Abstract
Background
Recently, a new coronavirus spreads rapidly throughout the countries and resulted in a worldwide epidemic. Interferons have direct antiviral and immunomodulatory effects. Antiviral effects may include inhibition of viral replication, protein synthesis, virus maturation, or virus release from infected cells. Previous studies have shown that some coronaviruses are susceptible to interferons. The aim of this study was to evaluate the therapeutic effects of IFN-β-1a administration in COVID-19.
Methods
In this prospective non-controlled trial, 20 patients included. They received IFN-β-1a at a dose of 44 µg subcutaneously every other day up to 10 days. All patients received conventional therapy including Hydroxychloroquine, and lopinavir/ritonavir. Demographic data, clinical symptoms, virological clearance, and imaging findings recorded during the study.
Results
The mean age of the patients was 58.55 ± 13.43 years. Fever resolved in all patients during first seven days. Although other symptoms decreased gradually. Virological clearance results showed a significant decrease within 10 days. Imaging studies showed significant recovery after 14-day period in all patients. The mean time of hospitalization was 16.8 ± 3.4 days. There were no deaths or significant adverse drug reactions in the 14-day period.
Conclusions
Our findings support the use of IFN-β-1a in combination with hydroxychloroquine and lopinavir/ritonavir in the management of COVID-19.
Clinical trial registration number: IRCT20151227025726N12.
Keywords: Interferon Beta-1a, COVID-19, Coronavirus, Pulmonary infection
1. Introduction
In late 2019, a new coronavirus that causes severe respiratory infections was identified. The virus spreads rapidly throughout the countries and resulted in a worldwide epidemic. This infection leads to multi organ failure, including acute respiratory distress syndrome (ARDS), acute cardiac injury, and shock. As of May 26, 2020, about 5,581,003 cases of COVID-19 were clinically confirmed and 347,516 deaths were reported [1]. In the absence of specific treatment for COVID-19, there is an immediate need to find alternative treatments to manage this pandemic. Several agents such as hydroxychloroquine, antiviral agents, corticosteroids, and immunomodulatory agents are being investigated for COVID-19 management [2], [3]. Pathophysiological studies have demonstrated the role of inflammatory mediators in COVID-19 pneumonia. It appears that imbalances between inflammatory and anti-inflammatory cytokines are the probable underlying mechanism [4], [5]. Hence, it is sensible to consider immunomodulatory agents for COVID-19 treatment. Among immunomodulatory agents, interferons (IFNs), which are proteins produced by certain cells in response to stimuli such as foreign cells (including tumor cells), bacteria, and viral antigens, play a dominant role [6]. They interact both with the IFN-producing cells and other cells through production of effector proteins [7]. There are three main types of IFNs, types I (alpha & beta), II (gamma), and III (lambda), which have direct antiviral and immunomodulatory effects [8]. Antiviral effects may include inhibition of viral replication, protein synthesis, virus maturation, or virus release from infected cells. Immunomodulatory effects may include the enhancement of macrophage, cytotoxic T cell, and natural killer cell activity [9], [10]. In addition, previous studies have shown that some coronaviruses, including avian infectious bronchitis virus, murine hepatitis virus, human coronavirus 229E, and SARS-CoV, are susceptible to type I IFN (IFN-β-1a) in vitro or in vivo [11]. IFN-α also showed immunomodulatory effects in response to virus infections however it is not easily available in the pharmaceutical market of our country. Therefore, we aimed to evaluate the therapeutic effects of IFN-β-1a administration in COVID-19.
2. Materials and methods
2.1. Setting
This study was a prospective non-controlled trial performed at Dr. Masih Daneshvari Hospital, Shahid Beheshti University of Medical Sciences, Tehran, Iran, in March 2020. This hospital is the main referral center for COVID-19 in Iran.
2.2. Patients
Patients were eligible for study inclusion if they were aged ≥18 years and had laboratory (reverse transcription polymerase chain reaction)-confirmed COVID-19 infection in the throat swab, onset of symptoms for <7 days, and severe disease. Severe disease was defined as a respiratory rate of ≥30 breaths/min or an oxygen saturation of ≤90% or a partial pressure of arterial oxygen to percentage of inspired oxygen ratio (PaO2/FiO2) of ≤300 mmHg.
