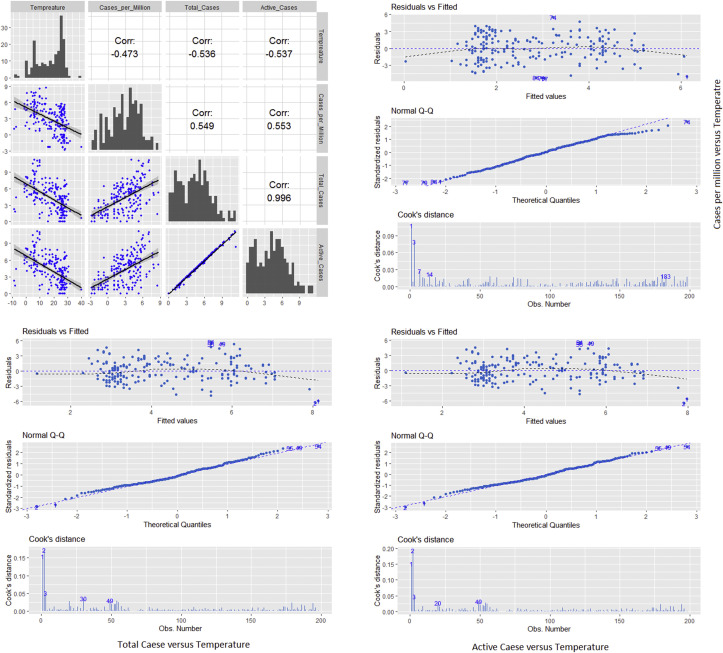
To verify and support the study of the earlier section, a log-linear model fitting approach has been adopted. The outcomes from modeling are shown in Table 2 and Fig. 2 . In Fig. 2, a matrix plot was drawn among temperature and three previously mentioned cases for the observations collected at April 18, 2020. Here, the temperature is measured in °C while all other variables are represented on natural logarithmic scales, where the base is e. On the diagonal of matrix plot the histograms are plotted for temperature, cases per million, total cases and active cases respectively, and it is helpful to identify the nature of the variables. In upper matrix plots, Pearson correlation coefficients (now, variables are in linear relationship) were determined. It can be seen that a negative relationship exists among variables and temperature with correlation coefficient values −0.501, −0.455, and −0.426 for cases per million, total cases, and active cases, respectively. The log-linear model was also estimated and fitted for COVID-19 considered cases and temperature. In the lower matrix plots, all the fitted models are sketched. The estimated values of parameters are , and for j = 1, 2, and 3, respectively (Table 2). All estimators were also tested and the respective P-values are less than .0001. As the estimates of for all three cases are negative, the models show the decreasing behavior of variables with respect to temperature. In Fig. 2, to support the purposed log-linear model for fitting, we additionally present important characteristics using graphs such as residuals, Q-Q, and Cook's distance plot. The residuals and Q-Q plot showed that the data fulfill the assumptions of fitting a log-linear model. Here, it was observed that in the Q-Q plot, few observations on both the tails behave abruptly. The Cook's distance plot also shows similar behavior. These observations may also be treated as extreme values or outliers.
Table 2.
Log-linear model estimates for fitting the relationship between the environment temperature and COVID-19 cases: countrwise analysis;, as of 25th March to 18th April, 2020.
| Date | Parameter | Cases per million | Total cases | Active cases |
|---|---|---|---|---|
| March 25, 2020 | Total country | 198 | 198 | 198 |
| Correlation coefficient | −0.4732 | −05368 | −0.5372 | |
| Estimated | 5.0537 | 6.9065 | 6.7650 | |
| Estimated | −0.1257 | −0.1437 | −0.1417 | |
| March 30, 2020 | Total country | 200 | 200 | 200 |
| Corr. Coefficient | −0.4812 | −0.5326 | −0.5349 | |
| Estimated | 5.6452 | 7.4464 | 7.2983 | |
| Estimated | −0.1243 | −0.1412 | −0.1430 | |
| April 06, 2020 | Total country | 200 | 200 | 200 |
| Correlation coefficient | −0.5074 | −0.4952 | −0.4957 | |
| Estimated | 7.1143 | 8.7121 | 8.4357 | |
| Estimated | −0.1557 | −0.1609 | −0.1594 | |
| April 12, 2020 | Total country | 200 | 200 | 200 |
| Correlation coefficient | −0.5030 | −0.4732 | −0.4471 | |
| Estimated | 7.367 | 8.9742 | 8.1017 | |
| Estimated | −0.1493 | −0.1550 | −0.1318 | |
| April 18, 2020 | Total country | 200 | 200 | 200 |
| Correlation coefficient | −0.5012 | −0.4558 | −0.4266 | |
| Estimated | 7.5013 | 9.1077 | 8.1521 | |
| Estimated | −0.1429 | −0.1484 | −0.1300 |
Note: Karl Pearson correlation coefficient is calculated for log-linear data. COVID-19, coronavirus disease 2019.
