Abstract
Background
The treatment of large bone defects in lower limbs is a serious challenge for orthopedic surgeons and patients. The bone transport technique using the Ilizarov method has become the main treatment option for the reconstruction of bone defect. However, inevitable difficulties and complications related to bone transport technique have been reported by many studies. The purpose of this study was to evaluate the effectiveness and complications of bone transport technique using Ilizarov method in the treatment of bone defect of lower extremity.
Methods
The study was conducted on 282 patients who underwent bone transport procedures using Ilizarov method at our institution from January 2007 to June 2017. Patient’s demographic data, complications and clinical outcomes at minimum of 2 years follow-up were collected and retrospectively analyzed. All difficulties that related to bone transport were documented according to Paley’s classification. The clinical outcomes were evaluated using Association for the Study and Application of the Method of Ilizarov criteria (ASAMI) at last clinical visit.
Results
There were 243 male and 39 females with a mean age of 40 years (range 18–65 years). The mean defect was 6.56 ± 2.15 cm, whereas single level transport in 221 cases and double level transport in 61 cases. There were 189 problems, 166 obstacles and 406 complications (257 minor and 149 major complications), and the average complication rate per patients consists of 0.91 minor and 0.53 major complications. The top five complications were pin-site infection (65.96%), axial deviation (40.78%), joint stiffness (23.76%), soft tissue incarceration (22.34%) and delayed union of the docking site (13.48%).The ASAMI bony result was excellent in 233 patients, good in 32, fair in 5 and poor in 12. The ASAMI functional result was excellent in 136 patients, good in 88, fair in 47, poor in 11.
Conclusion
Bone transport is a reliable method for reconstruction of bone defects in the femur and tibia. Awareness of predictable complications is beneficial to prevent or early detection of the expected complication which can improve the risk-benefit balance.
Keywords: Bone defect, Bone transport, Complication, External fixation
Background
The treatment of large bone defects caused by trauma, developmental deformities, resection of tumor or osteomyelitis in lower limbs is a serious challenge for orthopedic surgeons and patients [1, 2]. Many surgical procedures have been proposed for the treatment of bone defect [3–6], and bone transport technique using the Ilizarov method is widely practiced in reconstructive surgery [7–10]. The Ilizarov method is based on the biology of the bone and the ability of the surrounding soft tissues to regenerate under tension stress, so it become the main treatment option for the reconstruction of bone defect due to it is characterized by rapid, simple, effective and minimally invasive, which can preserve the biomechanical microenvironment needed for fracture healing [9, 11–14].
Although the treatment of bone defect using bone transport technique has been used widely include reconstruction of the bone defect along with soft-tissue coverage, correction of the joint contractures or malalignment. However, inevitable difficulties and complications related to bone transport technique using the Ilizarov method have been reported by many studies [9, 13–19]. It is remaining a major concern to these complications which could affect on the clinical outcomes.
Therefore, the purpose of our study was to retrospectively analyze and evaluate the bone transport-related complications of patients in our institution over the past 10 years in order to predict the risk and related factors of complications.
Methods
Patients
This retrospectively study included 282 patients who underwent bone transport procedures in lower extremity using the Ilizarov method at our institution from Jan 2007 to June 2017, including 243 male and 39 females with a mean age of 40 years (range 18–65 years). Patients older than 18 years with bone defect more than 3 cm in the lower extremity were included. Patients with bone defect caused by pathological fractures, associated vascular and nerve injury, age > 65 years, poor compliance, and any other illness that can affect bone healing (such as diabetes, hypertension, osteoporosis, kidney disease, etc.) were excluded. This study was approved by the Ethical Committee of our institution.
Surgical technique
A complete removal of hardware, radical debridement of all necrotic and infected bone and soft tissue, and/or implantation of an antibiotic-impregnated cement spacer to improve stability were performed prior to bone transport. Cortical bleeding, described as the so-called “paprika sign”, was accepted as an indication of vital osseous tissue [20]. Specimens were taken and sent for bacterial culture and drug susceptibility tests to guide the surgeon for the appropriate postoperative antibiotics. Local tissue flap or directly suture without tension was performed to reconstruct the small soft tissue defects, whereas flap transfer or free skin grafting was used to cover the larger wound.
Bone transport was initiated when clinical manifestations and laboratory indicators showed the infective process had resolved. Preoperative anteroposterior and lateral X-rays were used to evaluate the defect size and plan the construction of the external fixator. The type of external fixator was comprehensively determined by the location of bone and soft tissue defect along with surgeon’s experience and patient’s acceptance. The osteotomy was performed using minimally invasive fashion using Gigli saw technique and special care was given to preserve as much periosteum as possible. Bone defect larger than 8 cm or exceeded 40% of the injured bone underwent a double level bone transport [21–23] procedure. All the procedures were conducted by the same surgical team.
Data collection
The demographic data include age, sex, weight and height (BMI = weight (kg) /height (m2)), injured bone, location of bone defect (proximal, middle and distal), defect size (DS), type of external fixation (circular (TrueLok Ring Fixation System, Orthofix, Verona, Italy) or monolateral (Limb Reconstruction System, LRS, Orthofix, Verona, Italy)), type of bone transport (single level and double level), direction of bone transport (from proximal to distal or distal to proximal in single level and converging or “twin” transport in double level) were collected.
