Introduction
Coronavirus Disease 2019 (COVID-19), caused by the novel severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), has been spreading in many countries, and this coronavirus epidemic has been labeled a world pandemic by the WHO.1 2 Although the epidemic has been basically controlled by the cooperation of central and local governments in China, nevertheless more than 3000 medical staff have been infected during the fight against the virus.3 4
Stroke is a common disease with high morbidity, high disability, high mortality and high recurrence rate. Neurointervention plays an important role in the diagnosis and treatment of stroke, especially for acute stroke, which could significantly reduce the mortality and disability rates.5 6 During the epidemic, neurointerventional staff are faced with the dual pressures of disease treatment and infection prevention. Therefore, the Chinese Federation of Interventional and Therapeutic Neuroradiology (CFITN) and the International Society for Neurovascular Disease (ISNVD) have called on neurointerventional specialists from departments of neurosurgery, neurology, and interventional radiology to discuss and compile this expert consensus based on their working experience in fighting against the epidemic and related regulations issued by National Health Commission7–9 The aim was to provide protective strategies and recommendations for medical staff to carry out neurointerventional procedures under the circumstances of the COVID-19 epidemic, and to provide references for neurointerventional physicians around the world.
Basic principles
First, according to clinical needs, neurointerventional surgery can be divided into emergency and elective surgery (or non-emergency surgery). It is recommended to suspend non-emergency neurointerventional surgeries, especially for the highly suspected and confirmed patients during the epidemic period.
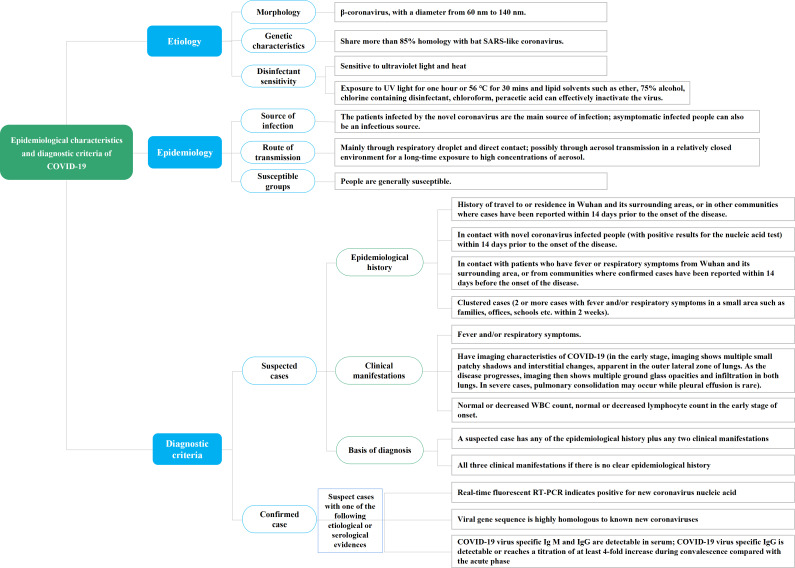
Second, neurointerventional staff should participate in the training to update their knowledge of the epidemic, especially the epidemiological characteristics and diagnostic criteria of COVID-19 (figure 1), the stratified precautions for medical staff during the COVID-19 epidemic (table 1), and the instructions regarding common disinfection supplies, etc. At the same time, temperature detection should be strengthened when entering the outpatient department, ward and catheterization lab. In addition, it is recommended to strengthen the immunity of staff in their daily life through reasonable rest, moderate exercise and a well-balanced diet.
Figure 1.
Epidemiological characteristics and diagnostic criteria of COVID-19. RT-PCR, reverse transcriptase polymerase chain reaction; SARS, severe acute respiratory syndrome; UV, ultraviolet; WBC, white blood cell.
Table 1.