Fig. 2.
A matrix plot among month average temperature (°C), cases per million, total cases, and active cases (except temperature all other variable are measured on logarithmic scale) of COVID-19 on April 18, 2020. COVID-19, coronavirus disease 2019.
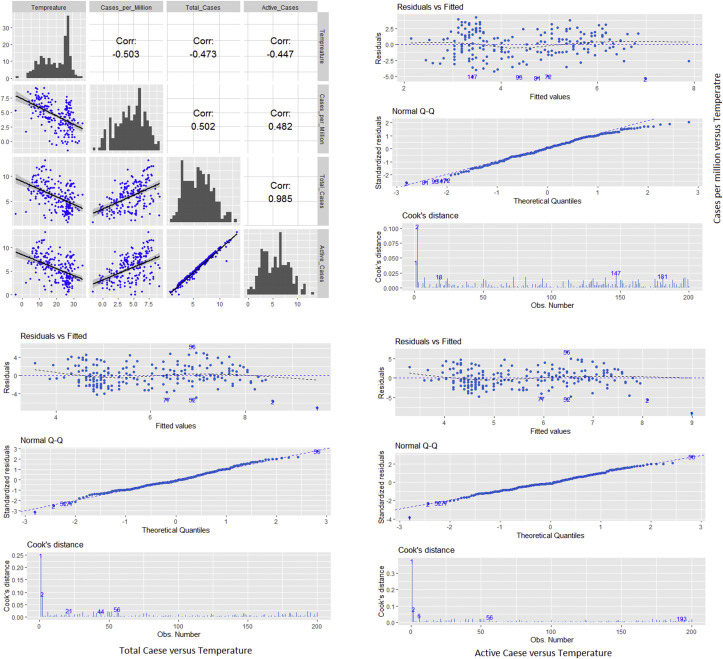
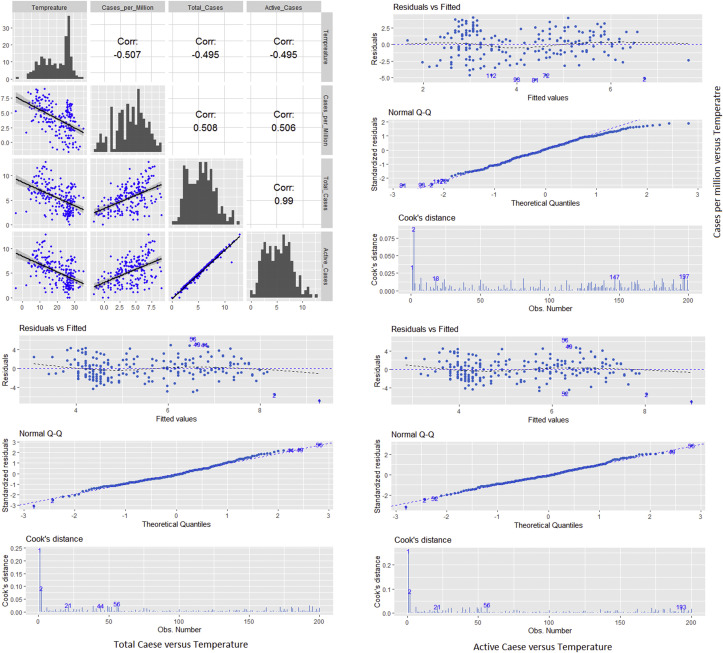
To establish the aforementioned findings, we used the observations particularly on other four days (25th March, 30th March, 6th April, and 12th April, 2020). We have noticed the consistency for estimated results and all models following the same pattern as the data obtained from dated April 18, 2020 (Supplementary Figs. S1–4). Sometime the slight differences in outcomes are obvious because few countries had contributed from early days, while others had participated significantly in the study later on. This effect has been discussed in Negative relationship exists between environment temperature and COVID-19 cases of the countries having at least 50 cases or more.