Postoperative data were recorded include distraction regenerate length (DRL), docking time (DT), regenerate consolidation time (CT), external fixation time (EFT/ET), external fixation index (EFI) and type of difficulties occurred during and after bone transport procedure. The EFT referred to the time spend on before removal of the external fixator. The EFI was defined as the ratio of the days of EFT to the DRL (centimeters). Radiographic evaluation was conducted every 2 weeks during the bone transport period and monthly in the consolidation phase. All patients were closely followed up at minimum of 2 years after the removal of external fixator.
According to Paley [24], difficulties that occur during limb lengthening were subclassified into problems, obstacles and complications. A problem is defined as a potential expected difficulty that arises during the distraction or fixation period that is fully resolved by the end of the treatment period by nonoperative means. An obstacle is defined as a potential expected difficulty that arises during the distraction or fixation period that is fully resolved by the end of the treatment period by operative means. Complications include any local or systemic intraoperative or perioperative complication, a difficulty during distraction or fixation that remains unresolved at the end of the treatment period, and any early or late posttreatment difficulty. True complications were subclassified as minor and major complications. Minor complications did not affect the final result or required nonoperative or a minor operative intervention, while major complications required a more complex and unplanned operative intervention or resulted in permanent sequelae. The bone and functional results were assessed by ASAMI [21] at the last clinical visit.
Postoperative management
All patients were encouraged to do isometric muscle and joint range of motion (ROM) exercise within the tolerance of pain on the second day after surgery. Antibiotics that are suitable according to the results of cultures and antibiotic susceptibility tests are applied intravenously for at least 3 weeks or until the erythrocyte sedimentation rate (ESR) and C-reactive protein (CRP) levels return to normal limits.
According to the reference data [25, 26], after latency period of 7 to 10 days, bone transport started at a rate of 1 mm (single level) or 2 mm (double level) daily, 4 times a day. The rate of bone transport was adjusted according to patients’ tolerance and the quality of the regenerate. The procedure of bone transport continued for 4 or 5 days to compress the docking site after the docking. The external fixator was dynamized before removal. And removal of the external fixator was conducted when the standard orthogonal radiographs showed sufficient consolidation of the distraction zone (dense bone formation) and solid docking site union (corticalization in 3 of 4 cortices). Additionally, all patients were put on the functional brace for 4–6 weeks for the protection of refracture.
Statistical analysis
Statistical analysis was performed with the SPSS 22.0 (IBM Corp, USA) and R Studio (Version 1.2.5001) with rms, ROCR, gplots and forest plot packages. Continuous variables were analyzed by Independent-samples T tests and expressed as the mean and standard deviation. And the count variables were analyzed by the Chi-square or Fisher’s test, expressing as number. Statistically significant difference was set at P < 0.05.
Variables with P < 0.05 were identified in the univariate logistic regression analysis (ULRA). And the variables with P < 0.1 in the ULRA were included in the multivariate logistic regression analysis (MLRA), then variables with P < 0.05 were screened out by the stepwise method and these variables were used to construct the nomograms. Finally, the ability of nomograms to distinguish the models was evaluated by the area under the curve (AUC) of the receiver operating characteristic (ROC) curve.
Results
The etiology of bone defect includes posttraumatic in 97 cases (17 femur and 80 tibias), osteomyelitis in 146 (31 femurs and 115 tibias), infected nonunion in 26 (11 femurs and 15 tibias) and atrophic nonunion in 13 (3 femurs and 10 tibias). A total of 220 tibial and 62 femoral bone transport procedures in our study were collected. The Ilizarov circular fixator was applied in 128 cases (all in tibia), and the monolateral fixator was applied in 154 cases (62 femurs,92 tibias). The average defect size was 6.56 ± 2.15 cm (range 3 to 14 cm). Based on the bone defect location, proximal 1/3 of the diaphysis in 32 cases (4 in femur, 28 in tibia), middle 1/3 in 129 (31 in femur, 98 in tibia) and distal 1/3 in 121 cases (27 in femur, 94 in tibia). A total of 221 cases underwent single level bone transport procedure and 61 cases were treated by double level bone transport.
The differences of DS, DT, CT, EFT and EFI between single level and double level were statistically significant(p < 0.05), whereas they were not statistically significant in the same level(p > 0.05). The mean EFI in the double level group is lower than that in the single level group. More details are shown in Table 1, 2 and 3.
Table 1.
Comparison of the single and double level bone transport group
| Single level group | Double level group | t | p-value | |
|---|---|---|---|---|
| DS (cm) | 5.84 ± 1.64 | 9.18 ± 1.78 | −13.714 | < 0.001 |
| DT(d) | 85.69 ± 22.83 | 70.90 ± 13.87 | 6.267 | < 0.001 |
| CT(d) | 254.34 ± 58.55 | 230.40 ± 39.52 | 2.986 | 0.003 |
| EFT(d) | 385.15 ± 89.01 | 340.62 ± 52.18 | 4.941 | < 0.001 |
| EFI(d/cm) | 66.54 ± 8.58 | 38.01 ± 6.52 | 23.930 | < 0.001 |
Values are presented as mean ± SD. DS defect size, DT docking time, CT consolidation time, EFT external fixation time, EFI external fixation index
Table 2.