Stratified precautions for medical staff during COVID-19 epidemic
| Grade | Scope of application | Protection requirements |
| Level protection I | (1) Observation for person contacting with confirmed COVID-19 cases. (2) Neurointerventional medical staff working in outpatient department | Wear white coats, disposable caps, disposable isolation gowns, disposable gloves and disposable surgical masks (replaced every 4 hours or replaced once contamination occurs) |
| Level protection II | (1) Neurointerventional staff conducting epidemiological investigations on close contacts, suspected or confirmed cases. (2) Neurointerventional staff who conduct diagnosis, treatment and disinfection in the isolation observation room, isolation ward or block | Wear disposable caps, medical respirators (such as N95 mask), anti-fog safety goggles or anti-fog protective shields, medical protective suits, disposable gloves, and disposable shoe covers |
| Level protection III | (1) Neurointerventional staff performing close procedures that may produce aerosol, such as endotracheal intubation, nebulization treatment, sputum induction, tracheotomy, chest physiotherapy, nasopharyngeal aspiration, positive pressure ventilation, high frequency oscillatory ventilation, cardiopulmonary resuscitation and postmortem lung biopsy, etc. (2) Neurointerventional staff who process the blood, secretions, feces, and bodies of the confirmed cases | Wear full face respirators or positive pressure respirators, medical protective suits, disposable gloves, and disposable shoe covers |
Third, medical institutions should inform patients without urgent medical to postpone treatment through extensive publicity and recommend them to consult health problems on the online clinic. Patients should wear facial masks and keep a distance of more than 1 meter from others during the whole period in hospital.
Infection prevention and control strategies for neurointerventional general outpatient and emergency outpatient
Infection prevention and control procedures
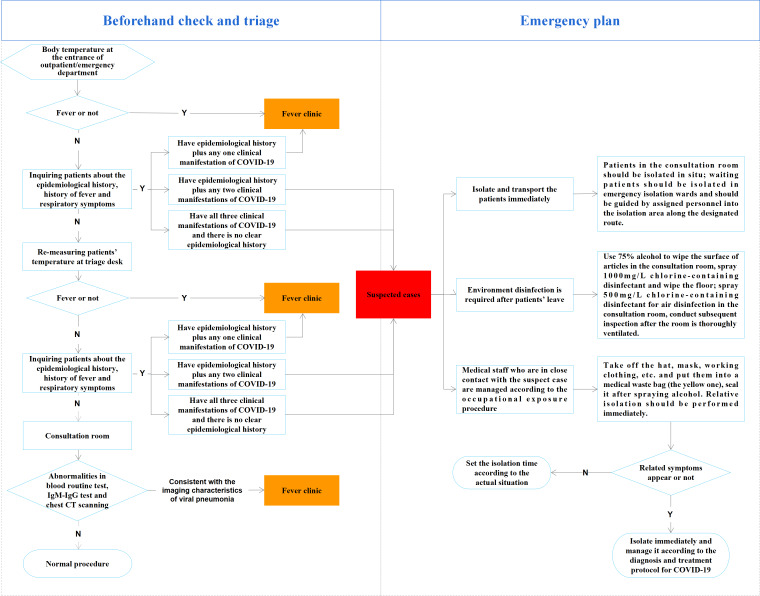
Neurointerventional emergency services should be provided under the unified management of the hospital. An appointment system should be implemented at the outpatient department. At the entrance of the outpatient and the triage desk, medical staff should repeatedly ask the patient and their companions about the epidemiological history, whether there is fever and other respiratory symptoms, etc, and should provide facial masks and instruct them to wear the masks properly. When patients enter the office, interventional physicians should not only inquire about their epidemiological history and related symptoms again, but also check the results of routine blood test, IgM-IgG antibody test (it depends on the hospital), as well as the chest CT findings. Once a suspect is found during the treatment, it is suggested they be transferred to the fever clinic for further exclusion, and the suspected cases should be transferred and isolated immediately according to the emergency plan. Environmental disinfection should be carried out straight away.10 Medical personnel in contact with patients are managed according to the occupational exposure procedures. The specific procedure and emergency plan are shown in figure 2.
