Abstract
Introduction
Measuring physiological parameters at depth is an emergent challenge for athletic training, diver’s safety and biomedical research. Recent advances in wearable sensor technology made this challenge affordable; however, its impact on breath-hold diving has never been comprehensively discussed.
Methods
We performed a systematic review of the literature in order to assess what types of sensors are available or suitable for human breath-hold diving, within the two-fold perspective of safety and athletic performance.
Results
In the 52 studies identified, sensed physiological variables were: electrocardiogram, body temperature, blood pressure, peripheral oxygen saturation, interstitial glucose concentration, impedance cardiography, heart rate, body segment inertia and orientation.
Conclusion
Limits and potential of each technology are separately reviewed. Inertial sensor technology and transmission pulse oximetry could produce the greatest impact on breath-hold diving performances in the future.
Keywords: Physiology, Patient monitoring, Telemetry, Computers, Equipment, Training
Introduction
Underwater activities are commonly performed for recreational, occupational or competitive purposes.[ 1 , 2] The most common approaches include either a self-contained underwater breathing apparatus (SCUBA) or breath-holding. These activities carry an intrinsic health risk due the physiological stresses related to hypoxaemia, hyper- or hypocapnia, hydrostatic pressure and cold water,[ 2] potentially resulting in loss of consciousness and drowning. Given that the majority of reported adverse events are related to a delay in recognizing a life-threatening problem,[ 1] the risk can be minimized through primary and secondary prevention strategies. In these contexts, field measurement of relevant physiological parameters is an emergent challenge, as the improvement of divers’ safety requires a better understanding of diving physiology. This challenge is being met thanks to technological advances in wearable sensors (i.e., water and pressure proofing, miniaturization and underwater communication).[ 3 , 4] In breath-hold (BH) diving, remarkable increases in the number of active competitors and dramatic improvement in diving performance have occurred in the last 20 years.[ 5] As BH divers rely only on their own physiological capabilities, sensor technology provides potential for training feedback and enhancement of human performance and safety.
This work aimed to systematically review wearable sensor technologies usable during BH diving, with the twofold perspective of inferring its potential applications to safety and performance. Specifically, this review aimed at addressing the following questions:
What type of wearable sensors can be used in human BH diving?
What wearable sensors used for SCUBA diving are potentially applicable also to BH diving?
What water- and pressure-proofing strategies have been adopted to adapt monitoring technology to the underwater environment?
At which depth have the various approaches been reported to work?
Although some of the physiological changes discussed in this review may apply to all types of diving (see e.g., the blood pressure increase[ 6]), the conclusions arrived at are specific to BH diving. Analogous reviews on SCUBA diving were previously published[ 3 , 4] and the interested reader may refer to them.
Methods
Article selection was based on a systematic search of the scientific databases PubMed and Scopus following the PRISMA guidelines.[ 7] To avoid outdated technology, only items published after January 2000 were included in the search. The keyword string was: (sensor OR ECG OR electrocardiogram OR “heart rate” OR “blood pressure” OR hemodynamics OR “oxygen saturation” OR EEG OR IMU OR “inertial measurement unit” OR accelerometer OR gyroscope OR “body temperature” OR “blood glucose”) AND (diver OR diving).
The title and abstract of each result were reviewed and evaluated based on the relevance to the aims of this study. When appropriate, full-text was obtained for a more detailed analysis. Article references were examined for further pertinent publications.
Inclusion criteria were that the publication: appeared in a peer-reviewed academic source; was related to the utilization or the development of wearable sensors explicitly or potentially applicable to human BH diving; included experiments carried out completely below the water level, at a depth (either real or simulated with a hyperbaric chamber) of more than 2 m. Exclusion criteria were: studies performed in shallow water (less than 2 m deep); sensors applicable only to SCUBA diving; invasive or non-portable sensors.
The following information was extracted from articles meeting the inclusion criteria: sensed physiological variable, sensor technology, sensor sealing precautions, studied diving mode, test environment, maximal tested depth.
Results and discussion
The initial search yielded 1,565 titles on Scopus and 760 on PubMed updated to 28 February 2019. Duplicates were removed, 248 abstracts were further analysed and subsequently 106 full-text papers were downloaded. After full-text assessment, we finally selected 52 publications for inclusion in this review (Figure 1). The parameters extracted from each publication are specifically reported in Tables 1-7 which will be discussed in detail below.
Figure 1.
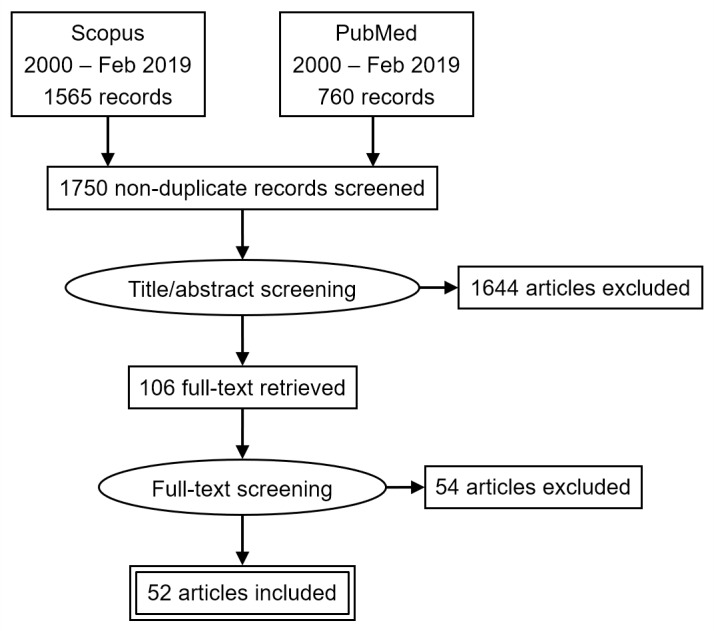
PRISMA flow diagram for the systematic review
Thirteen studies involved BH diving, 38 SCUBA diving and one saturation diving. Tested depths ranged from 2 to 160 metres’ sea or fresh water. Sensed physiological variables were: electrocardiogram (ECG, 19 studies), body temperature (six studies), arterial blood pressure (ABP, five studies), peripheral oxygen saturation (SpO2, five studies), interstitial glucose concentration (five studies), impedance cardiography (four studies), heart rate (13 studies), body segments inertia and orientation (three studies), electroencephalogram (one study). Six studies involved simultaneous measurements of multiple parameters, such as ECG and impedance cardiography (one study), ECG and SpO2 (one study), ECG, ABP and SpO2 (two studies), heart rate and core and skin temperature (one study), ECG and body temperature (one study). In all studies, an appropriate casing was used for the water- and pressure-proofing of electronic components.