Participants were excluded if they were pregnant or breast-feeding, allergic to IFN, had other evidence that could explain the cause for pneumonia such as influenza A virus infection, influenza B virus infection, bacterial pneumonia, or fungal pneumonia or noninfectious causes.
2.3. Informed consent
Patients, or their legally authorized representative, provided written informed consent for study participation. Our study was performed in accordance with the Declaration of Helsinki and was approved by the ethics committee of Shahid Beheshti University of Medical Sciences (IR.SBMU.NRITLD.REC.1398.102). This trial registered in Iranian Registry of Clinical Trials with number IRCT20151227025726N12.
2.4. Interventions
In total, 20 eligible patients with confirmed COVID-19 were assigned to receive IFN-β-1a (ReciGen®, CinnaGen, Iran) subcutaneously. Simultaneously, the patients received conventional antiviral regimen of hydroxychloroquine (200 mg P.O. BID) and lopinavir/ritonavir (200/50 mg P.O.; two tablets QID) for 5 days. Oxygenation with nasal cannula, high-flow therapy, noninvasive strategies, or mechanical ventilation was considered for all patients.
Subcutaneous administration of IFN-β-1a at a dose of 44 µg (equivalent to 12 million international units) was initiated on day 1 of hospitalization and continued every other day until day 10. Injections were administered in the peri-umbilical area of the abdomen, and injection sites were changed for each administration.
2.5. Outcomes
Demographic data, including age, gender, past medical history, and type of exposure, were recorded for all patients at baseline.
Primary outcome was the symptoms remission. Fever, cough, dyspnea, myalgia, malaise, rhinorrhea, arthralgia, chest pain, headache, vomiting, diarrhea, and sore throat were evaluated every day for 14 days. Laboratory results measured at baseline and at days 7 and 14.
As Secondary Outcomes, lung images were assessed during the 14 days of hospitalization. Chest X-ray and computed tomography (CT) imaging comparison was performed between baseline and day 14. Mortality rate, intensive care unit stay, hospital stay, and occurrence of any adverse drug reaction were also recorded. Virological clearance during the study period at admission time, day 5, and day 10 were recorded by the cycle threshold (Ct) value. Ct value ≥37 was considered as negative [12].
2.6. Statistical analysis
The results were summarized and analyzed using the SPSS v.24.0 software (IBM Corp., Armonk, NY, USA). A P value of <0.05 was considered as the significance level. Repeat-measure ANOVA was used to examine the differences between measurements.
3. Results
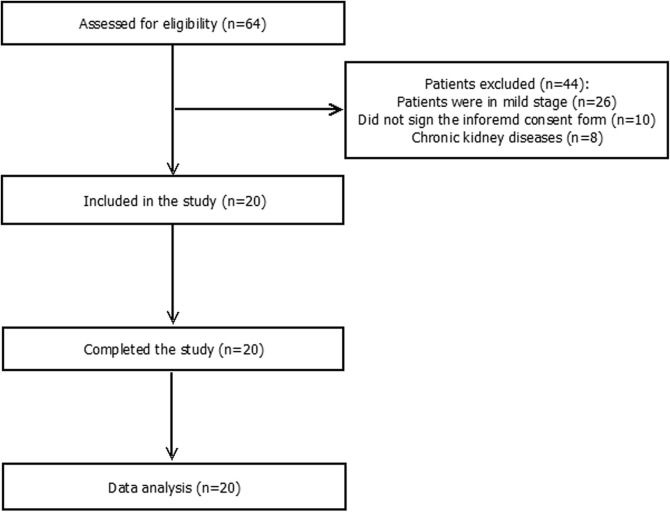
In this non-controlled trial, of the 64 eligible patients, 20 were included. All the 20 patients completed the study successfully. The CONSORT diagram of the study is presented in Fig. 1 .
Fig. 1.
The CONSORT diagram of the study.
The mean age of the patients was 58.55 ± 13.43 years. The youngest patient was a 37-year-old man and the oldest patient was 86 years old. The male-to-female ratio in the study was 4:1. Hypertension was the most comorbidity among patients. Demographic data of patients are summarized in Table 1 .