Comparison of femur and tibia in different group
| Single level group | Double level group | |||||||
|---|---|---|---|---|---|---|---|---|
| Femur | Tibia | t | p-value | Femur | Tibia | t | p-value | |
| DS (cm) | 5.75 ± 1.77 | 5.87 ± 1.61 | −0.437 | 0.663 | 9.39 ± 1.47 | 9.11 ± 1.87 | 0.520 | 0.605 |
| DT(d) | 85.54 ± 24.27 | 85.73 ± 22.49 | −0.050 | 0.960 | 71.64 ± 12.44 | 70.67 ± 14.40 | 0.227 | 0.821 |
| CT(d) | 264.02 ± 67.94 | 251.66 ± 55.59 | 1.296 | 0.196 | 235.29 ± 36.54 | 228.91 ± 40.66 | 0.525 | 0.602 |
| EFT(d) | 393.02 ± 92.35 | 382.97 ± 88.21 | 0.691 | 0.490 | 345.36 ± 46.39 | 339.17 ± 54.22 | 0.385 | 0.701 |
| EFI(d/cm) | 67.72 ± 11.26 | 66.22 ± 7.69 | 1.073 | 0.285 | 37.19 ± 4.65 | 38.26 ± 7.02 | −0.536 | 0.594 |
Values are presented as mean ± SD. DS defect size, DT docking time, CT consolidation time, EFT external fixation time, EFI external fixation index
Table 3.
Comparison of single and double level group in different bone
| Femur | Tibia | |||||||
|---|---|---|---|---|---|---|---|---|
| SLG | DLG | t | p-value | SLG | DLG | t | p-value | |
| DS (cm) | 5.75 ± 1.77 | 9.39 ± 1.47 | −7.021 | < 0.001 | 5.87 ± 1.61 | 9.11 ± 1.87 | −11.738 | < 0.001 |
| DT(d) | 85.54 ± 24.27 | 71.64 ± 12.44 | 2.057 | 0.044 | 85.73 ± 22.49 | 70.67 ± 14.4 | 4.307 | < 0.001 |
| CT(d) | 264.02 ± 67.94 | 235.29 ± 36.54 | −3.396 | 0.001 | 251.66 ± 55.59 | 228.91 ± 40.66 | 2.595 | 0.010 |
| EFT(d) | 393.02 ± 92.35 | 345.36 ± 46.39 | −2.170 | 0.034 | 382.97 ± 88.21 | 339.17 ± 54.2 | 3.207 | 0.002 |
| EFI(d/cm) | 67.72 ± 11.26 | 37.19 ± 4.65 | 9.856 | < 0.001 | 66.22 ± 7.69 | 38.26 ± 7.02 | 22.311 | < 0.001 |
Values are presented as mean ± SD. DS defect size, DT docking time, CT consolidation time, EFT external fixation time, EFI external fixation index, SLG single level group, DLG double level group
Based on the ASAMI scoring, bony result was excellent in 233 patients (82.62%), good in 32(11.35%), fair in 5(1.77%), poor in 12(4.26%). The functional result was excellent in 136 patients (48.23%), good in 88 (31.21%), fair in 47 (16.67%), poor in 11 (3.90%). The excellent and good rates of bony results was 93.97% (265 of 282), while that of the functional results was 79.43% (224 of 282). (Table 4).
Table 4.
Results of ASAMI scores
| Excellent | Good | Fair | Poor | Failure | ||
|---|---|---|---|---|---|---|
| ASAMI | Bone grade | 233 | 32 | 5 | 12 | – |
| Function grade | 136 | 88 | 47 | 11 | 0 | |
| ASAMI Criteria | ||||||
| Bone results | ||||||
|
Excellent: Union, no infection, deformity < 7°, limb length discrepancy (LLD) < 2.5 cm Good: Union plus any two of the following: absence of infection, deformity < 7°, LLD < 2.5 cm. Fair: Union plus any one of the following: absence of infection, deformity < 7°, LLD < 2.5 cm. Poor: Nonunion/refracture/union plus infection plus deformity > 7° plus LLD > 2.5 cm | ||||||
| Functional results | ||||||
|
Excellent: Active, no limp, minimum stiffness (loss of < 15°knee extension/< 15°ankle dorsiflexion) no reflex sympathetic dystrophy (RSD), insignificant pain. Good: Active, with one or two of the following: limb, stiffness, RSD, significant pain Fair: Active, with three or all of the following: limb, stiffness, RSD, significant pain Poor: Inactive (unemployment or inability to return to daily activities because of injury) Failure: Amputation | ||||||
There were 189 problems, 166 obstacles and 406 complications (257 minor complications and 149 major complications) in our study (Table 5). Complications were more prevalent in the single level group (329 complications of 221 patients), whilst it was less in the double level group (77 complications of 61 patients) (Table 5). Most common major complications include joint stiffness (37.58%), delayed union of the docking site (19.46%), axial deviation (18.79%), refracture (8.05%), and muscle contractures (6.04%). Most common minor complications were axial deviation (33.85%), soft tissue incarceration (24.51%), pin-site infection (22.18%), muscle contractures (10.12%), and joint stiffness (4.28%). The average complication rate per patients consists of 0.91 minor and 0.53 major complications (Table 6).
Table 5.
