Abstract
Coronavirus disease 2019 (COVID-19) has quickly spread globally, causing a real pandemic. In this critical scenario, lung cancer patients scheduled for surgical treatment need to continue to receive optimal care while protecting them from an eventual severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection. Adequate use of personal protective equipment (PPE) during aerosol-generating procedures (AGPs) and a COVID-19 specific intraoperative management are paramount in order to prevent cross infections. New suggestions or improvement of existing contagion control guidance are needed, even in case of non-symptomatic patients, possibly responsible for virus spread.
Key Words: COVID-19, 2019-nCoV, coronavirus, lung cancer, thoracic anesthesia, airway management
CORONAVIRUS DISEASE 2019 (COVID-19) has spread rapidly throughout Wuhan, China, and worldwide,1 giving rise to a public health emergency. This outbreak was declared a pandemic by the World Health Organization on March 11, 2020.2 The pathogen responsible has been identified as a novel enveloped RNA beta-coronavirus named “severe acute respiratory syndrome coronavirus 2” (SARS-CoV-2).3 This infection causes clusters of severe respiratory illness similar to severe acute respiratory syndrome coronavirus (SARS-CoV).1 SARS-CoV-2 mostly spreads via droplets, contact, and natural aerosols from human to human. Although the transmission source of COVID-19 is mainly through infected symptomatic patients,4 human-to-human transmission can occur during the asymptomatic incubation period of COVID-19 (ranging from 2- to- 14 days).5 , 6 The determined viral load was found to be comparable in asymptomatic and symptomatic patients with COVID-19, with a possible viral transmission from asymptomatic or minimally symptomatic patients to other persons.7 , 8
Elective surgery deferral, along with adopting workflow patterns to control infection pathways, have been introduced to prevent nosocomial COVID-19 spread.9 From this perspective, nonemergency surgery in COVID-19–positive patients should be postponed. In spite of this critical scenario, lung cancer patients scheduled for surgical treatment need to continue to receive adequate care while protecting them from undergoing surgery during a simultaneous SARS-CoV-2 infection.10 During the COVID-19 outbreak, improvement of contagion prevention and control has become a paramount issue in this novel healthcare setting. The increased awareness of individual protection, sufficient personal protective equipment (PPE), and proper promptness and response would play an important role in lowering the risk of hospital- acquiredinfections.11 Aerosol-generating procedures (AGPs), such as endotracheal intubation and airway surgical or endoscopic procedures, may put healthcare workers (HCWs) at high risk of contagion.12 Moreover, due to lung separation need, airway management for thoracic surgery requires high-complexity strategies that can expose anesthesiologists to an increased risk of infection.
In light of these issues related to the new COVID-19 pandemic, perioperative patient management should be systematically rearranged. To minimize cross-infection risk, new advice or reinforcement of existing infection control guidelines is needed, considering every patient undergoing surgery as potentially positive for infection.
Although no studies have been published yet to support these recommendations due to the exceptional shortness of time of the current emergency, these perspectives were developed by an expert team working in a high-volume thoracic surgery center during the COVID-19 outbreak and could be valuable to prevent nosocomial infections in this challenging situation. This manuscript aims to provide suggestions and special features of anesthetic management for thoracic surgery during the COVID-19 surge, considering also published recommendations.
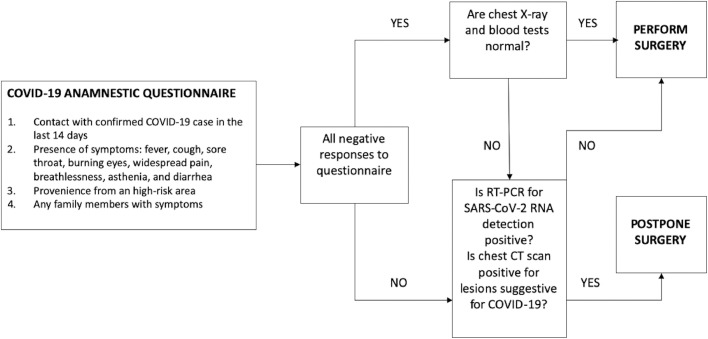
Preoperative Screening
Before hospitalization, patients scheduled for lung surgery should be carefully screened throughout a telephone interview for a possible SARS-CoV-2 infection. A previous contact of the patient with a confirmed case of COVID-19 in the last 2 weeks or the presence of any family members with symptoms should be investigated. Symptoms such as fever, cough, sore throat, burning eyes, widespread pain, breathlessness, asthenia, and diarrhea or a provenience from a high-risk region were also screened. In the case of 1 positive response, patients should undergo reverse transcriptase-polymerase chain reaction (RT-PCR) testing to detect SARS-CoV-2 RNA. This test should be performed with both nasopharyngeal and oropharyngeal swabs to improve the detection rate of nucleic acid and reduce the chance of a false negative.13 , 14 In the case of RT-PCR unavailability, chest computed tomography (CT) has shown high sensitivity, and it could be a useful and fast diagnostic tool in patients with clinical and epidemiologic features compatible with COVID-19 infection,15 although its role as a screening test is still debated.16 , 17 In the case of all negative responses to the questionnaire, COVID-19–related blood test anomalies such as lymphopenia, increased values of C-reactive protein, lactate dehydrogenase, erythrocyte sedimentation rate, and D-dimer, as well as low concentrations of serum albumin and hemoglobin18 or x-ray abnormalities (bilateral or peripheral consolidation and/or ground-glass opacities),19 , 20 also require further investigations such as RT-PCR and CT-scan.21 If SARS-CoV-2 infection is diagnosed, surgery should be postponed (at least 7-14 days from the end of symptoms and after a negative swab result). An algorithm summarizing the previously mentioned suggestions for patients’ screening for COVID-19 is shown in Figure 1 .