Table 1.
Demographic information of patients.
| Age | |
|---|---|
| Age, years | 58.55 ± 13.43 |
| 18–29 | 0 (0%) |
| 30–39 | 1 (5%) |
| 40–49 | 4 (20%) |
| 50–59 | 6 (30%) |
| 60–69 | 6 (30%) |
| 70–79 | 1 (5%) |
| 80–89 | 2 (10%) |
| Sex | |
| Male | 16 (80%) |
| Female | 4 (20%) |
| Past Medical History | |
| Hypertension | 4 (20%) |
| Chronic Pulmonary Diseases | 3 (15%) |
| Chronic Cardiac Diseases | 2 (10%) |
| Diabetes | 2 (10%) |
| Benning prostatic hypertrophy | 1 (5%) |
| Smoking | 1 (5%) |
| Cerebrovascular Diseases | 0 (0%) |
Time of symptom onset until hospitalization was 6.5 ± 2.8 days (min., 2 days; max., 12 days). The results revealed that 15 (75%) patients had fever, 16 (80%) had cough, and 17 (85%) had dyspnea at admission. Malaise was noted in all patients, but myalgia, rhinorrhea, arthralgia, chest pain, headache, vomiting, diarrhea, and sore throat were less frequent. Fever resolved in all patients after 8 days. Although other symptoms decreased gradually, cough, dyspnea, myalgia, and malaise still persisted in the patients. Most patients received high-flow oxygen with nasal cannula during hospitalization. Three (15%) patients received noninvasive mechanical ventilation for low oxygen saturation. These patients were weaned from the noninvasive mechanical ventilation after 5–10 days. The mean time of hospitalization was 16.8 ± 3.4 days (min., 14 days; max., 25 days). There were no deaths or significant adverse drug reactions in the 14-day period. The symptoms and oxygenation status are presented in Table 2 .
Table 2.
Symptoms of patients during the study.
| Day 1 | Day 2 | Day 3 | Day 4 | Day 5 | Day 6 | Day 7 | Day 8 | Day 9 | Day 10 | Day 11 | Day 12 | Day 13 | Day 14 | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Symptoms | ||||||||||||||
| Fever | 15 (75%) | 17 (85%) | 19 (95%) | 19 (95%) | 16 (80%) | 12 (60%) | 4 (20%) | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) |
| Cough | 16 (80%) | 16 (80%) | 16 (80%) | 15 (75%) | 15 (75%) | 16 (80%) | 15 (75%) | 15 (75%) | 13 (65%) | 10 (50%) | 10 (50%) | 10 (50%) | 10 (50%) | 9 (45%) |
| Dyspnea | 17 (85%) | 17 (85%) | 17 (85%) | 16 (80%) | 16 (80%) | 15 (75%) | 10 (50%) | 7 (35%) | 7 (35%) | 4 (20%) | 4 (20%) | 4 (20%) | 4 (20%) | 2 (10%) |
| Myalgia | 9 (45%) | 9 (45%) | 10 (50%) | 8 (40%) | 8 (40%) | 8 (40%) | 8 (40%) | 7 (35%) | 7 (35%) | 7 (35%) | 6 (30%) | 6 (30%) | 5 (25%) | 5 (25%) |
| Malaise | 20 (100%) | 18 (90%) | 16 (80%) | 16 (80%) | 18 (90%) | 17 (85%) | 16 (80%) | 17 (85%) | 17 (85%) | 15 (75%) | 14 (70%) | 11 (55%) | 10 (50%) | 10 (50%) |
| Rhinorrhea | 9 (45%) | 9 (45%) | 9 (45%) | 8 (40%) | 7 (35%) | 5 (25%) | 5 (25%) | 1 (5%) | 1 (5%) | 1 (5%) | 1 (5%) | 1 (5%) | 0 (0%) | 0 (0%) |
| Arthralgia | 6 (30%) | 5 (25%) | 1 (5%) | 1 (5%) | 1 (5%) | 1 (5%) | 1 (5%) | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) |
| Chest Pain | 3 (15%) | 3 (15%) | 3 (15%) | 3 (15%) | 3 (15%) | 4 (20%) | 1 (5%) | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) |
| Headache | 7 (35%) | 5 (25%) | 2 (10%) | 1 (5%) | 1 (5%) | 1 (5%) | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) |