All these findings support our earlier establishment firmly that in warmer countries the chance of patients to contract COVID-19 is less than that in colder countries. Therefore, the results can be drawn firmly from univariate analysis.
Negative relationship exists between environment temperature and COVID-19 cases of the countries having at least 50 cases or more
It was noticed that all the countries under this study did not have the uniform COVID-19 observations till dated April 18, 2020. In fact, observation values of total cases (cases per million or active cases) are very low in countries lying in the hotter temperature zone. Therefore, observations from such countries may influence the performance of estimators significantly. Therefore, a comparative analysis has been performed for temperature and considered three variables as per the total number of cases (Table 3 ). Here, we grouped the countries as they have greater than or equal to 1, 50, 100, and 1000 total number of COVID-19 cases at the date of study. In Table 3, one row mentioned the number of countries comes under these groups at a particular day. We calculated Karl Pearson correlation coefficient for log-linear data with Spearman and Kendall correlation coefficients. Particularly, the mean, median, and standard deviation (SD) of temperatures were measured for a group designed as per total number of cases.
Table 3.
Comparative analysis among correlation coefficients and temperature variations for the countries having at least 50, 100, and 1000 COVID-19 cases.
| Total case ≥ | Cases per million |
Total cases |
Active cases |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 50 | 100 | 1000 | 1 | 50 | 100 | 1000 | 1 | 50 | 100 | 1000 | |
| 25th March, 2020 | ||||||||||||
| Total country | 198 | 112 | 91 | 31 | 198 | 112 | 91 | 31 | 198 | 112 | 91 | 31 |
| Pearson | −0.47 | −0.41 | −0.43 | −0.42 | −0.54 | −0.31 | −0.28 | −0.19 | −0.54 | −0.31 | −0.29 | −0.18 |
| Spearman | −0.47 | −0.40 | −0.43 | −0.31 | −0.54 | −0.30 | −0.24 | −0.10 | −0.54 | −0.31 | −0.26 | −0.10 |
| Kendall | −0.32 | −0.28 | −0.29 | −0.22 | −0.37 | −0.20 | −0.15 | −0.08 | −0.37 | −0.20 | −0.16 | −0.05 |
| Temperature mean | 17.84 | 13.71 | 12.86 | 8.98 | 17.84 | 13.71 | 12.86 | 8.98 | 17.84 | 13.71 | 12.86 | 8.98 |
| Temperature median | 21.00 | 12.75 | 12.00 | 6.50 | 21.00 | 12.75 | 12.00 | 6.50 | 21.00 | 12.75 | 12.00 | 6.50 |
| Temperature SD | 9.81 | 9.41 | 8.86 | 6.45 | 9.81 | 9.41 | 8.86 | 6.45 | 9.81 | 9.41 | 8.86 | 6.45 |
| 30th March, 2020 | ||||||||||||
| Total country | 200 | 123 | 110 | 43 | 200 | 123 | 110 | 43 | 200 | 123 | 110 | 43 |
| Pearson | −0.48 | −0.42 | −0.44 | −0.55 | −0.53 | −0.37 | −0.34 | −0.32 | −0.53 | −0.38 | −0.34 | −0.31 |
| Spearman | −0.49 | −0.41 | −0.44 | −0.46 | −0.54 | −0.38 | −0.34 | −0.24 | −0.55 | −0.39 | −0.35 | −0.25 |
| Kendall | −0.34 | −0.28 | −0.31 | −0.32 | −0.37 | −0.25 | −0.22 | −0.14 | −0.37 | −0.26 | −0.23 | −0.15 |