Fig 1.
COVID-19 anamnestic questionnaire and screening algorithm for patients scheduled for lung elective surgery. COVID-19, coronavirus disease 2019; CT, computed tomography; RT-PCR, reverse transcriptase-polymerase chain reaction; SARS-CoV-2, severe acute respiratory syndrome coronavirus 2.
With the growing pandemic, some authors have also suggested that elective patients should undergo RT-PCR tests for COVID-19 prior to surgery.22 , 23 This intervention could be an effective strategy to prevent possible cross-infection in HCWs and patients in the perioperative setting in high-prevalence areas, always taking into consideration a possible false-negative result.
Perioperative Management
Despite this critical situation, lung malignancy remains the most common cause of cancer death globally, representing a relevant healthcare burden.24 Adequate care should continue to be guaranteed to these patients, and inappropriate surgical delay should be avoided. Nevertheless, with the spreading of the pandemic, healthcare resources could be exhausted in high-prevalence areas, making elective surgery difficult to perform even in cancer patients, especially if an intensive care unit (ICU) is expected to be required in the postoperative course. During the outbreak, the management of patients requiring major oncologic surgery within adapted and often short time frames is a challenging concern. A possible increased susceptibility to COVID-19 due to immunosuppressive changes around surgery should be considered. This condition can accelerate and exacerbate infection progression, increasing the risk of postoperative complications and mortality.25 , 26 The surgical indication should be evaluated carefully, taking into account all the above-mentioned aspects and evaluating a risk/ benefit ratio for each situation based on a multidisciplinary discussion.
Before hospitalization, because hospital resources could be exhausted, it should be ensured that they are still available (eg, hospital bed, ICU). During a hospital stay, any patient with suspected new onset of fever or respiratory symptoms should be isolated (in a single negative- pressure room) and investigated thoroughly to rule out SARS-CoV-2 infection.27
During the hospital stay the number of visitors should be restricted to limit contagion. Social distancing in the common areas should be based on current recommendations provided by the Centers for Disease Control and Prevention, reducing the number of people and trying to maintain a distance (approximately 2 meters) between individuals when possible.23 , 28 All visitors to the hospital should also wear face masks and use 75% alcohol hand sanitizer prior to entry.29
Intraoperative Infection Control Precautions and Personal Protective Equipment
In the hospital setting, standard precautions presume that every patient is potentially infected or colonized with a pathogen that could be transmitted to HCWs.30 For patients suspected to be infected or colonized with infectious agents, additional control measures to effectively prevent transmission are required.31 Airborne precautions are applied by personnel involved in AGPs (tracheal intubation, noninvasive ventilation, tracheotomy, cardiopulmonary resuscitation, manual ventilation before intubation, and bronchoscopy)32 to prevent the spread of infectious agents transmitted by the airborne route. Because airway viral load is estimated to be very high,6 personnel involved in AGPs are at high risk of contagion. In the course of the COVID-19 outbreak, new recommendations or reinforcement of existing infection control guidelines to protect both patients and HCWs are required.31 , 32
During the widespread SARS outbreaks in 2003, the human transmission of SARS-CoV also highlighted the need for vigilance and improvement of infection control measures.31 A systematic review focused on the SARS-CoV epidemic highlighted that HCWs performing endotracheal intubation had a higher risk of viral contagion (odds ratio [OR] 6.6, 95% confidence interval [CI] 2.3-18.9) than other AGPs such as noninvasive ventilation (OR 3.1, 95% CI 1.4-6.8), tracheotomy (OR 4.2, 95% CI 1.5-11.5), and manual ventilation before intubation (OR 2.8, 95% CI 1.3-6.4).33
AGPs should be performed in a negative- pressure/airborne- isolation operating room (OR).32 , 34 If negative pressure is not available, positive- pressure system and air conditioning should be turned off.35 Respirator masks (FFP2 or FFP3, filtering facepiece respirator mask) are the most used PPE to control the transmission of airborne infections, especially in SARS-CoV-2–suspected or infected patients.36
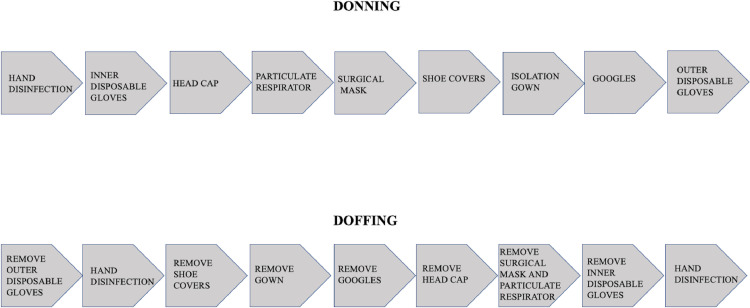
Although particulate respirators are recommended in COVID-19–infected patients and in this difficult scenario PPE are often short in supply, airway management during thoracic anesthesia requires adequate precautions to be applied to all patients. Moreover, procedures for putting on and taking off PPE, patient transport, operating room (OR) managing plan, anesthesia work environment, and anesthesia protocols should be established by each single institution.34
When managing patients with confirmed or suspected infection, shielding health personnel from infection is a priority.34 HCWs protection involves not only the use of PPE but all the strategies for infection prevention and control.37 Using adequate precautions and appropriate PPE, the risk of transmission with AGPs can be significantly decreased. In the OR, rigorous application of COVID-19–specific infection control procedures has effectively demonstrated a low rate of SARS-CoV-2 transmission from patients to healthcare workers despite lengthy exposure time.38
Suggested procedures for putting on and removing PPE39, 40, 41, 42 are shown in Figure 2 .