Difficulties related to the bone transport procedure
| Single level group | Double level group | Total | |||
|---|---|---|---|---|---|
| Femur | Tibia | Femur | Tibia | ||
| Problem | 41 | 103 | 14 | 31 | 189 |
| Obstacle | 47 | 64 | 18 | 37 | 166 |
| Complication | 68 | 261 | 23 | 54 | 406 |
| Problem: A potential expected difficulty that arises during the distraction or fixation period that is fully resolved by the end of the treatment period by nonoperative means. | |||||
| Obstacle: A potential expected difficulty that arises during the distraction or fixation period that is fully resolved by the end of the treatment period by operative means. | |||||
| Complication: Any local or systemic intraoperative or perioperative complication, a difficulty during distraction or fixation that remains unresolved at the end of the treatment period, and any early or late posttreatment difficulty. | |||||
Table 6.
Bone transport-related complications
| Complications | Minor | Major |
|---|---|---|
| Deep pin tract infection or pin loosening | 57 | 3 |
| Muscle contractures | 26 | 9 |
| Joint stiffness | 11 | 56 |
| Axial deviation | 87 | 28 |
| Soft tissue incarceration | 63 | 0 |
| Neurological injury | 0 | 0 |
| Vascular injury | 0 | 0 |
| Delayed consolidation | 4 | 7 |
| Delayed union | 9 | 29 |
| Nonunion | 0 | 5 |
| Refracture | 0 | 12 |
| Total | 257 | 149 |
The top five complications of our study were pin-site infection (65.96%), axial deviation (40.78%), joint stiffness (23.76%), soft tissue incarceration (22.34%) and delayed union of the docking site (13.48%) (Table 6). Pin tract infection was occurred in most of the patients and managed by daily pin site care and oral antibiotics, 60 patients suffered deep pin tract infection or pin loosening and successfully treated by pin replacement and intravenous antibiotics. Axial deviation occurred in 115 patients, modification of the apparatus or inserting an additional Schanz screw(s) to pull the bone out of its deviated position was required before the end of the treatment. Joint stiffness occurred in 67 cases and treated with physiotherapy along with joint release if needed. Soft tissue incarceration was noted in 63 cases and managed by freshening the bone ends, opening the medullary canal and resection of invaginated soft-tissue. Delayed union was presented in 38 cases and treated by “accordian” technique or bone grafting if it was developed to nonunion.
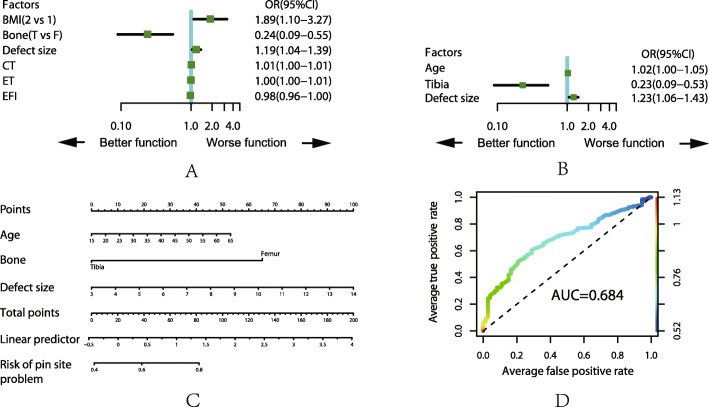
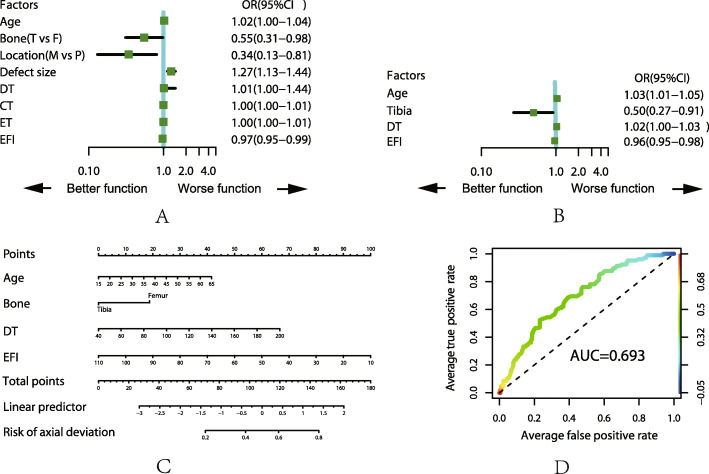
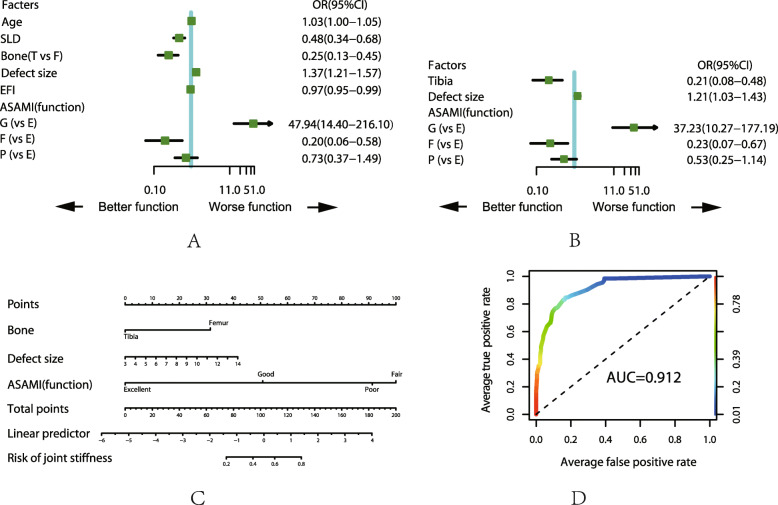
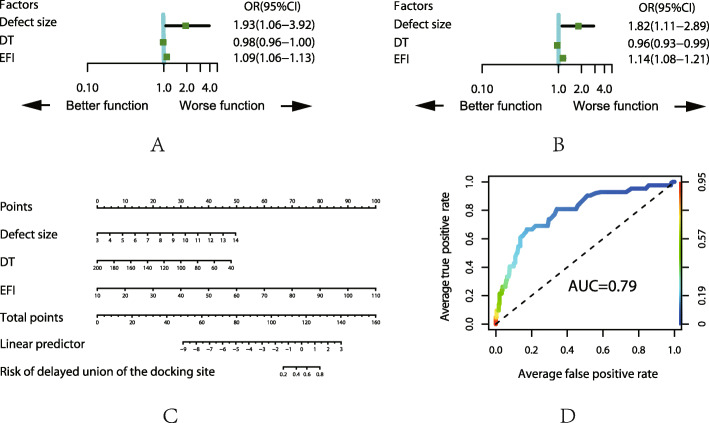
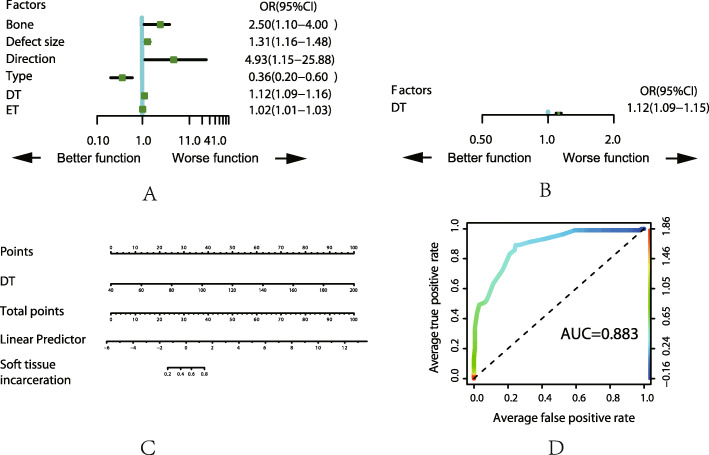
For the top five complications, we analyzed those with the related factors by ULRA, MLRA, nomogram and AUC, the details are shown in Fig. 1, 2, 3, 4, and 5. It is generally believed that the model with AUC of 0.50–0.75 is acceptable, and our results are all in this range.
Fig. 1.
Analysis of the complication of pin site problem. a Result of ULRA. b Result of MLRA. c Nomogram to predict the probability of pin site problem. d ROC curves for validating the discrimination power of the nomogram. BMI (1 = underweight, 2 = normal, 3 = overweight, 4 = obesity), Bone (F = femur, T = tibia)