| Temperature mean | 17.86 | 14.31 | 13.70 | 10.97 | 17.86 | 14.31 | 13.70 | 10.97 | 17.86 | 14.31 | 13.70 | 10.97 |
| Temperature median | 21.00 | 13.90 | 13.00 | 8.00 | 21.00 | 13.90 | 13.00 | 8.00 | 21.00 | 13.90 | 13.00 | 8.00 |
| Temperature SD | 9.78 | 9.41 | 9.39 | 8.88 | 9.78 | 9.41 | 9.39 | 8.88 | 9.78 | 9.41 | 9.39 | 8.88 |
| 6th April, 2020 | ||||||||||||
| Total country | 200 | 137 | 125 | 61 | 200 | 137 | 125 | 61 | 200 | 137 | 125 | 61 |
| Pearson | −0.51 | −0.55 | −0.56 | −0.56 | −0.50 | −0.41 | −0.37 | −0.28 | −0.49 | −0.41 | −0.38 | −0.29 |
| Spearman | −0.50 | −0.54 | −0.55 | −0.58 | −0.49 | −0.41 | −0.38 | −0.30 | −0.49 | −0.41 | −0.38 | −0.29 |
| Kendall | −0.34 | −0.38 | −0.39 | −0.40 | −0.33 | −0.28 | −0.25 | −0.18 | −0.33 | −0.28 | −0.26 | −0.17 |
| Temperature mean | 19.84 | 17.81 | 17.30 | 15.32 | 19.84 | 17.80 | 17.30 | 15.32 | 19.84 | 17.81 | 17.30 | 15.32 |
| Temperature median | 22.00 | 16.50 | 15.50 | 14.00 | 22.00 | 16.50 | 15.50 | 14.00 | 22.00 | 16.50 | 15.50 | 14.00 |
| Temperature SD | 8.00 | 7.96 | 7.96 | 7.53 | 8.00 | 7.96 | 7.96 | 7.53 | 8.00 | 7.96 | 7.96 | 7.53 |
| 12th April, 2020 | ||||||||||||
| Total country | 200 | 146 | 130 | 71 | 200 | 146 | 130 | 71 | 200 | 146 | 130 | 71 |
| Pearson | −0.50 | −0.52 | −0.56 | −0.50 | −0.47 | −0.42 | −0.37 | −0.20 | −0.45 | −0.41 | −0.36 | −0.20 |
| Spearman | −0.50 | −0.53 | −0.55 | −0.51 | −0.46 | −0.42 | −0.37 | −0.15 | −0.44 | −0.41 | −0.37 | −0.17 |
| Kendall | −0.34 | −0.37 | −0.38 | −0.35 | −0.31 | −0.28 | −0.24 | −0.08 | −0.31 | −0.28 | −0.24 | −0.10 |
| Temperature mean | 19.84 | 18.21 | 17.54 | 15.25 | 19.84 | 18.21 | 17.54 | 15.25 | 19.84 | 18.21 | 17.54 | 15.25 |
| Temperature median | 22.00 | 17.25 | 16.00 | 13.50 | 22.00 | 17.25 | 16.00 | 13.50 | 22.00 | 17.25 | 16.00 | 13.50 |
| Temperature SD | 8.00 | 7.92 | 7.93 | 7.50 | 8.00 | 7.92 | 7.93 | 7.50 | 8.00 | 7.92 | 7.93 | 7.50 |
| 18th April, 2020 | ||||||||||||
| Total country | 200 | 155 | 136 | 78 | 200 | 155 | 136 | 78 | 200 | 155 | 136 | 78 |
| Pearson | −0.50 | −0.54 | −0.55 | −0.48 | −0.46 | −0.45 | −0.38 | −0.18 | −0.43 | −0.42 | −0.36 | −0.16 |
| Spearman | −0.50 | −0.55 | −0.57 | −0.49 | −0.45 | −0.44 | −0.38 | −0.14 | −0.42 | −0.41 | −0.36 | −0.13 |
| Kendall | −0.34 | −0.38 | −0.40 | −0.35 | −0.31 | −0.30 | −0.26 | −0.08 | −0.30 | −0.28 | −0.25 | −0.08 |
| Temperature mean | 19.84 | 18.71 | 17.90 | 15.51 | 19.84 | 18.71 | 17.90 | 15.51 | 19.84 | 18.71 | 17.90 | 15.51 |
| Temperature median | 22.00 | 18.50 | 16.50 | 13.50 | 22.00 | 18.50 | 16.50 | 13.50 | 22.00 | 18.50 | 16.50 | 13.50 |
| Temperature SD | 8.00 | 7.98 | 7.97 | 7.69 | 8.00 | 7.98 | 7.97 | 7.69 | 8.00 | 7.98 | 7.97 | 7.69 |
Note: Karl Pearson correlation coefficient is calculated for log-linear data. Temperature is in °C. COVID-19, coronavirus disease 2019; SD, standard deviation.
