Abstract
Objective:
To describe the syndrome of physician burnout within neonatology, its relation to neonatal quality of care, and outline potential solutions.
Findings:
Burnout affects up to half of physicians, including up to one-third of neonatologists, at any given time. It is linked to suicidality, substance abuse, and intent to leave practice, and it is strongly associated with reduced quality of care in the published literature. Resilience and mindfulness interventions rooted in positive psychology may reduce burnout among individual providers. Because burnout is largely driven by organizational factors, system-level attention to leadership, teamwork, and practice efficiency can reduce burnout at the level of the organization.
Conclusions:
Burnout is common among neonatologists and consistently relates to decreased quality of patient care in a variety of dimensions. Personal resilience training and system-wide organizational interventions are needed to reverse burnout and promote high-quality neonatal care.
SUMMARY
Burnout is highly prevalent in neonatology, and associates with negative outcomes for providers, patients, and organizations. Individual interventions include resilience and mindfulness training rooted in positive psychology. Organizational interventions include developing physician-leaders, cultivating community and organizational culture, improving practice efficiency, and optimizing administrative policies.
INTRODUCTION
Physician burnout
Neonatology is a profession with demanding work schedules, intense interpersonal interactions, frequent complex and high-stakes decisions in the face of uncertainty, and rapidly developing new technologies. Many neonatologists chose this career because they were inspired by the potential to make a meaningful and longstanding difference in the lives of the patients and their families, but the modern practice environment now makes professional satisfaction more challenging. Neonatologists, along with physicians as a whole, are burdened by decreasing autonomy, reduced time at the bedside, and increasing barriers to balancing work and personal responsibilities. It is not surprising that burnout in physicians is much higher than in the general working population and remains high despite increasing recognition of its effects.1
Burnout is a work-related, reversible syndrome primarily consisting of emotional exhaustion and/or depersonalization. It is inversely related to well-being, professional fulfillment, and compassion satisfaction.2–4 The prevalence of neonatologist burnout is not well described, but is estimated to be 20–30%.4–6 Although some drivers of burnout may be independent of specialization, neonatologists may experience unique drivers of burnout. For example, neonatologist exposure to the suffering and death of infants – a painful and unsettling experience – may cause emotional labor and moral distress, leading to compassion fatigue and emotional exhaustion.4,7 Furthermore, the complexities of working with families of critically ill babies can be taxing and ethically challenging.8
Definition and measurement
Burnout is identified through survey instruments, most commonly the Emotional Exhaustion and Depersonalization subscales of the Maslach Burnout Inventory (MBI).9 The Emotional Exhaustion subscale consists of 9 prompts (i.e. “I feel emotionally drained from my work.”), and the Depersonalization subscale consists of 5 prompts (i.e. “I’ve become more callous toward people since I took this job.”). Both are scored on a 7-point Likert scale from “Never” (0) to “Every day” (6). A score of ≥27 for Emotional Exhaustion or ≥10 for Depersonalization is typically considered indicative of burnout symptoms. However, there are a myriad of alternative burnout inventories and scoring methods represented in the literature, each with different lengths and markers of psychometric validity as outlined in Table 1.
Table 1.
Selected burnout inventories, scales, and psychometric profiles
| Burnout instrument | Number of prompts | Scale used | Internal consistency (Cronbach’s α) | Test–retest reliability (r) | Concurrent validity (r) |
|---|---|---|---|---|---|
| Maslach Burnout Inventory (MBI)10 | |||||
| MBI – Emotional Exhaustion | 9 | 0 – 6 | 0.80 – 0.92 | 0.65 | 0.35 – 0.55 |
| MBI – Depersonalization | 5 | 0 – 6 | 0.36 – 0.86 | 0.60 | 0.14 – 0.36 |
| MBI – Personal Accomplishment | 8 | 0 – 6 | 0.65 – 0.83 | 0.67 | 0.10 – 0.18 |
| Copenhagen Burnout Inventory (CBI)11 | |||||
| CBI – Personal fatigue | 6 | 1 – 5 | 0.89 – 0.93 | 0.95 | 0.03 – 0.67 |
| CBI – Work fatigue | 7 | 1 – 5 | 0.84 – 0.88 | 0.83 – 0.84 | -- |
| CBI – Client–related burnout | 6 | 1 – 5 | 0.78 – 0.87 | 0.90 | 0.22 – 0.63 |
| Single–Item Burnout Measure12 | 1 | 1 – 5 | n/a | 0.79 | |
| Oldenburg Burnout Inventory (OLBI)13 | |||||
| OLBI – Exhaustion | 8 | 1 – 4 | 0.66 – 0.89 | 0.73 | -- |
| OLBI – Disengagement | 8 | 1 – 4 | 0.65 – 0.93 | 0.67 | -- |
| Shirom–Melamed Burnout Measure14 | 14 | 1 – 7 | 0.82 – 0.88 | -- | 0.35 – 0.52 |
| Professional Fulfillment Index – Overall burnout scale2 | 10 | 0 – 4 | 0.92 | 0.80 | 0.71 |
| Bergen Burnout Inventory15 | 15 | 1 – 4 | 0.83 – 0.85 | -- | -- |
| Copenhagen Psychosocial Questionnaire – Burnout dimension16 | 6 | 1 – 5 | 0.75 – 0.85 | 0.72 – 0.82 | -- |
| Professional Quality of Life Scale17 | 30 | 1 – 5 | 0.74 – 0.80 | -- | 0.44 – 0.51 |
| SCORE – Personal burnout scale18,19 | 5 | 0 – 4 | 0.85 – 0.93 | -- | -- |
| Utrecht Burnout Scale20 | 17 | 0 – 6 | 0.84 – 0.92 | 0.89 | 0.35 – 0.58 |
Reproduced with permission from Tawfik et al. Evidence Relating Health Care Provider Burnout and Quality of Care: A Systematic Review and Meta-analysis. Annals of Internal Medicine. 2019; 171: 555–567. doi:10.7326/M19-1152 ©American College of Physicians.