Fig 2.
Sequences for putting on and removing personal protective equipment (PPE).
Airway Management
During this outbreak, standard precautions are applied in the general population (avoid mass gathering, keep distance greater than 1 meter between 2 people). In the healthcare settings, these precautions have great importance in light of a possible viral transmission during the incubation period or from asymptomatic patients. Several recommendations have been established for COVID-19–infected or-suspected patients, and standardized protective measures are also suggested for OR procedures in unsuspected patients. Therefore, extensive COVID-19–specific anesthesia guidelines need to be developed and applied to prevent nosocomial cross-infections. Moreover, thoracic anesthesia requires advanced airway management and lung isolation; thus, additional precautions are mandatory.42 , 43
The use of a double- lumen tube (DLT) for one-lung ventilation (OLV) is suggested in this critical setting. DLTs have been previously shown to be the primary choice for OLV in 95% of patients due to their ease and rapidity of placement.44 Moreover, DLTs can be checked by auscultation and observation of chest wall movements, differing from bronchial blockers (BBs), which require bronchoscope use for their positioning. During the COVID-19 outbreak, routine bronchoscope use is not recommended,4 , 45 and its use should be restricted to minimize the need to open and manipulate the airway. Bronchoscopy should be reserved for difficult airway management or troubleshooting tube misplacement that cannot be solved with minimal DLT movements.46 If bronchoscopy is required, a disposable tool should be preferred.42
In addition, transthoracic ultrasound (US) scanning has been proposed as a valuable tool to confirm DLT placement. The correct position of the DLT can be predicted when, during OLV, lung US reveals proper lung isolation (absence of “lung sliding” and presence of “lung pulse” seen on the side of surgery and “lung sliding” sign seen on the opposite side), with normal airway pressure and oxygenation.47
All the procedures that could cause aerosolized virus spreading should be avoided. A 3-minute preoxygenation and rapid- sequence induction to avoid bag-mask ventilation are also suggested. The more expert anesthesiologist should perform endotracheal intubation using a videolaryngoscope, preferably with disposable blades and a separate screen to minimize patient contact.40 A complete neuromuscular blockade should be ensured to prevent cough reflex during endotracheal intubation. Rocuronium (1 mg/kg) may be preferred to succinylcholine as a muscle relaxant for the absence of major adverse effects and for its longer half-life, which effectively prevents coughing or vomiting that might occur when the shorter-acting neuromuscular-blocking agent subsides after a failed intubation attempt.35 , 48, 49, 50, 51
Bronchial and tracheal cuffs should be inflated immediately after DLT placement to avoid leakage.
High-efficiency particulate air (HEPA) filters are especially efficient in removing particulates 0.01 to 0.3 μm.52 With the SARS-CoV-2 diameter about 0.1 μm (0.06-0.14 μm), a HEPA filter is likely to be able to capture agglomerate of viruses and drops.53 HEPA filters should be applied between the mask and the breathing circuit and on the inspiratory and expiratory limbs of the breathing circuit (Fig 3 , A).
Fig 3.
(A) HEPA filter applied on the inspiratory and expiratory limbs of the breathing circuit. (B) HEPA filter applied between the double catheter mount and the breathing circuit and on the DLT lumen excluded. (C) Protective transparent drape used during a rigid bronchoscopy. DLT, double lumen tube; HEPA, high-efficiency particulate air.
During mechanical ventilation, any unnecessary circuit disconnections should be avoided. However, OLV management with a DLT usually includes clamping the appropriate lumen and opening the corresponding operative lumen to facilitate lung deflation. For this reason, an additional filter should be added to the open operative DLT lumen54 (Fig 3, B). Application of suction to the operative lung to accelerate lung collapse should be avoided if possible. If suctioning is required it should be performed under apnea or using a closed-circuit system.42
If postoperative ventilation is required, it would be advantageous to use a BB, avoiding the necessity of a catheter exchange and minimizing airway manipulation at the end of surgery. According to standard recommendations, awake fiberoptic intubation with a single- lumen endotracheal tube and BB is also suggested for predicted difficult airway,55 a quite frequent occurrence in thoracic anesthesia (10.8%).44
Extubation, being a high-risk AGP, should be performed in the OR with minimal agitation and coughing to limit virus spread.56 The use of barrier devices over the patient's head, such as clear plastic drapes or an aerosol box, could be helpful and effective in limiting aerosolization and droplet spray that can cause contamination of the surrounding surfaces and HCWs during extubation.57 , 58
A summary of suggested procedures that can be applied to all patients undergoing thoracic anesthesia in this critical period of COVID-19 outbreak is shown in Table 1 .4 , 12 , 30 , 32 , 34 , 37 , 40 , 42 , 49 , 59
Table 1.
