Abstract
Introduction
We aimed to analyze the psychological status in patients with breast cancer (BC) in the epicenter of the coronavirus disease 2019 (COVID-19) pandemic.
Patients and Methods
A total of 658 individuals were recruited from multiple BC centers in Hubei Province. Online questionnaires were conducted, and these included demographic information, clinical features, and 4 patient-reported outcome scales (Generalized Anxiety Disorder Questionnaire [GAD-7], Patient Health Questionnaire [PHQ-9], Insomnia Severity Index [ISI], and Impact of Events Scale-Revised [IES-R]). Multivariable logistic regression analysis was designed to identify potential factors on mental health outcomes.
Results
Questionnaires were collected from February 16, 2020 to February 19, 2020, the peak time point of the COVID-19 outbreak in China. Of patients with BC, 46.2% had to modify planned necessary anti-cancer treatment during the outbreak. Severe anxiety and severe depression were reported by 8.9% and 9.3% of patients, respectively. Severe distress and insomnia were reported by 20.8% and 4.0% of patients, respectively. Multivariable logistic regression analysis demonstrated poor general condition, shorter duration after BC diagnosis, aggressive BC molecular subtypes, and close contact with patients with COVID-19 as independent factors associated with anxiety. Poor general condition and central venous catheter flushing delay were factors that were independently associated with depression. In terms of insomnia, poor generation condition was the only associated independent factor. Poor physical condition and treatment discontinuation were underlying risk factors for distress based on multivariable analysis.
Conclusion
High rates of anxiety, depression, distress, and insomnia were observed in patients with BC during the COVID-19 outbreak. Special attention should be paid to the psychological status of patients with BC, especially those with poor general condition, treatment discontinuation, aggressive molecular subtypes, and metastatic BC.
Keywords: Breast cancer, COVID-19, Epicenter, Psychological status
Micro-Abstract
During the coronavirus disease 2019 (COVID-19) outbreak in China, fear about COVID-19, together with worry about progression of cancer, caused strong emotional stress in patients with cancer. We evaluated patient-reported outcome in 658 patients with breast cancer (BC) and survivors recruited from multiple BC centers in Hubei Province using 4 standardized assessment scales. Multivariable logistic regression analysis was used to identify potential affecting factors on mental health outcomes. High rates of anxiety, depression, distress, and insomnia were observed in patients with BC during the COVID-19 outbreak. Based on our results, living in Wuhan, poor general condition by self-identification, shorter duration after BC diagnosis, aggressive BC molecular subtypes, metastatic BC clinical stage, treatment discontinuation, central venous catheter flushing delay, or close contact with patients with COVID-19 are associated risk factors for poorer psychological status. Special attention should be paid to the psychological status of patients with BC, especially those with poor general condition, treatment discontinuation, aggressive molecular subtypes, and metastatic BC.
Introduction
Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) was initially identified in patients in Wuhan, Hubei Province, in December, 2019.1 The pandemic disease caused by this virus was named by the World Health Organization (WHO) as coronavirus disease 2019 (COVID-19).2 In late January of 2020, Chinese authorities placed a lockdown on Hubei Province to contain this disease.1 , 3 In addition, nearly all the medical resources were organized and more than 40,000 healthcare workers from other cities were dispatched to work together in Wuhan and other cities of Hubei.4 These measures and sacrifices have resulted in decreased rates of transmission and better outcomes in China.5
Studies from China have demonstrated that patients with cancer are significantly more likely to experience worse outcomes to COVID-19 infection,6 , 7 which has led to a re-evaluation of the risk/benefit balance in cancer therapies.8 , 9 Indeed, almost all the patients with cancer in Wuhan, the epicenter of COVID-19 in China, had to discontinue or delay their normal anticancer therapy owing to lockdown policies, limited medical resources, and the predicted increased risk of infection at the initial time of the outbreak. After the outbreak was under control, modified therapeutic regimens were recommended, and online prescriptions were available for patients with cancer because nearly all the cancer clinics were still not active. These changes can lead to significant increases in the psychological burden of patients with cancer, especially for those with breast cancer (BC).
BC is the most common cancer among women worldwide. The mean age of patients with BC in China is 45 to 55 years, which is considerably younger than for Western women, according to epidemiologic data from China.10 A diagnosis of BC can result in long-lasting mental health effects on women,11 such as physical hardship, traumatic events during treatment, fear of recurrence, etc. Furthermore, mental illness can further exacerbate the quality of life of patients with BC, resulting in worse BC outcomes.12 During the COVID-19 crisis, patients with BC in Hubei Province were exposed to a very high risk of COVID-19 infection and interruptions of standard medical care. Therefore, it is crucial to understand quality of life factors so they may be addressed during this outbreak and hopefully result in less stress for patients with BC. In this study, we conducted a survey to measure the psychological status of patients with BC and survivors and to identify potential affecting factors in the epicenter of COVID-19 in China at the peak time point of the crisis.
Patients and Methods
Patients
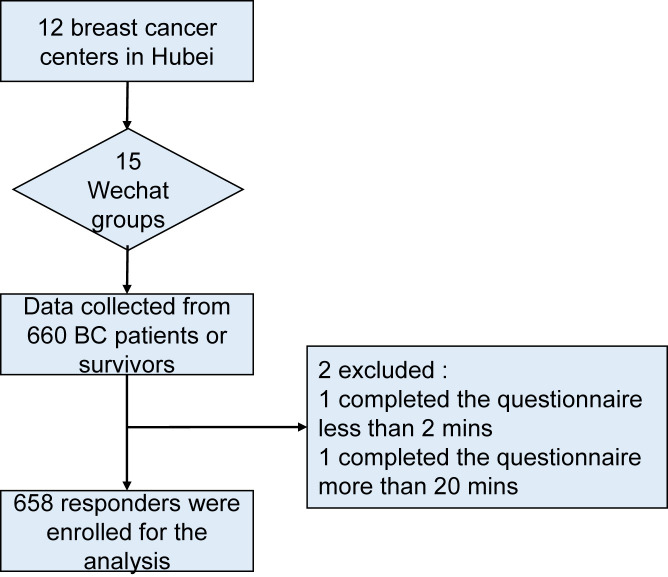
Patients with BC and survivors from the epicenter of COVID-19 in China, Hubei Province, were enrolled for this survey study. The study was sponsored by the BC center in Renmin Hospital of Wuhan University and was supported by several BC centers in Hubei province. All the enrolled patients signed digital informed consent before accessing the questionnaire online, consisting of a series of questions including demographic characteristics, clinical features of BC, current treatment, and patient-reported outcomes (PROs) using 4 validated psychological assessment scales. The 4 scales included Generalized Anxiety Disorder Questionnaire (GAD-7), Patient Health Questionnaire (PHQ-9), Insomnia Severity Index (ISI), and Impact of Events Scale-Revised (IES-R). Patients with BC were asked to answer all the questions anonymously through Wechat software, a popular social media platform in China. The local Wechat communication groups were set up originally for patients with BC to connect with their doctors for daily medical consultant and support. The questionnaires were issued to each local WeChat group for patients with BC from February 16 to 19, 2020. Data were collected from 660 patients with BC automatically after the questionnaires were returned. Two participants who completed the entire questionnaire less than 2 minutes or more than 20 minutes were excluded. Therefore, after the evaluation of questionnaires for eligibility, 658 participants were enrolled for analysis. The flowchart of the patient selection is shown in Figure 1 . This study protocol was approved by the Institutional Ethics Committee in Renmin Hospital of Wuhan University.