Although there has been suspicion that variability in assessment methods reduces the ability to draw conclusions,21 the relationship between burnout and quality of care in the published literature – regardless of assessment tool – is well-established.22
RISK FACTORS
Individual factors and work-life integration
Although burnout is a work-related syndrome, the work responsibilities of a physician interact heavily with family life and personal identity, and these domains are firmly related to physician well-being as illustrated in Figure 1.23,24
Figure 1.
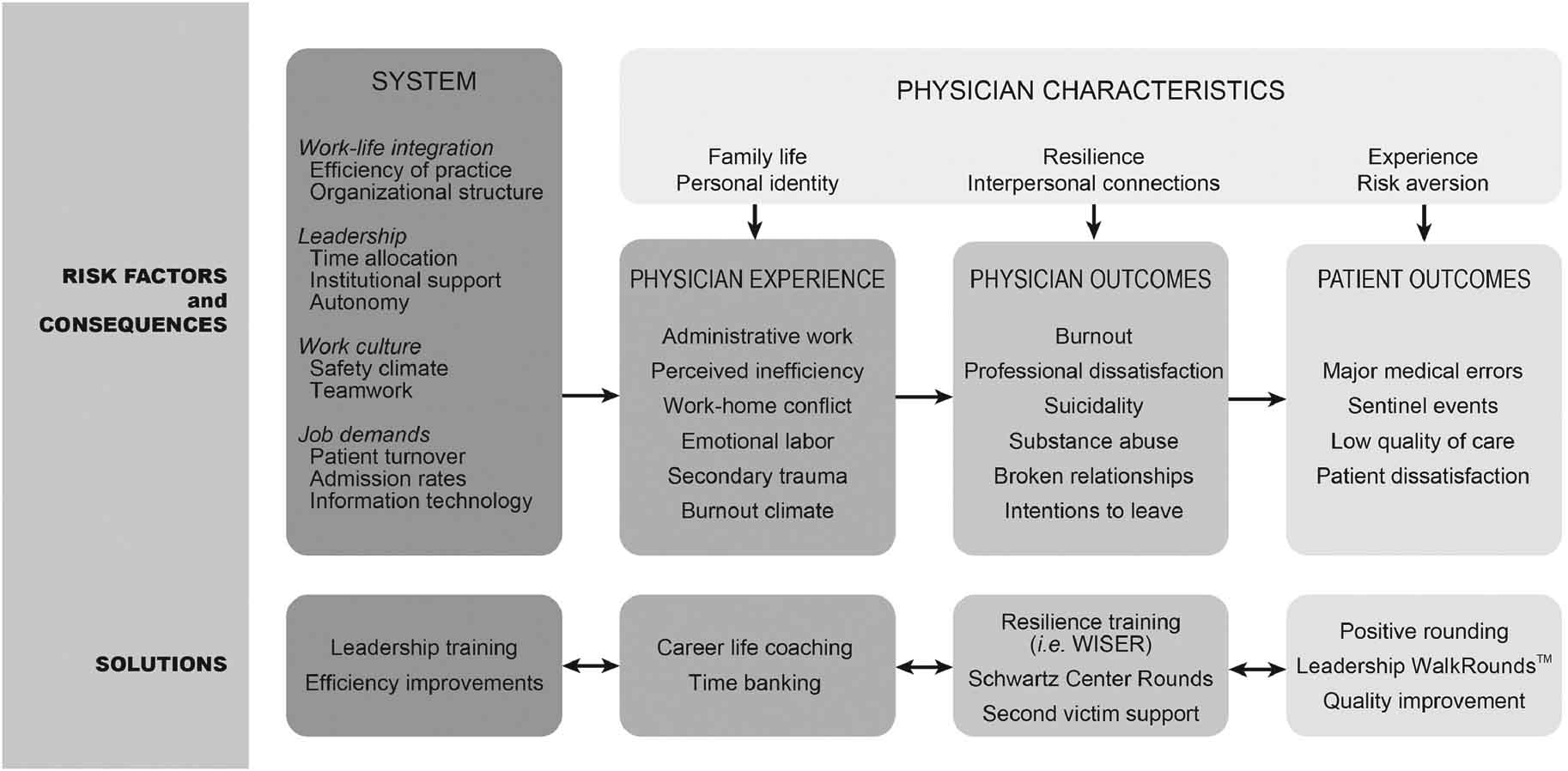
Conceptual framework relating system risk factors to physician experience, with downstream consequences on physician outcomes and patient outcomes, plus examples of potential solutions. WISER: Web-based Implementation of the Science of Enhancing Resilience.