Figure 2.
Standard screening procedure in outpatient/ emergency department and emergency plan.
Strategies of self-protection for medical staff
Standard prevention procedure during treatment: Physicians should wear white coats, caps and surgical masks. In high-infected areas, safety goggles, N95 respirator and disposable isolation gowns should also be worn. Physicians should strictly follow the Hand Hygiene Rules for Medical Staff 11 to keep good hand hygiene. Once a suspected case is found, the physician should remain cool-headed and immediately leave the office to upgrade the protection level.
Infection prevention and control strategies for neurointerventional ward and block
Infection prevention and control procedures
An emergency isolation ward should be set up for the isolation and treatment of suspected or confirmed cases. Epidemic prevention and control procedures should be established and adequate disinfection and protective supplies for acute respiratory infections should be prepared in advance. Patients with negative test results can be admitted to the general ward. For suspected patients, the expert group for COVID-19 in the hospital should hold a consultation to determine whether they were infected. If it cannot be determined, the patient should be sent to a separate ward and further confirmed as soon as possible. Suspected or confirmed patients should be admitted to the designated ward for COVID-19, and hospitals without the conditions should not accept those patients and should transfer them to other designated hospitals. The spatial distance between beds in the ward should be more than 1 meter; the population density in the ward, and the number of accompanying nursing personnel and visitors, should be minimized.
Strategies of self-protection for medical staff
Medical staff should strictly implement the stratified precautions for medical staff during the COVID-19 epidemic, they should avoid unnecessary contact when communicating with patients, and keep a safe distance of more than 1 meter.
Infection prevention and control strategies for the catheterization lab
Medical supplies preparation
In addition to general surgical instruments, sufficient personal protective equipment should be provided, including N95 respirators, safety goggles or face shields, isolation gowns, protective suits, shoe covers or boot covers, and full face respirators, etc.
Requirements for the operating room
In principle, diagnosis and treatment of the suspected patient should be carried out in a negative pressure interventional room. If it is not available, a dedicated operating room should be designated. The catheterization lab is preferably a separate room. If there is more than one operating room in the lab, the room closest to the entrance should be selected. The laminar air flow, ventilation and air-conditioning system should be turned off before any medical practice, and a cabinet-type air sterilizer could be used in the room.
A clean area and a semi-contaminated area should be set up in the catheterization lab. Medical staff should replace their isolation gowns or protective suits in the designated area.
Items in the operating room should be cleaned, and medicines, instruments and equipment not necessary for the operation should be removed.
Management of suspected or confirmed patients
For suspected or confirmed patients requiring interventional treatment, the informed consent should in principle be signed by a family member who has no history of close contact with the patient. The family members who had close contact with the patient should communicate with the physician by telephone under isolation, and the telephone recording should be kept as evidence. For patients without family members, the physician should report the case to the medical affairs department.
The number of medical professionals involved in surgery should be reduced. It is recommended that one nurse in the room and one nurse outside the room should be arranged. The personnel inside should not leave the operation room during the whole procedure, and the personnel outside should not enter the room without permission. In the interventional operating room, adequate preparation should be made for the medical materials required for the operation in order to reduce the frequency of door opening. The stratified precautions for medical staff during the COVID-19 epidemic should be strictly implemented. The disposable protective suits, boot covers, caps, masks and gloves should be removed and placed in double-layered medical waste bags after surgery. Meanwhile, all medical staff should rinse their hands according to the seven steps of hand washing under running water for at least 2 mins.
For patients receiving non-general anesthesia, surgical masks should be worn during surgery. For patients receiving general anesthesia, endotracheal intubation, not using a laryngeal mask, should be done in a special and isolated room to avoid the generation of aerosol. The anesthesia machine should be disinfected after surgery.
