Abstract
Background
Increasing hospice need, a growing shortage of hospice providers, and concerns about in-person services because of coronavirus disease 2019 (COVID-19) require hospices to innovate care delivery.
Measures
This project compared outcomes between hospice reauthorization visits conducted via telehealth and in person. After each visit, providers, patients, and caregivers completed telehealth acceptance surveys, and providers recorded reauthorization recommendations.
Intervention
Providers conducted 88 concurrent in-person and telehealth visits between June and November 2019.
Outcomes
No statistically significant differences in reauthorization recommendations were found between telehealth and in-person visits. Satisfaction with telehealth was high; 88% of patients/caregivers and 78% of providers found telehealth services as effective as in-person visits.
Conclusions/Lessons Learned
Results indicate that telehealth can successfully support clinical decision making for hospice reauthorization. These findings show telehealth to be reliable and acceptable for certain types of hospice care even before COVID-19, which emphasizes its importance both during and after the current public health emergency.
Key Words: Hospice, hospice reauthorization, telehealth, clinical decision making
Key Message
Face-to-face hospice recertification visits impose significant burden for hospice providers and increase risk of COVID-19 exposure. Our findings suggest that telehealth is as reliable as in-person visits for assessing hospice recertification eligibility and is well received among patients and providers. Telehealth holds great promise for improving efficiency without compromising quality.
Introduction
Medicare's hospice benefit provides palliative care, including medical, nursing, psychological, emotional, and spiritual supports, to patients with a life expectancy of six months or less and their families. Hospice providers face growing challenges associated with a rapidly aging population and increased complexity of care. The number of Americans aged 65 and older is projected to rise from 52 million in 2018 to 95 million by 2060.1 According to the National Institute on Aging, approximately 85% of adults older than 65 years have at least one chronic condition and more than 60% have two or more chronic conditions.2 Although the most common primary diagnosis at hospice admission remains cancer,3 patients with cancer diagnoses spend the fewest average days in hospice care per patient, and patients with dementia diagnoses spend the most average days in hospice per patient.4 Early indications suggest that coronavirus disease 2019 (COVID-19) may also have an impact on hospice care because of medical complexity and increased awareness about the importance of end-of-life planning.5 , 6
As of January 1, 2011, the Centers for Medicare and Medicaid Services (CMS) began requiring U.S. hospices to conduct face-to-face (F2F) visits before the 180th-day recertification and each subsequent 60-day recertification to assess a patient's eligibility for continued hospice care. These visits must be conducted by a hospice physician or a hospice nurse practitioner.7 In light of rising health care costs and reductions in reimbursements, including those imposed by sequestration (annual 2% reduction in Medicare spending through 2023), CMS is under more pressure to reduce costs. In 2016, CMS began paying lower rates for routine home care after the first 60 days of hospice care,8 the first major reimbursement change to hospice payment methodology since the Medicare benefit was created in 1982. As the number of people enrolled in hospice and thus overall hospice utilization increases, hospice providers will likely need to find more efficient ways to address patient and caregiver needs.
The number of Medicare decedents using hospice care has also steadily increased from 0.53 million, representing 23% of Medicare decedents, in 2000 to nearly 1.5 million, representing 42% of Medicare decedents, in 2017.9 , 10 Currently, between 1 and 2 million people enroll in hospice services annually. In 2017, Medicare patients received 113.6 million total days of hospice care, at a cost of $18.99 billion. More than 20% of these patients received more than 180 days of care.10 As patients become more aware of the benefits of hospice services and as enrollment in hospice continues to increase, more patients are expected to follow an extended hospice trajectory and require ongoing recertification of hospice benefits.