| Vomiting | 3 (15%) | 2 (10%) | 3 (15%) | 1 (5%) | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) |
| Diarrhea | 1 (5%) | 1 (5%) | 1 (5%) | 1 (5%) | 1 (5%) | 1 (5%) | 1 (5%) | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) |
| Sore Throat | 9 (45%) | 10 (50%) | 11 (55%) | 8 (40%) | 6 (30%) | 6 (30%) | 6 (30%) | 6 (30%) | 5 (25%) | 2 (10%) | 2 (10%) | 1 (5%) | 0 (0%) | 0 (0%) |
Laboratory parameters were measured at admission and at days 7 and 14. The mean ± standard deviation (SD) of white blood count (WBC; cells × 103/µL) was 5.10 ± 1.41 at admission, which increased to 8.32 ± 5.55 on day 7. The mean ± SD of lymphocyte count was 1126.86 ± 311.06 on day 1; 2103.32 ± 2644.54 on day 7; and 1303.44 ± 463.22 on day 14. No abnormality was noted in hemoglobin, platelet, urea, creatinine, aspartate transaminase, alanine transaminase (ALT), and alkaline phosphatase levels. The laboratory results are presented in Table 3 .
Table 3.
Laboratory results at admission and at days 7 and 14.
| Day 1 | Day 7 | Day 14 | P Value | |
|---|---|---|---|---|
| Hemoglobin (g/dL) | 14.30 ± 1.86 | 13.69 ± 1.07 | 13.37 ± 0.69 | 0.087 |
| White blood cells (103/µL) | 5.10 ± 1.41 | 8.32 ± 5.55 | 5.78 ± 1.76 | 0.405 |
| Lymphocytes (Cells/µL) | 1126.86 ± 311.06 | 2103.32 ± 2644.54 | 1303.44 ± 463.22 | 0.067 |
| Platelet (Thousands/µL) | 165.79 ± 50.70 | 178.00 ± 43.84 | 258.22 ± 50.94 | 0.071 |
| Urea (mg/dL) | 32.70 ± 11.00 | 31.62 ± 16.98 | 29.64 ± 18.14 | 0.592 |
| Creatinine (mg/dL) | 1.27 ± 0.26 | 1.30 ± 0.34 | 1.22 ± 0.35 | 0.035 |
| AST (Units/L) | 41.79 ± 22.25 | 41.22 ± 12.85 | 54.33 ± 30.47 | 0.184 |
| ALT (Units/L) | 34.16 ± 20.62 | 33.86 ± 16.16 | 51.82 ± 31.25 | 0.321 |
| ALP (Units/L) | 166.94 ± 38.97 | 160.40 ± 31.47 | 158.89 ± 40.17 | 0.335 |
Virological clearance study showed that all patients had positive RT-PCR samples on admission time (median Ct value: 28.94). On day 5, 14 patients (70%) had positive RT-PCR samples (median Ct value: 32.93). On day 10, all patients had negative RT-PCR samples except two patients (10%) (Ct values: 34.72 and 34.86). The results of virological clearance in all patients are summarized in Table 4 .
Table 4.
Virological clearance results in all patients during the study.
| Patient number/day | Day 0 | Day 5 | Day 10 |
|---|---|---|---|
| Patient 1 | 25.61 | 34.81 | Negative |
| Patient 2 | 29.72 | 33.12 | Negative |
| Patient 3 | 27.22 | 31.16 | Negative |
| Patient 4 | 29.15 | 33.86 | Negative |
| Patient 5 | 30.15 | Negative | Negative |
| Patient 6 | 29.84 | 34.47 | Negative |
| Patient 7 | 31.03 | Negative | Negative |
| Patient 8 | 25.95 | 32.74 | Negative |
| Patient 9 | 30.11 | 29.78 | 34.72 |
| Patient 10 | 26.32 | 29.64 | Negative |
| Patient 11 | 28.02 | 34.73 | Negative |
| Patient 12 | 24.18 | 29.11 | Negative |
| Patient 13 | 27.18 | 34.05 | Negative |
| Patient 14 | 31.12 | Negative | Negative |
| Patient 15 | 32.67 | 34.45 | 34.86 |
| Patient 16 | 22.3 | 25.44 | Negative |
| Patient 17 | 31.17 | Negative | Negative |
| Patient 18 | 28.74 | 26.52 | Negative |
| Patient 19 | 31.19 | Negative | Negative |
| Patient 20 | 28.71 | Negative | Negative |
Negative RT-PCR was defined as Ct value ≥ 37.