Fig. 2.
Analysis of the complication of pin site problem. a Result of ULRA. b Result of MLRA. c Nomogram to predict the probability of pin site problem. d ROC curves for validating the discrimination power of the nomogram. Bone (F = femur, T = tibia), Location (P = proximal, M = middle)
Fig. 3.
Analysis of the complication of joint stiffness. a Result of ULRA. b Result of MLRA. c Nomogram to predict the probability of pin site problem. d ROC curves for validating the discrimination power of the nomogram. Bone (F = femur, T = tibia), ASAMI (E = excellent, G = good, F = fair, P = poor)
Fig. 4.
Analysis of the complication of delayed union of the docking site. a Result of ULRA. b Result of MLRA. c Nomogram to predict the probability of pin site problem. d ROC curves for validating the discrimination power of the nomogram
Fig. 5.
Analysis of the complication of soft tissue incarceration. a Result of ULRA. b Result of MLRA. c Nomogram to predict the probability of pin site problem. d ROC curves for validating the discrimination power of the nomogram
Discussion
Our results showed that double level bone transport can greatly shorten the treatment time compared with single level bone transport. In previous studies [27–31], the mean EFI was 50.0 days/cm (range 43.1 to 58.1 days/cm) in patients treated by single level bone transport, and it is lower than that in our study (66.54 ± 8.58 days/cm). This can be explained by the mechanism of bone defect in our study is mostly caused by posttraumatic osteomyelitis (51.77%) which requires repeated debridement before the initiation of bone transport, the microenvironment for bone regeneration and soft-tissue coverage may destructed, both docking union and regenerate mineralization become time consuming process.
The majority of patients had suffered from various complications during the long treatment period [24, 32, 33]. In the Paley and Maar’s study [34], 19 patients with tibial bone defects were treated with bone transport by Ilizarov method, union was achieved in all cases but 22 minor and 19 major complications were observed, the mean complication rate per patient was 1.15 minor and 1.00 major complications. As for Spieql U et al.9, total of 25 patients were included in their study, the patients suffered 22 minor and 13 major complications, and the average complication rate consists of 0.88 minor and 0.52 major complications per patients. Other authors also reported high complication rates in the bone transport procedure [27, 30]. In our study, the average complication rate per patients consists of 0.91 minor and 0.53 major complications.
Pin track problems
ULRA showed that the presence of pin track problems is less in patient with less BMI, smaller defect size in tibia, shorter CT, ET and EFI. It is due to less soft coverage of tibia in thin patient and shorter time spent in external fixator can significantly reduce the occurrence of pin track problem.