Figure 1.
The Flowchart of the Recruitment of Participants Enrolled for the Analysis
Abbreviation: BC = breast cancer.
Patient-reported Outcomes
PROs of patients with BC in the epicenter of the COVID-19 outbreak in China were evaluated using 4 Chinese versions of validated questionnaires.13, 14, 15, 16 GAD-7, a 7-item self-reported scale, was used to briefly measure anxiety disorders of the patients. Evaluation scores of 0, 1, 2, and 3 for 7 items represent the response categories of ‘not at all,’ ‘several days,’ ‘more than half the days,’ and ‘nearly every day,’ respectively. The cutoff point of the sum score for mild is a score of 5; for moderate is 10 and for severe is 15. Depression was measured by PHQ-9, a 9-question instrument, to screen for the presence and severity of depression. Responses of each question range from “0” (not at all) to “3” (nearly every day). Depression severity was classified into none (0-4), mild (5-9), moderate (10-14), and severe (> 15) according to the Diagnostic and Statistical Manual of Mental Disorders, fourth edition criteria. ISI is a self-assessment tool measuring the patient’s perception of both nocturnal and diurnal symptoms of insomnia. It has 7 questions. A 4-point Likert scale is used to rate each item (eg, 0 = none, 4 = very severe), yielding a total score ranging from 0 to 28. The total score is interpreted as follows: absent of insomnia (0-7); sub-threshold insomnia (8-14); moderate insomnia (15-21); and severe insomnia (22-28). The IES-R, also a self-reported questionnaire, yields a total score (ranging from 0 to 88). It was used to measure distress symptoms caused by the COVID-19 outbreak. The IES-R and subscale scores can also be calculated for the intrusion, avoidance, and hyperarousal status. These PRO tools have established sensitivity, specificity, reliability, and factorial and procedural validity.
Statistical Analysis
All statistical analysis were carried out with R software (version 3.5.1). Based on nonnormal distribution, the nonparametric Wilcoxon rank-sum test and Kruskal-Wallis test were used to compare the severity of each symptom among 2 or more groups. The univariable and multivariable logistic regression models were used to identify potential risk factors affecting psychological status for patients with BC. The association between risk factors and PROs are presented as odds radios (ORs) and 95% confidence intervals (CIs). The statistical significance level was set at P < .05, and all tests were 2-tailed.
Results
Baseline Characteristics of Patients With BC in the Center of COVID-19 Outbreak in China
After excluding 2 patients who completed the entire questionnaire in less than 2 minutes or more than 20 minutes, a total of 658 patients with BC were enrolled in this analysis, including 247 (37.5%) cases from Wuhan (the epicenter of the outbreak in China), and 411 (62.5%) cases from cities outside Wuhan in Hubei Province. The baseline characteristics of patients with BC are shown in Table 1 . The majority of the patients were from cities (485/658; 73.8%), younger than 55 years old (516/658; 78.4%), no bachelor’s or higher degree (515/658; 78.3%), married (584/658; 88.9%), and annual income less than $15,000 (554/658; 84.2%). Most of the patients presented with good or average physical condition by self-identification (496/658; 75.4%), had early stage BC (392/658; 59.6%), reported a history of prior breast surgery (628/658; 95.4%), and were recommend to undergo BC treatment during COVID-19 (474/658; 72.0%). Of 474 patients with BC recommended to undergo BC treatment, 219 (46.2%) patients had to discontinue or modify their planned necessary anticancer treatments, including systemic therapy and local therapy, during the outbreak. It also led to delays in the central venous catheter (CVC) flushing of over 4 weeks in 40.6% (164/276) of patients with implanted CVCs. The efficacy of compromised anti-cancer therapeutic regimens (519/966; 53.7%) was the main concern among these patients with BC, followed by the fear about infection of COVID-19 (191/966; 19.8%).
Table 1.
Patients Characteristics
| Characteristic | N (%)a |
|---|---|
| No. patients | 658 |
| Wuhan exposure | |
| Yes | 247 (37.5) |
| No | 411 (62.5) |
| Residence location | |
| Urban | 485 (73.8) |
| Rural | 173 (26.2) |
| Age, y | |
| ≤40 | 152 (23.1) |
| 40-54 | 364 (55.3) |
| 55-64 | 123 (18.7) |
| ≥65 | 19 (2.9) |
| Highest level of education | |
| Elementary school or less | 44 (6.7) |
| Middle school | 184 (28.0) |
| High school | 287 (43.6) |
| Bachelor’s degree or higher | 143 (21.7) |
| Annual income, US dollars | |
| <$7500 | 351 (53.3) |
| $7500-$15,000 | 203 (30.9) |
| $15,000-$43,000 | 95 (14.4) |
| >$43,000 | 9 (1.4) |
| Marital status | |
| Unmarried | 19 (2.9) |
| Married | 584 (88.9) |
| Divorced/widowed | 55 (8.2) |
| General health condition by self-identification | |
| Well | 269 (40.9) |
| Average | 227 (34.5) |
| Poor | 162 (24.6) |
| BC diagnosis time | |
| Within 1 year | 296 (45.0) |
| 1-5 years | 313 (47.6) |
| More than 5 years | 49 (7.4) |
| Stage of BC | |
| Early | 392 (59.6) |
| Metastatic | 115 (17.5) |
| Unknown | 151 (22.9) |
| Molecular subtype of BC | |
| TNBC | 127 (19.3) |
| Luminal | 177 (26.9) |
| HER2 | 196 (29.8) |
| Unknown | 158 (24.0) |
| History of BC surgery | |
| Yes | 628 (95.4) |
| No | 30 (4.6) |
| Recommend anti-cancer therapy | |
| Yes | 474 (72.0) |
| No | 184 (28.0) |
| Discontinued anticancer therapyb | |
| Endocrine therapy | 168 (32.9) |
| Targeted therapy | 105 (20.6) |
| Chemotherapy | 133 (26.1) |
| Radiotherapy | 27 (5.3) |
| Traditional Chinese medicine | 77 (15.1) |
| Duration of therapy interruptionc | |
| Less than 2 weeks | 135 (28.5) |
| 2-4 weeks | 102 (21.5) |
| Undefined | 131 (27.6) |
| Unknown | 88 (18.6) |
| No therapy discontinued | 18 (3.8) |
| CVC maintenance | |
| Not delayed | 112 (17.0) |
| Delayed | 164 (24.9) |
| No CVC | 382 (58.1) |
| Diagnosis of COVID-19 | |
| Yes | 1 (0.2) |
| No | 637 (96.8) |
| Unknown | 20 (3.0) |
| Close contact with patient with COVID-19 | |
| Yes | 48 (7.3) |
| No | 561 (85.3) |
| Unknown | 49 (7.4) |
| Worried aboutd | |
| Changed BC therapeutic regimen | 53 (5.5) |
| Delayed BC therapeutic regimen | 266 (27.5) |
| Suboptimal therapy for BC | 200 (20.7) |
| Infection of COVID-19 | 191 (19.8) |
| Discrimination | 21 (2.2) |
| Other | 101 (10.4) |
| None | 134 (13.9) |
Abbreviations: BC = breast cancer; COVID-19 = coronavirus disease 2019; CVC = central venous catheter; HER2 = human epidermal growth factor receptor 2; TNBC = triple negative breast cancer.