It was noticed that the number of countries was consistently increasing in each group from first day of study until today (Table 3). Other variables those have the influence of these designed groups in table were descriptive measures of temperature. For example, at dated 18th April for cases per million, the mean of temperature among groups varied from 19.8 °C to 15.5 °C and similarly for median of temperature from 22 °C to 13.5 °C with SD from 8.0 °C to 7.6 °C. These measures are getting a wider range, that is, average minimum and average maximum difference as approaches toward back days. Similar behavior can be seen for total case and active case columns in Table 3. If the number of a country in a group is lesser then respective temperature SD is also small. This is obvious because of as total cases restriction increases the countries in a group comes from a more homogenous temperature zone. So, as the restriction of total number of cases increases from 1 to 1000 the average temperature and SD decreases simultaneously. These homogenous temperature zones impact can be seen through the respective correlation coefficients directly. For example, at dated 18th April, 2020 for active cases as average temperature reduces from 19.8 °C to 15.5 °C/22 °C–13.5 °C for mean/median with number of countries from 200 to 78 and hence correlation coefficients increase drastically from −0.45 to −0.15, −0.42 to −0.12 and −0.29 to −0.07 for Pearson, Spearman and Kendall coefficient, respectively. The similar outcomes can be seen for other cases and as well as on other days. So, it can be interpreted as the correlation coefficient is decreasing because of it is calculated for within more homogenous time zone countries. That is why it is approaching toward the zero and trying to show an independent relationship with larger total number restriction. Here it is to be noted that as one is going backward in days for within group the correlation coefficients are performing consistently. So, the results drawn on the behalf of earlier table can be considered stable.
All these findings further suggest that a negative link exists between environment temperature and COVID-19 cases.
Discussion
The recent ongoing pandemic of COVID-19 is growing rapidly throughout the world, which emerged in Wuhan, China, at the end of the year 2019. As of 18th April 2020, more than 2.4 million confirmed cases have been reported from 200 countries. This fatal outbreak has already killed almost 150,000 individuals worldwide. In the last few weeks, the numbers of infection cases and deaths had been found to increase with a tremendous high rate. To date, no medicines or vaccines are available for its treatment. All countries are strictly forcing various strategies such as travel restrictions, social distancing, and quarantines as preventive measures. To prevent infection, the travel connection between different countries, states, and cities has been restricted from the end of March, 2020. Various countries have also imposed curfews and lockdowns to prevent the direct contact between individuals. In this context, many people, scientists, researchers, and others think that novel coronavirus infection may be decreased as the summer comes, that is, as the environment temperature increases. It has been reported that infection and transmission of many virus types including influenza depends on air temperature and humidity.10 , 11 However, no such report has yet been published in case of this viral infection and/or transmission. The recent report suggests that the viability of this new coronavirus greatly varies on different object surfaces such as stainless steel, plastic, cardboard, copper, and so on.12 Here, object surface temperature might influence the longevity of the active virus particles. Thus, this study has given an attention to see the link between air temperature and COVID-19 cases. It was carefully observed that countries having larger COVID-19 cases are mostly located above of the latitude of Wuhan, which indicated that there might be a negative relationship between temperature and COVID-19 cases (Fig. 1). Next, the countrywise statistical analysis by various statistical methods has found a significant negative correlation between various COVID-19 cases including total cases, active cases, and cases per million of a country with MAET. Similar negative relationships between these two parameters at the MAET were found when the data of the countries having at least 50, 100, 1000 or more COVID-19 confirm cases (Table 3). All these observations suggest that low temperature might be a risk factor for COVID-19 cases. Next, we wanted to know whether the summer temperature can decrease this viral infection. Similar to our study, Chan et al.13, 2011 reported that viability of other types of SARS coronaviruses was decreased with high temperature and low humidity environment. Their study also suggests that tropical countries have low risk of SARS coronavirus infection as compared with relatively cold countries. Thus, this present study gives a hint that the summer may reduce the SARS-CoV-2 infection/transmission rate as compared with the current season. Cold environment modulates many biological functions in our body. Our recent studies including other investigations have suggested that cold environment might be a risk factor for cancer diseases because cold adaption in long duration may provoke the cancer risk probably by altering various physiological and cellular functions with the influence of epigenetic changes and bringing mutations in tumor suppressor genes.7 , 8 , 14, 15, 16, 17 It was also reported that cold exposure decreased antitumor immunity to increase cancer growth and metastasis in an animal model.18 Similarly, various studies documented that cold environment is relatively susceptible to viral infection because of suppression of immune responses.19 Studies also reported the link between cold environment and asthma.20 In regard to COVID-19, all people may not be infected upon exposure of this novel coronavirus. Some of them may be infected. Some infected people develop severe acute respiratory distress symptoms.21 The recent clinical study reported that severe cases of this virus infected patients have lower monocytes, eosinophil, basophils, and T cells.22 This viral infection may not vary much with respect to the age of the individual, but fatality is more in the case of old individuals.21 The immune system of the elderly may not support enough to provide adaptive and boost immune responses to fight this novel coronavirus infection and its severity. In this situation, people living in cold environments might be an additional risk for COVID-19 severity. However, at this time, this study is unable to explain of how some cold countries have relatively higher coronavirus infected cases. Is it just the cold or are there additional factors? Second, is it possible that the warm temperature kills more viruses but also the ones that are able to grow are less virulent and cause less damage? Moreover, extended analysis with a large set of data is required to prove this negative link between environment temperature and COVID-19 cases.