Lung CT and chest X-ray were performed at admission and on day 14. The CT images revealed ground glass opacity in 16 patients and X-ray images revealed bilateral infiltration in 14 patients. As can be seen in Fig. 2 , recovery occurred after 14 days.
Fig. 2.
Lung computed tomography and chest X-ray showing ground glass opacity and bilateral infiltration, respectively, at admission (left pictures). The images on the right reveal recovery after 14 days of treatment with IFN-β-1a.
4. Discussion
In this study, we evaluated the therapeutic efficacy and safety of IFN-β-1a in patients with COVID-19. The results revealed the efficacy of IFN-β-1a in combination with hydroxychloroquine, and lopinavir/ritonavir in reducing the disease symptoms. This result was supported by the lung CT and chest X-ray images that showed dramatic response to this combination treatment. Regarding safety concerns, no significant adverse drug reactions or mortality was noted in this study.
IFNs mediate several biological effects. They modulate both T- and B-lymphocyte responses by promoting the proliferation of memory T cells, stimulating the differentiation of Th1 cells, inducing IFN-γ secretion from T cells, and promoting isotype switching in B cells and differentiation into plasma cells [13]. IFN-α and IFN-β upregulate major histocompatibility complex class I proteins [14]. Moreover, IFNs activate macrophages, trigger and enhance the cytotoxicity of natural killer cells, and regulate the maturation and terminal differentiation of dendritic cells [15]. They have widespread potential as therapeutic agents for viral infections and are currently the preferred drug for chronic hepatitis B and C infections [16]. IFNs inhibit viral infection by preventing viral entry into target cells and by blocking different stages of the viral replication cycle for different viruses. IFN-α and IFN-β play a critical role in linking the innate and adaptive immune responses to viral challenge [17]. To date, there are no published studies regarding the therapeutic efficacy of IFNs on COVID-19, although some studies have evaluated their efficacy in treating SARS, MERS, and Ebola.
Hensley et al. reported that IFN-β-1a could be an effective therapeutic agent for SARS-CoV infections. In that study, IFN-β-1a demonstrated potent antiviral activity and acceptable safety profiles, suggesting its efficacy in coronavirus treatment [11].
Al-Tawfiq et al. evaluated the effects of ribavirin and IFN combination in patients with MERS. They administered IFN-α 2b (100 µg) subcutaneously once a week for two doses. They suggested that ribavirin and IFN could be effective in some patients, but it is associated with mortality in critically ill patients. Additionally, they found that this combination is more beneficial in patients who are not critically ill [18]. Because our most of our patients were in the non-critical phase of COVID-19, the results cannot be generalized for all patients.
Ranirti et al. evaluated the therapeutic efficacy of IFN-β-1a in acute respiratory distress (ARDS). They administered IFN-β-1a through the intravenous route and found that the drug was ineffective in treating ARDS. This could be due to the presence of the released cytokines. Therefore, it can be concluded that IFN-β-1a is not an appropriate therapeutic agent for patients with critical disease and that it is to be initiated in the early phase of the disease [19].
Blanco-Melo et al. compared the transcriptional response of SARS-CoV-2 with other respiratory viruses to identify transcriptional signatures that may underlie COVID-19 pathophysiology. They treated infected cells with universal IFN-β and assessed viral levels at the RNA and protein levels. They found that addition of IFN-I resulted in a dramatic reduction in virus replication. Finally, they concluded that the response to SARS-CoV-2 is imbalanced with regard to controlling virus replication versus activation of the adaptive immune response [20].