Percentages are weighted to account for the sample size (n = 658).
Percentages are weighted to account for the total responder size (n = 510).
Percentages are weighted to the size of the group of patients recommended for anti-cancer therapy (n = 474).
Percentages are weighted to account for the size of the total responder group (n = 966).
PRO Measurements of Patients With BC
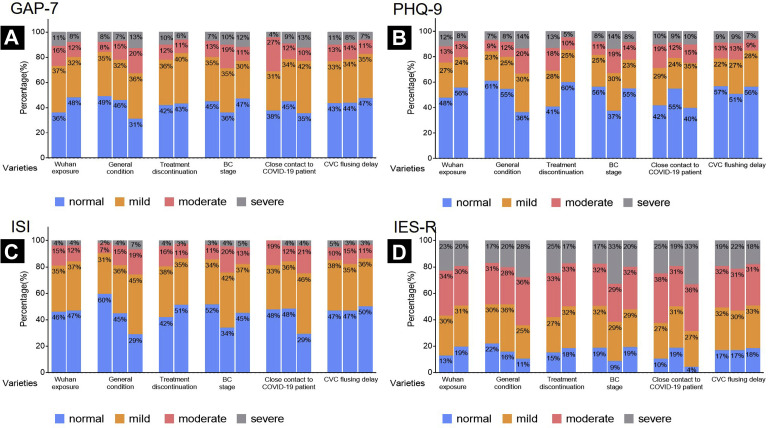
The mean scores were 6.01 ± 5.35 and 5.80 ± 5.66 for the GAD-7 and PHQ-9, respectively (Table 2 ). There were 34.0%, 13.3%, and 8.9% patients categorized into the mild, moderate, and severe anxiety categories, respectively. There were 25.2%, 12.8%, and 9.3% patients who reported mild, moderate, and severe depression, respectively. The mean scores were 8.66 ± 6.29 and 28.17 ± 18.23 for the ISI and IES-R, respectively (Table 2). There were 36.2%, 12.9%, and 4.0% patients, respectively, who reported mild, moderate, and severe insomnia. There were 30.7%, 31.5%, and 20.8% patients who described mild, moderate, and severe distress symptoms. Subscale scores of IES-R were calculated to evaluate the intrusion, avoidance, and hyperarousal status (Table 2).
Table 2.
Overview of the Scores on the 4 Scales Including 3 Subscales of IES-R Among Patients With BC
| Scales | Mean ± SD | Min, Max | Median | IQR |
|---|---|---|---|---|
| GAD-7 | 6.01 ± 5.35 | 0, 21 | 5 | 1-9 |
| PHQ-9 | 5.80 ± 5.66 | 0, 27 | 4 | 1-9 |
| ISI | 8.66 ± 6.29 | 0, 28 | 8 | 4-13 |
| IES-R total | 28.17 ± 18.23 | 0, 88 | 27 | 15-41 |
| Intrusion | 10.41 ± 6.81 | 0, 32 | 10 | 6-15 |
| Avoidance | 10.28 ± 6.94 | 0, 32 | 10 | 5-15 |
| Hyperarousal | 7.47 ± 5.35 | 0, 24 | 7 | 3-11 |
Abbreviations: BC = breast cancer; GAD-7 = Generalized Anxiety Disorder Questionnaire; IES-R = Impact of Events Scale-Revised; IQR = interquartile range; ISI = Insomnia Severity Index; PHQ-9 = Patient Health Questionnaire; SD = standard deviation.
Patients with Wuhan exposure, poor general condition by self-identification, treatment discontinuation, and who had metastatic BC were more likely to report experiencing severe symptoms of anxiety, depression, insomnia, and distress (Table 3 ; Supplemental Table 1 and Supplemental Figure 1 in the online version). Patients with BC with Wuhan exposure (P = .001), poor general condition by self-identification (P < .001), treatment discontinuation (P < .001), metastatic BC (P = .018), CVC flushing delay exceeding 4 weeks (P = .002), and BC diagnosis within 1 year (P = .029) were found to have an association with symptoms of anxiety. In addition, patients with Wuhan exposure (P = .010), poor general physical condition (P < .001), treatment discontinuation (P < .001), and metastatic BC (P < .001), close contact to a patient with COVID-19 (P = .027), CVC flushing delay exceeding 4 weeks (P = .004), and BC diagnosis within 1 year (P = .034) tended to have an association with symptoms of depression. The patients with BC who had poor general condition (P < .001), treatment discontinuation (P = .031), and metastatic BC (P < .001) were more likely to have severe insomnia. Furthermore, patients with Wuhan exposure (P = .026) and who had poor general condition (P < .001), treatment discontinuation (P = .031), metastatic BC (P = .004), and close contact with a patient with COVID-19 (P = .004) had a higher risk of distress during the outbreak.
Table 3.
Severity Categories of Anxiety, Depression, Insomnia, and Distress in Patients With BC
| Severity Category | Total, N (%) | Wuhan Exposure |
General Condition by Self-identification |
Treatment Discontinuationa |
BC Clinical Stage |
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| N (%) |
P Value | N (%) |
P Value | N (%) |
P Value | N (%) |
P Value | ||||||||
| Yes | No | Well | Average | Poor | Yes | No | Early | Metastatic | N/A | ||||||
| GAD-7, anxiety symptoms | |||||||||||||||
| Normal | 287 (43.6) | 90 (36.4) | 197 (47.9) | .001 | 133 (49.4) | 104 (45.8) | 50 (30.9) | <.001 | 119 (41.6) | 80 (42.5) | <.001 | 175 (44.7) | 41 (35.7) | 71 (47.0) | .018 |
| Mild | 224 (34.0) | 91 (36.8) | 133 (32.4) | 93 (34.6) | 73 (32.2) | 58 (35.8) | 103 (36.0) | 75 (39.9) | 139 (35.4) | 40 (34.8) | 45 (29.8) | ||||
| Moderate | 88 (13.4) | 39 (15.8) | 49 (11.9) | 22 (8.2) | 34 (15.0) | 32 (19.8) | 36 (12.6) | 21 (11.2) | 50 (12.8) | 22 (19.1) | 16 (10.6) | ||||
| Severe | 59 (9.0) | 27 (11.0) | 32 (7.8) | 21 (7.8) | 16 (7.0) | 22 (13.6) | 28 (9.8) | 12 (6.4) | 28 (7.1) | 12 (10.4) | 19 (12.6) | ||||
| PHQ-9, depression symptoms | |||||||||||||||
| Normal | 347 (52.7) | 118 (47.8) | 229 (55.7) | .010 | 164 (61.0) | 124 (54.6) | 59 (36.4) | <.001 | 89 (40.7) | 153 (60.0) | <.001 | 221 (56.4) | 43 (37.4) | 83 (55.0) | <.001 |
| Mild | 166 (25.2) | 68 (27.5) | 98 (23.8) | 60 (22.3) | 57 (25.1) | 49 (30.2) | 62 (28.3) | 65 (25.5) | 98 (25.0) | 34 (29.6) | 34 (22.5) | ||||
| Moderate | 84 (12.8) | 32 (13.0) | 52 (12.7) | 25 (9.3) | 27 (11.9) | 32 (19.8) | 39 (17.8) | 25 (9.8) | 41 (10.5) | 22 (19.1) | 21 (13.9) | ||||