The accumulating evidence reveals that the severity is more in cases of patients with COVID-19 having preexisting health issues such as diabetes, hypertension, obesity, cancer, and heart and kidney diseases.23 , 24 All published reports state that the virus enters inside the cells by endocytosis process, where the viral spike proteins (S) interact with cell surface receptor angiotensin-converting enzyme 2 (ACE-2) proteins present over epithelial cells of the respiratory tract, lungs ,and other tissues.25 , 26 It has also been suggested that this coronavirus enters in the circulation and infects various organ tissues (kidney, cardiac muscles, colon, adipocytes, and so on) having higher expression of ACE-2 on their cell surface.27 Here, the host cell serine protease transmembrane Serine Protease 2 (TMPRSS2) primes spike glycoprotein (S) to facilitate infection.26 For example, patients with type II diabetes may have high risk of coronavirus infection because of high expression of ACE-2 expression in the pancreas.28 Similarly, adipose tissue may express more ACE-2 than lungs epithelial cells, thus obese people may have also high risk of this viral infection.29 Studies reported that the patients with high body mass index had severe form of this virus infection.30 It has also been suggested that some drugs used for the treatment of hypertension and diabetes may increase the expression of ACE-2 which invites the higher risk of virus infection.23 , 24 All these findings suggest that the high expression of ACE-2 and TMPRSS2 in host cells is a great risk factor for this novel coronavirus infection. Moreover, implemented strategies for preventive measures to control the spreading of infection greatly vary from one country to others, which may also affect this negative relationship. Moreover, sensitivity of coronavirus (SARS-CoV-2) to temperature may vary from one mutant type to others. In addition, the efficacy of such infection may differ in various ages, races, ethnicities, and genders. Beside these, infectivity may also be dependent on various other local contextual factors such as hygiene practices, population crowding, and living style.31
This study has been carried out at a very early stage as COVID-19 became a worldwide outbreak. And due to some limitations, the comorbidity factors are not included at this study. In future work, we can upgrade the same result with great extent by considering additional covariates (e.g., factors such as diabetes, obesity, hypertension, cancers, and humidity of a country).
This pilot study proposes that high temperature may delay this novel coronavirus infection. Of course, experimental study can say whether and how cold environment augments coronavirus infection and/transmission.
Author statements
Ethical approval
None sought.
Funding
None declared.
Competing interests
All authors declare that they have no conflict of interest.
Acknowledgment
C.C.M. is supported by University Grants Commission [30–49/2014 (BSR)], Department of Biotechnology, India [6242-P9/RGCB/PMD/DBT/CCML/2015], and Department of Science and Technology (India)-Russian Foundation of Basic Research [INT/RUS/RFBR/P-256]. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.puhe.2020.05.065.
Appendix A. Supplementary data
The following are the Supplementary data to this article:
Multimedia component 1
Supplementary Fig. S1.
A matrix plot among month average temperature (°C), cases per million, total cases and active cases (except temperature all other variable are measured on logarithmic scale) of Covid-19 on April 12, 2020.