Work-home conflict is a perceived need to fulfill work and personal responsibilities simultaneously, resulting in a requirement to prioritize one over the other. Such conflicts are highly prevalent (with 44–62% of physicians and their partners reporting such conflicts in any given 3-week period) and are associated with younger age, female sex, academic practice, and higher work hours.23,24 Work-home conflict correlates with increased burnout and depressive symptoms, lower quality of life, and decreased career satisfaction.25,26 Conversely, having the ability and opportunity to adequately balance work commitments and personal obligations, often termed work-life integration, strongly relates to reduced burnout.3,27
An existing gender gap in physician burnout may be partially attributed to differences in work-home conflict. Women are more likely to experience both burnout and work-home conflict, and are also nearly 3 times as likely to believe that child-rearing has hindered their career advancement.23,28 These increased rates of work-home conflict among women physicians are widespread among specialties and have been detected as early as 6 months into internship.26 However, this issue is particularly relevant in pediatric specialties where more than half of the working force is female. Among pediatricians, being female is independently associated with lower perceived work-life integration and career satisfaction.29
Within neonatology, burnout prevalence has been found to be higher among those with greater years of experience in one study.5 However, it is not known if this association reflects cumulative stress from adverse experiences, career advancement, personal changes, or other age-related factors. In addition, working day shifts has been associated with slightly higher rates of burnout, particularly among nurses.5 It has been hypothesized that these differences may be related to increased job demands during daytime hours or increased emotional labor if goals of care discussions and withdrawal of technological support occur more commonly during daytime hours.5 Additional emotional labor may occur when patient families distrust physicians, with burnout among resident physicians found to inversely correlate with perceptions of trust.30
Organizational factors
Physician experience and risk for burnout is heavily influenced by the surrounding work environment. This environment is in turn affected by decisions at the local leadership level, by the culture of teamwork and safety, and by the particular patient care demands.
The style, perceptions, and quality of local organizational leadership can profoundly influence physician well-being. In a single-center study of nearly 3000 physicians from diverse specialties, behaviors of the first-line physician leadership explained 11% of the variance in burnout and 47% of the variance in job satisfaction among divisions.31 Job satisfaction strongly relates to how leaders allocate physicians’ time. Among academic physicians, Demmy et al reported a positive correlation between job satisfaction and institutional support for clinical/research interests.32 Other studies indicate that physicians who spend greater than 20% of their time on the aspect of work that is most meaningful to them have a lower likelihood of burnout, suggesting that the identification and promotion of meaningful time allocation may improve physician well-being.33 In a study of pediatricians, clinical decision-making autonomy associated with less burnout, better work-life integration, and higher career satisfaction.29
Interpersonal interactions at work can also affect physician well-being. Neonatology is a highly interactive field requiring shared responsibility for patient safety, strong teamwork, and shared experiences of patient outcomes. Safety climate represents a recognition of the shared responsibility for patient safety and the patterns of behavior intended to minimize patient harm,34 typically measured via survey responses (e.g. Safety Attitudes Questionnaire, SCORE survey, and the Hospital Survey on Patient Safety Culture).27,35,36 A better safety climate in a work-unit is strongly associated with lower rates of burnout, likely related to a commitment to shared values and the resultant impetus for teamwork and collaboration.3,37
Teamwork, a core component of patient safety, can mitigate some of the negative effects of excess workload and poor practice efficiency. Beyond simply reducing the workload for individual team members, a strong sense of teamwork can cement an individual’s work experience within a positive social construct fostering resilience and mutual support.38 On the other hand, poor teamwork can result in increased task load, inefficient workflows, and social isolation, which may contribute both to emotional exhaustion (a chronic state of physical and emotional depletion secondary to chronic stress) and depersonalization (a detachment from the self and indifference towards work).37 In one longitudinal study, emotional exhaustion also predicted subsequent poor teamwork, indicating that poor teamwork and burnout may be linked bi-directionally, creating the potential for a self-perpetuating cycle.39
Particularly, in intensive care settings such as the NICU, job demands may outweigh job resources. Job demands directly related to the needs of the patients, such as patient turnover and admission rates, are associated with higher burnout in the NICU.40 Yet job demands also include organizational requirements not directly related to patient care. Electronic health record (EHR) implementation is one notable method through which job demands have increased in recent years, as physicians spend more time on documentation, order entry, and communication tasks than previously required.41 If job resources to assist physicians with these burdens do not increase concomitantly, EHR implementation can result in a higher likelihood of burnout, with EHR factors explaining 7% of the variation in physician burnout in one recent study.40,42 However, the EHR also provides opportunities for improved efficiency through team-based documentation and automation of repetitive tasks, that may be harnessed to improve physician satisfaction.43,44
CONSEQUENCES OF BURNOUT
Provider consequences
Physician burnout contributes to a variety of adverse effects at the physician, patient, and organization levels, with links to physician suicidality, alcohol abuse, and broken relationships.45–48 Suicidal ideation is strongly associated with burnout, and suicide rates among physicians are higher than the general population, with up to 5.7 times the risk among female physicians.45,49 Although the prevalence of alcohol abuse within pediatric specialties is lower than the average for all physicians, there exists a strong association between alcohol abuse and burnout independent of specialty.47 No similar relationship has been demonstrated for other substances of abuse.47 Finally, work-home conflict is closely related to burnout, and spouses/partners of physicians who spend less time with them at home report lower relationship satisfaction.48
Employment consequences
Burnout also carries employment implications that threaten the ability of health care organizations to provide high quality patient care.50 Burnout is, therefore, an organizational problem indicating a need for process improvement rather than an individual problem in need of remediation. This distinction is particularly important when job demands are at risk of outweighing resources, as disciplinary action against physicians experiencing burnout could contribute to workforce shortages in addition to stigmatizing providers affected by it.51 Physicians with burnout are also more likely to consider leaving their current position, resulting in impaired retention and recruitment of physicians that could further exacerbate workforce shortages and increased work-home conflict among those remaining.28,52 Burnout-related physician turnover also has deep financial effects, costing the US health care system approximately $4.6 billion annually.50,53 Of note, burnout can result in unprofessional behavior or impaired quality of care, and thus it is imperative to develop a culture wherein individuals have the psychological safety to speak up when they need assistance or have suggestions for process improvement, with those who exhibit unprofessional behavior held accountable.54
Patient Consequences
Physician burnout associates with diminished quality of care in a variety of domains, including poor adherence to best practice guidelines, increased medical errors, poor patient outcomes, and reduced patient satisfaction.22,55–60 In a 2015 meta-analysis, Salyers et al59 reported effect sizes of r=−0.26 and r=−0.23 for the relationship between burnout and quality and safety outcomes, respectively. More recently, a 2017 meta-analysis by Panagioti et al.60 reported summary odds ratios of 1.96 for patient safety incidents and 2.28 for reduced patient satisfaction among physicians with burnout. In a 2019 meta-analysis, Tawfik et al22 identified 114 unique combinations of burnout and quality of care metrics reported in the literature, over half of which had significant summary effect sizes relating burnout to impaired quality of care.