ELECTROCARDIOGRAM AND HEART RATE
The ECG has previously been applied to BH diving and unsurprisingly was the most common physiological variable recorded.[ 8] As reported in Table 1, depth ranged between 2–70 m. In ECG monitoring there are two different elements that must be waterproofed: the electrodes and the electronics. Performing differential measurements between devices, such as ECG the front-end electronics typically require amplifiers which present high input impedance, high level of gain and a large common-mode rejection ratio (CMRR). These must provide a large amount of gain for very low-level signals, often in the presence of high noise levels. Immersion in salt water introduces a parallel resistance between electrodes, increasing the load and decreasing the signal by an amount that depends on water conductivity (i.e., salinity) and electrodes properties. Therefore, the optimal and most widespread solution was to place electrodes under a dry suit.[ 9 - 13] Alternatively, electrode insulation was achieved via direct coverage with biocompatible adhesive patches[ 14 - 19] or with hydrophobic dental impression material.[ 20 - 23] All the reported solutions avoided modifying the original manufactured skin-electrode interface while maintaining the correct inter-electrode insulation. Finally, a novel solution based on intrinsically waterproof electrodes has been recently developed.[ 24]
Table 1. Studies reporting measurement of the electrocardiogram and heart rate. BH = breath hold. HVP = hypdrophilic vinyl polysiloxane. NS = not specified. PC = personal computer. S = SCUBA. trans = transmission. WHC = wet hyperbaric chamber. * = probably not monitored in real-time due to Bluetooth constraints underwater .
| Sensor | Ref. | Diving mode | Setting | Tested depth (m) | Manufacturer | Real-time display | Data storage or display | Data trans | Water-and pressure-proofing of the wearable sensor | Max. depth (m) |
| Electrodes | 40 | BH | WHC | 55 | NS | Yes | ECG recorder | Not specified | Not specified | – |
| Electrodes + ECG transmitter | 13 | S | WHC | 27 | Fukuda-Denshi | Yes | ECG recorder (Dynascope DS-1040) | Wireless | All inside diver’s dry suit | – |
| 12 | S | Pool | 2 | Prototype | Yes | Data logger | Wireless (acoustic) | Electrodes: under diver’s dry suit; ECG transmitter: inside cylindrical housing attached to an aqualung | – | |
| 46 | S | Sea | 20 | Nihon-Kohden | No | ECG transmitter | Cable | Electrodes: not specified; ECG transmitter: water- and pressure-proof case. | – | |
| Electrodes + ECG recorder | 17 | BH | Sea | 70 | Sorin Group | Yes | ECG recorder (storage); PC (display) | Cable | Electrodes: covered with transparent adhesive (Tegaderm, 3M, St. Paul, Minn., USA); ECG Holter: plastic tube (Comex SA, Marseille, France) | 190 |
| 14 | S | Pool | 4 | Reynolds Medical | No | ECG recorder | Cable | Electrodes: waterproof tape; ECG recorder: professional diving pouch (TMT, ewa-marine) | – | |
| 47 | S | Lake | 8 | PicoMed | No | ECG recorder | Cable | Electrodes: special clips; ECG recorder: not specified | – | |
| 15 | S | Sea | 25 | Mortara | No | ECG recorder | Cable | Electrodes: first layer (Visulin, Hartmann) + second layer (Steri-Drapes, 3M); ECG Holter recorder: pressure-proof anticorodal aluminium housing, with a plexiglass cover (Metralab s.r.l.) | 50 | |
| 9, 10 | S | Sea | 30[9] 61[9] | Rozinn-Electronics[9], NS[10] | No | ECG recorder | Cable | All inside diver’s dry suit | – | |
| Electrode patches embedded in an ECG recorder | 16 | BH | WHC | 20 | NS | No | ECG recorder | Embedded | Electrodes: special adhesive patch; ECG recorder: water- and pressure-proof case | – |
| Electrodes + data logger | 20–23 | BH | Pool | 2[20,21] 10.5[22,23] | Prototype | Yes | Data logger | Cable | Electrodes: HVP dental impression material (Elite H-D+, Zhermack); Data logger: lexan tube | 200 |
| 19 | S | Pool | 4.6 | UFI | Yes | Data logger | Cable | Electrodes: benzoin + waterproof tape + moleskin; Data logger: not shown | – | |
| Electrodes + ECG sensor + smartphone | 11 | S | Pool | 2.7 | Shimmer-Research Ltd | Only vibratory alerts | Smartphone | Wireless (Bluetooth) | All inside diver’s dry suit; Smartphone: professional diving pouch | – |
| Electrodes + Monitoring Board | 18 | S | Sea | 30 | Prototype | Yes | PC | Cable to a Bluetooth buoy | Electrodes: hot glue + self-adhesive waterproof film (Tegaderm, 3M); ECG Monitor: Case (DryCase 2000, OtterBox) | – |
| Electrodes chest strap + ECG transmitter | 24 | S | Pool | 4.5 | Prototype | Yes | PC | Wireless (Bluetooth)* | Electrodes: intrinsically waterproof (hydrophobic, Carbon Black/Polydimethylsiloxane electrodes, meshed with embedded copper mesh); ECG transmitter: not specified | – |
| Electrodes chest strap + wrist monitor | 26,30,36,37 | BH[37] S[26,30,36] | Sea | 3[36] 5[30] 20[26,37] | Polar | Yes | Wrist monitor | Wireless | Electrodes: built-in water insulation (textile electrodes); Monitor: built-int waterproof case | 50 |
| 25 | S | Pool | 4.5 | Timex | Yes | Wrist monitor | Wireless | Not specified | – | |
| 27–29 31–35 | S | Sea | 18[27,28,33-35] 20[29] 54[32] 65[31] | Scubapro-Uwatec | Yes | Wrist monitor | Wireless | Electrodes: built-in water insulation; Monitor: built-int waterproof case | 120 |
The ECG signal analysis can be restricted to heart rate only, as in commercial cardiotachometers and diving computers, which were studied at 3–65 m depth[ 25 - 37] or in shallow water during static apnoea competitions.[ 38 , 39] Cardiac arrhythmias are common during BH diving[ 40 , 41] and real-time ECG analysis can be used to trigger alert signals based on pre-determined criteria.[ 11] Moreover, heart rate response to exercise is only partially suppressed by the diving reflex and still remains influenced by the metabolic rate:[ 17 , 42 - 45] it could be therefore monitored by an experienced diver as a real-time surrogate of the energy cost of underwater swimming.