The result of the MLRA showed that less occurrence of pin tract problem in younger patients with smaller tibial defect. Immune system is stronger with better elasticity of local soft tissue in younger patient compared with older one. Besides, more resistance was encounter due to abundant muscle coverage in femur than tibia which can explain the higher occurrence of pin tract problem in femoral bone transport than in tibia.
Axial deviation
ULRA showed that younger people with bone defect located in the middle 1/3 of tibia suffered less probability of axial deviation. This can be explained by stability of pins are stronger in younger patients (less occurrence of osteoporosis compared with older patient) and muscle tension have less effect in middle 1/3 bone defect during bone transport. The possibility of axial deviation is also less in cases with smaller defect size and shorter DT, CT, ET and EFI which is consisted with the generally accepted theory, the stability of external fixator will be reduced with longer time spend on fixator mountain. The MLRA demonstrated that younger patient, tibial defect, shorter DT and EFI are related with less probability of axial deviation.
Joint stiffness
ULRA showed that older people with larger femoral defect using double level bone transport tend to have joint stiffness. Additionally, longer EFI lead to prolonged fixation time and patient may reluctant to perform functional exercise which may increase the chance of joint stiffness. As for ASAMI score, the fair and poor grade were not clinically significant. Aforementioned result was also found in the MLRA. Isometric muscle and joint range of motion (ROM) exercise within the tolerance of pain on the second day after surgery is strongly recommended to prevent the occurrence of joint stiffness.
Delayed union
Both ULRA and MLRA showed that delayed union is more likely to occur in patient with large defect size, longer docking time and EFI. The bone end become ossified due to microvascular occlusion before contact with longer docking time. Moreover, improper application of the external fixator or poor alignment may alter the biomechanical environment required by bone union, in addition, less functional exercise causes less physiological stress stimulation on the bone end, all of these factors contributed to the occurrence of delayed union.
Soft tissue incarceration
ULRA showed that patient with smaller femoral defect using double level “twin” bone transport is less likely to suffer soft tissue incarceration. Additionally, longer DT and ET also increase the chance of soft tissue incarceration. The result of MLRA demonstrated that only DT is significantly associated with the occurrence of soft tissue incarceration.
In the present study, we used ASAMI scoring system to evaluate the effectiveness of the method of bone transport. The excellent and good rates of bony results was higher than that of functional results and these results were similar to other studies [15, 35, 36].
A total of 12 patients suffered refracture either on docking site or regenerate region. Among them, 4 cases were due to early removal of external fixator and 8 cases were due to a fall injury (5 cases) or a car accident (3 cases) after the removal of the protective plaster and all of them achieved union by open reduction and plate fixation.
Ilizarov method is inadvisable for the socially disadvantaged patients, especially those with poorly managed mental illness or those without a supportive family environment, mainly due to prolonged treatment period associated with potential complications. A number of factors may contribute to the occurrence of complications during the bone transport procedure. Based on our retrospective study, age, BMI, defect size, injured bone, location of bone defect, type of bone transport, direction of bone transport, docking time, regenerate consolidation time, external fixation time and external fixation index are statistically significantly associated with the occurrence of complications; age, defect size and external fixation time are the prominent predictors of complications.
The present study had several limitations. First, considering its retrospective nature and relatively small sample size, prudent attitude should be adopted regarding the interpretations of our bone and functional outcomes. Second, longer follow-up time is necessary to better evaluate the clinical efficacy. Third, further investigations, especially multi-centered trails with a larger sample size should be conducted to overcome the limitations of our study.
Conclusion
Our study presents the results of 282 consecutive cases using single or double level bone transport with particular reference to the complications and its related factors. Bone transport is a reliable method for reconstruction of bone defects in the femur and tibia caused by variety of reasons. Awareness of predictable complications is beneficial to prevent or early detection of the expected complication which can improve the risk-benefit balance. Regular follow-up, prudent patient selection, shorter fixator’s time and particular attention during the process are necessary to reduce the related complications.
Acknowledgements
Not applicable.
Abbreviations
- ASAMIA
Association for the Study and Application of the Method of Ilizarov criteria
- DS
Defect size
- DRL
Distraction regenerate length
- DT
Docking time
- CT
Regenerate consolidation time
- EFT/ET
External fixation time
- EFI
External fixation index
- ROM
Range of motion
- ESR
Erythrocyte sedimentation rate
- CRP
C-reactive protein
- AUC
Area under the curve
- ROC
Receiver operating characteristic
- ULRA
Univariate logistic regression analysis
- MLRA
Multivariate logistic regression analysis
Authors’ contributions
YSL: Conducted the study. Collected, analyzed and interpreted the data. Wrote the manuscript. MY: Designed the study. Interpreted the data. Edited the manuscript. ZHL: Statistical analyzed and interpreted the data. JLL: Created and statistical analyzed the data. CM: Planned the project. Reviewed the manuscript. AY: Planned the project. Reviewed the manuscript. Final approval of the version to be submitted: YSL, MY, ZHL, JLL, CM, AY. The author(s) read and approved the final manuscript.
Funding
This work was supported by the grants from National Natural Science Foundation of China (No. 81560357 and 81760397). The funding body was involved in the collection, analysis, and interpretation of data by supporting with salary for the time needed. They were not involved in the design or writing the manuscript.