The requirement that recertification visits be conducted F2F places increasing strain on limited physician and nursing resources. According to the American Academy of Hospice and Palliative Medicine, there are only 6400 active Hospice and Palliative Medicine-certified physicians in the U.S. as of 2016.11 The need for Hospice and Palliative Medicine physicians is projected to grow between 10,600 and 24,000 by 2040;12 in addition, early indications are that need may increase even further than anticipated because of increased hospice enrollment associated with COVID-19. Although not as well studied, similar shortages are seen among advanced practice providers, nurses, chaplains, and social workers.13 Travel time required to conduct F2F recertification visits has a large impact on provider productivity and the cost of delivering patient care, particularly in rural areas, where staffing shortages are often more prominent. Although some people enter hospice as inpatients, most hospice patients receive care at home. Nursing homes and assisted living facilities may be included in this category as such facilities are often the residents' homes. A national study of patients who received routine hospice care between 2009 and 2014 showed that 48.7% received hospice care in private homes, 33.6% in nursing homes, and 17.7% in assisted living facilities.14
The growing number of older adults experiencing prolonged advanced illness and greater acceptance of hospice across a broad range of chronic illnesses and severe acute illness because of COVID-19, coupled with decreasing Medicare reimbursements and staffing shortages, requires hospices to find new and more efficient ways to deliver affordable high-quality care. This project addressed this challenge by evaluating the potential to use telehealth in place of F2F recertification visits. Results were measured by comparing recertification recommendations between in-person and telehealth providers and assessing patient, caregiver, and provider acceptance of telehealth technology.
Methods
This project was reviewed by the Colorado Multiple Institutional Review Board and determined to be quality improvement, not human subjects research. Results were later considered in the context of the Institute for Healthcare Improvement model for improvement.15 , 16
Population
Patients who were receiving hospice care from TRU Community Care and who were scheduled for an upcoming reauthorization visit between June 5, 2019 and November 27, 2019 were invited to participate in this initiative. Recognizing the vulnerable nature of this patient population, the decrease in decisional capacity often experienced by persons near the end of life, and the integral role of the caregiver in hospice care delivery, patients' primary caregivers were also invited to participate. TRU Community Care personnel explained the initiative and obtained agreement from patients and/or caregivers before engaging them in telehealth visits. All patients and/or caregivers who agreed to participate were included in data analysis. Patients and caregivers were paired together in dyads for data collection and analysis purposes. A total of 88 patients were included as participants. Provider data were obtained from those who conducted reauthorization visits either in person or by telehealth during the project period. A total of five providers participated in this initiative.
Data Collection
A standard visit protocol was used for reauthorization visits. In-person and telehealth visits were conducted jointly with the same patients, in effect conducting both types of visit for each patient with both in-person and telehealth providers at the same time. This was done to reduce burden for hospice patients, rather than asking patients to experience two separately scheduled reauthorization visits in a short time frame. Two licensed hospice care providers (physicians or nurse practitioners) participated in each reauthorization visit in addition to in-person nursing staff. In-person physicians were paired with telehealth physicians and in-person nurse practitioners were paired with telehealth nurse practitioners for reauthorization visits to reduce potential bias by provider type. One provider was present in person, and one provider attended via telehealth, using a securely encrypted connection to a tablet computer. Mobile hot spots and in-home wireless networks were used to maximize connection quality. In-person hospice nurses asked patients and caregivers questions according to the visit protocol and announced vital signs and results from physical examinations, whereas providers listened and observed. At the end of the visit, providers asked additional unstructured questions and engaged with patients and caregivers directly. The in-person nurses administered postvisit surveys to patients and caregivers, whereas both providers self-administered their own postvisit surveys. Both providers also recorded their opinion as to whether they would recommend the patient for reauthorization of services based on the information obtained during the visit. These recommendations did not represent binding reauthorization decisions but were to directly ascertain the impact of visit-based information in making a final reauthorization determination. Survey items were drawn from the Telehealth Usability Questionnaire, a validated instrument for measuring telehealth acceptance among both patients and providers.17 All participants were encouraged to share both positive and negative reactions. Hospice personnel entered survey responses into a secure REDCap database for analysis by the evaluation team.18 , 19
Data Analysis
SAS software, Version 9.4 (SAS Institute, Cary, NC) was used for statistical analysis. Descriptive statistics were used to understand the participant population, summarize attitudes toward telehealth, and detect any erroneous values. McNemar's testing was used on paired nominal data with matched pairs of subjects to test for statistical differences in hospice reauthorization recommendations between the two care delivery modes: telehealth visits and in-person visits. In general, McNemar's test is used with two-by-two contingency tables with a dichotomous trait to determine whether there is marginal homogeneity. In this project, the in-person and telehealth visits that took place at the same time with the same patient were considered as a matched pair of observations, with analysis used to detect outcome differences between them. Technology acceptance by patients, caregivers, and hospice care providers was assessed through univariate analysis of survey data collected from patients and caregivers, considered as a dyad, and from providers.
