Abstract
Background
Abusive head injuries in infants may be occult but clinically or forensically important. Data conflict regarding yield of neuroimaging in detecting occult head injuries in infants evaluated for physical abuse, with prior studies identifying yields of 4.3–37.3 %.
Objectives
(1) To quantify yield of computed tomography or magnetic resonance imaging in identification of occult head injuries in infants with concerns for physical abuse and (2) to evaluate risk factors for occult head injuries.
Participants and Setting
We conducted a retrospective, stratified, random systematic sample of 529 infants < 12 months evaluated for physical abuse at 4 urban children’s hospitals in the United States from 2008–2012. Infants with signs or symptoms suggesting head injury or skull fracture on plain radiography (N = 359), and infants without neuroimaging (N = 1) were excluded.
Methods
Sampling weights were applied to calculate proportions of infants with occult head injuries. We evaluated for associations between hypothesized risk factors (age < 6 months, rib or extremity fracture, facial bruising) and occult head injury using chi-square tests.
Results
Of 169 neurologically normal infants evaluated for abuse, occult head injury was identified in 6.5 % (95 % CI: 2.6, 15.8). Infants < 6 months were at higher risk (9.7 %; 95 % CI: 3.6, 23.3) than infants 6–12 months (1.0 %; 95 % CI: 1.3, 20.2). Rib fracture, extremity fracture and facial bruising were not associated with occult head injury.
Conclusions
Occult head injuries were less frequent than previously reported in some studies, but were identified in 1 in 10 infants <6 months. Clinicians should have a low threshold to obtain neuroimaging in young infants with concern for abuse.
Keywords: Traumatic brain injury, Child abuse
1. Introduction
Abusive head trauma (AHT) is the leading cause of fatal child physical abuse in young children (Klevens & Leeb, 2010). Prior work has shown that missed cases of AHT are common and place children at risk of suffering medical complications from delays in treatment as well as sustaining additional abusive injuries including fatal injuries (Jenny, Hymel, Ritzen, Reinert, & Hay, 1999; Letson et al., 2016). Young victims of abuse may have clinically or forensically significant head injuries not detected on history or physical examination. Neuroimaging is needed to identify clinically occult head injuries, but is associated with risk. The decision to obtain neuroimaging must be made by balancing the risk of missing a clinically or forensically important head injury with the risks associated with the imaging modality. Computed tomography (CT) carries radiation-associated risk while magnetic resonance imaging (MRI) carries sedation-associated risks and may be less readily available than CT, particularly in the emergency setting (Char, Ramamoorthy, & Wise-Faberowski, 2016; Miglioretti et al., 2013; Ramgopal, Karim, Subramanian, Furtado, & Marin, 2020). Greater understanding of which children undergoing evaluations for physical abuse are at highest risk for head injury would allow for better-informed risk-benefit assessments during clinical decision-making.
Prior estimates of the yield of neuroimaging in young children at risk for occult head injury have varied widely, ranging from 4.3–37.3% (Boehnke et al., 2018; Laskey, Holsti, Runyan, & Socolar, 2004; Rubin, Christian, Bilaniuk, Zazyczny, & Durbin, 2003; Shaikh, Wrotniak, & Mazur, 2019; Wilson et al., 2014). These estimates have largely been derived from single center studies and from work that focused exclusively on children evaluated by child protection teams (CPTs). CPTs are specialized multidisciplinary teams that may consist of child abuse pediatricians, social workers, and other providers who assess children for whom there is concern for child abuse or neglect (Tien, Bauchner, & Reece, 2002). The availability of CPTs to provide in-person consultation varies across hospitals (Tien et al., 2002). Therefore, not all children evaluated for abuse are seen by CPTs. In particular, those evaluated in emergency departments (ED) may not be referred to CPTs. Prior research has shown that skeletal surveys may be obtained without a CPT consult, and that CPT consultation is less likely if the skeletal survey is negative for fracture (Wood et al., 2019). Whether data addressing neuroimaging yields from studies of children referred to CPTs can be extrapolated to the larger population of at-risk children is unclear. In addition, there is known variation across EDs in their use of neuroimaging to assess the larger population of children presenting following blunt head trauma (Stanley et al., 2014). EDs and hospitals could also have varying practices in use of neuroimaging to screen for occult head injury in infants for whom there is concern for abuse. Multicenter studies not limited to CPT evaluations are therefore important and needed to balance potential selection biases.