NICU patients are particularly vulnerable to perturbations in the quality of care, and the relationship between burnout and quality of care in the NICU is an ongoing area of research. Profit et al. found that burnout tends to cluster within NICUs, exhibiting climate-like features, and that NICUs with high burnout were more likely to have scores below 75/100 on safety climate surveys.61 A related study by Tawfik et al. found evidence relating individual components of emotional exhaustion to health care-associated infections, though not all relationships were significant.62 Among NICU nurses, Rochefort et al. report a negative association between emotional exhaustion and subjective assessment of quality of care,63 and Winning et al. recently reported a positive association between burnout and involvement in adverse patient events.64 These findings are similar to those found among other inpatient pediatrics settings, with burnout often negatively associated with safety climate and self-reported quality of care, but less frequently related to objectively-measured outcomes.65–67
Causal theory
The observed relationships between burnout and quality of care are likely multifactorial and causality is difficult to establish. Individuals experiencing burnout may have less time or commitment to optimize the care of their patients, take more unnecessary risks, or lack ability to pay attention to necessary details or recognize the consequences of their actions.68 On the other hand, exposure to adverse patient events or recognition of poor quality of care may result in moral distress to the providers. This phenomenon is often referred to as secondary trauma, particularly in relation to sentinel events or important safety incidents, however it is possible that it could arise from frequent minor incidents as well.69 In this instance, the adverse event precipitates burnout from resulting moral distress.
SOLUTIONS
Individual resilience
Despite the well-documented descriptions of burnout and its relation to quality of care, few interventions to build resilience have been rigorously tested in clinical trials. Psychological research has consistently shown that experiencing positive emotions is central to building resilience and improves sense of purpose and recovery after emotional upheavals or other secondary trauma.70 Though not studied in NICU care, randomized controlled trials of meditation suggest that positive emotion is important in improving well-being.70 Interventions designed to elicit positive emotions and connections with colleagues, such as the Web-based Implementation of the Science of Enhancing Resilience (WISER) program (enrollment available at hsq.dukehealth.org/tools) and the Colleagues Meeting to Promote and Sustain Satisfaction (COMPASS) program, have shown consistent benefit at reducing physician burnout among NICU providers and internal medicine physicians.71,72 Other interventions commonly focus on stress management, mindfulness-based exercises, or self-care, with the majority reporting 4 to 7-point reductions in emotional exhaustion scores (on a 54-point scale).73
Organizations can also play a part in promoting the development of personal resilience skills, and thus contribute to individuals’ attention to self-care. Supporting these approaches at an organizational level may increase physician engagement while also conveying organizational commitment to well-being. Widespread introduction of these approaches may also promote psychological safety and reduce the stigma often attached to psychological interventions. However, it is likely that physician receptiveness will be greatest when promoting these tools in the context of other organizational changes to promote well-being and in combination with protected time or other support.74 Broad uptake of these practices will likely require that physician and organizational culture place value on self-care and provide time to participate in such activities.
System-level interventions
Ultimately, burnout is a work-related phenomenon rooted in organizational causes. Burnout also clusters within NICUs, indicating that it is a group-level construct more than an individual phenomenon.37 Thus, a system-level approach is needed to prevent and reduce burnout, regardless of improvements in individual resilience. Key organizational features promoting well-being include high-quality leadership, teamwork culture, and efficiency of practice. Each of these features contribute to improved well-being, but effective leaders are foundational to establishing a culture that gives everybody a voice, an environment that balances support with accountability, and a care context that promotes professional satisfaction.