Results
A total of 88 patients were included as participants in the final analysis. One patient/caregiver survey was completed for each patient participant, and two health care provider surveys for each patient were completed separately by in-person and telehealth providers (n = 176; representing 88 telehealth visits and 88 in-person visits conducted concurrently).
Telehealth Visits Compared With In-Person Visits for Hospice Reauthorization
There was no statistically significant difference (P = 0.74; 80% CI) in hospice care reauthorization recommendations made by providers engaging in telehealth visits compared with recommendations made by providers engaging in-person visits. Seventy-eight telehealth visits (88.6%) and 77 in-person visits (87.5%) resulted in aligned reauthorization recommendations. Fig. 1 depicts reauthorization recommendations by visit type.
Fig. 1.
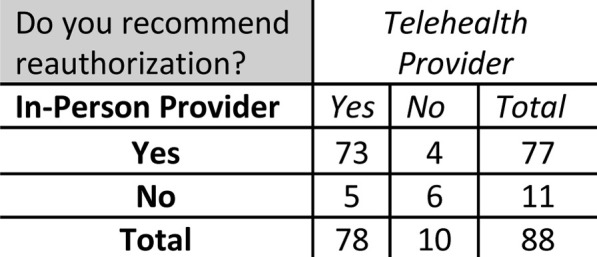
Reauthorization recommendations by visit type.
Patient and Caregiver Perspectives on Telehealth
Table 1 illustrates patient/caregiver assessments of satisfaction with using hospice telehealth services and communicating with their providers via telehealth. On average, the great majority of patients were accepting the service, as represented by an answer of strongly agree or agree. Among respondents, approximately 94% of the time patients felt comfortable and about 6% of the time patients felt neutral about telehealth services. About 88.6% of the time, patients reported being satisfied with the services overall and 91.7% of the time, patients agreed they would use this technology again.
Table 1.
Patient/Caregiver Satisfaction With Hospice Telehealth
| Statement | Strongly Agree (1) |
Agree (2) |
Somewhat Agree (3) |
Neutral (4) |
Somewhat Disagree (5) |
Disagree (6) |
Mean | SD |
|---|---|---|---|---|---|---|---|---|
| N (%) | ||||||||
| Patient satisfaction with hospice telehealth services | ||||||||
| I liked being able to talk to my care provider on a video call today | 33 (39.8) | 32 (38.6) | 8 (9.6) | 10 (12.0) | — | — | 1.94 | .99 |
| I am comfortable talking to my care provider on a video call | 35 (42.2) | 38 (45.8) | 5 (6.0) | 4 (4.8) | — | 1 (1.2) | 1.78 | .91 |
| Statement | Strongly Agree (1) |
Agree (2) |
Somewhat Agree (3) |
Neutral (4) |
Somewhat Disagree (5) |
Disagree (6) |
Strongly Disagree (7) |
Mean |
|---|---|---|---|---|---|---|---|---|
| N (%) | SD | |||||||
| Patient satisfaction with telehealth interactions with providers | ||||||||
| I feel comfortable communicating with the clinician using the telehealth system | 35 (41.2) | 37 (43.5) | 8 (9.4) | 5 (5.9) | — | — | — | 1.79 .84 |
| Telehealth is an acceptable way to receive healthcare services | 26 (31.0) | 36 (42.9) | 7 (8.3) | 6 (7.1) | 7 (8.3) | 2 (2.4) | — | 2.26 1.33 |
| I would use telehealth services again | 34 (40.5) | 33 (39.3) | 10 (11.9) | 5 (6.0) | 1 (1.2) | 1 (1.2) | — | 1.92 1.03 |
| Overall, I am satisfied with this telehealth system | 29 (34.5) | 34 (40.5) | 9 (10.7) | 10 (11.9) | — | 2 (2.4) | — | 2.10 1.15 |
Note: Not all patients answered all survey items.