Given these limitations in our current knowledge, our goals were to (1) quantify yield of neuroimaging to identify occult head injuries in children less than 12 months of age evaluated for concerns for abuse and (2) evaluate risk factors associated with occult head injuries in a multi-center sample of children undergoing evaluation for abuse, not limited to subspecialty CPTs.
2. Methods
This retrospective, descriptive study combined administrative data from 4 urban, tertiary children’s hospitals in the United States (U.S.) that contribute data to the Pediatric Health Information System (PHIS) with clinical data from chart review. PHIS is a large administrative database of more than 40 U.S. hospitals that includes diagnosis and resource utilization information (Fisher, Lindenauer, & Feudtner, 2012). Given that our study required clinical information not available within PHIS, we selected 4 hospitals across the U.S. who agreed to perform detailed chart abstraction of clinical information. We utilized PHIS data from only these participating 4 hospitals to first identify a larger population (PHIS Sample) of potential subjects. Sampling was then performed to identify a representative subpopulation (Chart Review Sample) for detailed chart abstraction. The Institutional Review Boards of the four participating centers approved this study.
2.1. Study population and sampling strategy
2.1.1. Parent study
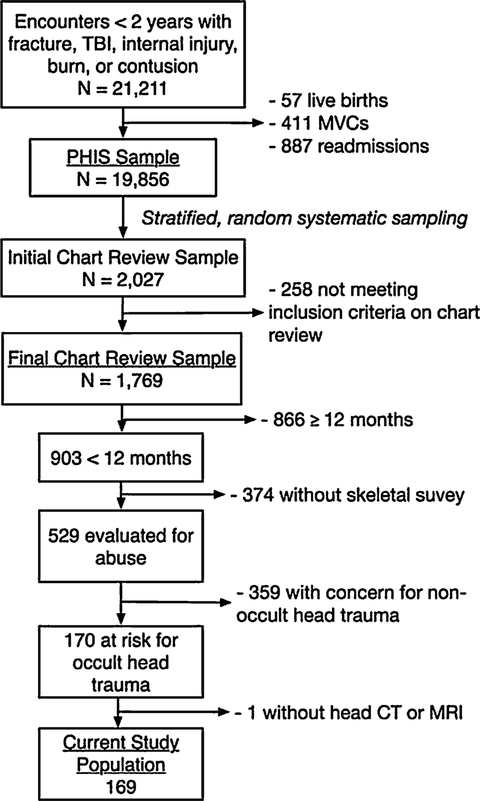
Our study was a secondary analysis of a subpopulation of a larger parent study that evaluated injured children < 2 years old who presented to a participating children’s hospital. The goals of the parent study were to evaluate skeletal survey performance and yield among injured children presenting to EDs. Methods and quality assurance measures of the larger study have been previously described (Henry et al., 2018; Wood et al., 2019). Briefly, for the larger study, we sampled the PHIS databases of the 4 participating hospitals to identify children with International Classification of Diseases, 9th revision, Clinical Modification (ICD-9-CM) codes for injury types that may raise concern for inflicted trauma, including: fracture (800–29), traumatic brain injury (803–4, 850–4), internal injury (860–9), burn (940–9), or contusion (920–4). Presentations following birth, motor vehicle collisions, and readmissions for previously diagnosed injuries were excluded (Fig. 1). A smaller Chart Review Sample was created using stratified, random systematic sampling to ensure adequate representation by age, sex, injury, injury etiology (abuse or non-abuse), and hospital (Fig. 1). Our sampling strategy has been previously described in greater detail (Wood et al., 2019). After sampling, each child’s PHIS record in the Initial Chart Review Sample was linked to his or her medical record to facilitate abstraction of clinical information not included within PHIS. Children not meeting the above inclusion and exclusion criteria after chart review and those with duplicate records were removed to generate the Final Chart Review Sample of the parent study. Sampling weights were assigned to each child in the Final Chart Review Sample to allow for representative hospital-level estimates.
Fig. 1.
Study population flow diagram.
2.1.2. Current study
To generate the current study population, we then used the clinical information from the Final Chart Review Sample to further narrow to a population of injured children < 12 months of age who presented without documented clinical signs of head injury, which is described further below. We elected to focus on children < 12 months of age due the peak incidence of AHT occurring in young infants and prior literature reporting more common neuroimaging screening in this age group compared to older children (Barr, Trent, & Cross, 2006; Laskey et al., 2004; Lee, Barr, Catherine, & Wicks, 2007; Wilson et al., 2014).