Perioperative Recommendations for Thoracic Anesthesia During the COVID-19 Pandemic
| Accurate patient screening throughout a telephone interview before hospitalization |
| Body temperature measurement of all patients before surgery |
| All patients should wear a surgical face mask. |
| Patients should wait in a preoperative holding area adjacent to the OR while maintaining social distancing. Patients should come alone (unless they have an extenuating circumstance requiring a family member to be present). |
| Adequate PPE: double gloves, eye protection, and fluid-resistant gowns Particulate respirators (eg, N95, FFP2, or equivalent standard) |
| Apply HEPA filter between the mask and the breathing circuit. |
| Avoid bag-mask (manual) ventilation prior to intubation. |
| If manual ventilation is necessary, small tidal volumes and two-hands grip to the face should be applied. |
| Preoxygenation with 100% oxygen (3 minutes) through circle circuit and open APL valve |
| Rapid sequence intubation technique (RSI) Complete neuromuscular blockade should be ensured to avoid cough reflex during intubation. |
| Rocuronium (1 mg/kg) may be preferred to succinylcholine as a neuromuscular-blocking agent. |
| Video laryngoscopy with disposable blades (preferably with a display separate from the blade) |
| Orotracheal intubation with DLT and immediate inflation of the tracheal and bronchial cuffs |
| Apply HEPA filter on the DLT lumen excluded. DLT position check by auscultation and observation of chest wall movements No routine bronchoscope use Apply HEPA filter on the inspiratory and expiratory limbs of the breathing circuit and between the double catheter mount and breathing circuit. |
| Avoid circuit disconnections (if needed: ventilator on standby/clamp endotracheal tube). |
| Set the ventilator to standby before each circuit disconnection. |
| Alveolar recruitment maneuvers and pulmonary re-expansion tests performed by circle breathing system |
| Extubation at TOF ratio >0.9 |
| Face mask repositioning to the patient after extubation |
| Postoperative surveillance in preoperative holding area adjacent to OR (avoiding the common areas, eg, recovery room, PACU) |
| If oxygen supply is required, apply nasal cannula preferably, and patients should wear a surgical face mask during O2 therapy. |
Abbreviations: APL, adjustable pressure-limiting valve; DLT, double lumen tube; HEPA, high-efficiency particulate air filter; OR, operating room; PACU, postanesthesia care unit; TOF, train-of-four.
Regional Anesthesia
Although regional anesthesia techniques are not considered AGPs and require standard precautions, because general anesthesia is needed for thoracic surgery anesthetic management, respiratory masks should be used during the procedures.60 Patients should wear surgical face masks to prevent transmission of COVID-19 and virus spread.61 Nerve blocks should be performed with US guidance to reduce the risk of local anesthetic systemic toxicity.62
Since the US machine has numerous surfaces that can serve as viral droplet reservoirs, protecting it with a single-use plastic transparent cover can help to prevent its contamination. The US probe should also be covered along its entire length with a disposable probe sheath.63
In this critical scenario, it is generally recommended that any additional analgesic block techniques should be avoided if adequate pain management can be achieved using alternate regimens such as systemic analgesia.60 Nevertheless, a risk/benefit ratio should be evaluated in each situation, considering that thoracotomy is one of the most painful surgical access and that loco-regional techniques are effective in pain management, reducing opioid use and related adverse effects, such as respiratory depression, sedation, nausea, and vomiting.64 In the authors' experience, applying the previously mentioned suggestions for regional analgesia, performing a minimally invasive peripheral technique, such as the erector spinae plane block, as part of multimodal pain management could be considered a safe and effective procedure for postoperative pain after lung surgery65 and can be a viable choice also during the pandemic. Moreover, because severe acute postoperative pain represents the most important risk factor for chronic pain after thoracic surgery, with a worse quality of life, pain management after surgery should not be disregarded even during this current critical situation.66
Endoscopic Operative Procedures
For airway endoscopic operative procedures, specific precautions should be adopted because of the increased risk of airborne viral transmission. During these high-risk AGPs, the entire staff should wear appropriate PPE and they should be performed in the OR with a negative-pressure/airborne isolation or turning off the positive- pressure system and air conditioning.
Rigid bronchoscopy requires general anesthesia. Topical anesthesia is also recommended to reduce upper airway reflexes and sedative agents’ requirement. To minimize the leak, bronchoscope silicone caps and packing of the oropharynx can be helpful.67 HEPA filter application on each interface to a ventilator is also suggested. To avoid an eventual airborne spread and to limit contamination, a protective transparent drape (Fig 3, C) (eg, covering for portable gamma camera system) can be used to limit contamination without interfering with the procedure.57
Furthermore, the airway management advised for flexible bronchoscopy is the use of controlled ventilation through positioning a supraglottic airway device (SGA). After achieving deep sedation, SGA insertion, and connection to the breathing circuit, the bronchoscope is inserted into the suction port of the swivel connector (Fig 4 ). SGA allows for better airway support and gas exchange while sharing the airway with flexible bronchoscopy.68 Topical anesthesia use remains a necessary approach.69 HEPA filter use is also suggested.
Fig 4.
Disposable bronchoscope insertion through the suction port of the swivel connector and a second-generation supraglottic airway device (i-gel).