Operating room environment: When a suspected or confirmed patient is planned to receive surgery, the buffer room should be closed first, and the surgery should only be performed when the operating room reaches a negative pressure of −5 Pa or below.
Medical waste management after surgery: Medical waste from confirmed or suspected cases should be included in the management of infectious medical waste, and should be managed strictly in accordance with regulations released by the government, such as the Measures for Medical Wastes Management of Medical and Health Institutions.12
Medical instruments management after surgery: After removing the sharp objects, all devices should be put into a double-layered medical waste bag with a special mark indicating COVID-19 infection, and the supply room should be notified to collect the waste bags soon afterwards.
Disposable products management after surgery: All disposable products should be put into a double-layered medical waste bag with a special mark indicating COVID-19 infection and placed separately.
Management of operating room after neurointerventional surgery
Lead aprons, medical consumables and instruments used should be disinfected after surgery. Terminal room disinfection should be carried out as well. After that, the air and surfaces in the operating room should be sampled for microbiological analysis by the infection management department. If the test results are satisfactory, the room is approved for the next surgery.13
High-efficiency particulate air filters in the negative pressure room should be replaced in a timely fashion when the surgeries for suspected or confirmed cases have finished.
Medical professionals involved in surgery should be under medical observation for a period of time.
Infection prevention and control strategies for emergency stroke patients
Medical treatment process for emergency patients
A standard screening procedure should be performed for all emergency patients before their admission (figure 2).
It is recommended that the confirmed patients without urgent medical needs should be transferred to the fever clinic first. For the critically ill patients combined with stroke, who are not suitable to be transferred to the fever clinic, the expert group for COVID-19 in the hospital should hold a consultation to determine whether they were infected.
Patients with subarachnoid hemorrhage should be strictly identified in accordance with the above procedures, as fever is a common symptom for this condition. For patients who are not completely excluded from the risk of COVID-19 infection, angiography, craniotomy or interventional treatment are not suggested to be performed in an emergency manner. Treatment with different protection levels could be arranged after the COVID-19 screening result is available.
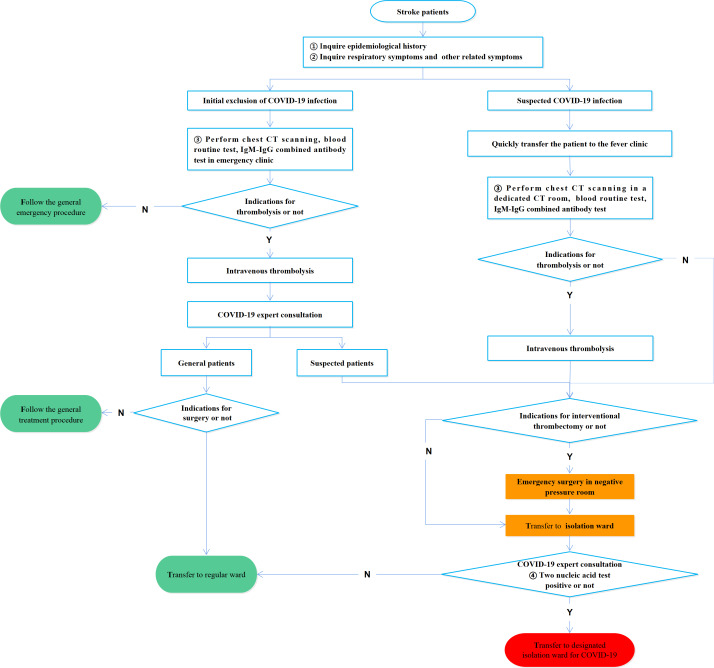
Use currently available guidelines and recommendations for identification and management of large vessel occlusion whenever possible.5 6 Head CT plus chest CT are recommended in the diagnostic workup of acute stroke patients. Before the operation, a quick consultation should be performed by the infectious diseases department or respiratory department to determine whether the patient is infected. The rescue process of acute stroke is shown in figure 3.