2.2. Data abstraction
Clinical information abstracted included reason for presentation, the first identified injury during the clinical encounter, physical examination findings, Glasgow Coma Scale (GCS), type of head imaging (computed tomography [CT] or magnetic resonance imaging [MRI]), reason for head imaging, and imaging findings. Chart abstractors selected “screening for occult head injury” if the child presented with a non-head injury, and the imaging was performed to screen for occult head injury. Two physicians (MKH, JNW) reviewed imaging reports to abstract injuries identified. Imaging findings were abstracted into pre-designated categorical variables and, occasionally, as unstructured data (free text fields) if the categorical variable did not apply. Cerebral edema, encephalomalacia, and facial fracture (orbital, mandibular) were not abstracted into pre-designated categorical fields and therefore were included in our analysis only when listed within a free-text field.
2.3. Inclusion and exclusion criteria of current study
2.3.1. Inclusion criteria
Our target study population was infants who presented with non-cranial injuries concerning for physical abuse and had neuroimaging performed for possible occult head injury. To identify this population, we first selected all children < 12 months of age who underwent a skeletal survey, as the American Academy of Pediatrics recommendations suggest that a skeletal survey should be performed for all injured infants with concern for abuse (Christian, Committee on Child Abuse and Neglect, & American Academy of Pediatrics, 2015; Section on Radiology & American Academy of Pediatrics, 2009). Only children undergoing head CT or brain MRI to screen for clinically occult head injury were included. For example, children presenting with a non-head injury such as a femur fracture who were undergoing neuroimaging to screen for occult head injury were included.
2.3.2. Exclusion criteria
We excluded children who underwent head imaging explicitly due to clinical concern for head injury (e.g. child presenting with scalp swelling or seizures). Reason for head imaging was defined as either “head injury suspected based on history of physical examination” or “screening for occult head injury.” Chart abstractors were instructed to choose “head injury suspected” if the neuroimaging was performed based on the presenting injury. In order to further ensure that we were not including children with signs or symptoms of head injury, we excluded patients with documented clinical and physical examination findings that could be suggestive of head injury. Clinical or physical examination findings that prompted exclusion were as follows: GCS < 15, lethargy, seizures at presentation, scalp injury (scalp bruising, abrasion, swelling, hematoma) or skull deformity on exam. Unstructured data (free text fields) were also reviewed within the relevant physical examination portions of the dataset to exclude children with physical examination findings concerning for head trauma such as full fontanelle or unresponsiveness. Children were excluded if a skull fracture was identified on skull radiograph or on skeletal survey, or if the first identified injury was traumatic brain injury. We included only infants without skull fractures on plain radiography because detection of a skull fracture in an infant would prompt further head imaging.
2.4. Outcome
Our outcome of interest was occult head injury identified on neuroimaging (CT or MRI). Occult head injury was defined as a head injury identified in our study population of children without clinical or physical examination findings concerning for head trauma nor skull fracture on skull radiography. We elected to define head injury broadly to provide an inclusive estimate of occult head injury. Head injury was defined as (1) non-parenchymal intracranial hemorrhage, (2) parenchymal injury or insult (contusion, hemorrhage, axonal injury, global or focal hypoxic ischemic injury), (3) cerebral edema, (4) encephalomalacia, (5) skull fracture not detected on plain radiography, and/or (6) facial fracture. Soft tissue swelling was not considered to be a head injury.
Two physicians (MKH, JNW) reviewed unstructured data for all head CT and brain MRIs to categorize these findings. During this review, if a report was unable to distinguish between a subarachnoid hemorrhage and a parenchymal contusion, the finding was coded as a subarachnoid hemorrhage.
2.5. Assessment of association of factors with occult head injury
Based on the literature, we selected a priori clinical findings that may be associated with occult head injury, as defined above (Rubin et al., 2003; Wilson et al., 2014). These included rib fractures, extremity fractures, facial bruises, and age < 6 months. To evaluate whether the yield of neuroimaging among children evaluated by CPTs was similar to the larger population of at-risk children evaluated for occult head injury, we tested for an association between CPT evaluation and occult head injury.
2.6. Analysis
Our analyses were conducted in Stata 15 (Williams, Palmes, Klinepeter, Pulley, & Foy, 2005). Descriptive statistics were performed. We present unweighted frequencies and weighted proportions. Due to our sampling strategy, proportions cannot be manually derived from any unweighted frequencies presented. Pearson chi-square tests were performed to assess for association between risk factors and the outcome of interest.
To ensure that possibly non-traumatic encephalomalacia was not contributing to our findings, we performed a sensitivity analysis that excluded patients with isolated encephalomalacia.