ARTERIAL BLOOD PRESSURE
Underwater ABP measurement was successfully carried out at depths between 2–10.5 m (Table 2). In designing the pressure transducer, electrical component waterproofing without preventing (or excessively delaying) barometric equalization in the reference chamber is critical to allow correct measurement in the aquatic environment, especially in dynamic conditions (ascent and descent).[ 48] We found only two different approaches to achieving this. The first solution was putting a commercial ABP device inside a downwardly-open plexiglass housing,[ 6] whose resulting water-air interface was set at the level of the middle of the blood pressure cuff. Subsequent studies improved the portability of the sensor, with the ABP device encapsulated into a Lexan tube directly located over the cuff, inflated with the gas coming from a SCUBA tank.[ 20 , 21 , 48 , 49] BH was reported to increase ABP either modestly[ 48] or dramatically.[ 50] Therefore, it would be useful to monitor individual ABP responses to BH diving both for research and screening purposes.
Table 2. Studies reporting measurement of arterial blood pressure. BH = breath hold. S = SCUBA, trans = transmission .
| Sensor | Ref. | Diving mode | Setting | Tested depth (m) | Manufacturer | Real-time display | Data storage or display | Data trans | Water-and pressure-proofing of the wearable sensor | Max. depth (m) |
| Cuff + differential pressure sensor + microcontroller (based on Korotkoff sounds) | 6 | S | Pool | 3 | Bosch & Sohn (BoSo) | Yes | On screen via a video-camera | Cable | Plexiglass housing for inflator/display (downwardly open for hydrostatic pressure equalisation); silicone sheath for cuff microphones | – |
| Cuff + differential pressure sensor + microcontroller (based on Korotkoff sounds) | 20 21 48 49 | BH[20,21,48],S[49] | Pool | 10.5 | Prototype | Yes | Microcontroller | Cable | Lexan tube, inflation air coming from a SCUBA tank | 200 |
IMPEDANCE CARDIOGRAPHY
Impedance cardiography allows for non-invasive monitoring of the electrical impedance changes in the thorax thus providing estimation of the cardiac stroke volume and, together with the ECG measurement, of several derived cardiovascular parameters. These systems usually rely on the use of a set of electrodes (at least four) placed on the thorax. An alternating high frequency small amplitude current is applied through two electrodes, whereas the electrical potential difference is measured using the other pair. Secured in a pressure chamber[ 40] or into an underwater torch case in open sea,[ 51 - 53] the device allows measurements up to 55 m depth (Table 3). While it represents an index of myocardial performance, it adds limited benefits for BH diving safety and performance compared to ECG alone.
Table 3. Studies reporting measurement of arterial blood pressure. BH = breath hold. S = SCUBA, trans = transmission .
| Sensor | Ref. | Diving mode | Setting | Tested depth (m) | Manufacturer | Real-time display | Data storage or display | Data trans | Water-and pressure-proofing of the wearable sensor | Max. depth (m) |
| Electrodes | 40 | BH | WHC | 55 | Bomed | Yes | Recorder | NS | Not specified | – |
| Electrodes + recorder | 51 52 53 | BH | Pool[52,53] Sea[51] | 3[52,53] 30[51] | 2C Technologies Inc | No | Recorder | Cable | Recorder: underwater torch case; Electrodes: surgical 15x10 cm patches (Plastod, Bologna, Italy) | 90 |
PERIPHERAL OXYGEN SATURATION
Arterial haemoglobin saturation is a key performance parameter for BH and reflects the partial pressure of O2 in the arterial blood. It can be measured non-invasively in the peripheral circulation (SpO2), although motion artefacts and reflex peripheral vasoconstriction prevents the utilization of classical transmission pulse oximeters at fingertip or earlobe. Accordingly, only reflectance pulse oximeters at the forehead were used underwater,[ 20 - 22 , 54] at a depth of 2–10 m (Table 4). In the design of the device, waterproofing was specifically obtained by soaking it in a highly sealing and electrically insulating polymeric material. Battery change was facilitated by introducing a separate waterproof compartment.
Table 4. Studies reporting measurement of peripheral oxygen saturation. BH = breath hold. trans = transmission .
| Sensor | Ref. | Diving mode | Setting | Tested depth (m) | Manufacturer | Real-time display | Data storage or display | Data trans | Water-and pressure-proofing of the wearable sensor | Max. depth (m) |
| Reflectance sensor (8000R) + module (OEM III) + data logger | 20–22 54 | BH | Pool | 2[20,21] 10.5[22,54] | Nonin | Yes | Data logger | Cable | Data logger: either (i) inside a lexan tube or (ii) filled with silicone gel (SilGel 612, Wacker Chemie AG) with a water- and pressure-proof compartment for battery | 200 |
The descent phase of a BH dive cannot be guided by pulse oximetry, because the depletion of oxygen stores is counterbalanced by transmission of the surrounding hydrostatic pressure to the alveolar gas, thus increasing arterial partial pressure of oxygen and resulting in a fairly stable SpO2 at 100%. Only during a prolonged period at depth and/or during the ascent (when there is reversal of the above process) would O2 depletion manifest as a decrease in SpO2. As a consequence of circulation time between lungs and forehead, the nadir of SpO2 at forehead occurs 4–8 s after surfacing,[ 55] or even later if cardiac output is reduced by a marked diving response.[ 53]
BODY SEGMENT INERTIA AND ORIENTATION
Classical movement analysis systems (optical motion capture, force and pressure measurement sensors, global positioning systems) are not suitable for the deep underwater environment. Inertia measurement units (IMU) incorporate accelerometers, gyroscopes and magnetometers in a small space and can be easily waterproofed. For these reasons, IMU arose as a powerful tool for the investigation of competitive swimmers’ biomechanics[ 56] and the energetics of air-breathing diving animals.[ 57 , 58] IMUs have been used in experimental studies on human divers in only three studies (Table 5), two conducted at a depth of 2 m[ 59 , 60] and one at 10 m.[ 61] Electrical insulation was achieved by means of either external cases[ 59 , 60] which can be easily acquired and applied, or by embedding the electronics in a polymeric potting compound.[ 61]
Table 5. Studies reporting measurement of body segment inertia and orientation. IMU = Inertia measurement unit. PC = personal computer. S = SCUBA. trans = transmission. * = personal communication .