Table 2 describes patient/caregiver and provider perspectives on the quality and effectiveness of hospice telehealth care interaction. More than 88% of the time, patients believed that talking to their provider in a telehealth visit was as effective as meeting in person. About 91.6% of the time, patients agreed they could easily hear their provider, 90.3% of the time they agreed they could express their opinions, and 84% of the time they felt that they could see their provider as well as if they had met in person. Providers also agreed during most visits that they could talk, hear, and express concern effectively with their patients using the telehealth system (μ = 85.3%). More than 78% of the time, providers felt the service was as effective as meeting in person, whereas 21.6% of the time providers reported that they disagreed or felt neutral about telehealth effectiveness.
Table 2.
Patient/Caregiver and Provider Perception of Hospice Telehealth
| Statement | Strongly Agree (1) |
Agree (2) |
Somewhat Agree (3) |
Neutral (4) |
Somewhat Disagree (5) |
Disagree (6) |
Strongly Disagree (7) |
Mean |
|---|---|---|---|---|---|---|---|---|
| N (%) | SD | |||||||
| Patient/caregiver perception of telehealth quality and effectiveness | ||||||||
| I could easily talk to the clinician using the telehealth system | 32 (38.6) | 36 (43.4) | 5 (6.0) | 7 (8.4) | 1 (1.2) | 2 (2.4) | — | 1.98 1.14 |
| I could hear the clinician clearly using the telehealth system | 32 (38.6) | 37 (44.6) | 7 (8.4) | 4 (4.8) | 1 (1.2) | 2 (2.4) | — | 1.93 1.08 |
| I felt I was able to express myself effectively | 34 (41.5) | 34 (41.5) | 6 (7.3) | 6 (7.3) | 1 (1.2) | 1 (1.2) | — | 1.89 1.04 |
| Using the telehealth system, I could see the clinician as well as if we met in person | 25 (30.9) | 33 (40.7) | 10 (12.4) | 7 (8.6) | 1 (1.2) | 5 (6.2) | — | 2.27 1.35 |
| Provider perception of telehealth quality and effectiveness | ||||||||
| I could easily talk to the patient and/or caregiver using the telehealth system | 49 (55.7) | 21 (22.9) | 7 (8.0) | — | 7 (8.0) | 2 (2.3) | 2 (2.3) | 1.97 1.52 |
| I could easily hear the patient and/or caregiver clearly using the telehealth system | 48 (54.6) | 20 (22.7) | 7 (8.0) | 1 (1.1) | 7 (8.0) | 3 (3.4) | 2 (2.3) | 2.05 1.59 |
| I felt I was able to express myself effectively | 51 (58.0) | 22 (25.0) | 7 (8.0) | 1 (1.1) | 5 (5.7) | — | 2 (2.3) | 1.81 1.33 |
| Using the telehealth system, I could see the patient and/or caregiver as well as if we met in person | 30 (34.1) | 18 (20.4) | 21 (23.9) | 2 (2.3) | 8 (9.1) | 7 (7.9) | 2 (2.3) | 2.65 1.72 |
Note: Not all patients answered all survey items.