3. Results
The larger parent study identified 1769 children meeting inclusion and exclusion criteria from a larger population of 21,211 children < 2 years with injuries (Fig. 1). Of the 1769, 903 were < 12 months of age, and 529 underwent a skeletal survey. Of the 529 evaluated for abuse, 170 did not have documented signs or symptoms of head trauma and were eligible for our study. Of these, 169 underwent CT or MRI to evaluate for occult head injury and were included in our analyses.
3.1. Study population characteristics
The study population was primarily < 6 months (63.7 %), white (73.7 %), and publicly insured (76.5 %; Table 1). The most common first injuries identified were extremity fractures (62.7 %) followed by bruising (27.1 %). A majority underwent subspecialty evaluation by a CPT (78.8 %). The primary neuroimaging modality was head CT (93.1 %). Approximately one-fifth (20.9 %) underwent a bran MRI, and 14.0 % underwent both CT and MRI. CT was the only neuroimaging modality in 79.1 %, while MRI was the only modality in 7.0 %. A large proportion of our study population (47.3 %) was discharged from the ED.
Table 1.
Study Cohort Characteristics*.
| Characteristic | % Study Population |
|---|---|
| Age | |
| < 6 months | 63.7 |
| ≥ 6 months | 36.3 |
| Race | |
| White | 73.7 |
| Black | 13.7 |
| Other/Unknown | 12.6 |
| Sex | |
| Female | 48.2 |
| Male | 51.8 |
| Insurance Type | |
| Private | 23.2 |
| Public | 76.5 |
| Unknown/Missing | 0.4 |
| First identified Injury | |
| Extremity Fracture | 62.7 |
| Bruises | 27.1 |
| Rib fracture | 6.6 |
| Burns | 1.1 |
| Other | 2.5 |
| Child Protection Team Evaluation | |
| No | 21.2 |
| Yes | 78.8 |
| Select Injuries | |
| Rib fracture | 23.4 |
| Extremity fracture | 65.0 |
| Facial bruise | 25.8 |
| Head Imaging | |
| CT | 93.0 |
| CT only | 79.1 |
| MRI | 20.9 |
| MRI only | 7.0 |
| CT and MRI | 14.0 |
| Encounter Type | |
| Inpatient | 46.7 |
| ED Visit | 47.3 |
| Observation | 5.9 |
Weighted percentages may not add up to 100 % due to rounding.
3.2. Yield of neuroimaging
An occult head injury was identified in 6.5 % (95 % CI: 2.6, 15.8; Table 2). Non-parenchymal intracranial hemorrhages were found in 2.5 % (95 % CI: 1.2, 5.1). Parenchymal injuries were identified in 0.6 % (95 % CI: 0.2, 1.8). Cerebral edema was found in 0.4 % (95 % CI: 0, 1.5 %). Encephalomalacia was the most common finding, occurring in 3.3 % (95 % CI: 0.6, 16.9). Skull fractures were identified in 0.7 % (95 % CI: 0.3, 2.0); no facial fractures were identified.
Table 2.
Detection of Occult Head Injury.
| Type of head injury | % with finding (95 % CI) |
|---|---|
| Non parenchymal intracranial hemorrhage | 2.5 (1.2, 5.1) |
| Parenchymal injury or insult* | 0.6 (0.2, 1.8) |
| Cerebral edema | 0.4 (0, 1.5) |
| Encephalomalacia | 3.3 (0.6, 16.9) |
| Skull fracture** | 0.7 (0.3, 2.0) |
| Facial Fracture | 0 |
| Any of the above | 6.5 (2.6, 15.8) |
Parenchymal injury or insult = hemorrhage, contusions, axonal injury, HIE, global or focal ischemic injury.
not detected on plain radiography.
3.3. Assessment of association of factors with detection of occult head injury
Younger age was associated with detection of occult head injury (Table 3). Occult head injury was detected in 9.7 % (95 % CI: 3.6, 23.3) of infants < 6 months of age compared to 1.0 % (95 % CI: 0.2, 4.4) of those 6–12 months of age (p = 0.002). The presence or absence of a rib fracture, extremity fracture, or facial bruising was not associated with occult head injury. Among children evaluated by a CPT, 8.2 % had an occult head injury. While there was no association between CPT consultation and detection of occult head injury, no occult head injuries were identified among children not evaluated by a CPT.
Table 3.