| Sensor | Ref. | Diving mode | Setting | Tested depth (m) | Manufacturer | Real-time display | Data storage or display | Data trans | Water-and pressure-proofing of the wearable sensor |
| Accelerometer + magnetometer + gyroscope (IMU) | 60 | S | Pool | 2 | ST Microelectronics + InvenSense | Yes | PC at surface | Cable | Lexan tube |
| 61 | S | Pool | 10 | Pololu | Yes | PC at surface | Cable | Spokes: 3D printed housing, filled with polyurethane potting compound; Hub: 5083 grade aluminium alloy housing | |
| 59 | S | Pool | 2* | Prototype | No | IMU | Cable | Professional diving case or pouch for cameras or mobile phones |
The main outcomes of Kuch et al.[ 60] and Goodfellow et al.[ 61] were, respectively, the reconstruction of diver’s posture (to detect anomalous behaviours) and path (to build an inertial based underwater navigation system). However, potential applications of IMU to BH diving extend to investigating the energy cost of underwater swimming, a major determinant of BH distance or depth.[ 62] Feedback on swimming economy would be crucial for improving performances of both dynamic and deep apnoeas, especially if provided in real-time. Groh et al.[ 59] moved in that direction, trying to establish a biomechanical model to describe leg and upper body orientation during fin kicking. Their proposed algorithm has the potential to be implemented into a wider training system for competitive or recreational divers. However, additional parameters still need to be measured in order to obtain a complete biomechanical model.
BODY TEMPERATURE
Superficial, rectal and ingestible temperature sensors were easily adapted to hyperbaric environments to investigate heat exchange in SCUBA[ 18 , 36 , 63 - 65] and saturation diving[ 66] at 3–160 m depth (Table 6). Built-in cases are the most common solutions to properly insulate superficial sensors, while rectal and ingestible sensors are designed to be resistant to gastrointestinal fluids thus are already waterproof. However no specifications were found concerning maximum ambient pressure in which those sensors may be operated. Electrical insulation of the data loggers was achieved by means of cases or housings designed to allow easy access.
Table 6. Studies reporting measurement of body temperature. NS = not specified. PC = personal computer. S = SCUBA. Sat = Saturation. trans = transmission .
| Sensor | Ref. | Diving mode | Setting | Tested depth (m) | Manufacturer | Real-time display | Data storage or display | Data trans | Water-and pressure-proofing of the wearable sensor |
| Ingestible temperature sensor + data logger | 65 | S | Pool | 3 | HQ Inc. | No | Data logger | Wireless | Temperature sensor: capsule; data logger: inside diver’s dry suit |
| 36 | S | Pool | 3 | Philips- Respironics | Yes | Data logger | Wireless | Temperature sensor: capsule; data logger: not specified | |
| 18 | S | Sea | 30 | Philips- Respironics | Yes | Data logger + PC on surface | Wireless (to data logger); Cable to bluetooth buoy (to PC) | Temperature sensor: capsule; data logger: case (DryCase 2000, OtterBox) | |
| 66 | Sat diving | Sea | 160 | Biomed d.o.o. | No | Data logger | Wireless | Temperature sensor: capsule; data logger: professional diving pouch | |
| Rectal temperature sensor + data logger | 63 | S | Sea | 10 | Grant- Instruments | Yes | Data logger | Cable | Temperature sensor: inside divers’ dry suit; data logger: above water surface |
| Skin temperature sensor + data logger | 63 | S | Sea | 10 | Grant- Instruments | Yes | Data logger | Cable | Temperature sensor: inside divers’ dry suit; data logger: above water surface |
| 64 | S | Sea | 8 | Grant- Instruments | Yes | Data logger | Cable | Temperature sensor: surgical tape (Blenderm, 3M); data logger: above water surface | |
| 36 | S | Sea | 3 | Philips- Respironics | Yes | Data logger | Wireless | Temperature sensor: built-in waterproof case; Data logger: not specified | |
| 18 | S | Sea | 30 | Philips- Respironics | Yes | Data logger + PC on surface | Wireless (to data logger); Cable to bluetooth buoy (to PC) | Temperature sensor: built-in waterproof case; data logger: Case (DryCase 2000, OtterBox) | |
| 66 | Sat diving | Sea | 160 | Biomed d.o.o. | No | Data logger | Embedded | Temperature sensor: embedded in the data logger; data logger: professional diving pouch |
Monitoring body temperature would be useful in repetitive diving, such as spearfishing competitions and professional dives, because it allows timely diagnosis and prevention of hypothermia.[ 67] This was reported to be a frequent event in Ama divers,[ 68] which could eventually elicit chronic adaptation to cold.[ 69] The usefulness of such monitoring is underscored also by the reduction in maximal BH duration in cold water due to an increased resting metabolic rate.[ 70] Some commercially available diving computers offer skin temperature measurement from the heart rate chest strap,[ 27 - 29 , 31 - 35] but have not been the subject of published scientific studies. In fact, it is noteworthy that the gold standard for a comprehensive characterization of human thermal balance is to measure both skin and core temperature.[ 71]
INTERSTITIAL GLUCOSE CONCENTRATION
Subcutaneous sensors for interstitial glucose concentration have been waterproofed with adhesive films and dental impression material[ 72 , 73] or simply kept under the dry suit[ 74 , 75] or even the wet suit.[ 76] In this case, there is no issue related to the direct contact with water, since the sensor (i.e. a thin needle) is placed within the interstitial fluid. Electrical insulation had to be ensured only to avoid issues related to power supply and data transmission. Devices were studied at depths 22–40 m (Table 7). In insulin-dependent diabetic SCUBA divers these devices may diagnose hypoglycaemia during the dive, although the very short immersion times hamper their usefulness for BH diving.