Postoperative Management and Patient Transfer
After surgery, patients should not be taken to common areas such as the recovery room or postanesthesia care unit.70 Postoperative surveillance should take place in the preoperative holding area adjacent to the OR. Because oxygen supplementation has been previously identified as an independent risk factor for super-spreading nosocomial outbreaks,71 during oxygen delivery, patients should wear a surgical face mask to prevent droplet transmission, and nasal cannula should be preferred. Patient transport, especially if postoperative mechanical ventilation is required and the patient is kept intubated, could lead to potential lack of compliance with infection control measures and requires special care. During intubated patients’ transfer to the ICU, HCWs should wear adequate PPE, use a single-patient respiratory bag with HEPA filter on the endotracheal tube, and avoid unnecessary disconnections.35 , 72 A “security team” to lead and guarantee clearance of bystanders for the whole designated route ahead of transporters is also advisable.72
Conclusions
In the course of the COVID-19 pandemic, perioperative management of patients scheduled for lung cancer surgery needs to be reassessed. Careful preoperative screening is necessary to identify possible SARS-CoV-2 infections. Because of the complexity of airway management for thoracic anesthesia, intraoperative precautions for contagion prevention should be implemented, with specific recommendations for healthcare providers and with universal application to all patients, even in the noninfected population, to prevent hospital-acquired infections in the OR setting.
During the observation period (February 28, 2020, to April 3, 2020), 105 patients underwent elective thoracic surgery. All patients were submitted to the anamnestic questionnaire before hospitalization. DLT was used in 100 patients, whereas 5 patients were managed throughout with a single- lumen tube and a BB because of predicted difficult airways. All BB were positioned with bronchoscope use. Among the patients managed throughout DLT, 10 patients required bronchoscopy due to tube malposition.
No HCWs or patients undergoing procedures reported SARS-CoV-2 infection in the postoperative course in this high-volume thoracic surgery center. The authors believe that the accurate preoperative selection of patients, combined with the adherence to the above-mentioned infection control procedures specific for thoracic surgery, has yielded positive outcomes.
Conflict of Interest
None.
Footnotes
The authors received no financial support for the research, authorship, and/or publication of this article.
References
- 1.Huang C., Wang Y., Li X. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395:497–506. doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.World Health Organization. WHO declares COVID-19 a pandemic. Available at:https://www.who.int/dg/speeches/detail/whodirector-%0Dgeneral-s-opening-remarks-at-the-media-briefing-on-covid-19—11-%0Dmarch-2020. Accessed April 7, 2020.
- 3.Lu R., Zhao X., Li J. Genomic characterisation and epidemiology of 2019 novel coronavirus: Implications for virus origins and receptor binding. Lancet. 2020;395:565–574. doi: 10.1016/S0140-6736(20)30251-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Chen R., People S. Expert consensus on preventing nosocomial transmission during respiratory care for critically ill patients infected by 2019 novel coronavirus pneumonia. Zhonghua Jie He He Hu Xi Za Zhi. 2020;20:1–21. doi: 10.3760/cma.j.cn112147-20200304-00239. [DOI] [PubMed] [Google Scholar]
- 5.Centers for Disease Control and Prevention. 2019 Novel coronavirus. Available at:https://www.cdc.gov/coronavirus/2019-ncov/about/transmission.html. Accessed March 18, 2020.
- 6.Li Q., Guan X., Wu P. Early transmission dynamics in wuhan, china, of novel coronavirus-infected pneumonia. N Engl J Med. 2020;382:1199–1207. doi: 10.1056/NEJMoa2001316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Chang D., Xu H., Rebaza A. Protecting health-care workers from subclinical coronavirus infection. Lancet Respir Med. 2020;8:e13. doi: 10.1016/S2213-2600(20)30066-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Zou L., Ruan F., Huang M. SARS-CoV-2 viral load in upper respiratory specimens of infected patients. N Engl J Med. 2020;382:1177–1179. doi: 10.1056/NEJMc2001737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Brindle M, Gawande A. Managing COVID-19 in surgical systems. Ann Surg. doi: 10.1097/SLA.0000000000003923. Accessed April 9, 2020. [e-pub ahead of print]. [DOI] [PMC free article] [PubMed]
- 10.Thoracic Surgery Outcomes Research Network I. COVID-19 guidance for triage of operations for thoracic malignancies: A consensus statement from Thoracic Surgery Outcomes Research Network. Ann Thorac Surg. doi: 10.1016/j.athoracsur.2020.03.005. Accessed April 17, 2020. [e-pub ahead of print]. [DOI] [PMC free article] [PubMed]
- 11.Wang J., Zhou M., Liu F. Reasons for healthcare workers becoming infected with novel coronavirus disease 2019 (COVID-19) in China. J Hosp Infect. 2020;105:100‐1. doi: 10.1016/j.jhin.2020.03.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Zuo MZ, Huang YG, Ma WH, et al. Expert recommendations for tracheal intubation in critically ill patients with noval coronavirus disease 2019. Chin Med Sci J. doi: 10.24920/003724. Accessed March 17, 2020. [e-pub ahead of print]. [DOI] [PMC free article] [PubMed]
- 13.Jin Y.H., Cai L., Cheng Z.S. A rapid advice guideline for the diagnosis and treatment of 2019 novel coronavirus (2019-nCoV) infected pneumonia (standard version) Mil Med Res. 2020;7:1–23. doi: 10.1186/s40779-020-0233-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hong K.H., Lee S.W., Kim T.S. Guidelines for laboratory diagnosis of coronavirus disease 2019 (COVID-19) in Korea. Ann Lab Med. 2020;40:351‐60. doi: 10.3343/alm.2020.40.5.351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Fang Y, Zhang H, Xie J, et al. Sensitivity of chest CT for COVID-19: Comparison to RT-PCR. Radiology. doi: 10.1148/radiol.2020200432. Accessed March 17, 2020. [e-pub ahead of print]. [DOI] [PMC free article] [PubMed]
- 16.American Society of Emergency Radiology (ASER). ASER COVID-19 Task Force: FAQs. Available at: www.aser.org/covid-19-faqs/. Accessed May 13, 2020.