| Severe | 61 (9.3) | 29 (11.7) | 32 (7.8) | 20 (7.4) | 19 (8.4) | 22 (13.6) | 29 (13.2) | 12 (4.7) | 32 (8.1) | 16 (13.9) | 13 (8.6) | ||||
| ISI, insomnia symptoms | |||||||||||||||
| Normal | 309 (47.0) | 114 (46.2) | 195 (47.4) | .096 | 160 (59.5) | 102 (44.9) | 47 (29.0) | <.001 | 92 (42.0) | 131 (51.4) | .031 | 202 (51.5) | 39 (33.9) | 68 (45.0) | <.001 |
| Mild | 238 (36.2) | 86 (34.8) | 152 (37.0) | 83 (30.9) | 82 (36.1) | 73 (45.1) | 84 (38.4) | 89 (34.9) | 134 (34.2) | 48 (41.7) | 56 (37.1) | ||||
| Moderate | 85 (12.9) | 36 (14.6) | 49 (11.9) | 20 (7.4) | 34 (15.0) | 31 (19.1) | 34 (15.5) | 28 (11.0) | 43 (11.0) | 23 (20.0) | 19 (12.6) | ||||
| Severe | 26 (3.9) | 11 (4.4) | 15 (3.7) | 6 (2.2) | 9 (4.0) | 11 (6.8) | 9 (4.1) | 7 (2.7) | 13 (3.3) | 5 (4.4) | 8 (5.3) | ||||
| IES-R, distress symptoms | |||||||||||||||
| Normal | 112 (17.0) | 32 (13.0) | 80 (19.5) | .026 | 59 (21.9) | 36 (15.9) | 17 (10.5) | <.001 | 33 (15.1) | 47 (18.4) | .031 | 73 (18.6) | 10 (8.7) | 29 (19.2) | .004 |
| Mild | 202 (30.7) | 74 (30.0) | 128 (31.1) | 80 (29.8) | 81 (35.7) | 41 (25.3) | 59 (26.9) | 81 (31.8) | 125 (31.9) | 34 (29.6) | 43 (28.5) | ||||
| Moderate | 207 (31.5) | 84 (34.0) | 123 (29.9) | 84 (31.2) | 64 (28.2) | 59 (36.4) | 73 (33.3) | 83 (32.5) | 125 (31.9) | 33 (28.7) | 49 (32.4) | ||||
| Severe | 137 (20.8) | 57 (23.0) | 80 (19.5) | 46 (17.1) | 46 (20.2) | 45 (27.8) | 54 (24.7) | 44 (17.3) | 69 (17.6) | 38 (33.0) | 30 (19.9) | ||||
P value was calculated using the nonparametric Wilcoxon rank-sum test and Kruskal-Wallis test.
Abbreviation: BC = breast cancer; GAD-7 = Generalized Anxiety Disorder Questionnaire; IES-R = Impact of Events Scale-Revised; ISI = Insomnia Severity Index; N/A = Not provided or not available; PHQ-9 = Patient Health Questionnaire.
Total size is the patients who were recommended for anti-cancer treatment during COVID-19 period: n = 474.
Supplemental Figure 1.
Stacked bar Plots to Identify Severity of Measurements and Associated Factors for Anxiety (A), Depression (B), Insomnia (C), and Distress (D) Symptoms Among Patients With BC in the Center of COVID-19 in China. (Interpretations: Wuhan Exposure: Yes vs. No; General Condition by Self-Identification: Well vs. Average vs. Poor; Treatment Discontinuation: Yes vs. No; Breast Cancer Stage: Early vs. Metastatic vs. N/A; Close Contact With Patient With COVID-19: Yes vs. No vs. N/A; CVC Flushing Delay: Delay vs. No Delay vs. No CVC)
Abbreviations: BC = breast cancer; CVC = central venous catheter; COVID-19 = coronavirus disease 2019.
Independent Risk Factors for Specific PRO Measurement
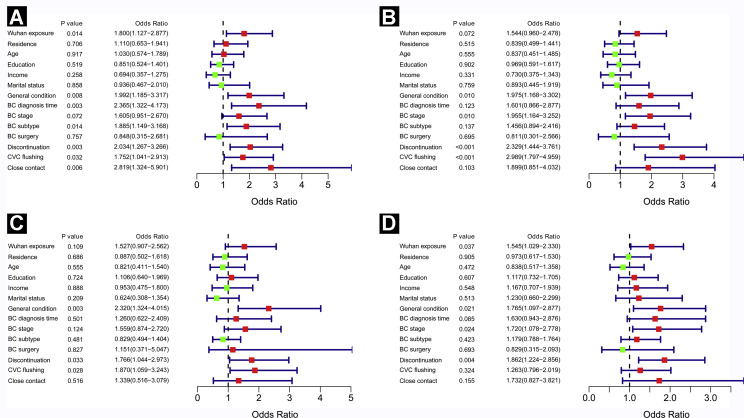
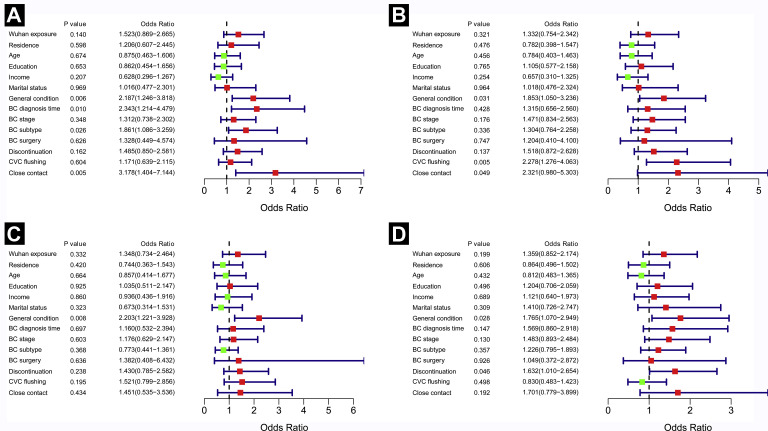
Univariable logistic regression analysis showed that patients with Wuhan exposure (P = .014), poor general condition by self-identification (P = .008), less than 4 months after BC diagnosis (P = .003), aggressive BC molecular subtypes (P = .014), treatment discontinuation (P = .003), CVC flushing delay exceeding 4 weeks (P = .032), and close contact with a patient with COVID-19 (P = .006) were more likely to report moderate and severe anxiety symptoms (see Supplemental Figure 2A in the online version). In addition, patients with BC with poor generation condition (P = .010), metastatic BC (P = .010), treatment discontinuation (P < .001), and CVC flushing delay exceeding 4 weeks (P < .001) had a higher risk of falling into moderate or severe depression (see Supplemental Figure 2B in the online version). Furthermore, patients with poor general condition (P = .003), treatment discontinuation (P = .033), or CVC flushing delay exceeding 4 weeks (P = .028) were more likely to have moderate or severe insomnia (see Supplemental Figure 2C in the online version). In addition, patients with BC with Wuhan exposure (P = .037), poor general condition (P = .021), metastatic BC (P = .024), and with treatment discontinuation (P = .004) might harbor a greater chance to present with distress (see Supplemental Figure 2D in the online version). With multivariate logistic regression analysis, poor general condition (P = .006), less than 4 months after BC diagnosis (P = .010), aggressive BC molecular subtypes (P = .026), and close contact with patients with COVID-19 (P = .005) were independent affecting risk factors for moderate or severe anxiety (Figure 2A ). In addition, poor general condition (P = .031) and CVC flushing interval exceeding 4 weeks (P = .005) were shown as independently associated factors with moderate or severe depression based on multivariate logistic regression analysis (Figure 2B). In terms of moderate or severe insomnia, poor general condition (P = .008) was the only independent affecting factor (Figure 2C). Poor physical condition (P = .028) and treatment discontinuation (P = .046) were independent risk markers for distress based on the multivariate analysis (Figure 2D).