Table 7. Studies reporting measurement of interstitial glucose concentration. S = SCUBA. trans = transmission .
| Sensor | Ref. | Diving mode | Setting | Tested depth (m) | Manufacturer | Real-time display | Data storage or display | Data trans | Water-and pressure-proofing of the wearable sensor |
| Subcutaneous glucometer + monitor | 72 | S | Sea | 21.5 | Medtronic | No | Monitor | Cable | Glucose sensor: hydrophilic vinylpolysiloxane material (Elite H-D, Zhermack) + doubled plastic adhesive dressing + an elastic collodion film between the two dressings; monitor: pressurized aluminium container |
| 73 | S | Sea | 20 | Medtronic | No | Monitor | Cable | Glucose sensor: taped with an Opsite film; monitor: water- and pressure-proof case | |
| 74 75 | S | Sea | 22[75] 24[74] | Medtronic | No | Monitor | Cable | All inside diver’s dry suit | |
| 76 | S | Sea | 40 | Dexcom | Yes | Monitor | Wireless | Glucose sensor: under diver’s wet suit; monitor: waterproof case with glass screen |
ELECTROENCEPHALOGRAM
One pilot study obtained electroencephalographic (EEG) recordings 4 m underwater[ 77] by protecting the electrodes under a full-face latex mask, further covered by a bathing cab. In this case, waterproofing is essential to ensure inter-electrode insulation and prevent surface biopotentials becoming equipotential, as discussed earlier in relation to ECG and impedance cardiography. Signals were transmitted via cable to an amplifier at the surface. Although acute cognitive impairment is an important safety issue in extreme BH diving, real-time applicability of EEG in this field remains unfeasible at this time. Nevertheless, it could be important to develop portable underwater EEG devices, especially to study development of adaptive changes in EEG reported in trained breath-hold divers.[ 78]
Conclusions
Since the first tests on BH diving populations,[ 79 , 80] the potential for carrying out physiological measurements during actual BH diving has increased dramatically. The wearable sensors implemented so far have contributed significantly to our understanding of BH diving physiology and to the safety of dives. Adequate waterproof characteristics seem to be achievable for systems originally designed for terrestrial use, provided that the issues of both sensor-body interface and electrical insulation are taken into account. However, the intrinsic depth limits of the adopted technology was not reported in several studies.
Another recent improvement involves the transmission and real-time processing of physiological measurements. On-line medical and physiological information transmission during diving could allow a prompt recognition of an increased risk or a clinical adverse event, leading to timely termination of the dive (for example, significant cardiac arrhythmias or an excessive rise in ABP). Further advances could be obtained by integrating different sensors into a unique "smart" suit. In addition to safety, the analysis of multiple data collected in the field would positively impact training and competition strategies, as happens in several other sporting disciplines. Among the sensors that we discussed, transmission pulse oximetry and inertial sensor technology seem to have the greatest potential for further technical improvement and innovative uses. The former could give feedback on available oxygen stores (with the limitations outlined above), and the latter on factors influencing oxygen consumption rate, possibly identifying the most economical swimming technique. Therefore, we expect them to produce the greatest impact in the future.
Footnotes
Conflict of interest and funding: nil
Contributor Information
Giovanni Vinetti, Department of Molecular and Translational Medicine, University of Brescia, Brescia, Italy; Department of Information Engineering, University of Brescia, Brescia, Italy.
Nicola F Lopomo, Department of Information Engineering, University of Brescia, Brescia, Italy.
Anna Taboni, Department of Anesthesiology, Pharmacology, Intensive Care and Emergencies, University of Geneva, Geneva, Switzerland.
Nazzareno Fagoni, Department of Molecular and Translational Medicine, University of Brescia, Brescia, Italy.
Guido Ferretti, Department of Molecular and Translational Medicine, University of Brescia, Brescia, Italy; Department of Anesthesiology, Pharmacology, Intensive Care and Emergencies, University of Geneva, Geneva, Switzerland.
References
- Buzzacott P, editor. DAN Annual diving report 2017 edition: A report on 2015 diving fatalities, injuries, and incidents. Durham (NC): Divers Alert Network; 2017. 10.1002/cphy.c160008 [DOI] [PubMed] [Google Scholar]
- Fitz-Clarke JR. Breath-hold diving. Compr Physiol. 2018;8:585–630. doi: 10.1002/cphy.c160008. [DOI] [PubMed] [Google Scholar]
- Cibis T, McEwan A, Sieber A, Eskofier B, Lippmann J, Friedl K, et al. Diving into research of biomedical engineering in scuba diving. IEEE Rev Biomed Eng. 2017;10:323–33. doi: 10.1109/RBME.2017.2713300. [DOI] [PubMed] [Google Scholar]
- Sieber A, L’Abbate A, Kuch B, Wagner M, Benassi A, Passera M, et al. Advanced instrumentation for research in diving and hyperbaric medicine. Undersea Hyperb Med. 2010;37:259–69. [PubMed] [Google Scholar]
- International Association for the Development of Apnea (AIDA). Athlete Rankings. Available from: https://www.aidainternational.org/Ranking/Rankings. [cited 2019 Feb 21].
- Almeling M, Wulf K, Schega L, Witten F, Niklas A. Blood pressure measurement in sport divers - Method and first results [Blutdruckmessung bei sporttauchern - Methode und erste ergebnisse] J fur Hypertonie. 2005;9(2):7–13. (Ger). [Google Scholar]
- Moher D, Liberati A, Tetzlaff J, Altman DG, PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ. 2009;339:b2535. doi: 10.1136/BMJ.B2535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wyss V. ECG of apneic subjects during immersion in water at various depths [Elettrocardiogramma di soggetti in apnea durante immersione in acqua a profondità diverse]. Boll Soc Ital Biol Sper. 1956;32:503–6. (Ita). [PubMed] [Google Scholar]