Association of factors with occult head injury.
| Factor | Any occult head Injury % (95 % CI) | P value* |
|---|---|---|
| Age | 0.002 | |
| < 6 months | 9.7 (3.6, 23.3) | |
| ≥ 6 months | 1.0 (0.2, 4.4) | |
| Rib Fracture | 0.38 | |
| Present | 10.4 (5.8, 18.0) | |
| Absent | 5.4 (1.3, 20.2) | |
| Extremity Fracture | 0.44 | |
| Present | 7.7 (2.3, 22.5) | |
| Absent | 4.3 (1.6, 11.0) | |
| Facial Bruising | 0.51 | |
| Present | 4.3 (1.4, 12.6) | |
| Absent | 7.3 (2.4, 20.1) | |
| Child Protection Team Evaluation | 0.30 | |
| Performed | 8.3 (3.2, 19.5) | |
| Not Performed | 0 |
Pearson chi square.
3.4. Encephalomalacia sensitivity analysis
In order to assess whether encephalomalacia was driving the association between young age and occult head imaging findings, we further evaluated this population. In total, there were 3 children (unweighted data) with encephalomalacia who otherwise met study inclusion criteria: 1 was preterm, 1 was full term, and 1 had an unknown gestational age. All were less than 6 months of age. With encephalomalacia excluded from the outcome, occult head injuries were identified in 3.4 % of children (95 % CI: 1.8, 6.2) in the study population. When stratified by age, occult head injuries occurred in 4.7 % (95 % CI: 2.4, 9.0) of children < 6 months and 1.0 % (95 % CI: 0.2, 4.4) of children 6–12 months (p = .039).
4. Discussion
This multicenter study examining the finding of occult head injury among infants presenting with injuries that raised concern for abuse is not limited to children with formal CPT evaluations. Our findings suggest that 1 in 15 infants < 12 months would need to undergo neuroimaging to identify one head injury. This yield is less than previously described in some studies, despite an intentionally broad primary outcome definition. If encephalomalacia is excluded from this outcome, the prevalence drops to 3.4 % suggesting that 29 infants would need to be imaged to identify one occult head injury. Our findings among children < 12 months are consistent with recent studies by Shaikh et al. and Fingarson et al. that showed neuroimaging yields of 5% and 8.2 %, respectively (Fingarson & Fortin, 2019; Shaikh et al., 2019). Despite this low imaging yield in children < 12 months, we found that nearly 10 % of infants < 6 months had an occult head injury.
In our study, all children found to have occult head injuries were evaluated by a CPT. Eight percent of children evaluated by a CPT were found to have occult head injury on neuroimaging. While there was no statistically significant difference between detection of occult head injuries among those evaluated by CPTs and those infants who were not, this may be a function of our study’s sample size and a resulting inability to show statistical significance. Studies solely addressing the neuroimaging yield among children evaluated by CPTs may not be fully generalizable to the larger population of at-risk children presenting to EDs for care.
Issues related to generalizability, differences in study populations, and selection biases may be at play in explaining differences between our work and 2 prior studies that reported neuroimaging yields of 20 % (Boehnke et al., 2018) and 37 % (Rubin et al., 2003). These studies focused largely on children evaluated by CPTs and had broader definitions of occult injury. For example, one single-center study of children < 2 years included children with skull fractures on plain radiography in addition to including scalp swelling in the definition of occult head injury (Rubin et al., 2003).
When evaluating neuroimaging yield across studies, imaging selection biases must be considered and it is important to evaluate the percentage of eligible patients who underwent neuroimaging. Thresholds for obtaining screening head imaging may have changed over time among studies throughout the literature or differ between centers. If imaging thresholds are disparate or in flux, the population imaged may change from higher risk of injury to a lower risk population across studies. When looking across prior work, the percentage of eligible patients who ultimately underwent neuroimaging ranges from 37 %–83 % (Boehnke et al., 2018; Fingarson & Fortin, 2019; Laskey et al., 2004; Rubin et al., 2003; Wilson et al., 2014). In our study, 99 % of subjects meeting our inclusion and exclusion criteria were imaged suggesting that our results may be less influenced by imaging selection biases.
Differences in patient populations presenting for evaluation may also contribute to the varying rates of yield across studies. The literature on yield of neuroimaging is largely derived from urban centers in the U.S., but how populations differ across centers regarding sociodemographic and clinical factors is not described. Differences in presenting injuries and severity of injuries across centers may contribute to neuroimaging screening practices. Prior literature suggests that sociodemographic factors including race and socioeconomic status may influence child abuse evaluation and reporting practices, but it is not known whether these factors influence neuroimaging decision-making (Lane & Dubowitz, 2007; Lane, Rubin, Monteith, & Christian, 2002; Wood et al., 2010).