Supplementary Fig. S2.
A matrix plot among month average temperature (°C), cases per million, total cases and active cases (except temperature all other variable are measured on logarithmic scale) of Covid-19 on April 6, 2020.
Supplementary Fig. S3.
A matrix plot among month average temperature (°C), cases per million, total cases and active cases (except temperature all other variable are measured on logarithmic scale) of Covid-19 on March 30, 2020.
Supplementary Fig. S4.
A matrix plot among month average temperature (°C), cases per million, total cases and active cases (except temperature all other variable are measured on logarithmic scale) of Covid-19 on March 25, 2020.
References
- 1.Lu R., Zhao X., Li J., Niu P., Yang B., Wu H. Genomic characterisation and epidemiology of 2019 novel coronavirus: implications for virus origins and receptor binding. Lancet. 2020;395:565–574. doi: 10.1016/S0140-6736(20)30251-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ji W., Wang W., Zhao X., Zai J., Li X. Cross-species transmission of the newly identified coronavirus 2019-nCoV. J Med Virol. 2020;92:433–440. doi: 10.1002/jmv.25682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Benvenuto D., Giovanetti M., Ciccozzi A., Spoto S., Angeletti S., Ciccozzi M. The 2019-new coronavirus epidemic: evidence for virus evolution. J Med Virol. 2020;92:455–459. doi: 10.1002/jmv.25688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sun P., Lu X., Xu C., Sun W., Pan B. Understanding of COVID-19 based on current evidence. J Med Virol. 2020;25:25722. doi: 10.1002/jmv.25722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Li Q., Guan X., Wu P., Wang X., Zhou L., Tong Y. Early transmission dynamics in wuhan, China, of novel coronavirus-infected pneumonia. N Engl J Med. 2020;382:1199–1207. doi: 10.1056/NEJMoa2001316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Xu X.W., Wu X.X., Jiang X.G., Xu K.J., Ying L.J., Ma C.L. Clinical findings in a group of patients infected with the 2019 novel coronavirus (SARS-Cov-2) outside of Wuhan, China: retrospective case series. Bmj. 2020;19 doi: 10.1136/bmj.m606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sharma A., Sharma T., Panwar M.S., Sharma D., Bundel R., Hamilton R.T. Colder environments are associated with a greater cancer incidence in the female population of the United States. Tumour Biol. 2017;39 doi: 10.1177/1010428317724784. 1010428317724784. [DOI] [PubMed] [Google Scholar]
- 8.Mandal C.C., Sharma A., Panwar M.S., Radosevich J.A. Is cholesterol a mediator of cold-induced cancer? Tumour Biol. 2016;37:9635–9648. doi: 10.1007/s13277-016-4799-2. [DOI] [PubMed] [Google Scholar]
- 9.Sharma A., Verma H.K., Joshi S., Panwar M.S., Mandal C.C. A link between cold environment and cancer. Tumor Biol. 2015:1–12. doi: 10.1007/s13277-015-3270-0. [DOI] [PubMed] [Google Scholar]
- 10.Lowen A.C., Steel J. Roles of humidity and temperature in shaping influenza seasonality. J Virol. 2014;88:7692–7695. doi: 10.1128/JVI.03544-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Steel J., Palese P., Lowen A.C. Transmission of a 2009 pandemic influenza virus shows a sensitivity to temperature and humidity similar to that of an H3N2 seasonal strain. J Virol. 2011;85:1400–1402. doi: 10.1128/JVI.02186-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.van Doremalen N., Bushmaker T., Morris D.H., Holbrook M.G., Gamble A., Williamson B.N. Aerosol and surface stability of SARS-CoV-2 as compared with SARS-CoV-1. N Engl J Med. 2020 Mar 17 doi: 10.1056/NEJMc2004973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Chan K.H., Peiris J.S., Lam S.Y., Poon L.L., Yuen K.Y., Seto W.H. The effects of temperature and relative humidity on the viability of the SARS coronavirus. Adv Virol. 2011;734690:1. doi: 10.1155/2011/734690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Sharma A., Verma H.K., Joshi S., Panwar M.S., Mandal C.C. A link between cold environment and cancer. Tumour Biol. 2015;36:5953–5964. doi: 10.1007/s13277-015-3270-0. [DOI] [PubMed] [Google Scholar]