- Noh Y, Posada-Quintero HF, Bai Y, White J, Florian JP, Brink PR, et al. Effect of shallow and deep SCUBA dives on heart rate variability. Front Physiol. 2018;9:110. doi: 10.3389/fphys.2018.00110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Olędzki S, Wojtarowicz A, Płońska-Gościniak SG, Lewandowski M, Gorący J. Scuba diving, patent foramen ovale and heart rhythm disturbances: The role of underwater Holter monitoring - Case report . Ann Noninvasive Electrocardiol. 2017;22:e12450. doi: 10.1111/anec.12450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cibis T, Groh BH, Gatermann H, Leutheuser H, Eskofier BM. Wearable real-time ECG monitoring with emergency alert system for scuba diving. In: Proceedings of the annual international conference of the IEEE engineering in medicine and biology society, EMBS. Milan, Italy: IEEE; 2015. p. 6074- 7. Available from: https://ieeexplore.ieee.org/document/7319777 [cited 2019 March 22]. [DOI] [PubMed] [Google Scholar]
- Istepanian RSH, Woodward B. The design and evaluation of a programmable underwater acoustic biotelemetry system for diver monitoring . Acta Acust. 2003;89:95–104. [Google Scholar]
- González Olea A, Trigueros MJL, Martínez IA, González CA, López BCA, Callejón PE. Physiological adaptation to cold water diving. [Adaptación fisiológica al buceo en aguas frías] . Arch Med Del Deport. 2001;18:603–11. Spanish. [Google Scholar]
- Schipke JD, Pelzer M. Effect of immersion, submersion, and scuba diving on heart rate variability . Br J Sports Med. 2001;35:174–80. doi: 10.1136/BJSM.35.3.174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bosco G, de Marzi E, Michieli P, Omar HR, Camporesi EM, Padulo J, et al. 12-lead Holter monitoring in diving and water sports: A preliminary investigation . Diving Hyperb Med. 2014;44:202–7. [PubMed] [Google Scholar]
- Ehrmann U, Pittner M, Paulat K, Radermacher P, Muth CM. Heart rate and metabolic effects during apnea diving. [Herzfrequenz und metabolische effekte beim apnoetauchen] . Dtsch Z Sportmed. 2004;55:295–8. (Ger). [Google Scholar]
- Lemaître F, Lafay V, Taylor M, Costalat G, Gardette B. Electrocardiographic aspects of deep dives in elite breath-hold divers . Undersea Hyperb Med. 2013;40:145–54. [PubMed] [Google Scholar]
- Schuster A, Castagna O, Schmid B, Cibis T, Sieber A. Underwater monitoring system for body temperature and ECG recordings . Underw Technol. 2017;34:135–9. [Google Scholar]
- Berry NT, Wideman L, Rhea CK, Labban JD, Chon KH, Shykoff BE, et al. Effects of prolonged and repeated immersions on heart rate variability and complexity in military divers . Undersea Hyperb Med. 2017;44:589–600. doi: 10.22462/11.12.2017.10. [DOI] [PubMed] [Google Scholar]
- Breskovic T, Uglesic L, Zubin P, Kuch B, Kraljevic J, Zanchi J, et al. Cardiovascular changes during underwater static and dynamic breath-hold dives in trained divers . J Appl Physiol (1985). 2011;111:673–8. doi: 10.1152/japplphysiol.00209.2011. [DOI] [PubMed] [Google Scholar]
- Kiviniemi AM, Breskovic T, Uglesic L, Kuch B, Maslov PZ, Sieber A, et al. Heart rate variability during static and dynamic breath-hold dives in elite divers . Auton Neurosci. 2012;169:95–101. doi: 10.1016/j.autneu.2012.05.004. [DOI] [PubMed] [Google Scholar]
- Kuch B, Bedini R, L’Abbate A, Wagner M, Buttazzo G, Sieber A. Embedded data logging platform for research in diving physiology. In: Proceedings of the 7th workshop on intelligent solutions in embedded systems, WISES 2009. Ancona, Italy: IEEE; 2009. p. 43- 8. Available from: https://ieeexplore.ieee.org/document/5186411 [cited 2019 March 22] [Google Scholar]
- Sieber A, Bedini R, Yong X, Navarri A, Luche MD, L’Abbate A, et al. High resolution ECG and depth data logger: A novel device to study breath hold diving induced variations of the PQ interval. Proceedings of the 1st international conference on biomedical electronics and devices – Volume 1. Funchal, Madeira, Portugal: SciTePress; 2008. p. 269- 75. Available from: https://www.scitepress.org/PublicationsDetail.aspx?ID=kixxvouoCSk=&t=1 [cited 2019 March 22] [Google Scholar]
- Noh Y, Bales JR, Reyes BA, Molignano J, Clement AL, Pins GD, et al. Novel conductive carbon black and polydimethlysiloxane ECG electrode: A comparison with commercial electrodes in fresh, chlorinated, and salt water . Ann Biomed Eng. 2016;44:2464–79. doi: 10.1007/s10439-015-1528-8. [DOI] [PubMed] [Google Scholar]
- Koehle MS, Hodges ANH, Lynn BM, Rachich MF, McKenzie DC. Diffusing capacity and spirometry following a 60-minute dive to 4.5 meters . Undersea Hyperb Med. 2006;33:109–18. [PubMed] [Google Scholar]
- Chouchou F, Pichot V, Garet M, Barthélémy J-C, Roche F. Dominance in cardiac parasympathetic activity during real recreational SCUBA diving . Eur J Appl Physiol. 2009;106:345–52. doi: 10.1007/s00421-009-1010-0. [DOI] [PubMed] [Google Scholar]
- Madden D, Barak O, Thom SR, Yang M, Bhopale VM, Ljubkovic M, et al. The impact of predive exercise on repetitive SCUBA diving . Clin Physiol Funct Imaging. 2016;36:197–205. doi: 10.1111/cpf.12213. [DOI] [PubMed] [Google Scholar]
- Susilovic-Grabovac Z, Obad A, Duplančić D, Banić I, Brusoni D, Agostoni P, et al. 2D speckle tracking echocardiography of the right ventricle free wall in SCUBA divers after single open sea dive . Clin Exp Pharmacol Physiol. 2018;45:234–40. doi: 10.1111/1440-1681.12883. [DOI] [PubMed] [Google Scholar]
- Steinberg F, Doppelmayr M. Executive functions of divers are selectively impaired at 20-meter water depth . Front Psychol. 2017;8:1000. doi: 10.3389/fpsyg.2017.01000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Flouris AD, Scott JM. Heart rate variability responses to a psychologically challenging scuba dive . J Sports Med Phys Fitness. 2009;49:382–6. [PubMed] [Google Scholar]