A recent survey of academic NICU medical directors found that only 40% had received any formal leadership training, and nearly half of respondents felt that leadership training would improve their effectiveness.75 These insights, plus the degree of influence that leaders exert on burnout and job satisfaction, suggest a tremendous opportunity for improvement through interventions that promote effective leadership. It has been hypothesized that a key mediating factor in mitigating physician burnout is frequent and useful feedback from leaders, mentors, or peers.76,77 An organizational commitment to selecting and developing high quality physician-leaders can serve to promote alignment of individual values and organizational priorities—a key construct undergirding physician interactions with leadership.78 Strategies include initial selection of leaders based on leadership potential, professional development and directed coaching, and training in leadership skills at all stages of career development.31,79
Leadership WalkRounds™ and positive rounding (a focus on things that go well) are concrete examples of strategies that can promote a positive physician culture, improve interactions with leadership, and promote a safety and teamwork climate when performed consistently and with appropriate feedback.18,80 WalkRounds™ feedback and positive rounding that deliberately seek to elicit positive emotion in addition to identifying risks to safety and quality have shown promise at improving well-being. By using prompts such as “Please share three things that are going well in this work setting, and one thing that could be better,” the emphasis shifts from deficiencies and fear to pride and hope. A cross-sectional analysis of 44 NICUs found that those with the most WalkRounds™ feedback had mean teamwork and safety climate scores that were up to 30 points higher than their counterparts with the least feedback, and burnout scores that were 10 points lower (all on 100-point scales).81
Other organizational interventions may seek to improve connections among colleagues and support personal resilience. One prominent example is Schwartz Center Rounds, which typically consists of a monthly lunch and a one hour discussion of the care of a particular patient. This discussion is open to all clinical and non-clinical staff, with an emphasis on the emotional and ethical consequences of caring for challenging patients. Several small studies have found introduction of Schwartz Rounds to be well-received by attendees, although limited data exist regarding its effect on burnout or other markers of well-being.82
Since work-home conflict is strongly associated with burnout, NICUs also have the opportunity to systematically support the role of physicians as caregivers. For women of childbearing age, this may include accommodations for breastfeeding, including time and physical space for pumping.83 Policies that promote equity amongst male and female physicians may include flexibility in work schedule to accommodate reduction in work with commensurate pay decreases, providing sick child care, or facilitating clinical coverage for physicians caring for a sick loved one.
Stemming from a recognition that policies alone are insufficient, career-life coaching programs have been developed in which participants work with a coach to create a customized plan identifying and balancing competing priorities, then work directly with their division leadership to implement this plan. Another related strategy is time-banking, which addresses time scarcity by awarding credits to physicians for engaging in team-oriented behaviors (e.g. serving on a selection committee or covering a clinical shift for a colleague on short notice). These credits are then redeemable for personal or professional time-saving services such as home meal delivery or office organizing.84 A pilot program that combined career-life coaching and time-banking was recently found to associate with improved wellness and satisfaction, and higher academic achievements than matched controls.84
In sum, a variety of interventions have demonstrated efficacy at reducing burnout, ranging from individual mindfulness strategies to organizational restructuring.73 However, it is not yet known which interventions provide the greatest effectiveness for specific groups of physicians or practice settings, or if particular combinations of interventions could provide multiplicative benefits. Additional clinical trials are needed to determine the relative effectiveness of burnout interventions for varying physicians and practice settings, and to determine if reducing burnout improves quality of care.73 Future trials should include widely-accepted core quality metrics where feasible, and employ research best practices such as trial registration and protocol pre-specification to reduce the risk for bias.22
Prevention
Prevention and early identification of burnout may further enhance the ability of organizations to improve physician well-being. No validated tools exist specifically for burnout prevention among physicians, but many of the strategies outlined above could be targeted to settings where physicians have known risk factors for burnout, rather than limited to settings where burnout has already been found to be prevalent. Physicians may also support their own burnout prevention, by deliberately seeking employment with organizations that prioritize their well-being, such as those that support work-life integration or leadership training. Routine screening for burnout is now common in many institutions, although a clear and evidence-based response to screening results is not yet established, limiting the utility of this approach outside of scholarly pursuits.85,86
CONCLUSION
In conclusion, healthcare provider burnout is highly prevalent, including among neonatologists. Physician well-being is critical to high quality patient care and organizational success, necessitating interventions to reverse this trend. Organizational interventions that can effectively reduce burnout and promote well-being include developing physician-leaders, cultivating community and organizational culture, improving practice efficiency, and optimizing administrative policies. In neonatology, additional emotional burden highlights the urgency of addressing this epidemic.
Acknowledgments
From the Stanford University School of Medicine
Supported in part by the Stanford Maternal and Child Health Research Institute and the Eunice Kennedy Shriver National Institute of Child Health and Human Development (R01 HD084679-01, Profit/Sexton Co-PI)
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
DISCLOSURES
The authors report no conflicts of interest, including no proprietary or commercial interest in any product mentioned or concept discussed in the article.
Contributor Information
Daniel S. Tawfik, Division of Pediatric Critical Care Medicine, Department of Pediatrics, Stanford University School of Medicine, Stanford, CA, USA 770 Welch Road, Suite 435, Palo Alto, CA, USA 94304.
Jochen Profit, Perinatal Epidemiology and Health Outcomes Research Unit, Division of Neonatology, Department of Pediatrics, Stanford University School of Medicine, Stanford, CA, USA; California Perinatal Quality Care Collaborative, Palo Alto, CA, USA.