Availability of data and materials
The datasets analysed during the current study are available from the corresponding author on reasonable request.
Ethics approval and consent to participate
This retrospective study was approved by the Ethics Committee of The First Affiliated Hospital of Xinjiang Medical University. Informed consent was waived due to the retrospective nature of this study.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no conflict of interest.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Yanshi Liu and Maimaiaili Yushan contributed equally to this work.
Contributor Information
Chuang Ma, Email: 8212682@qq.com.
Aihemaitijiang Yusufu, Email: ahmatjang@163.com.
References
- 1.Lasanianos NG, Kanakaris NK, Giannoudis PV. Current management of long bone large segmental defects. Orthopaedics and Trauma. 2010;24(2):149–163. doi: 10.1016/j.mporth.2009.10.003. [DOI] [Google Scholar]
- 2.Reichert JC, Saifzadeh S, Wullschleger ME, Epari DR, Schutz MA, Duda GN, Schell H, van Griensven M, Redl H, Hutmacher DW. The challenge of establishing preclinical models for segmental bone defect research. BIOMATERIALS. 2009;30(12):2149–2163. doi: 10.1016/j.biomaterials.2008.12.050. [DOI] [PubMed] [Google Scholar]
- 3.Aronson J, Johnson E, Harp JH. Local bone transportation for treatment of intercalary defects by the Ilizarov technique. Biomechanical and clinical considerations Clin Orthop Relat Res. 1989;243:71–79. [PubMed] [Google Scholar]
- 4.Osterman AL, Bora FW. Free vascularized bone grafting for large-gap nonunion of long bones. Orthop Clin North Am. 1984;15(1):131–142. [PubMed] [Google Scholar]
- 5.Papineau LJ. Excision-graft with deliberately delayed closing in chronic osteomyelitis. Nouv Press Med. 1973;2(41):2753–2755. [PubMed] [Google Scholar]
- 6.Rose RE. The Ilizarov technique in the treatment of tibial bone defects. Case reports and review of the literature. West Indian Med J. 2002;51(4):263–267. [PubMed] [Google Scholar]
- 7.Baumgart R, Schuster B, Baumgart T. Callus distraction and bone transport in the treatment of bone defects. ORTHOPADE. 2017;46(8):673–680. doi: 10.1007/s00132-017-3441-3. [DOI] [PubMed] [Google Scholar]
- 8.Borzunov DY, Balaev PI, Subramanyam KN. Reconstruction by bone transport after resection of benign tumors of tibia: a retrospective study of 38 patients. Indian J Orthop. 2015;49(5):516–522. doi: 10.4103/0019-5413.164042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Spiegl U, Patzold R, Friederichs J, Hungerer S, Militz M, Buhren V. Clinical course, complication rate and outcome of segmental resection and distraction osteogenesis after chronic tibial osteitis. Injury. 2013;44(8):1049–1056. doi: 10.1016/j.injury.2013.05.003. [DOI] [PubMed] [Google Scholar]
- 10.Vesely R, Prochazka V. Callus distraction in the treatment of post-traumatic defects of the femur and tibia. Acta Chir Orthop Traumatol Cechoslov. 2016;83(6):388–392. [PubMed] [Google Scholar]
- 11.Rohilla R, Siwach K, Devgan A, Singh R, Wadhwani J, Ahmed N. Outcome of distraction osteogenesis by ring fixator in infected, large bone defects of tibia. J Clin Orthop Trauma. 2016;7(Suppl 2):201–209. doi: 10.1016/j.jcot.2016.02.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Sadek AF, Laklok MA, Fouly EH, Elshafie M. Two stage reconstruction versus bone transport in management of resistant infected tibial diaphyseal nonunion with a gap. Arch Orthop Trauma Surg. 2016;136(9):1233–1241. doi: 10.1007/s00402-016-2523-8. [DOI] [PubMed] [Google Scholar]
- 13.Tetsworth K, Paley D, Sen C, Jaffe M, Maar DC, Glatt V, Hohmann E, Herzenberg JE. Bone transport versus acute shortening for the management of infected tibial non-unions with bone defects. Injury. 2017;48(10):2276–2284. doi: 10.1016/j.injury.2017.07.018. [DOI] [PubMed] [Google Scholar]
- 14.Yin P, Zhang L, Li T, Zhang L, Wang G, Li J, Liu J, Zhou J, Zhang Q, Tang P. Infected nonunion of tibia and femur treated by bone transport. J Orthop Surg Res. 2015;10:49. doi: 10.1186/s13018-015-0189-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Aktuglu K, Erol K, Vahabi A. Ilizarov bone transport and treatment of critical-sized tibial bone defects: a narrative review. J Orthop Traumatol. 2019;20(1):22. doi: 10.1186/s10195-019-0527-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Girard PJ, Kuhn KM, Bailey JR, Lynott JA, Mazurek MT. Bone transport combined with locking bridge plate fixation for the treatment of tibial segmental defects: a report of 2 cases. J Orthop Trauma. 2013;27(9):e220–e226. doi: 10.1097/BOT.0b013e31827069b9. [DOI] [PubMed] [Google Scholar]