Supplemental Figure 2.
Forest Plots to Identify Independent Affecting Factors for Anxiety (A), Depression (B), Insomnia (C), and Distress (D) Symptoms Among Patients With BC in the Center of COVID-19 in China Using Univariable Logistic Regression Analysis. (Interpretations: Wuhan Exposure: Yes vs. No; Residence: Urban vs. Rural; Age: ≥ 55 years Old vs. ≤ 54 years Old; Education: High School or More vs. Middle School or less; Income: ≤ $15,000 per Year vs. >$15,000 per Year; Marital Status: Single (including Widowed/Divorced) vs. Married; General Condition by Self-Identification: Poor vs. Well/Average; BC Diagnosis Time: ≤ 1 Year vs. > 1 year; BC Stage: Metastatic vs. Early; BC Subtype: TNBC/HER2 vs. Luminal; BC Surgery History: Yes vs. No; Treatment Discontinuation: Yes vs. No; CVC Flushing: Interval Exceeding 4 weeks vs. Interval Within 4 Weeks; Close Contact: Close Contact With Patient With COVID-19 vs. No Close Contact With Patient With COVID-19.)
Abbreviations: BC = breast cancer; COVID-19 = coronavirus disease 2019; CVC = central venous catheter; HER2 = human epidermal growth factor receptor 2; TNBC = triple negative breast cancer.
Figure 2.
Forest Plots to Identify Independent Affecting Factors for Anxiety (A), Depression (B), Insomnia (C), and Distress (D) Symptoms Among Patients With BC in the Center of COVID-19 in China Using Multivariable Logistic Regression Analysis. (Interpretations: Wuhan Exposure: Yes vs. No; Residence: Urban vs. Rural; Age: ≥ 55 years Old vs. ≤ 54 years Old; Education: High School or More vs. Middle School or less; Income: ≤ $15,000 per Year vs. > $15,000 per Year; Marital Status: Single (including Widowed/Divorced) vs. Married; General Condition by Self-Identification: Poor vs. Well/Average; BC Diagnosis Time: ≤ 1 Year vs. > 1 year; BC Stage: Metastatic vs. Early; BC Subtype: TNBC/HER2 vs. Luminal; BC Surgery History: Yes vs. No; Treatment Discontinuation: Yes vs. No; CVC Flushing: Interval Exceeding 4 weeks vs. Interval Within 4 Weeks; Close Contact: Close Contact With Patient With COVID-19 vs. No Close Contact With Patient With COVID-19)
Abbreviations: BC = breast cancer; COVID-19 = coronavirus disease 2019; CVC = central venous catheter; HER2 = human epidermal growth factor receptor 2; TNBC = triple negative breast cancer.
Discussion
Wuhan, a metropolis of 11 million residents in central China’s Hubei Province, became the epicenter of COVID-19 in January 2020. Rapidly rising numbers of infected cases put the local health care system under tremendous stress,3 occupying and affecting the medical needs for patients with non-COVID-19, especially for patients with cancer. In addition, patients with cancer were exposed to a higher risk of infection with COVID-19, and experienced worse outcomes after infection during the COVID-19 epidemic.6 , 7 Under this unique circumstance, patients with cancer faced COVID-19 infections and interruption of cancer treatment, resulting in significant mental stress. In this study, we investigated PROs in patients with BC in the epicenter at the peak timepoint of the COVID-19 outbreak.
We found a wide range of abnormal quality of life metrics that patients with BC experienced, including stress, anxiety, fear, depression, and distress. Approximate 10% of patients with BC showed severe depression and anxiety. Over one-fifth of patients with BC presented severe distress symptoms during the COVID-19 outbreak. The scores in our study were significantly higher than patients with BC under normal conditions in previous studies, which showed about only 3.5% patients reported severe anxiety and depression,17, 18, 19, 20, 21 indicating an additional increase of mental stress on the patients with BC by the COVID-19 crisis.
We identified factors affecting PROs of the patients with BC during the COVID-19 pandemic that may help to make effective measures to reduce stress for these patients. Based on our results, living in Wuhan, poor general condition by self-identification, shorter duration after BC diagnosis, aggressive BC molecular subtypes, metastatic BC clinical stage, treatment discontinuation, CVC flushing delay, or close contact with patients with COVID-19 are associated risk factors for poorer psychological status. Notably, poor general condition, namely with comorbidities, was the only overlapping independent affecting factor for all 4 PRO metrics. Several studies have found that patients with BC with comorbidities have worse outcome than patients without comorbidities under normal conditions.22 , 23 In addition, the death rate among patients with COVID-19 with one or more comorbidities was much higher than those without comorbidities.24, 25, 26, 27 Therefore, patients with BC with comorbidities faced more stress, which can affect their mental health under this unique circumstance, which we demonstrated. Thus more attention should be paid and some effective measures should be taken to reduce the stress during the COVID-19 crisis among patients with comorbidities.
During the outbreak, changes to usual clinical practice for patients with BC were necessary.28, 29, 30, 31, 32 Notably, the efficacy of compromised anti-cancer therapeutic regimens (519/966; 53.7%) was the main concern among these patients with BC, followed by the fear about infection of COVID-19 (191/966; 19.8%). A number of modifications to standard treatment paradigms were implemented. For example, during the outbreak, capecitabine was preferentially prescribed for patients with triple negative BC. Pyrotinib, an oral pan-HER receptor tyrosine kinase inhibitor, which was approved in China, was recommended for human epidermal growth factor receptor 2 (HER2)-positive patients with BC. Several months of neoadjuvant endocrine therapy and delay in surgery was recommended for hormone receptor-positive patients with early BC. In terms of CVC maintenance delay, we opened a special clinic to care for CVC weekly. In addition, we rapidly established and expanded telemedicine efforts through social media, offering outpatient service and prescription or medical consulting. Optimization of physician-to-patient communication was critical for shared decision-making of therapeutic changes.
There are several limitations of our study. There was a possible selection bias for the patients enrolled in this study. Those patients without smartphones or not in the local Wechat groups may not be involved in our survey. In addition, this is a cross-sectional observational study; we need a control cohort to compare the differences of psychological status under different situations and to confirm the effect of COVID-19 in patients with BC. Furthermore, our population was diverse and heterogeneous in terms of disease states, which limits the power to each relevant clinical subgroup.
Conclusions
In summary, our study indicates that the psychological status of patients with BC deserves more attention during the COVID-19 pandemic. Patients with BC are likely to experience adverse mental well-being. Effective measures should be taken to minimize mental health issues and to provide psychological support.
Clinical Practice Points
-
•
During the COVID-19 outbreak in China, fear about COVID-19, together with worry about progression of cancer, causes strong emotional stress in patients with cancer. High rates of anxiety, depression, distress, and insomnia were observed in patients with breast cancer during the COVID-19 outbreak.