- Ljubkovic M, Gaustad SE, Marinovic J, Obad A, Ivancev V, Bilopavlovic N, et al. Ultrasonic evidence of acute interstitial lung edema after SCUBA diving is resolved within 2–3 h . Respir Physiol Neurobiol. 2010;171:165–70. doi: 10.1016/J.RESP.2010.02.008. [DOI] [PubMed] [Google Scholar]
- Møllerløkken A, Breskovic T, Palada I, Valic Z, Dujic Z, Brubakk AO. Observation of increased venous gas emboli after wet dives compared to dry dives . Diving Hyperb Med. 2011;41:124–8. [PubMed] [Google Scholar]
- Bilopavlovic N, Marinovic J, Ljubkovic M, Obad A, Zanchi J, Pollock NW, et al. Effect of repetitive SCUBA diving on humoral markers of endothelial and central nervous system integrity . Eur J Appl Physiol. 2013;113:1737–43. doi: 10.1007/s00421-013-2600-4. [DOI] [PubMed] [Google Scholar]
- Madden D, Thom SR, Yang M, Bhopale VM, Ljubkovic M, Dujic Z. High intensity cycling before SCUBA diving reduces post-decompression microparticle production and neutrophil activation . Eur J Appl Physiol. 2014;114:1955–61. doi: 10.1007/s00421-014-2925-7. [DOI] [PubMed] [Google Scholar]
- Zanchi J, Ljubkovic M, Denoble PJ, Dujic Z, Ranapurwala S, Pollock NW. Influence of repeated daily diving on decompression stress . Int J Sports Med. 2014;35:465–8. doi: 10.1055/s-0033-1334968. [DOI] [PubMed] [Google Scholar]
- Castagna O, Desruelle AV, Blatteau JE, Schmid B, Dumoulin G, Regnard J. Alterations in body fluid balance during fin swimming in 29°C water in a population of special forces divers . Int J Sports Med. 2015;36:1125–33. doi: 10.1055/s-0035-1555854. [DOI] [PubMed] [Google Scholar]
- Lee J-Y, Lee H-H, Kim S, Jang Y-J, Baek Y-J, Kang K-Y. Diving bradycardia of elderly Korean women divers, haenyeo, in cold seawater: A field report . Ind Health. 2016;54:183–90. doi: 10.2486/indhealth.2015-0043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lindholm P, Nordh J, Gennser M. The heart rate of breath-hold divers during static apnea: Effects of competitive stress . Undersea Hyperb Med. 2006;33:119–24. [PubMed] [Google Scholar]
- Lemaître F, Bernier F, Petit I, Renard N, Gardette B, Joulia F. Heart rate responses during a breath-holding competition in well-trained divers . Int J Sports Med. 2005;26:409–13. doi: 10.1055/s-2004-821159. [DOI] [PubMed] [Google Scholar]
- Gentile C, La Scala S. Hemodynamic and respiratory changes in athletes during deep breath-hold diving . Minerva Anestesiol. 2001;67:875–80. (Ita). [PubMed] [Google Scholar]
- Ferrigno M, Grassi B, Ferretti G, Costa M, Marconi C, Cerretelli P, et al. Electrocardiogram during deep breath-hold dives by elite divers . Undersea Biomed Res. 1991;18:81–91. [PubMed] [Google Scholar]
- Manley L. Apnoeic heart rate responses in humans. A review . Sport Med. 1990;9:286–310. doi: 10.2165/00007256-199009050-00004. [DOI] [PubMed] [Google Scholar]
- Smeland EB, Owe JO, Andersen HT. Modification of the 'diving bradycardia' by hypoxia or exercise . Respir Physiol. 1984;56:245–51. doi: 10.1016/0034-5687(84)90108-7. [DOI] [PubMed] [Google Scholar]
- Bergman SA, Campbell JK, Wildenthal K, Dujic Z. “Diving reflex” in man: Its relation to isometric and dynamic exercise . J Appl Physiol. 1972;33:27–31. doi: 10.1152/jappl.1972.33.1.27. [DOI] [PubMed] [Google Scholar]
- Wein J, Andersson JP, Erdéus J. Cardiac and ventilatory responses to apneic exercise . Eur J Appl Physiol. 2007;100:637–44. doi: 10.1007/s00421-007-0411-1. [DOI] [PubMed] [Google Scholar]
- Togawa S, Yamami N, Shibayama M, Nakayama H, Nozawa T, Mano Y, et al. Evaluation of scuba diving work load . Japanese J Phys Fit Sport Med. 2006;55:341–6. doi: 10.7600/jspfsm.55.341. [DOI] [Google Scholar]
- Winkler BE, Tetzlaff K, Muth C-M, Paulat K, Hebestreit H, Pollock NW. Scuba-dive-related changes in heart rate in children . Pediatr Exerc Sci. 2011;23:388–98. doi: 10.1123/pes.23.3.388. [DOI] [PubMed] [Google Scholar]
- Sieber A, L’Abbate A, Passera M, Garbella E, Benassi A, Bedini R. Underwater study of arterial blood pressure in breath-hold divers . J Appl Physiol (1985) 2009;107:1526–31. doi: 10.1152/japplphysiol.91438.2008. [DOI] [PubMed] [Google Scholar]
- Sieber A, Kuch B, L’Abbate A, Wagner M, Dario P, Bedini R, et al. An underwater blood pressure measuring device . Diving Hyperb Med. 2008;38:128–34. [PubMed] [Google Scholar]
- Ferrigno M, Ferretti G, Ellis A, Warkander D, Costa M, Cerretelli P, et al. Cardiovascular changes during deep breath-hold dives in a pressure chamber . J Appl Physiol (1985). 1997;83:1282–90. doi: 10.1152/jappl.1997.83.4.1282. [DOI] [PubMed] [Google Scholar]
- Marongiu E, Crisafulli A, Ghiani G, Olla S, Roberto S, Pinna M, et al. Cardiovascular responses during free-diving in the sea . Int J Sports Med. 2015;36:297–301. doi: 10.1055/s-0034-1389969. [DOI] [PubMed] [Google Scholar]
- Tocco F, Crisafulli A, Marongiu E, Milia R, Kalb A, Concu A, et al. A portable device to assess underwater changes of cardio dynamic variables by impedance cardiography . J Phys Conf Ser. 2012;407:012026. doi: 10.1088/1742-6596/407/1/012026. [DOI] [Google Scholar]
- Tocco F, Marongiu E, Pinna M, Roberto S, Pusceddu M, Angius L, et al. Assessment of circulatory adjustments during underwater apnoea in elite divers by means of a portable device . Acta Physiol (Oxf). 2013;207:290–8. doi: 10.1111/apha.12000. [DOI] [PubMed] [Google Scholar]
- Kuch B, Koss B, Dujic Z, Buttazzo G, Sieber A. A novel wearable apnea dive computer for continuous plethysmographic monitoring of oxygen saturation and heart rate . Diving Hyperb Med. 2010;40:34–40. [PubMed] [Google Scholar]
- Choi SJ, Ahn HJ, Yang MK, Kim CS, Sim WS, Kim JA, et al. Comparison of desaturation and resaturation response times between transmission and reflectance pulse oximeters . Acta Anaesthesiol Scand. 2010;54:212–7. doi: 10.1111/j.1399-6576.2009.02101.x. [DOI] [PubMed] [Google Scholar]