Discussion
The results of this project suggest that telehealth and in-person visits are equally effective in supporting needed clinical decision making for hospice service reauthorization. Moreover, high acceptance among patients, caregivers, and providers indicate that telehealth services are not perceived as inferior to in-person visits for recertification, although it should be noted that patients and caregivers (88%) were more likely than providers (78%) to perceive telehealth favorably. These findings are also supported by those from previous research indicating that telehealth solutions used more generally in palliative care and hospice may contribute to cost savings, increased clinical effectiveness, and increased quality of care.20 , 21 Other studies confirm that telehealth increases feelings of connection to providers among palliative care and hospice patients in rural settings,22 and that video telehealth was perceived to improve access and enhance feelings of connection between patients and providers.23 Taken together, the results of this project demonstrate promise for the use of telehealth services to improve hospice provider efficiency and productivity and reduce unnecessary costs without compromising either patient satisfaction or quality of care.
Although the number of patients not recommended for reauthorization during this project was small, inter-rater reliability could be assessed in a larger study to understand potential gaps. This initial project was powered to detect statistical differences for a small effect size at 80% CI. Future studies could support insight into potential differences between patient groups at higher levels of confidence.
The importance of these findings in the context of providing safe and high-quality care during the COVID-19 pandemic caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) cannot be understated. As this work was completed before the initial outbreak, the results reflect telehealth effectiveness and acceptability among a community of patients, caregivers, and providers who were not influenced by fears or concerns about developing COVID-19. The measures taken by CMS to expand support for hospice telehealth services in response to the pandemic are supported by these findings, with additional implications for the appropriateness of implementing these approaches as policy. Moreover, additional direct benefits in this time of crisis are clear.24 , 25 Through using telehealth in pace of F2F visits, exposure risks to both the already-limited hospice and palliative care workforce and to an exceptionally vulnerable patient population can be reduced. Utilization of other scarce resources, such as personal protective equipment, can also be reduced through telehealth. More flexible scheduling because of reductions in travel time may improve timeliness of visits and reduce productivity costs, while also increasing provider capacity to respond to more emergent needs.
Although the results of this project are promising, future research is needed to explore possibilities for sustained impact over time both across patient populations and across the course of patients' hospice experiences. Work is also needed to explore both initial efficacy and effectiveness at scale for telehealth-supported hospice care beyond reauthorization visits. Still, one thing is exceptionally clear: the potential of telehealth to transform hospice care both in this time of crisis and in creating new standards for practice is momentous.
Disclosures and Acknowledgments
This work was supported by the NextFifty Initiative (grant number: 8179). The authors declare no conflicts of interest.
References
- 1.Vespa J., Medina L., Armstrong D.M. U.S. Census Bureau; Washington, DC: 2020. Demographic turning points for the United States: Population projections for 2020 to 2060. Current Population Reports, P25-1144. [Google Scholar]
- 2.NIA. Supporting older patients with chronic conditions 2017. Available from https://www.nia.nih.gov/health/supporting-older-patients-chronic-conditions. Accessed May 18, 2020.
- 3.Rothenberg L., Doberman D., Simon L., Gryczynski J., Cordts G. Patients surviving six months in hospice care: who are they? J Palliat Med. 2014;17:899–905. doi: 10.1089/jpm.2013.0512. [DOI] [PubMed] [Google Scholar]
- 4.Hargraves J., Brennan N. Medicare hospice spending hit $15.8 billion in 2015, varied by locale, diagnosis. Health Aff. 2016;35:1902–1907. doi: 10.1377/hlthaff.2016.0650. [DOI] [PubMed] [Google Scholar]
- 5.Birnstengel G. How COVID-19 is straining hospice care. PBS News Hour. 2020 [Google Scholar]
- 6.Parker J. 2020. Hospice providers quickly opening inpatient units for COVID-19 patients. Chicago, IL: Hospice News. [Google Scholar]
- 7.Centers for Medicare & Medicaid Services (CMS), HHS. Medicare program; hospice wage index for fiscal year 2012. Final rule. Fed Regist. 2011;76:47302–47352. [PubMed] [Google Scholar]
- 8.Stevenson D.G., Huskamp H. Health affairs. 2016. https://www.healthaffairs.org/do/10.1377/hblog20160104.052496/full/ Available from. Accessed May 18, 2020.