REFERENCES
- 1.Shanafelt TD, West CP, Sinsky C, et al. Changes in Burnout and Satisfaction With Work-Life Integration in Physicians and the General US Working Population Between 2011 and 2017. Mayo Clin Proc. 2019. [DOI] [PubMed] [Google Scholar]
- 2.Trockel M, Bohman B, Lesure E, et al. A Brief Instrument to Assess Both Burnout and Professional Fulfillment in Physicians: Reliability and Validity, Including Correlation with Self-Reported Medical Errors, in a Sample of Resident and Practicing Physicians. Acad Psychiatry. 2018;42(1):11–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Schwartz SP, Adair KC, Bae J, et al. Work-life balance behaviours cluster in work settings and relate to burnout and safety culture: a cross-sectional survey analysis. BMJ Qual Saf. 2019;28(2):142–150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Weintraub AS, Geithner EM, Stroustrup A, Waldman ED. Compassion fatigue, burnout and compassion satisfaction in neonatologists in the US. Journal of perinatology: official journal of the California Perinatal Association. 2016;36(11):1021–1026. [DOI] [PubMed] [Google Scholar]
- 5.Tawfik DS, Sexton JB, Kan P, et al. Burnout in the neonatal intensive care unit and its relation to healthcare-associated infections. Journal of perinatology: official journal of the California Perinatal Association. 2017;37(3):315–320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bellieni CV, Righetti P, Ciampa R, Iacoponi F, Coviello C, Buonocore G. Assessing burnout among neonatologists. The journal of maternal-fetal & neonatal medicine: the official journal of the European Association of Perinatal Medicine, the Federation of Asia and Oceania Perinatal Societies, the International Society of Perinatal Obstet. 2012;25(10):2130–2134. [DOI] [PubMed] [Google Scholar]
- 7.Prentice TM, Gillam L, Davis PG, Janvier A. The use and misuse of moral distress in neonatology. Semin Fetal Neonatal Med. 2018;23(1):39–43. [DOI] [PubMed] [Google Scholar]
- 8.Donohue PK, Williams EP, Wright-Sexton L, Boss RD. “It’s Relentless”: Providers’ Experience of Pediatric Chronic Critical Illness. Journal of palliative medicine. 2018;21(7):940–946. [DOI] [PubMed] [Google Scholar]
- 9.Maslach C, Jackson SE. Maslach Burnout Inventory. In. Palo Alto, CA: Consulting Psychologists Press, Inc; 1981. [Google Scholar]
- 10.Poghosyan L, Aiken LH, Sloane DM. Factor structure of the Maslach burnout inventory: An analysis of data from large scale cross-sectional surveys of nurses from eight countries. International Journal of Nursing Studies. 2009;46(7):894–902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Mahmoudi S, Atashzadeh-Shoorideh F, Rassouli M, Moslemi A, Pishgooie AH, Azimi H. Translation and Psychometric Properties of the Copenhagen Burnout Inventory in Iranian Nurses. Iran J Nurs Midwifery Res. 2017;22(2):117–122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Dolan ED, Mohr D, Lempa M, et al. Using a single item to measure burnout in primary care staff: a psychometric evaluation. Journal of General Internal Medicine. 2015;30(5):582–587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Baka L, Basinska BA. [Psychometric properties of the Polish version of the Oldenburg Burnout Inventory (OLBI)]. Med Pr. 2016;67(1):29–41. [DOI] [PubMed] [Google Scholar]
- 14.Lundgren-Nilsson A, Jonsdottir IH, Pallant J, Ahlborg G Jr. Internal construct validity of the Shirom-Melamed Burnout Questionnaire (SMBQ). BMC Public Health. 2012;12:1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Salmela-Aro K, Rantanen J, Hyvonen K, Tilleman K, Feldt T. Bergen Burnout Inventory: reliability and validity among Finnish and Estonian managers. Int Arch Occup Environ Health. 2011;84(6):635–645. [DOI] [PubMed] [Google Scholar]
- 16.Thorsen SV, Bjorner JB. Reliability of the Copenhagen Psychosocial Questionnaire. Scand J Public Health. 2010;38(3 Suppl):25–32. [DOI] [PubMed] [Google Scholar]
- 17.Hemsworth D, Baregheh A, Aoun S, Kazanjian A. A critical enquiry into the psychometric properties of the professional quality of life scale (ProQol-5) instrument. Appl Nurs Res. 2018;39:81–88. [DOI] [PubMed] [Google Scholar]
- 18.Sexton JB, Adair KC, Leonard MW, et al. Providing feedback following Leadership WalkRounds is associated with better patient safety culture, higher employee engagement and lower burnout. BMJ Qual Saf. 2018;27(4):261–270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Sexton JB, Schwartz SP, Chadwick WA, et al. The associations between work-life balance behaviours, teamwork climate and safety climate: cross-sectional survey introducing the work-life climate scale, psychometric properties, benchmarking data and future directions. BMJ Quality & Safety. 2017;26(8):632–640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Torabinia M, Mahmoudi S, Dolatshahi M, Abyaz MR. Measuring engagement in nurses: the psychometric properties of the Persian version of Utrecht Work Engagement Scale. Med J Islam Repub Iran. 2017;31:15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Rotenstein LS, Torre M, Ramos MA, et al. Prevalence of Burnout Among Physicians: A Systematic Review. JAMA. 2018;320(11):1131–1150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Tawfik DS, Scheid A, Profit J, et al. Evidence Relating Health Care Provider Burnout and Quality of Care: A Systematic Review and Meta-analysis. Annals of internal medicine. 2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Dyrbye LN, Shanafelt TD, Balch CM, Satele D, Sloan J, Freischlag J. Relationship between work-home conflicts and burnout among American surgeons: a comparison by sex. Arch Surg. 2011;146(2):211–217. [DOI] [PubMed] [Google Scholar]