- 15.Voskarides K. Combination of 247 genome-wide association studies reveals high cancer risk as a result of evolutionary adaptation. Mol Biol Evol. 2018;35:473–485. doi: 10.1093/molbev/msx305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Mravec B., Tibensky M. Increased cancer incidence in “cold” countries: an (un) sympathetic connection? J Therm Biol. 2020:102538. doi: 10.1016/j.jtherbio.2020.102538. [DOI] [PubMed] [Google Scholar]
- 17.Bandyopadhayaya S., Ford B., Mandal C.C. Cold-hearted: a case for cold stress in cancer risk. J Therm Biol. 2020:102608. doi: 10.1016/j.jtherbio.2020.102608. [DOI] [PubMed] [Google Scholar]
- 18.Kokolus K.M., Capitano M.L., Lee C.T., Eng J.W., Waight J.D., Hylander B.L. Baseline tumor growth and immune control in laboratory mice are significantly influenced by subthermoneutral housing temperature. Proc Natl Acad Sci U S A. 2013;110:20176–20181. doi: 10.1073/pnas.1304291110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.LaVoy E.C., McFarlin B.K., Simpson R.J. Immune responses to exercising in a cold environment. Wilderness Environ Med. 2011;22:343–351. doi: 10.1016/j.wem.2011.08.005. [DOI] [PubMed] [Google Scholar]
- 20.Xu Z., Crooks J.L., Davies J.M., Khan A.F., Hu W., Tong S. The association between ambient temperature and childhood asthma: a systematic review. Int J Biometeorol. 2018;62:471–481. doi: 10.1007/s00484-017-1455-5. [DOI] [PubMed] [Google Scholar]
- 21.Shi Y., Wang Y., Shao C., Huang J., Gan J., Huang X. 2020 Mar 23. COVID-19 infection: the perspectives on immune responses: cell Death Differ. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Qin C., Zhou L., Hu Z., Zhang S., Yang S., Tao Y. Dysregulation of immune response in patients with COVID-19 in Wuhan, China. Clin Infect Dis. 2020;12 doi: 10.1093/cid/ciaa248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Fang L., Karakiulakis G., Roth M. Are patients with hypertension and diabetes mellitus at increased risk for COVID-19 infection? Lancet Respir Med. 2020 Apr;8(4):e21. doi: 10.1016/S2213-2600(20)30116-8. Epub 2020 Mar 11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Sommerstein R., Kochen M.M., Messerli F.H., Gräni C. Coronavirus disease 2019 (COVID-19): do angiotensin-converting enzyme inhibitors/angiotensin receptor blockers have a biphasic effect? J Am Heart Assoc. 2020;9:1. doi: 10.1161/JAHA.120.016509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Zhou P., Yang X.L., Wang X.G., Hu B., Zhang L., Zhang W. A pneumonia outbreak associated with a new coronavirus of probable bat origin. Nature. 2020;579:270–273. doi: 10.1038/s41586-020-2012-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Hoffmann M., Kleine-Weber H., Schroeder S., Krüger N., Herrler T., Erichsen S. SARS-CoV-2 cell entry depends on ACE2 and TMPRSS2 and is blocked by a clinically proven protease inhibitor. Cell. 2020;181:271–280. doi: 10.1016/j.cell.2020.02.052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Huang J., Song W., Huang H., Sun Q. Pharmacological therapeutics targeting RNA-dependent RNA polymerase, proteinase and spike protein: from mechanistic studies to clinical trials for COVID-19. J Clin Med. 2020;9 doi: 10.3390/jcm9041131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Bornstein S.R., Dalan R., Hopkins D., Mingrone G., Boehm B.O. Endocrine and metabolic link to coronavirus infection. Nat Rev Endocrinol. 2020;16:297–298. doi: 10.1038/s41574-020-0353-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Jia X., Yin C., Lu S., Chen Y., Liu Q., Bai J. Preprints.org; 2020. Two things about COVID-19 might need attention. [Google Scholar]
- 30.Kassir R. Risk of COVID-19 for patients with obesity. Obes Rev. 2020 Jun;21(6) doi: 10.1111/obr.13034. Epub 2020 Apr 13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Lee A. Wuhan novel coronavirus (COVID-19): why global control is challenging? Publ Health. 2020;179:A1–A2. doi: 10.1016/j.puhe.2020.02.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Multimedia component 1