-
•
Special attention should be paid to the psychological status of patients with breast cancer, especially those with poor general condition, treatment discontinuation, aggressive molecular subtypes, and metastatic breast cancer.
Disclosure
The authors have stated that they have no conflicts of interest.
Acknowledgments
This research was supported by the grants from the Fundamental Research Funds for the Central Universities (2042019kf0229), the Science and Technology Major Project of Hubei Province (Next-Generation AI Technologies) (2019AEA170), Medical Science Advancement Program of Wuhan University (TFLC2018001), the National Key R&D Program of China (2018YFC1314600). The authors would like to thank multiple medical centers in Hubei for the distribution and assessment of the questionnaires.
Footnotes
L.J. and C.A.S.-M. contributed equally to this work as first authors.
Supplemental table and figures accompanying this article can be found in the online version at https://doi.org/10.1016/j.clbc.2020.06.003.
Supplemental Data
Supplemental Table 1.
Severity Categories of Anxiety, Depression, Insomnia, and Distress in Patients With BC
| Severity Category | Total, N (%) | Marital Status |
Close Contact With Patient With COVID-19 |
CVC Flushing |
BC Diagnosis Time |
Annual Income |
||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| N (%) |
P Value | N (%) |
P Value | N (%) |
P Value | N (%) |
P Value | N (%) |
P Value | |||||||||
| Married | Singlea | Yes | No | N/A | Delay Over 4 Weeks | Delay Less Than 4 Weeks | No CVC | ≤1 Year | >1 Year | ≤$15,000 | >$15,000 | |||||||
| GAD-7, anxiety symptoms | ||||||||||||||||||
| Normal | 287 (43.6) | 255 (43.7) | 32 (43.2) | .881 | 18 (37.5) | 252 (44.8) | 17 (35.4) | .079 | 61 (43.4) | 45 (43.7) | 181 (47.4) | .002 | 123 (41.6) | 164 (45.3) | .029 | 243 (43.9) | 44 (42.3) | .327 |
| Mild | 224 (34.0) | 199 (34.1) | 25 (33.8) | 15 (31.2) | 189 (33.6) | 20 (41.7) | 52 (33.3) | 38 (34.4) | 134 (35.1) | 99 (33.4) | 125 (34.5) | 180 (32.4) | 44 (42.3) | |||||
| Moderate | 88 (13.4) | 78 (13.3) | 10 (13.5) | 13 (27.1) | 70 (12.5) | 5 (10.4) | 26 (13.2) | 20 (13.5) | 42 (11.0) | 39 (13.2) | 49 (13.6) | 79 (14.3) | 9 (8.7) | |||||
| Severe | 59 (9.0) | 52 (8.9) | 7 (9.5) | 2 (4.2) | 51 (9.1) | 6 (12.5) | 25 (10.1) | 9 (8.4) | 25 (6.5) | 35 (11.8) | 24 (6.6) | 52 (9.4) | 7 (6.7) | |||||
| PHQ-9, depression symptoms | ||||||||||||||||||
| Normal | 347 (52.7) | 314 (53.8) | 33 (44.6) | .205 | 20 (41.7) | 308 (54.8) | 19 (39.6) | .027 | 80 (56.6) | 52 (50.7) | 215 (56.3) | .004 | 150 (50.7) | 197 (54.4) | .034 | 289 (52.2) | 58 (55.8) | .393 |
| Mild | 166 (25.2) | 146 (25.0) | 20 (27.0) | 14 (29.2) | 135 (24.0) | 17 (35.4) | 26 (21.9) | 31 (27.0) | 109 (28.5) | 72 (24.3) | 94 (26.0) | 136 (24.5) | 30 (28.8) | |||||
| Moderate | 84 (12.8) | 72 (12.3) | 12 (16.2) | 9 (18.7) | 68 (12.1) | 7 (14.6) | 36 (12.7) | 15 (12.8) | 33 (8.6) | 40 (13.5) | 44 (12.1) | 74 (13.4) | 10 (9.6) | |||||
| Severe | 61 (9.3) | 52 (8.9) | 9 (12.2) | 5 (10.4) | 51 (9.1) | 5 (10.4) | 22 (8.8) | 14 (9.5) | 25 (6.6) | 34 (11.5) | 27 (7.5) | 55 (9.9) | 6 (5.8) | |||||
| ISI, insomnia symptoms | ||||||||||||||||||
| Normal | 309 (47.0) | 278 (47.6) | 31 (41.9) | .193 | 23 (47.9) | 272 (48.4) | 14 (29.2) | .092 | 67 (46.9) | 51 (47.0) | 191 (50.0) | .112 | 134 (45.3) | 175 (48.3) | .220 | 252 (45.5) | 57 (54.8) | .099 |
| Mild | 238 (36.2) | 214 (36.6) | 24 (32.4) | 16 (33.3) | 200 (35.6) | 22 (45.8) | 55 (38.2) | 45 (35.1) | 138 (36.1) | 111 (37.5) | 127 (35.1) | 205 (37.0) | 33 (31.7) | |||||
| Moderate | 85 (12.9) | 73 (12.5) | 12 (16.2) | 9 (18.8) | 66 (11.7) | 10 (20.8) | 34 (9.6) | 11 (14.7) | 40 (10.5) | 41 (13.8) | 44 (12.2) | 73 (13.2) | 12 (11.6) | |||||
| Severe | 26 (3.9 | 19 (3.3) | 7 (9.5) | 0 (0) | 24 (4.3) | 2 (4.2) | 8 (5.3) | 5 (3.2) | 13 (3.4) | 10 (3.4) | 16 (4.4) | 24 (4.3) | 2 (1.9) | |||||
| IES-R, distress symptoms | ||||||||||||||||||
| Normal | 112 (17.0) | 99 (17.0) | 13 (17.5) | .920 | 5 (10.4) | 105 (18.7) | 2 (4.2) | .004 | 31 (17.1) | 11 (17.0) | 70 (18.3) | .056 | 38 (12.8) | 74 (20.4) | .177 | 92 (16.6) | 20 (19.2) | .243 |
| Mild | 202 (30.7) | 179 (30.6) | 23 (31.1) | 13 (27.1) | 176 (31.3) | 13 (27.1) | 41 (32.0) | 37 (30.0) | 124 (32.5) | 96 (32.4) | 106 (29.3) | 170 (30.7) | 32 (30.8) | |||||