- 24.Dyrbye LN, Sotile W, Boone S, et al. A survey of U.S. physicians and their partners regarding the impact of work-home conflict. Journal of general internal medicine. 2014;29(1):155–161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Dyrbye LN, Freischlag J, Kaups KL, et al. Work-home conflicts have a substantial impact on career decisions that affect the adequacy of the surgical workforce. Arch Surg. 2012;147(10):933–939. [DOI] [PubMed] [Google Scholar]
- 26.Guille C, Frank E, Zhao Z, et al. Work-Family Conflict and the Sex Difference in Depression Among Training Physicians. JAMA internal medicine. 2017;177(12):1766–1772. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Sexton JB, Schwartz SP, Chadwick WA, et al. The associations between work-life balance behaviours, teamwork climate and safety climate: cross-sectional survey introducing the work-life climate scale, psychometric properties, benchmarking data and future directions. BMJ Qual Saf. 2017;26(8):632–640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Shanafelt TD, Mungo M, Schmitgen J, et al. Longitudinal Study Evaluating the Association Between Physician Burnout and Changes in Professional Work Effort. Mayo Clin Proc. 2016;91(4):422–431. [DOI] [PubMed] [Google Scholar]
- 29.Starmer AJ, Frintner MP, Freed GL. Work-Life Balance, Burnout, and Satisfaction of Early Career Pediatricians. Pediatrics. 2016;137(4). [DOI] [PubMed] [Google Scholar]
- 30.Huang EC, Pu C, Huang N, Chou YJ. Resident burnout in Taiwan Hospitals-and its relation to physician felt trust from patients. J Formos Med Assoc. 2019;118(10):1438–1449. [DOI] [PubMed] [Google Scholar]
- 31.Shanafelt TD, Gorringe G, Menaker R, et al. Impact of organizational leadership on physician burnout and satisfaction. Mayo Clin Proc. 2015;90(4):432–440. [DOI] [PubMed] [Google Scholar]
- 32.Demmy TL, Kivlahan C, Stone TT, Teague L, Sapienza P. Physicians’ perceptions of institutional and leadership factors influencing their job satisfaction at one academic medical center. Academic medicine: journal of the Association of American Medical Colleges. 2002;77(12 Pt 1):1235–1240. [DOI] [PubMed] [Google Scholar]
- 33.Shanafelt TD, West CP, Sloan JA, et al. Career fit and burnout among academic faculty. Archives of internal medicine. 2009;169(10):990–995. [DOI] [PubMed] [Google Scholar]
- 34.Tawfik DS, Thomas EJ, Vogus TJ, et al. Safety climate, safety climate strength, and length of stay in the NICU. BMC Health Serv Res. 2019;19(1):738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Profit J, Etchegaray J, Petersen LA, et al. The Safety Attitudes Questionnaire as a tool for benchmarking safety culture in the NICU. Arch Dis Child Fetal Neonatal Ed. 2012;97(2):F127–132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Profit J, Lee HC, Sharek PJ, et al. Comparing NICU teamwork and safety climate across two commonly used survey instruments. BMJ Qual Saf. 2016;25(12):954–961. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Profit J, Sharek PJ, Amspoker AB, et al. Burnout in the NICU setting and its relation to safety culture. BMJ Qual Saf. 2014;23(10):806–813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Tawfik DS, Sexton JB, Adair KC, Kaplan HC, Profit J. Context in Quality of Care: Improving Teamwork and Resilience. Clin Perinatol. 2017;44(3):541–552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Welp A, Meier LL, Manser T. The interplay between teamwork, clinicians’ emotional exhaustion, and clinician-rated patient safety: a longitudinal study. Crit Care. 2016;20(1):110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Tawfik DS, Phibbs CS, Sexton JB, et al. Factors Associated With Provider Burnout in the NICU. Pediatrics. 2017;139(5). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Baumann LA, Baker J, Elshaug AG. The impact of electronic health record systems on clinical documentation times: A systematic review. Health Policy. 2018;122(8):827–836. [DOI] [PubMed] [Google Scholar]
- 42.Kroth PJ, Morioka-Douglas N, Veres S, et al. Association of Electronic Health Record Design and Use Factors With Clinician Stress and Burnout. JAMA Netw Open. 2019;2(8):e199609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Pozdnyakova A, Laiteerapong N, Volerman A, et al. Impact of Medical Scribes on Physician and Patient Satisfaction in Primary Care. Journal of general internal medicine. 2018;33(7):1109–1115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Guo U, Chen L, Mehta PH. Electronic health record innovations: Helping physicians - One less click at a time. Health Inf Manag. 2017;46(3):140–144. [DOI] [PubMed] [Google Scholar]
- 45.Shanafelt TD, Balch CM, Dyrbye L, et al. Special report: suicidal ideation among American surgeons. Arch Surg. 2011;146(1):54–62. [DOI] [PubMed] [Google Scholar]
- 46.Center C, Davis M, Detre T, et al. Confronting depression and suicide in physicians: a consensus statement. JAMA. 2003;289(23):3161–3166. [DOI] [PubMed] [Google Scholar]
- 47.Oreskovich MR, Shanafelt T, Dyrbye LN, et al. The prevalence of substance use disorders in American physicians. Am J Addict. 2015;24(1):30–38. [DOI] [PubMed] [Google Scholar]
- 48.Shanafelt TD, Boone SL, Dyrbye LN, et al. The medical marriage: a national survey of the spouses/partners of US physicians. Mayo Clin Proc. 2013;88(3):216–225. [DOI] [PubMed] [Google Scholar]