Hadjadj et al. performed an immune analysis that included phenotypical profiling of immune cells, whole blood transcriptomic, and cytokine quantification on 50 patients with COVID-19. They characterized impaired IFN-I response by a low interferon production and activity, with consequent downregulation of interferon-stimulated genes in severe and critically ill patients [21].
We had three main limitations in this study including lack of the control group, confounding effects of concurrent medications, and small sample size. Also, the ethical challenges push us not to consider the control group who were deprived of effective treatment. In this study, all patients received the combination of IFN-β-1a, hydroxychloroquine, and lopinavir/ritonavir according to the national Iranian guideline on COVID-19 treatment and we could not administer solely IFN-β-1a [22]. Hence, the net therapeutic effect of IFN-β-1a along with all other drugs may not be established exactly. With considering the mentioned limitations, the results of this study should be interpreted cautiously and further large trials are needed to show the therapeutic effects of IFN-β-1a in COVID-19. Also, we suggest future trials to consider the therapeutic effects of other types of IFN including IFN-α in COVID-19. Our findings support the use of IFN-β-1a in combination with hydroxychloroquine and lopinavir/ritonavir in the management of COVID-19.
Funding Sources
None.
CRediT authorship contribution statement
Farzaneh Dastan: Conceptualization, Methodology, Writing - review & editing, Supervision. Seyed Alireza Nadji: Investigation, Writing - review & editing. Ali Saffaei: Investigation, Formal analysis, Writing - original draft, Writing - review & editing, Visualization. Majid Marjani: Methodology, Writing - review & editing. Afshin Moniri: Methodology, Writing - review & editing. Hamidreza Jamaati: Conceptualization, Writing - review & editing. Seyed MohammadReza Hashemian: Conceptualization, Writing - review & editing. Parvaneh Baghaei Shiva: Data curation, Writing - review & editing. Atefeh Abedini: Data curation, Writing - review & editing. Mohammad Varahram: Investigation, Writing - review & editing. Sahar Yousefian: Data curation, Software, Writing - review & editing. Payam Tabarsi: Conceptualization, Methodology, Writing - review & editing, Project administration.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.intimp.2020.106688.
Appendix A. Supplementary material
The following are the Supplementary data to this article:
References
- 1.Wu Z., McGoogan J.M. Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China: summary of a report of 72314 cases from the Chinese center for disease control and prevention. JAMA. 2020 doi: 10.1001/jama.2020.2648. [DOI] [PubMed] [Google Scholar]
- 2.Zhang L., Liu Y. Potential interventions for novel coronavirus in China: A systematic review. J. Med. Virol. 2020;92:479–490. doi: 10.1002/jmv.25707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Sahraei Z., Shabani M., Shokouhi S., Saffaei A. Aminoquinolines against coronavirus disease 2019 (COVID-19): Chloroquine or Hydroxychloroquine. Int. J. Antimicrob. Agents. 2020 doi: 10.1016/j.ijantimicag.2020.105945. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Channappanavar R., Perlman S. Pathogenic human coronavirus infections: causes and consequences of cytokine storm and immunopathology. Seminars Immunopathol. 2017;39:529–539. doi: 10.1007/s00281-017-0629-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Zheng H.-Y., Zhang M., Yang C.-X., Zhang N., Wang X.-C., Yang X.-P. Elevated exhaustion levels and reduced functional diversity of T cells in peripheral blood may predict severe progression in COVID-19 patients. Cell. Mol. Immunol. 2020 doi: 10.1038/s41423-020-0401-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.González-Navajas J.M., Lee J., David M., Raz E. Immunomodulatory functions of type I interferons. Nat. Rev. Immunol. 2012;12:125–135. doi: 10.1038/nri3133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Medrano R.F.V., Hunger A., Mendonça S.A., Barbuto J.A.M., Strauss B.E. Immunomodulatory and antitumor effects of type I interferons and their application in cancer therapy. Oncotarget. 