Many prior studies have had small sample sizes (Fingarson & Fortin, 2019; Laskey et al., 2004; Rubin et al., 2003; Shaikh et al., 2019; Wilson et al., 2014), and would likely have had wide confidence intervals if calculated. Our study is no exception. Our point estimate of 6.5 % had a 95 % confidence interval of 2.6–15.8%. This CI is, however, outside the range of the largest estimate yield reported of 37 % (95 % CI: 24 %, 51 %) (Rubin et al., 2003).
Faced with our data and the widely variable results previously reported (Boehnke et al., 2018; Laskey et al., 2004; Rubin et al., 2003; Shaikh et al., 2019; Wilson et al., 2014), we suggest that young children, particularly those < 6 months of age, are at the highest risk for occult head injury and should be imaged when there is concern for physical abuse. The risks of missing a clinically or forensically significant injury should be weighed against the risks associated with CT and MRI. As these risks decrease with lower radiation doses or the potential of fast MRI without sedation, the risk-benefit equation may change. With recent promising results of the sensitivity of fast MRI, this may offset this risk-benefit ratio in favor of fast MRI at centers where this is an available modality (Berger, Furtado, Flom, Fromkin, & Panigrahy, 2020; Lindberg et al., 2019).
Our findings should be considered within the context of six important limitations. First, as a retrospective study we were limited to those clinical and physical examination findings that were documented in the child’s medical record. We must infer from the signs and symptoms documented in the medical record, for example, that a clinician did not have concerns for head trauma. Second, we were unable to determine the order in which imaging studies were obtained. We elected to only include skull fractures that were not apparent on plain radiography. Some patients whose neuroimaging revealed an occult head injury could have been excluded if the neuroimaging was obtained before a skeletal survey that showed a skull fracture. Third, we relied on clinical imaging reports to establish injury diagnoses. Multiple non-blinded clinical radiologists contributed across institutions to the clinical radiology reports. Measures of inter-rater reliability cannot be assessed. Fourth, our sample size is small leading to wide confidence intervals. While young age persisted as a risk factor for occult head trauma, the lack of association among other risks factors may be a function of lack of power. In the setting of limited power, we were only able to present unadjusted outcomes. Datasets drawing on a larger sample allowing for multivariable models would be valuable. Fifth, our findings revealed a high relative prevalence of encephalomalacia, which may or may not be indicative of trauma. For this reason we presented results with and without encephalomalacia. Lastly, our data are also derived exclusively from children’s hospitals and may not be generalizable to the larger population of injured children presenting to general EDs.
5. Conclusions
The yield of neuroimaging in identification of occult injuries among children with concern for physical abuse is lower than previously reported in some studies (Boehnke et al., 2018; Laskey et al., 2004; Rubin et al., 2003), but in infants < 6 months of age, the yield was 9.7 % (95 % CI: 3.6, 23.3). This yield is in the range of reported yields for skeletal surveys which are a mandatory part of the evaluation for physical abuse in young children (Duffy, Squires, Fromkin, & Berger, 2011). Our results support that infants, particularly those < 6 months of age, are at the highest risk for occult head injury and should be imaged when presenting with injuries that raise concern for physical abuse.
Acknowledgements
We are grateful to Janet Fromkin, MD, Pamela Rubin, RN, Benjamin Murphy, MD, Monica Nielsen-Parker, MSW, Colleen E. Bennett, MD, and Valerie Mondestin, MHA for their many hours dedicated to chart abstraction.
Financial disclosure statement
Salary support was provided by the National Institute of Health / Eunice Kennedy Shriver National Institute of Child Health and Human Development Career Development Award 1K23HD071967-04 (Dr. Wood). A portion of Dr. Lindberg’s work was supported by the Eunice Kennedy Shriver National Institute of Child Health and Human Development K23HD083559. Children’s Hospital of Philadelphia has received payment for Dr. Henry’s, Dr. Fortin’s, and Dr. Wood’s expert testimony following subpoenas in cases of suspected child abuse. This project was supported by grant number F32HS024194 from the Agency for Healthcare Research and Quality (Dr. Henry). The content is solely the responsibility of the authors and does not necessarily represent the official views of the Agency for Healthcare Research and Quality. Study sponsors were not involved in the study design; the collection, analysis, and interpretation of data; the writing of the report; or the decision to submit the paper for publication.