- 9.MEDPAC . MEDPAC; Washington, DC: 2019. Hospice services payment system. [Google Scholar]
- 10.NHPCO . 2018 ed. NHPCO; Alexandria, VA: 2019. Facts and figures. [Google Scholar]
- 11.Quigley L., Salsberg E., Lupu D. George Washington University Health Workforce Institute; Washington, DC: 2017. Profile of active hospice and palliative medicine physicians, 2016. [Google Scholar]
- 12.Lupu D., Quigley L., Mehfoud N., Salsberg E. The growing demand for hospice and palliative medicine physicians: will the supply keep up? J Pain Symptom Manage. 2018;55:1216–1223. doi: 10.1016/j.jpainsymman.2018.01.011. [DOI] [PubMed] [Google Scholar]
- 13.Kamal A., Bull J., Swetz K. Future of the palliative care workforce: preview to an impending crisis. Am J Med. 2017;130:113–114. doi: 10.1016/j.amjmed.2016.08.046. [DOI] [PubMed] [Google Scholar]
- 14.Unroe K., Bernard B., Stump T., Tu W., Callahan C. Variation in hospice services by location of care: nursing home versus assisted living facility versus home. J Am Geriat Soc. 2017;65:1490–1496. doi: 10.1111/jgs.14826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Langley G.L., Moen R.D., Nolan K.M. Jossey-Bass; San Francisco, CA: 1996. The improvement guide: A practical approach to enhancing organizational performance. [Google Scholar]
- 16.Deming W.E. Massachusetts Institute of Technology; Cambridge, MA: 1994. The new economics for industry, government, education. [Google Scholar]
- 17.Parmanto B., Lewis A.N., Jr., Bertolet M.H. Development of the telehealth usability questionnaire (TUO) Int J Telerehabil. 2016;8:3–10. doi: 10.5195/ijt.2016.6196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Harris P., Taylor R., Minor B. The REDCap consortium: building an international community of software partners. J Biomed Inform. 2019;95:103208. doi: 10.1016/j.jbi.2019.103208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Harris P., Taylor R., Thielke R. A metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42:377–381. doi: 10.1016/j.jbi.2008.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Rogante M., Giacomozzi C., Grigioni M., Kairy D. Telemedicine in palliative care: a review of systematic reviews. Ann Ist Super Sanita. 2016;52:434–442. doi: 10.4415/ANN_16_03_16. [DOI] [PubMed] [Google Scholar]
- 21.Head B., Schapmire T., Zheng Y. Telehealth in palliative care—a systematic review of patient-reported outcomes. J Hosp Palliat Nurs. 2017;19:130–139. [Google Scholar]
- 22.Bakitas M., Elk R., Astin M. Systematic review of palliative care in the rural setting. Cancer Control. 2015;22:450–464. doi: 10.1177/107327481502200411. [DOI] [PubMed] [Google Scholar]
- 23.Steindal S., Nes A., Godskesen T. Patients' experiences of telehealth in palliative home care: scoping review. J Med Internet Res. 2020;22:e16218. doi: 10.2196/16218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Humphreys J., Schoenherr L., Giovanni E. Rapid implementation of inpatient telepalliative medicine consultations during COVID-19 pandemic. J Pain Symptom Manage. 2020;60 doi: 10.1016/j.jpainsymman.2020.04.001. e54–e59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Calton B., Abedini N., Fratkin M. Telemedicine in the time of coronavirus. J Pain Symptom Manage. 2020;60 doi: 10.1016/j.jpainsymman.2020.03.019. e12–e14. [DOI] [PMC free article] [PubMed] [Google Scholar]