Figure 3.
Emergency treatment procedures for acute stroke.
Strategies of self-protection for medical staff
Neurointerventional radiologists involved in emergency work should implement the first-level precautions and immediately increase the level of precaution once the suspected case is admitted.
The consultation room should be fixed to ensure that there is no crossover with the infected patients during diagnosis and treatment.
Acknowledgments
We appreciate the work of Jingge Zhao at Henan Provincial People's Hospital in providing the medical illustrations for this publication.
Footnotes
YH, TH, MW and LJ contributed equally.
Collaborators: The Chinese Federation of Interventional and Therapeutic Neuroradiology (CFITN) and the International Society for Neurovascular Disease (ISNVD): Yongjie Ma, Fei Chen, Zheng Wang, Feng Ling, Yiling Cai, Hong Shan, Weijian Jiang, Bo Hong, Bing Leng, Zhongrong Miao, Huaizhang Shi, Jie Shuai, Xiaodong Xie, Zhenwei Zhao, Xiaoxin Bai, Zuoquan Chen, Jianping Deng, Chuanzhi Duan, Yaohua Fan, Chuan He, Xuying He, Chuansheng Liang, Jianmin Liu, Chaohua Wang, Daming Wang, Donghai Wang, Feng Wang, Xinjian Yang, Peng Zhang, Hongbo Zheng, Yufeng Zheng, Liangfu Zhu, Jun Li, Mingchang Li, Ming Yang, Jiaxing Yu, Yuehua Zhao.
Contributors: YH, TH, TL, MW, YG, EMH, HZ were the primary authors and, as such, were responsible for overseeing construction of the document outline, gathering of evidence, and drafting of the manuscript. HZ and LJ acted as the representatives of the Board of the Chinese Federation of Interventional and Therapeutic Neuroradiology (CFITN), and MW, YG and EMH acted as the representatives of the Board of the International Society for Neurovascular Disease (ISNVD) and provided commentary and editing on behalf of the Board and of the Society as a whole. HZ, as senior author, was responsible for organizing the writing group, overseeing the outline construction, facilitating communication between the writing group and the Expert Consensus Committee, drafting and editing of the manuscript, and the submission/proofing for publication.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Disclaimer: This literature review (‘Review’) is provided for informational and reference purposes only. Adherence to any consensus included in this review will not ensure successful prevention and control of COVID-19 in every situation. Furthermore, the consensus contained in this review should not be interpreted as setting a standard of care, or be deemed inclusive of all proper methods of care nor exclusive of other methods of care reasonably directed to obtaining the same results. This consensus reflects the best available information at the time the review was prepared. The results of future studies may require revisions to the recommendations in this review to reflect new data. CFITN and ISNVD do not warrant the accuracy or completeness of the review and assumes no responsibility for any injury or damage to persons or property arising out of or related to any use of this review or for any errors or omissions.
Competing interests: None declared.
Patient consent for publication: Not required.
Ethics approval: The consensus of experts does not involve the rights of patients or doctors, so it is exempted from the approval of the ethics committee.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data availability statement: Data are available in a public, open access repository
Contributor Information
On behalf of the Chinese Federation of Interventional and Therapeutic Neuroradiology (CFITN) and the International Society for Neurovascular Disease (ISNVD):
Yongjie Ma, Fei Chen, Zheng Wang, Feng Ling, Yiling Cai, Hong Shan, Weijian Jiang, Bo Hong, Bing Leng, Zhongrong Miao, Huaizhang Shi, Jie Shuai, Xiaodong Xie, Zhenwei Zhao, Xiaoxin Bai, Zuoquan Chen, Jianping Deng, Chuanzhi Duan, Yaohua Fan, Chuan He, Xuying He, Chuansheng Liang, Jianmin Liu, Chaohua Wang, Daming Wang, Donghai Wang, Feng Wang, Xinjian Yang, Peng Zhang, Hongbo Zheng, Yufeng Zheng, Liangfu Zhu, Jun Li, Mingchang Li, Ming Yang, Jiaxing Yu, and Yuehua Zhao
References
- 1. World Health Organization WHO characterizes COVID-19 as a pandemic, 2020. Available: https://www.who.int/emergencies/diseases/novel-coronavirus-2019/events-as-they-happen [Accessed 18 Mar 2020].