| Moderate | 207 (31.5) | 188 (32.2) | 19 (25.7) | 18 (37.5) | 172 (30.6) | 17 (35.4) | 44 (31.6) | 43 (31.4) | 120 (31.4) | 100 (33.8) | 107 (29.6) | 171 (30.9) | 36 (34.6) | |||||
| Severe | 137 (20.8) | 118 (20.2) | 19 (25.7) | 12 (25.0) | 109 (19.4) | 16 (33.3) | 48 (19.3) | 21 (21.6) | 68 (17.8) | 62 (21.0) | 75 (20.7) | 121 (21.8) | 16 (15.4) | |||||
| Severity category | Total, N (%) | Residence |
Age, y |
Education |
History of BC Surgery |
BC Molecular Subtype |
|||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| N (%) |
P Value | N (%) |
P Value | N (%) |
P Value | N (%) |
P Value | N (%) |
P Value | ||||||||
| Urban | Rural | ≤55 | >55 | Middle School or Less | High School or Higher | Yes | No | TNBC and HER2 | Luminal | N/A | |||||||
| GAD-7, anxiety symptoms | |||||||||||||||||
| Normal | 287 (43.6) | 212 (43.7) | 75 (43.3) | .576 | 222 (43.0) | 65 (45.8) | .645 | 99 (43.4) | 188 (43.7) | .937 | 274 (43.6) | 13 (43.3) | .387 | 134 (41.4) | 75 (42.4) | 78 (49.4) | .126 |
| Mild | 224 (34.0) | 163 (33.6) | 61 (35.3) | 183 (35.5) | 41 (28.9) | 76 (33.3) | 148 (34.4) | 216 (34.4) | 8 (26.7) | 103 (31.9) | 74 (41.8) | 47 (29.7) | |||||
| Moderate | 88 (13.4) | 66 (13.6) | 22 (12.7) | 67 (13.0) | 21 (14.8) | 30 (13.2) | 58 (13.5) | 85 (13.6) | 3 (10.0) | 48 (14.9) | 19 (10.7) | 21 (13.3) | |||||
| Severe | 59 (9.0) | 44 (9.1) | 15 (8.7) | 44 (8.5) | 15 (10.5) | 23 (10.1) | 36 (8.4) | 53 (8.4) | 6 (20.0) | 38 (11.8) | 9 (5.1) | 12 (7.6) | |||||
| PHQ-9, depression symptoms | |||||||||||||||||
| Normal | 347 (52.7) | 258 (53.2) | 89 (51.4) | .822 | 272 (52.7) | 75 (52.8) | .968 | 129 (56.6) | 218 (50.7) | .135 | 332 (52.9) | 15 (50.0) | .288 | 163 (50.4) | 94 (53.1) | 90 (57.0) | .072 |
| Mild | 166 (25.2) | 121 (25.0) | 45 (26.0) | 130 (25.2) | 36 (25.3) | 50 (21.9) | 116 (27.0) | 162 (25.8) | 4 (13.3) | 81 (25.1) | 50 (28.2) | 35 (22.2) | |||||
| Moderate | 84 (12.8) | 55 (11.3) | 29 (16.8) | 71 (13.8) | 13 (9.2) | 29 (12.7) | 55 (12.8) | 79 (12.6) | 5 (16.7) | 40 (12.4) | 24 (13.6) | 20 (12.6) | |||||
| Severe | 61 (9.3) | 51 (10.5) | 10 (5.8) | 43 (8.3) | 18 (12.7) | 20 (8.8) | 41 (9.5) | 55 (8.7) | 6 (20.0) | 39 (12.1) | 9 (5.1) | 13 (8.2) | |||||
| ISI, insomnia symptoms | |||||||||||||||||
| Normal | 309 (47.0) | 229 (47.2) | 80 (46.2) | .866 | 238 (46.1) | 71 (50.0) | .351 | 107 (46.9) | 202 (47.0) | .357 | 296 (47.1) | 13 (43.4) | .334 | 150 (46.9) | 79 (44.6) | 80 (50.6) | .173 |
| Mild | 238 (36.2) | 175 (36.1) | 63 (36.4) | 190 (36.8) | 48 (33.8) | 87 (38.2) | 151 (35.1) | 226 (36.0) | 12 (40.0) | 114 (35.6) | 66 (37.3) | 58 (36.7) | |||||
| Moderate | 85 (12.9) | 65 (13.4) | 20 (11.6) | 69 (13.4) | 16 (11.3) | 22 (9.6) | 63 (14.7) | 81 (12.9) | 4 (13.3) | 41 (12.8) | 26 (14.7) | 15 (9.5) | |||||
| Severe | 26 (3.9) | 16 (3.3) | 10 (5.8) | 19 (3.7) | 7 (4.9) | 12 (5.3) | 14 (3.2) | 25 (4.0) | 1 (3.3) | 15 (4.7) | 6 (3.4) | 5 (3.2) | |||||
| IES-R, distress symptoms | |||||||||||||||||
| Normal | 112 (17.0) | 84 (17.3) | 28 (16.2) | .484 | 78 (15.1) | 34 (23.9) | .210 | 39 (17.1) | 73 (17.0) | .698 | 109 (17.4) | 3 (10.0) | .099 | 50 (15.5) | 30 (16.9) | 32 (20.3) | .117 |
| Mild | 202 (30.7) | 151 (31.1) | 51 (29.5) | 164 (31.8) | 38 (26.8) | 73 (32.0) | 129 (30.0) | 195 (31.0) | 7 (23.4) | 96 (29.7) | 55 (31.1) | 51 (32.3) | |||||
| Moderate | 207 (31.5) | 153 (31.6) | 54 (31.2) | 166 (32.2) | 41 (28.9) | 72 (31.6) | 135 (31.4) | 197 (31.4) | 10 (33.3) | 100 (31.0) | 55 (31.1) | 52 (32.9) | |||||
| Severe | 137 (20.8) | 97 (20.0) | 40 (23.1) | 108 (20.9) | 29 (20.4) | 44 (19.3) | 93 (21.6) | 127 (20.2) | 10 (33.3) | 77 (23.8) | 37 (20.9) | 23 (14.5) | |||||
P value was calculated using the nonparametric Wilcoxon signed-rank test and Kruskal-Wallis test.
Abbreviations: BC = breast cancer; COVID-19 = coronavirus disease 2019; CVC = central venous catheter; GAD-7 = Generalized Anxiety Disorder Questionnaire; HER2 = human epidermal growth factor receptor 2; IES-R = Impact of Events Scale-Revised; ISI = Insomnia Severity Index; N/A = Not provided or not available; PHQ-9 = Patient Health Questionnaire; TNBC = triple negative breast cancer.
Single category included widowed and divorced participants.