- 17.American College of Radiology. ACR recommendations for the use of chest radiography and computed tomography (CT) for suspected COVID-19 infection. Available at: https://www.acr.org/Advocacy-and-Economics/ACR-Position-Statements/Recommendations-for-Chest-Radiography-and-CT-for-Suspected-COVID19-Infection. Accessed May 13, 2020.
- 18.Lippi G., Plebani M. Laboratory abnormalities in patients with COVID-2019 infection. Clin Chem Lab Med. 2020;58:1131–1134. doi: 10.1515/cclm-2020-0198. [DOI] [PubMed] [Google Scholar]
- 19.Kooraki S., Hosseiny M., Myers L. Coronavirus outbreak: What the Department of Radiology should know. J Am Coll Radiol. 2020;17:447–451. doi: 10.1016/j.jacr.2020.02.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Wong HYF, Lam HYS, Fong AH, et al. Frequency and distribution of chest radiographic findings in COVID-19 positive patients [e-pub ahead of print]. Radiology. doi: 10.1148/radiol.2020201160. Accessed April 6, 2020. [DOI] [PMC free article] [PubMed]
- 21.Li Y., Xia L. Coronavirus disease 2019 (COVID-19): Role of chest CT in diagnosis and management. AJR Am J Roentgenol. 2020;214:1280–1286. doi: 10.2214/AJR.20.22954. [DOI] [PubMed] [Google Scholar]
- 22.He Y., Wei J., Bian J. Chinese Society of Anesthesiology expert consensus on anesthetic management of cardiac surgical patients with suspected or confirmed coronavirus disease 2019. J Cardiothorac Vasc Anesth. 2020;34:1397‐401. doi: 10.1053/j.jvca.2020.03.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Li W, Huang J, Guo X, et al. Anesthesia management and perioperative infection control in patients with the novel coronavirus. J Cardiothorac Vasc Anesth. doi: 10.1053/j.jvca.2020.03.035. Accessed May 13, 2020. [e-pub ahead of print]. [DOI] [PMC free article] [PubMed]
- 24.Maconachie R., Mercer T., Navani N. Lung cancer: Diagnosis and management: Summary of updated NICE guidance. BMJ. 2019;364:1–4. doi: 10.1136/bmj.l1049. [DOI] [PubMed] [Google Scholar]
- 25.Besnier E., Tuech J., Schwarz L. We asked the experts: Covid-19 outbreak: Is there still a place for scheduled surgery? Reflection from pathophysiological data. World J Surg. 2020;44:1695‐8. doi: 10.1007/s00268-020-05501-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Lei S, Jiang F, Su W, et al. Clinical characteristics and outcomes of patients undergoing surgeries during the incubation period of COVID-19 infection [e-pub ahead of print]. EClinicalMedicine. doi: 10.1016/j.eclinm.2020.100331. [DOI] [PMC free article] [PubMed]
- 27.Al-Balas M, Al-Balas HI, Al-Balas H. Surgery during the COVID-19 pandemic: A comprehensive overview and perioperative care. Am J Surg. doi: 10.1016/j.amjsurg.2020.04.018. Accessed May 13, 2020. [e-pub ahead of print]. [DOI] [PMC free article] [PubMed]
- 28.Centers for Disease Control and Prevention. Preventing COVID-19 spread in communities. Available at: https://www.cdc.gov/coronavirus/2019-ncov/community/index.html. Accessed May 14, 2020.
- 29.Schwartz J, King C, Yen M. Protecting healthcare workers during the coronavirus disease 2019 (COVID-19) outbreak : Lessons from Taiwan's severe acute respiratory syndrome response. Clin Infect Dis. doi: 10.1093/cid/ciaa255. Accessed May 13, 2020. [e-pub ahead of print]. [DOI] [PMC free article] [PubMed]
- 30.Centers for Disease Control and Prevention. Interim infection prevention and control recommendations for patients with confirmed 2019 novel coronavirus (2019-nCoV) or persons under investigation for 2019-nCoV in healthcare settings. Available at: https://www.cdc.gov/coronavirus/2019-nCoV. Accessed March 17, 2020.
- 31.Siegel J.D., Rhinehart E., Jackson M. Guideline for Isolation Precautions: Preventing Transmission of Infectious Agents in Healthcare Settings. 2007 doi: 10.1016/j.ajic.2007.10.007. Last update July 2019. Available at: https://www.cdc.gov/infectioncontrol/guidelines/isolation/index.html. Accessed March 17, 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Peng P.W.H., Ho P.L., Hota S.S. Outbreak of a new coronavirus: What anaesthetists should know. Br J Anaesth. 2020;124:497‐501. doi: 10.1016/j.bja.2020.02.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Tran K., Cimon K., Severn M. Aerosol generating procedures and risk of transmission of acute respiratory infections to healthcare workers: A systematic review. PLoS One. 2012;7:e35797. doi: 10.1371/journal.pone.0035797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Kim H.J., Ko J.S., Kim T.Y. Recommendations for anesthesia in patients suspected of coronavirus 2019-nCoV infection. Korean J Anesthesiol. 2020;73:89‐91. doi: 10.4097/kja.20110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Chen X., Liu Y., Gong Y. Perioperative management of patients infected with the novel coronavirus recommendation from the joint task force of the Chinese Society of Anesthesiology and the Chinese Association of Anesthesiologists. Anesthesiology. 2020;132:1307‐16. doi: 10.1097/ALN.0000000000003301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Centers for Disease Control and Prevention. Strategies for optimizing the supply of N95 respirators. Available at:https://www.cdc.gov/coronavirus/2019-ncov/hcp/respirators-strategy/index.html. Accessed March 24, 2020.