- 17.Iacobellis C, Berizzi A, Aldegheri R. Bone transport using the Ilizarov method: a review of complications in 100 consecutive cases. Strategies Trauma Limb Reconstr. 2010;5(1):17–22. doi: 10.1007/s11751-010-0085-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Krappinger D, Irenberger A, Zegg M, Huber B. Treatment of large posttraumatic tibial bone defects using the Ilizarov method: a subjective outcome assessment. Arch Orthop Trauma Surg. 2013;133(6):789–795. doi: 10.1007/s00402-013-1712-y. [DOI] [PubMed] [Google Scholar]
- 19.Liodakis E, Kenawey M, Krettek C, Ettinger M, Jagodzinski M, Hankemeier S. Segmental transports for posttraumatic lower extremity bone defects: are femoral bone transports safer than tibial? Arch Orthop Trauma Surg. 2011;131(2):229–234. doi: 10.1007/s00402-010-1129-9. [DOI] [PubMed] [Google Scholar]
- 20.Kocaoglu M, Eralp L, Rashid HU, Sen C, Bilsel K. Reconstruction of segmental bone defects due to chronic osteomyelitis with use of an external fixator and an intramedullary nail. J Bone Joint Surg Am. 2006;88(10):2137–2145. doi: 10.2106/JBJS.E.01152. [DOI] [PubMed] [Google Scholar]
- 21.Paley D, Catagni MA, Argnani F, Villa A, Bijnedetti GB, Cattaneo R. Ilizarov Treatment of Tibial Nonunions With Bone Loss. Clin Orthop Relat R. 1989;&NA;(241). [PubMed]
- 22.Borzunov DY. Long bone reconstruction using multilevel lengthening of bone defect fragments. Int Orthop. 2012;36(8):1695–1700. doi: 10.1007/s00264-012-1562-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Borzunov DY, Chevardin AV. Ilizarov non-free bone plasty for extensive tibial defects. Int Orthop. 2013;37(4):709–714. doi: 10.1007/s00264-013-1799-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Paley D. Problems, obstacles, and complications of limb lengthening by the Ilizarov technique. Clin Orthop Relat Res. 1990;250:81–104. [PubMed] [Google Scholar]
- 25.Herzenberg JE, Waanders NA. Calculating rate and duration of distraction for deformity correction with the Ilizarov technique. Orthop Clin North Am. 1991;22(4):601–611. [PubMed] [Google Scholar]
- 26.Ilizarov GA. Clinical application of the tension-stress effect for limb lengthening. Clin Orthop Relat Res. 1990;250:8–26. [PubMed] [Google Scholar]
- 27.Dendrinos GK, Kontos S, Lyritsis E. Use of the Ilizarov technique for treatment of non-union of the tibia associated with infection. J Bone Joint Surg Am. 1995;77(6):835–846. doi: 10.2106/00004623-199506000-00004. [DOI] [PubMed] [Google Scholar]
- 28.Liantis P, Mavrogenis AF, Stavropoulos NA, Kanellopoulos AD, Papagelopoulos PJ, Soucacos PN, Babis GC. Risk factors for and complications of distraction osteogenesis. Eur J Orthop Surg Traumatol. 2014;24(5):693–698. doi: 10.1007/s00590-013-1261-7. [DOI] [PubMed] [Google Scholar]
- 29.Saran N, Hamdy RC. DEXA as a predictor of fixator removal in distraction osteogenesis. Clin Orthop Relat Res. 2008;466(12):2955–2961. doi: 10.1007/s11999-008-0514-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Suger G, Fleischmann W, Hartwig E, Kinzl L. Open segmental bone transport. A therapeutic alternative in post-traumatic and osteitis soft tissue and bone defects. Unfallchirurg. 1995;98(7):381–385. [PubMed] [Google Scholar]
- 31.Wang H, Wei X, Liu P, Fu YH, Wang PF, Cong YX, Zhang BF, Li Z, Lei JL, Zhang K, Zhuang Y. Quality of life and complications at the different stages of bone transport for treatment infected nonunion of the tibia. Medicine (Baltimore) 2017;96(45):e8569. doi: 10.1097/MD.0000000000008569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Hantes ME, Malizos KN, Xenakis TA, Beris AE, Mavrodontidis AN, Soucacos PN. Complications in limb-lengthening procedures: a review of 49 cases. Am J Orthop (Belle Mead NJ) 2001;30(6):479–483. [PubMed] [Google Scholar]
- 33.Noonan KJ, Leyes M, Forriol F, Canadell J. Distraction osteogenesis of the lower extremity with use of monolateral external fixation. A study of two hundred and sixty-one femora and tibiae. J Bone Joint Surg Am. 1998;80(6):793–806. doi: 10.2106/00004623-199806000-00003. [DOI] [PubMed] [Google Scholar]
- 34.Paley D, Maar DC. Ilizarov bone transport treatment for tibial defects. J Orthop Trauma. 2000;14(2):76–85. doi: 10.1097/00005131-200002000-00002. [DOI] [PubMed] [Google Scholar]
- 35.Farmanullah KMS, Awais SM. Evaluation of management of tibial non-union defect with Ilizarov fixator. J Ayub Med Coll Abbottabad. 2007;19(3):34–36. [PubMed] [Google Scholar]
- 36.Magadum MP, Basavaraj YC, Phaneesha MS, Ramesh LJ. Acute compression and lengthening by the Ilizarov technique for infected nonunion of the tibia with large bone defects. J Orthop Surg (Hong Kong) 2006;14(3):273–279. doi: 10.1177/230949900601400308. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets analysed during the current study are available from the corresponding author on reasonable request.