Abbreviations
- AHT
abusive head trauma
- CT
computed tomography
- CPT
child protection team
- ED
emergency department
- GCS
glasgow coma scale
- ICD-9-CM
international classification of diseases, 9threvision, clinical modification
- MRI
magnetic resonance imaging
- MVCs
motor vehicle crashes
- PHIS
pediatric health information system
- TBI
traumatic brain injury
Footnotes
Declaration of Competing Interest
Dr. Lindberg has provided paid expert witness testimony in cases of alleged child physical abuse.
References
- Barr RG, Trent RB, & Cross J (2006). Age-related incidence curve of hospitalized shaken Baby Syndrome cases: Convergent evidence for crying as a trigger to shaking. Child Abuse & Neglect, 30(1), 7–16. 10.1016/j.chiabu.2005.06.009. [DOI] [PubMed] [Google Scholar]
- Berger RP, Furtado AD, Flom LL, Fromkin JB, & Panigrahy A (2020). Implementation of a brain injury screen MRI for infants at risk for abusive head trauma. Pediatric Radiology, 50(Jan. (1)), 75–82. 10.1007/s00247-019-04506-1. [DOI] [PubMed] [Google Scholar]
- Boehnke M, Mirsky D, Stence N, Stanley RM, Lindberg DM, & Ex S. i. (2018). Occult head injury is common in children with concern for physical abuse. Pediatric Radiology, 48(8), 1123–1129. 10.1007/s00247-018-4128-6. [DOI] [PubMed] [Google Scholar]
- Char D, Ramamoorthy C, & Wise-Faberowski L (2016). Cognitive dysfunction in children with heart disease: The role of anesthesia and sedation. Congenital Heart Disease, 11(3), 221–229. 10.1111/chd.12352. [DOI] [PubMed] [Google Scholar]
- Christian CW, Committee on Child Abuse and Neglect, & American Academy of Pediatrics (2015). The evaluation of suspected child physical abuse. Pediatrics, 135(5), e1337–1354. 10.1542/peds.2015-0356. [DOI] [PubMed] [Google Scholar]
- Duffy SO, Squires J, Fromkin JB, & Berger RP (2011). Use of skeletal surveys to evaluate for physical abuse: Analysis of 703 consecutive skeletal surveys. Pediatrics, 127(1), e47–52. 10.1542/peds.2010-0298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fingarson A, & Fortin K (2019). Yield of neuroimaging in infant physical abuse evaluations: Do infant age and injury type matter? The Journal of Emergency Medicine, 57(2), 195–202. 10.1016/j.jemermed.2019.03.041. [DOI] [PubMed] [Google Scholar]
- Fisher BT, Lindenauer PK, & Feudtner C (2012). In-Hospital databases In Strom BL, Kimmel SE, & Hennessy S (Eds.). Pharmacoepidemiology (pp. 244–258). (5th ed.). Chichester, West Sussex, UK: Hoboken Wiley-Blackwell. [Google Scholar]
- Henry MK, French B, Feudtner C, Zonfrillo MR, Lindberg DM, Anderst JD, … Wood JN (2018). Cervical spine imaging and injuries in young children with non-motor vehicle crash-associated traumatic brain injury. Pediatric Emergency Care 10.1097/PEC.0000000000001455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jenny C, Hymel KP, Ritzen A, Reinert SE, & Hay TC (1999). Analysis of missed cases of abusive head trauma. JAMA, 281(7), 621–626. Retrieved from https://www.ncbi.nlm.nih.gov/pubmed/10029123. [DOI] [PubMed] [Google Scholar]
- Klevens J, & Leeb RT (2010). Child maltreatment fatalities in children under 5: findings from the national violence death reporting system. Child Abuse & Neglect, 34(4), 262–266. 10.1016/j.chiabu.2009.07.005. [DOI] [PubMed] [Google Scholar]
- Lane WG, & Dubowitz H (2007). What factors affect the identification and reporting of child abuse-related fractures? Clinical Orthopaedics and Related Research, 461, 219–225. 10.1097/BLO.0b013e31805c0849. [DOI] [PubMed] [Google Scholar]
- Lane WG, Rubin DM, Monteith R, & Christian CW (2002). Racial differences in the evaluation of pediatric fractures for physical abuse. JAMA, 288(13), 1603–1609. 10.1001/jama.288.13.1603. [DOI] [PubMed] [Google Scholar]