2017;8:71249–71284. doi: 10.18632/oncotarget.19531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Osterlund P., Veckman V., Sirén J., Klucher K.M., Hiscott J., Matikainen S. Gene expression and antiviral activity of alpha/beta interferons and interleukin-29 in virus-infected human myeloid dendritic cells. J. Virol. 2005;79:9608–9617. doi: 10.1128/JVI.79.15.9608-9617.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lin F-c, Young H.A. Interferons: Success in anti-viral immunotherapy. Cytokine Growth Factor Rev. 2014;25:369–376. doi: 10.1016/j.cytogfr.2014.07.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Samuel C.E. Antiviral actions of interferons. Clin. Microbiol. Rev. 2001;14:778–809. doi: 10.1128/CMR.14.4.778-809.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hensley L.E., Fritz L.E., Jahrling P.B., Karp C.L., Huggins J.W., Geisbert T.W. Interferon-beta 1a and SARS coronavirus replication. Emerg. Infect. Dis. 2004;10:317–319. doi: 10.3201/eid1002.030482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.V.M. Corman, O. Landt, M. Kaiser, R. Molenkamp, A. Meijer, D.K.W. Chu et al., Detection of 2019 novel coronavirus (2019-nCoV) by real-time RT-PCR. Euro surveillance : bulletin Europeen sur les maladies transmissibles = European communicable disease bulletin. 25 (2020) 2000045. [DOI] [PMC free article] [PubMed]
- 13.Kaiko G.E., Horvat J.C., Beagley K.W., Hansbro P.M. Immunological decision-making: how does the immune system decide to mount a helper T-cell response? Immunology. 2008;123:326–338. doi: 10.1111/j.1365-2567.2007.02719.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Xia S., Tao Y., Cui L., Yu Y., Xu S.M.H.C. Class I Molecules exacerbate viral infection by disrupting type I. interferon signaling. J. Immunol. Res. 2019;2019:5370706. doi: 10.1155/2019/5370706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Müller L., Aigner P., Stoiber D. Type I Interferons and Natural Killer Cell Regulation in Cancer. Front. Immunol. 2017;8:304. doi: 10.3389/fimmu.2017.00304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Teijaro J.R. Type I interferons in viral control and immune regulation. Curr. Opin. Virol. 2016;16:31–40. doi: 10.1016/j.coviro.2016.01.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Davidson S., Maini M.K., Wack A. Disease-promoting effects of type I interferons in viral, bacterial, and coinfections. J. Interferon Cytokine Res.: Off. J. Int. Soc. Interferon Cytokine Res. 2015;35:252–264. doi: 10.1089/jir.2014.0227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Al-Tawfiq J.A., Momattin H., Dib J., Memish Z.A. Ribavirin and interferon therapy in patients infected with the Middle East respiratory syndrome coronavirus: an observational study. Int. J. Infect. Dis. 2014;20:42–46. doi: 10.1016/j.ijid.2013.12.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Bellingan G., Maksimow M., Howell D.C., Stotz M., Beale R., Beatty M. The effect of intravenous interferon-beta-1a (FP-1201) on lung CD73 expression and on acute respiratory distress syndrome mortality: an open-label study. Lancet Respir. Med. 2014;2:98–107. doi: 10.1016/S2213-2600(13)70259-5. [DOI] [PubMed] [Google Scholar]
- 20.Blanco-Melo D., Nilsson-Payant B.E., Liu W.-C., Uhl S., Hoagland D., Møller R. Imbalanced Host Response to SARS-CoV-2 Drives Development of COVID-19. Cell. 2020 doi: 10.1016/j.cell.2020.04.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.J. Hadjadj, N. Yatim, L. Barnabei, A. Corneau, J. Boussier, H. Pere, et al. Impaired type I interferon activity and exacerbated inflammatory responses in severe Covid-19 patients, medRxiv. 2020: 2020.04.19.20068015. [DOI] [PMC free article] [PubMed]
- 22.Jamaati H., Dastan F., Tabarsi P., Marjani M., Saffaei A., Hashemian S.M. A fourteen-day experience with coronavirus disease 2019 (COVID-19) induced acute respiratory distress syndrome (ARDS): an Iranian treatment protocol. Iran. J. Pharmaceut. Res. 2020 doi: 10.22037/ijpr.2020.113337.14239. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.