- Mooney R, Corley G, Godfrey A, Quinlan LR, ÓLaighin G. Inertial sensor technology for elite swimming performance analysis: A systematic review . Sensors. 2016;16:18. doi: 10.3390/s16010018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Halsey LG, Shepard ELC, Wilson RP. Assessing the development and application of the accelerometry technique for estimating energy expenditure . Comp Biochem Physiol A Mol Integr Physiol. 2011;158:305–14. doi: 10.1016/j.cbpa.2010.09.002. [DOI] [PubMed] [Google Scholar]
- Elliott KH. Measurement of flying and diving metabolic rate in wild animals: Review and recommendations . Comp Biochem Physiol A Mol Integr Physiol. 2016;202:63–77. doi: 10.1016/j.cbpa.2016.05.025. [DOI] [PubMed] [Google Scholar]
- Groh BH, Cibis T, Schill RO, Eskofier BM. IMU-based pose determination of scuba divers’ bodies and shanks. In: 2015 IEEE 12th international conference on wearable and implantable body sensor networks, BSN 2015. Cambridge (MA): IEEE; 2015. Available from: https://ieeexplore.ieee.org/document/7299376. [cited 2019 March 22]. [Google Scholar]
- Kuch B, Haasl S, Wagner M, Buttazzo G, Sieber A. Preliminary report: Embedded platform for inertial based underwater navigation. In: 2011 Proceedings of the 9th international workshop on intelligent solutions in embedded systems, WISES 2011. Regensburg, Germany: IEEE; 2011. p. 101- 8 Available from: https://ieeexplore.ieee.org/document/6086028. [cited 2019 March 22]. [Google Scholar]
- Goodfellow GM, Neasham JA, Rendulic I, Nad D, Miskovic N. DiverNet - A network of inertial sensors for real time diver visualization. In: SAS 2015 - 2015 IEEE sensors applications symposium, proceedings. Zadar, Croatia: IEEE; 2015. Available from: https://ieeexplore.ieee.org/document/7133640. [cited 2019 March 22]. [Google Scholar]
- Ferretti G. Extreme human breath-hold diving . Eur J Appl Physiol. 2001;84:254–71. doi: 10.1007/s004210000377. [DOI] [PubMed] [Google Scholar]
- Risberg J, Hope A. Thermal insulation properties of argon used as a dry suit inflation gas . Undersea Hyperb Med. 2001;28:137–43. [PubMed] [Google Scholar]
- Hope A, Hjelle J, Aanderud A. Time and temperature effects on body fluid loss during dives with the open hot-water suit . Aviat Space Environ Med. 2005;76:655–60. [PubMed] [Google Scholar]
- Vrijdag XC, van Ooij P-JA, van Hulst RA. Argon used as dry suit insulation gas for cold-water diving . Extrem Physiol Med. 2013;2:17. doi: 10.1186/2046-7648-2-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mekjavić B, Golden FS, Eglin M, Tipton MJ. Thermal status of saturation divers during operational dives in the North Sea . Undersea Hyperb Med. 2001;28:149–55. [PubMed] [Google Scholar]
- Pendergast DR, Lundgren CEG. The underwater environment: cardiopulmonary, thermal, and energetic demands . J Appl Physiol (1985). 2009;106:276–83. doi: 10.1152/japplphysiol.90984.2008. [DOI] [PubMed] [Google Scholar]
- Kang DH, Kim PK, Kang BS, Song SH, Hong SK. Energy metabolism and body temperature of the ama . J Appl Physiol. 1965;20:46–50. doi: 10.1152/jappl.1965.20.1.46. [DOI] [PubMed] [Google Scholar]
- Ferretti G, Costa M. Diversity in and adaptation to breath-hold diving in humans . Comp Biochem Physiol Part A Mol Integr Physiol. 2003;136:205–13. doi: 10.1016/S1095-6433(03)00134-X. [DOI] [PubMed] [Google Scholar]
- Sterba JA, Lundgren CEG. Diving bradycardia and breath-holding time in man . Undersea Biomed Res. 1985;12:139–50. [PubMed] [Google Scholar]
- Ferretti G, Veicsteinas A, Rennie DW. Conductive and convective heat flows of exercising humans in cold water . J Appl Physiol (1985). 1989;67:2473–80. doi: 10.1152/jappl.1989.67.6.2473. [DOI] [PubMed] [Google Scholar]
- Bonomo M, Cairoli R, Verde G, Morelli L, Moreo A, Grottaglie MD, et al. Safety of recreational scuba diving in type 1 diabetic patients: the deep monitoring programme . Diabetes Metab. 2009;35:101–7. doi: 10.1016/j.diabet.2008.08.007. [DOI] [PubMed] [Google Scholar]
- Lormeau B, Sola A, Tabah A, Chiheb S, Dufaitre L, Thurninger O, et al. Blood glucose changes and adjustments of diet and insulin doses in type 1 diabetic patients during scuba diving (for a change in French regulations) . Diabetes Metab. 2005;31:144–51. doi: 10.1016/S1262-3636(07)70180-5. [DOI] [PubMed] [Google Scholar]
- Adolfsson P, Örnhagen H, Jendle J. Accuracy and reliability of continuous glucose monitoring in individuals with type 1 diabetes during recreational diving . Diabetes Technol Ther. 2009;11:493–7. doi: 10.1089/dia.2009.0017. [DOI] [PubMed] [Google Scholar]
- Adolfsson P, Örnhagen H, Jendle J. The benefits of continuous glucose monitoring and a glucose monitoring schedule in individuals with type 1 diabetes during recreational diving . J Diabetes Sci Technol. 2008;2:778–84. doi: 10.1177/193229680800200505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pieri M, Cialoni D, Marroni A. Continuous real-time monitoring and recording of glycemia during scuba diving: Pilot study . Undersea Hyperb Med. 2016;43:265–72. [PubMed] [Google Scholar]
- Schneider S, Cheung JJH, Frick H, Krehan S, Micke F, Sauer M, et al. When neuroscience gets wet and hardcore: Neurocognitive markers obtained during whole body water immersion . Exp Brain Res. 2014;232:3325–31. doi: 10.1007/s00221-014-4019-5. [DOI] [PubMed] [Google Scholar]
- Ratmanova P, Semenyuk R, Popov D, Kuznetsov S, Zelenkova I, Napalkov D, et al. Prolonged dry apnoea: Effects on brain activity and physiological functions in breath-hold divers and non-divers . Eur J Appl Physiol. 2016;116:1367–77. doi: 10.1007/s00421-016-3390-2. [DOI] [PubMed] [Google Scholar]
- Teruoka G. Die Ama und ihre Arbeit - Vorläufiger Bericht. Eine Untersuchung über die japanischen Taucherinnen . Arbeitsphysiologie. 1932;5:239–51. doi: 10.1007/BF02009115. (Ger). [DOI] [Google Scholar]
- Rahn H, Tetsuro Y, editors. Physiology of breath-hold diving and the Ama of Japan: Papers. Washington (DC): The National Academies Press; 1965. [Google Scholar]