- 2. Chinese Center for Disease Control and Prevention COVID-19 outbreak distribution [In Chinese], 2020. Available: http://2019ncov.chinacdc.cn/2019-nCoV/ [Accessed 19 Mar 2020].
- 3. Epidemiology Working Group for NCIP Epidemic Response, Chinese Center for Disease Control and Prevention The epidemiological characteristics of an outbreak of 2019 novel coronavirus diseases (COVID-19). Chin J Epidemiol 2020;41:145–51. [In Chinese]. [Google Scholar]
- 4. Wu Z, Mcgoogan JM. Characteristics of and important lessons from the Coronavirus Disease 2019 (COVID-19) outbreak in China: summary of a report of 72 314 cases from the Chinese Center for Disease Control and Prevention. JAMA 2020. [DOI] [PubMed] [Google Scholar]
- 5. Turc G, Bhogal P, Fischer U, et al. European Stroke Organisation (ESO)- European Society for Minimally Invasive Neurological Therapy (ESMINT) guidelines on mechanical thrombectomy in acute ischemic stroke. J Neurointerv Surg 2019;11:535–8. 10.1136/neurintsurg-2018-014568 [DOI] [PubMed] [Google Scholar]
- 6. Kayan Y, Meyers PM, Prestigiacomo CJ, et al. Current endovascular strategies for posterior circulation large vessel occlusion stroke: report of the Society of NeuroInterventional Surgery Standards and Guidelines Committee. J Neurointerv Surg 2019;11:1055–62. 10.1136/neurintsurg-2019-014873 [DOI] [PubMed] [Google Scholar]
- 7. China National Health Commission Diagnosis and treatment protocol for novel coronavirus pneumonia (trial version 7) [In Chinese], 2020. Available: http://www.nhc.gov.cn/yzygj/s7653p/202003/46c9294a7dfe4cef80dc7f5912eb1989.shtml [Accessed 20 Mar 2020].
- 8. China National Health Commission Technical guidelines for the prevention and control of infection by the novel coronavirus in medical institutions (first edition) [In Chinese], 2020. Available: http://www.nhc.gov.cn/yzygj/s7659/202001/b91fdab7c304431eb082d67847d27e14.shtml [Accessed 20 Mar 2020].
- 9. China National Health Commission Guidelines on the usage of common medical protective equipment against novel coronavirus infection (trial version) [In Chinese], 2020. Available: http://www.nhc.gov.cn/yzygj/s7659/202001/e71c5de925a64eafbe1ce790debab5c6.shtml [Accessed 20 Mar 2020].
- 10. China National Health Commission Standard management of outpatient and emergency hospital infection in medical institutions [In Chinese], 2018. Available: http://www.nhc.gov.cn/wjw/s9496/201805/fa830cbf8b5a4ef3a1f6615a46a350a0.shtml [Accessed 22 Mar 2020].
- 11. China National Health Commission Hand hygiene rules for medical staff [In Chinese], 2019. Available: http://www.nhc.gov.cn/wjw/s9496/202002/dbd143c44abd4de8b59a235feef7d75e.shtml [Accessed 22 Mar 2020].
- 12. China National Health Commission Measures for medical wastes management of medical and health institutions [In Chinese], 2003. [Accessed 23 Mar 2020].
- 13. China National Health Commission Technical specifications for disinfection of medical institutions [In Chinese], 2012. Available: http://www.nhc.gov.cn/wjw/s9496/201204/54510.shtml [Accessed 22 Mar 2020].