References
- 1.Zhu N., Zhang D., Wang W., et al. China Novel Coronavirus Investigating and Research Team. A novel coronavirus from patients with pneumonia in China, 2019. N Engl J Med. 2020;382:727–733. doi: 10.1056/NEJMoa2001017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Guan W.J., Ni Z.Y., Hu Y., et al. China Medical Treatment Expert Group for Covid-19.. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med. 2020;382:1708–1720. doi: 10.1056/NEJMoa2002032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ji Y., Ma Z., Peppelenbosch M.P., Pan Q. Potential association between COVID-19 mortality and health-care resource availability. Lancet Glob Health. 2020;8:e480. doi: 10.1016/S2214-109X(20)30068-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Zhou G., Chen S., Chen Z. Back to the spring of Wuhan: facts and hope of COVID-19 outbreak. Front Med. 2020;14:113–116. doi: 10.1007/s11684-020-0758-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Chinazzi M., Davis J.T., Ajelli M., et al. The effect of travel restrictions on the spread of the 2019 novel coronavirus (COVID-19) outbreak. Science. 2020;368:395–400. doi: 10.1126/science.aba9757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Liang W., Guan W., Chen R., et al. Cancer patients in SARS-CoV-2 infection: a nationwide analysis in China. Lancet Oncol. 2020;21:335–337. doi: 10.1016/S1470-2045(20)30096-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Yu J., Ouyang W., Chua M.L.K., Xie C. SARS-CoV-2 transmission in patients with cancer at a tertiary care hospital in Wuhan, China. JAMA Oncol 2020 Mar 25;e200980. https://doi.org/10.1001/jamaoncol.2020.0980 Online ahead of print. [DOI] [PMC free article] [PubMed]
- 8.Cortiula F., Pettke A., Bartoletti M., Puglisi F., Helleday T. Managing COVID-19 in the oncology clinic and avoiding the distraction effect. Ann Oncol. 2020;31:553–555. doi: 10.1016/j.annonc.2020.03.286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Burki T.K. Cancer care in the time of COVID-19. Lancet Oncol. 2020;21:628. doi: 10.1016/S1470-2045(20)30201-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Fan L., Strasser-Weippl K., Li J.J., et al. Breast cancer in China. Lancet Oncol. 2014;15:e279–e289. doi: 10.1016/S1470-2045(13)70567-9. [DOI] [PubMed] [Google Scholar]
- 11.Abdollahi A., Panahipour H., Hosseinian S., Allen K.A. The effects of perceived stress on hope in women with breast cancer and the role of psychological hardiness. Psychooncology. 2019;28:1477–1482. doi: 10.1002/pon.5102. [DOI] [PubMed] [Google Scholar]
- 12.Carreira H., Williams R., Müller M., Harewood R., Stanway S., Bhaskaran K. Associations between breast cancer survivorship and adverse mental health outcomes: a systematic review. J Natl Cancer Inst. 2018;110:1311–1327. doi: 10.1093/jnci/djy177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Zhang Y.L., Liang W., Chen Z.M., et al. Validity and reliability of Patient Health Questionnaire-9 and Patient Health Questionnaire-2 to screen for depression among college students in China. Asia Pac Psychiatry. 2013;5:268–275. doi: 10.1111/appy.12103. [DOI] [PubMed] [Google Scholar]
- 14.He X.Y., Li C., Qian J., Cui H.S., Wu W. Reliability and validity of a generalized anxiety disorder scale in general hospital outpatients. Shanghai Arch Psychiatry. 2010;22:200–203. [Google Scholar]
- 15.Yu D.S.F. Insomnia Severity Index: psychometric properties with Chinese community-dwelling older people. J Adv Nurs. 2010;66:2350–2359. doi: 10.1111/j.1365-2648.2010.05394.x. [DOI] [PubMed] [Google Scholar]
- 16.Wu K.K., Chan K.S. The development of the Chinese version of Impact of Event Scale–Revised (CIES-R) Soc Psychiatry Psychiatr Epidemiol. 2003;38:94–98. doi: 10.1007/s00127-003-0611-x. [DOI] [PubMed] [Google Scholar]
- 17.Lan B., Jiang S., Li T., Sun X., Ma F. Depression, anxiety, and their associated factors among Chinese early breast cancer in women under 35 years of age: a cross sectional study. Curr Probl Cancer. 2020:100558. doi: 10.1016/j.currproblcancer.2020.100558. [DOI] [PubMed] [Google Scholar]
- 18.Kaster T.S., Sommer J.L., Mota N., Sareen J., El-Gabalawy R. Post-traumatic stress and cancer: findings from a cross-sectional nationally representative sample. J Anxiety Disord. 2019;65:11–18. doi: 10.1016/j.janxdis.2019.04.004. [DOI] [PubMed] [Google Scholar]
- 19.Oliveri S., Arnaboldi P., Pizzoli S.F.M., et al. PTSD symptom clusters associated with short- and long-term adjustment in early diagnosed breast cancer patients. Ecancermedicalscience. 2019;13:917. doi: 10.3332/ecancer.2019.917. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Fleming L., Randell K., Stewart E., et al. Insomnia in breast cancer: a prospective observational study. Sleep. 2019;42:zsy245. doi: 10.1093/sleep/zsy245. [DOI] [PubMed] [Google Scholar]
- 21.Tag Eldin E.S., Younis S.G., El Aziz L.M.A., Tag Eldin A., Erfan S.T. Evaluation of sleep pattern disorders in breast cancer patients receiving adjuvant treatment (chemotherapy and/or radiotherapy) using polysomnography. J BUON. 2019;24:529–534. [PubMed] [Google Scholar]
- 22.Kiderlen M., de Glas N.A., Bastiaannet E., et al. Impact of comorbidity on outcome of older breast cancer patients: a FOCUS cohort study. Breast Cancer Res Treat. 2014;145:185–192. doi: 10.1007/s10549-014-2917-7. [DOI] [PubMed] [Google Scholar]
- 23.Webster S., Lawn S., Chan R., Koczwara B. The role of comorbidity assessment in guiding treatment decision-making for women with early breast cancer: a systematic literature review. Support Care Cancer. 2020;28:1041–1050. doi: 10.1007/s00520-019-05218-w. [DOI] [PubMed] [Google Scholar]
- 24.Yang X., Yu Y., Xu J., et al. Clinical course and outcomes of critically ill patients with SARS-CoV-2 pneumonia in Wuhan, China: a single-centered, retrospective, observational study. Lancet Respir Med. 2020;8:475–481. doi: 10.1016/S2213-2600(20)30079-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Yang J., Zheng Y., Gou X., et al. Prevalence of comorbidities in the novel Wuhan coronavirus (COVID-19) infection: a systematic review and meta-analysis. Int J Infect Dis. 2020;94:91–95. doi: 10.1016/j.ijid.2020.03.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Wu C., Chen X., Cai Y., et al. Risk factors associated with acute respiratory distress syndrome and death in patients with coronavirus disease 2019 pneumonia in Wuhan, China. JAMA Intern Med 2020 Mar 13;e200994. https://doi.org/10.1001/jamainternmed.2020.0994 Online ahead of print. [DOI] [PMC free article] [PubMed]
- 27.Wang D., Hu B., Hu C., et al. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus-infected pneumonia in Wuhan, China. JAMA. 2020;323:1061–1069. doi: 10.1001/jama.2020.1585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Jazieh A.R., Al Hadab A., Al Olayan A., et al. Managing oncology services during a major coronavirus outbreak: lessons from the Saudi Arabia experience. JCO Glob Oncol. 2020;6:518–524. doi: 10.1200/GO.20.00063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Porzio G., Cortellini A., Bruera E., et al. Home care for cancer patients during COVID-19 pandemic: the “double triage” protocol. J Pain Symptom Manage 2020 Mar 31;S0885-3924(20)30172-X. https://doi.org/10.1016/j.jpainsymman.2020.03.021 Online ahead of print. [DOI] [PMC free article] [PubMed]
- 30.Ueda M., Martins R., Hendrie P.C., et al. Managing cancer care during the COVID-19 pandemic: agility and collaboration toward a common goal. J Natl Compr Canc Netw 2020 Mar 20;1-4. https://doi.org/10.6004/jnccn.2020.7560 Online ahead of print. [DOI] [PubMed]
- 31.Al-Shamsi H.O., Alhazzani W., Alhuraiji A., et al. A practical approach to the management of cancer patients during the novel coronavirus disease 2019 (COVID-19) pandemic: an international collaborative group. Oncologist 2020 Apr 3. https://doi.org/10.1634/theoncologist.2020-0213 Online ahead of print. [DOI] [PMC free article] [PubMed]
- 32.National University Cancer Institute of Singapore (NCIS) Workflow Team A segregated-team model to maintain cancer care during the COVID-19 outbreak at an academic center in Singapore. Ann Oncol 2020 Mar 31;S0923-7534(20)36410-3. https://doi.org/10.1016/j.annonc.2020.03.306 Online ahead of print. [DOI] [PMC free article] [PubMed]