- 37.World Health Organization. Novel coronavirus (2019-nCoV) technical guidance: Infection prevention and control. Available at:https://www.who.int/emergencies/diseases/novel-coronavirus-2019/technical-guidance/infection-prevention-and-control. Accessed March 17, 2020.
- 38.Zhao S., Ling K., Yan H. Anesthetic management of patients with suspected or confirmed 2019 novel coronavirus infection during emergency procedures. J Cardiothorac Vasc Anesth. 2020;34:1125‐31. doi: 10.1053/j.jvca.2020.02.039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.World Health Organization. Clinical management of severe acute respiratory infection when novel coronavirus (2019-nCoV) infection is suspected: Interim guidance. Available at:https://www.who.int/publications-detail/clinical-%0D%0Amanagement-of-severe-acute-respiratory-infection-%0D%0Awhen-novel-coronavirus-(ncov)-infection-is-suspected.%0D%0A. Accessed March 27, 2020.
- 40.Sorbello M., El-Boghdadly K., Di Giacinto I. The Italian coronavirus disease 2019 outbreak: Recommendations from clinical practice. Anaesthesia. 2020;75:724‐32. doi: 10.1111/anae.15049. [DOI] [PubMed] [Google Scholar]
- 41.Luo M., Cao S., Weil L. Precautions for intubating patients with COVID-19. Anesthesiology. 2020;132:1616‐8. doi: 10.1097/ALN.0000000000003288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Şentürk M, El Tahan MR, Szegedi LL, et al. Thoracic anesthesia of patients with suspected or confirmed 2019 novel coronavirus infection: Preliminary recommendations for airway management by the EACTA Thoracic Subspecialty Committee. J Cardiothorac Vasc Anesth. doi: 10.1053/j.jvca.2020.03.059. [e-pub ahead of print]. [DOI] [PMC free article] [PubMed]
- 43.Thornton M, Reid D, Shelley B, et al. Management of the airway and lung isolation for thoracic surgery during the COVID-19 pandemic: Recommendations for clinical practice endorsed by the Association for Cardiothoracic Anaesthesia and Critical Care and the Society for Cardiothoracic Surgery in Great Britain and Ireland. Anaesthesia. doi: 10.1111/anae.15112. Accessed May 13, 2020. [e-pub ahead of print]. [DOI] [PubMed]
- 44.Langiano N., Fiorelli S., Deana C. Airway management in anesthesia for thoracic surgery: A “real life” observational study. J Thorac Dis. 2019;11:3257–3269. doi: 10.21037/jtd.2019.08.57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Wahidi MM, Shojaee S, Lamb CR, et al. The use of bronchoscopy during the COVID-19 pandemic: CHEST/AABIP guideline and expert panel report. Chest. doi: 10.1016/j.eclinm.2020.100331. Accessed May 13, 2020. [e-pub ahead of print]. [DOI] [PMC free article] [PubMed]
- 46.Brodsky J.B., Lemmens H.J.M. Left double-lumen tubes: Clinical experience with 1,170 patients. J Cardiothorac Vasc Anesth. 2003;17:289–298. doi: 10.1016/s1053-0770(03)00046-6. [DOI] [PubMed] [Google Scholar]
- 47.Parab S.Y., Divatia J.V., Chogle A. A prospective comparative study to evaluate the utility of lung ultrasonography to improve the accuracy of traditional clinical methods to confirm position of left sided double lumen tube in elective thoracic surgeries. Indian J Anaesth. 2015;59:476–481. doi: 10.4103/0019-5049.162983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Misiołek H., Tombarkiewicz M., Zajaczkowska-Druzba K. Rocuronium vs atracurium vs suxamethonium for double-lumen endobronchial tube intubation. Anestezjol Intens Ter. 2009;41:68–72. [PubMed] [Google Scholar]
- 49.Cheung J.C., Ho L.T., Cheng J.V. Staff safety during emergency airway management for COVID-19 in Hong Kong. Lancet Respir Med. 2020;8:e19. doi: 10.1016/S2213-2600(20)30084-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Swaminathan A.K., Mallemat H. Rocuronium should be the default paralytic in rapid sequence intubation. Ann Emerg Med. 2018;71:397‐8. doi: 10.1016/j.annemergmed.2017.04.039. [DOI] [PubMed] [Google Scholar]
- 51.Tran D.T., Newton E.K., Mount V.A. Rocuronium versus succinylcholine for rapid sequence induction intubation. Cochrane Database Syst Rev. 2015;2015 doi: 10.1002/14651858.CD002788.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Centers for Disease Control and Prevention. Guidance for filtration and air-cleaning systems to protect building environments from airborne chemical, biological, radiological attacks. Available at:https://www.cdc.gov/niosh/docs/2003-136/default.html. Accessed May 13, 2020.