- Laskey AL, Holsti M, Runyan DK, & Socolar RR (2004). Occult head trauma in young suspected victims of physical abuse. The Journal of Pediatrics, 144(6), 719–722. 10.1016/j.jpeds.2004.02.023. [DOI] [PubMed] [Google Scholar]
- Lee C, Barr RG, Catherine N, & Wicks A (2007). Age-related incidence of publicly reported shaken baby syndrome cases: is crying a trigger for shaking? Journal of Developmental and Behavioral Pediatrics, 28(4), 288–293. 10.1097/DBP.0b013e3180327b55. [DOI] [PubMed] [Google Scholar]
- Letson MM, Cooper JN, Deans KJ, Scribano PV, Makoroff KL, Feldman KW, et al. (2016). Prior opportunities to identify abuse in children with abusive head trauma. Child Abuse & Neglect, 60, 36–45. 10.1016/j.chiabu.2016.09.001. [DOI] [PubMed] [Google Scholar]
- Lindberg DM, Stence NV, Grubenhoff JA, Lewis T, Mirsky DM, Miller AL, … Runyan DK (2019). Feasibility and accuracy of fast MRI versus CT for traumatic brain injury in young children. Pediatrics, 144(4), 10.1542/peds.2019-0419. [DOI] [PubMed] [Google Scholar]
- Miglioretti DL, Johnson E, Williams A, Greenlee RT, Weinmann S, Solberg LI, … Smith-Bindman R (2013). The use of computed tomography in pediatrics and the associated radiation exposure and estimated cancer risk. JAMA Pediatrics, 167(8), 700–707. 10.1001/jamapediatrics.2013.311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ramgopal S, Karim SA, Subramanian S, Furtado AD, & Marin JR (2020). Rapid brain MRI protocols reduce head computerized tomography use in the pediatric emergency department. BMC Pediatrics, 20(1), 14 10.1186/s12887-020-1919-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rubin DM, Christian CW, Bilaniuk LT, Zazyczny KA, & Durbin DR (2003). Occult head injury in high-risk abused children. Pediatrics, 111(6 Pt 1), 1382–1386. Retrieved from https://www.ncbi.nlm.nih.gov/pubmed/12777556. [DOI] [PubMed] [Google Scholar]
- Section on Radiology, & American Academy of Pediatrics (2009). Diagnostic imaging of child abuse. Pediatrics, 123(5), 1430–1435. 10.1542/peds.2009-0558. [DOI] [PubMed] [Google Scholar]
- Shaikh H, Wrotniak BH, & Mazur PM (2019). Occult head injury in children less than 2 years with suspected child abuse in the emergency department. Pediatric Emergency Care, 35(9), 596–599. 10.1097/PEC.0000000000001187. [DOI] [PubMed] [Google Scholar]
- Stanley RM, Hoyle JD Jr., Dayan PS, Atabaki S, Lee L, Lillis K, … Pediatric Emergency Care Applied Research, N (2014). Emergency department practice variation in computed tomography use for children with minor blunt head trauma. The Journal of Pediatrics, 165(6), 1201–1206. 10.1016/j.jpeds.2014.08.008 e1202. [DOI] [PubMed] [Google Scholar]
- Tien I, Bauchner H, & Reece RM (2002). What is the system of care for abused and neglected children in children’s institutions? Pediatrics, 110(6), 1226–1231. 10.1542/peds.110.6.1226. [DOI] [PubMed] [Google Scholar]
- Williams J, Palmes G, Klinepeter K, Pulley A, & Foy J (2005). Referral by pediatricians of children with behavioral health disorders. Clinical Pediatrics, 44, 343–349. [DOI] [PubMed] [Google Scholar]
- Wilson PM, Chua M, Care M, Greiner MV, Keeshin B, & Bennett B (2014). Utility of head computed tomography in children with a single extremity fracture. The Journal of Pediatrics, 164(6), 1274–1279. 10.1016/j.jpeds.2013.12.041. [DOI] [PubMed] [Google Scholar]
- Wood JN, Hall M, Schilling S, Keren R, Mitra N, & Rubin DM (2010). Disparities in the evaluation and diagnosis of abuse among infants with traumatic brain injury. Pediatrics, 126(3), 408–414. 10.1542/peds.2010-0031. [DOI] [PubMed] [Google Scholar]
- Wood JN, Henry MK, Berger RP, Lindberg DM, Anderst JD, Song L, … Feudtner C (2019). Use and utility of skeletal surveys to evaluate for occult fractures in young injured children. Academic Pediatrics, 19(4), 428–437. 10.1016/j.acap.2018.08.007. [DOI] [PMC free article] [PubMed] [Google Scholar]