- 53.Zhu N., Zhang D., Wang W. A novel coronavirus from patients with pneumonia in China, 2019. N Engl J Med. 2020;382:727–733. doi: 10.1056/NEJMoa2001017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Tryphonopoulos P, McFaul C, Gagne S, et al. COVID-19 and one lung ventilation. Anesth Analg. doi: 10.1213/ANE.0000000000004915. Accessed May 13, 2020. [e-pub ahead of print]. [DOI] [PMC free article] [PubMed]
- 55.Merli G., Guarino A., Della Rocca G. Airway management in thoracic anesthesia and lung. Minerva Anestesiol. 2009;75:59–96. [PubMed] [Google Scholar]
- 56.Yang M., Dong H., Lu Z. Role of anaesthesiologists during the COVID-19 outbreak in China. Br J Anaesth. 2020;124:666‐9. doi: 10.1016/j.bja.2020.03.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Matava C.T., Yu J., Denning F.S. Clear plastic drapes may be effective at limiting aerosolization and droplet spray during extubation: Implications for COVID-19. Can J Anesth. 2020;67:902–904. doi: 10.1007/s12630-020-01649-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Girgis AM, Merna NA, Tilvawala CG, et al. Novel coronavirus disease 2019 (COVID-19) aerosolization box: Design modifications for patient safety. J Cardiothorac Vasc Anesth. doi: 10.1053/j.jvca.2020.05.001. Accessed May 13, 2020. [e-pub ahead of print]. [DOI] [PMC free article] [PubMed]
- 59.Brewster D.J., Chrimes N., Do T.B.T. Consensus statement: Safe airway society principles of airway management and tracheal intubation specific to the COVID-19 adult patient group. Med J Aust Adv. 2020;212:472–481. doi: 10.5694/mja2.50598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.American Society of Regional Anesthesia and Pain Medicine. Practice recommendations on neuraxial anesthesia and peripheral nerve blocks during the COVID-19 pandemic—A joint statement by the American Society of Regional Anesthesia and Pain Medicine (ASRA) and European Society of Regional Anesthesia and Pain Therapy. Available at:https://www.asra.com/page/2905/practice-recommendations-on-neuraxial-anesthesia-and-peripheral-nerve-blocks-dur. Accessed May 13, 2020.
- 61.He Y, Wei J, Bian J, et al. Regional anesthesia during the COVID-19 pandemic: A time to reconsider practices? (Letter #2). Can J Anaesth. doi: 10.1007/s12630-020-01682-9. Accessed May 6, 2020. [e-pub ahead of print]. [DOI]
- 62.El-Boghdadly K., Pawa A., Chin K.J. Local anesthetic systemic toxicity: Current perspectives. Local Reg Anesth. 2018;11:35–44. doi: 10.2147/LRA.S154512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Lie S.A., Wong S.W., Wong L.T. Practical considerations for performing regional anesthesia: Lessons learned from the COVID-19 pandemic. Can J Anesth. 2020;67:885–892. doi: 10.1007/s12630-020-01637-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Kehlet H., Wilkinson R.C., Fischer H.B. PROSPECT: Evidence-based, procedure-specific postoperative pain management. Best Pr Res Clin Anaesthesiol. 2007;21:149–159. doi: 10.1016/j.bpa.2006.12.001. [DOI] [PubMed] [Google Scholar]
- 65.Fiorelli S, Leopizzi G, Menna C, et al. Ultrasound-guided erector spinae plane block versus intercostal nerve block for post-minithoracotomy acute pain management: A randomized controlled trial. J Cardiothorac Vasc Anesth. doi: 10.1053/j.jvca.2020.01.026. Accessed May 13, 2020. [e-pub ahead of print]. [DOI] [PubMed]
- 66.Fiorelli S, Cioffi L, Menna C, et al. Chronic pain after lung resection: Risk factors, neuropathic pain, and quality of life. J Pain Symptom Manage. doi: 10.1016/j.jpainsymman.2020.03.012. Accessed May 6, 2020. [e-pub ahead of print]. [DOI] [PubMed]
- 67.Chadha M., Kulshrestha M., Biyani A. Anaesthesia for bronchoscopy. Indian J Anaesth. 2015;59:565–573. doi: 10.4103/0019-5049.165851. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Alon D., Pertzov B., Gershman E. The safety of laryngeal mask airway-assisted bronchoscopy versus standard nasal bronchoscopy. Respiration. 2017;93:279–284. doi: 10.1159/000456551. [DOI] [PubMed] [Google Scholar]
- 69.José R.J., Shaefi S., Navani N. Anesthesia for bronchoscopy. Curr Opin Anaesthesiol. 2014;27:453–457. doi: 10.1097/ACO.0000000000000087. [DOI] [PubMed] [Google Scholar]
- 70.Tang L.Y., Wang J. Anesthesia and COVID-19: What we should know and what we should do. Semin Cardiothorac Vasc Anesth. 2020;24:127‐37. doi: 10.1177/1089253220921590. [DOI] [PubMed] [Google Scholar]
- 71.Yu I.T., Xie Z.H., Tsoi K.K. Why did outbreaks of severe acute respiratory syndrome occur in some hospital wards but not in others? Clin Infect Dis. 2007;44:1017–1025. doi: 10.1086/512819. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Liew M.F., Siow W.T., Yau Y.W. Safe patient transport for COVID-19. Crit Care. 2020;24:94. doi: 10.1186/s13054-020-2828-4. [DOI] [PMC free article] [PubMed] [Google Scholar]