- 49.Hawton K, Clements A, Sakarovitch C, Simkin S, Deeks JJ. Suicide in doctors: a study of risk according to gender, seniority and specialty in medical practitioners in England and Wales, 1979–1995. J Epidemiol Community Health. 2001;55(5):296–300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Shanafelt T, Goh J, Sinsky C. The Business Case for Investing in Physician Well-being. JAMA internal medicine. 2017;177(12):1826–1832. [DOI] [PubMed] [Google Scholar]
- 51.Shanafelt TD, Dyrbye LN, West CP. Addressing Physician Burnout: The Way Forward. JAMA. 2017;317(9):901–902. [DOI] [PubMed] [Google Scholar]
- 52.Shanafelt TD, Dyrbye LN, West CP, Sinsky CA. Potential Impact of Burnout on the US Physician Workforce. Mayo Clin Proc. 2016;91(11):1667–1668. [DOI] [PubMed] [Google Scholar]
- 53.Han S, Shanafelt TD, Sinsky CA, et al. Estimating the Attributable Cost of Physician Burnout in the United States. Annals of internal medicine. 2019. [DOI] [PubMed] [Google Scholar]
- 54.Egener BE, Mason DJ, McDonald WJ, et al. The Charter on Professionalism for Health Care Organizations. Academic medicine: journal of the Association of American Medical Colleges. 2017;92(8):1091–1099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Tawfik DS, Profit J, Morgenthaler TI, et al. Physician Burnout, Well-being, and Work Unit Safety Grades in Relationship to Reported Medical Errors. Mayo Clin Proc. 2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Welp A, Meier LL, Manser T. Emotional exhaustion and workload predict clinician-rated and objective patient safety. Frontiers in Psychology. 2015;5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Dewa CS, Loong D, Bonato S, Trojanowski L. The relationship between physician burnout and quality of healthcare in terms of safety and acceptability: a systematic review. BMJ Open. 2017;7(6):e015141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Hall LH, Johnson J, Watt I, Tsipa A, O’Connor DB. Healthcare Staff Wellbeing, Burnout, and Patient Safety: A Systematic Review. Plos One. 2016;11(7). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Salyers MP, Bonfils KA, Luther L, et al. The Relationship Between Professional Burnout and Quality and Safety in Healthcare: A Meta-Analysis. Journal of General Internal Medicine. 2017;32(4):475–482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Panagioti M, Geraghty K, Johnson J, et al. Association Between Physician Burnout and Patient Safety, Professionalism, and Patient Satisfaction: A Systematic Review and Meta-analysis. JAMA Intern Med. 2018;178(10):1317–1330. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 61.Profit J, Sharek PJ, Amspoker AB, et al. Burnout in the NICU setting and its relation to safety culture. Bmj Quality & Safety. 2014;23(10):806–813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Tawfik DS, Sexton JB, Kan P, et al. Burnout in the neonatal intensive care unit and its relation to healthcare-Associated infections. Journal of Perinatology. 2017;37(3):315–320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Rochefort CM, Clarke SP. Nurses’ work environments, care rationing, job outcomes, and quality of care on neonatal units. J Adv Nurs. 2010;66(10):2213–2224. [DOI] [PubMed] [Google Scholar]
- 64.Winning AM, Merandi JM, Lewe D, et al. The emotional impact of errors or adverse events on healthcare providers in the NICU: The protective role of coworker support. Journal of Advanced Nursing. 2018;74(1):172–180. [DOI] [PubMed] [Google Scholar]
- 65.Alves D, Guirardello E. Safety climate, emotional exhaustion and job satisfaction among Brazilian paediatric professional nurses. International Nursing Review. 2016;63(3):328–335. [DOI] [PubMed] [Google Scholar]
- 66.Weigl M, Schneider A, Hoffmann F, Angerer P. Work stress, burnout, and perceived quality of care: a cross-sectional study among hospital pediatricians. European Journal of Pediatrics. 2015;174(9):1237–1246. [DOI] [PubMed] [Google Scholar]
- 67.Holden RJ, Patel NR, Scanlon MC, Shalaby TM, Arnold JM, Karsh B-T. Effects of mental demands during dispensing on perceived medication safety and employee well-being: A study of workload in pediatric hospital pharmacies. Research in Social & Administrative Pharmacy. 2010;6(4):293–306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Halbesleben JR, Rathert C. Linking physician burnout and patient outcomes: exploring the dyadic relationship between physicians and patients. Health Care Management Review. 2008;33(1):29–39. [DOI] [PubMed] [Google Scholar]
- 69.Van Gerven E, Vander Elst T, Vandenbroeck S, et al. Increased Risk of Burnout for Physicians and Nurses Involved in a Patient Safety Incident. Medical care. 2016;54(10):937–943. [DOI] [PubMed] [Google Scholar]
- 70.Fredrickson BL, Cohn MA, Coffey KA, Pek J, Finkel SM. Open hearts build lives: positive emotions, induced through loving-kindness meditation, build consequential personal resources. J Pers Soc Psychol. 2008;95(5):1045–1062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.West CP, Dyrbye LN, Rabatin JT, et al. Intervention to promote physician well-being, job satisfaction, and professionalism: a randomized clinical trial. JAMA internal medicine. 2014;174(4):527–533. [DOI] [PubMed] [Google Scholar]
- 72.Sexton JB, Adair KC. Forty-five good things: a prospective pilot study of the Three Good Things well-being intervention in the USA for healthcare worker emotional exhaustion, depression, work-life balance and happiness. BMJ Open. 2019;9(3):e022695. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.West CP, Dyrbye LN, Erwin PJ, Shanafelt TD. Interventions to prevent and reduce physician burnout: a systematic review and meta-analysis. Lancet (London, England). 2016;388(10057):2272–2281. [DOI] [PubMed] [Google Scholar]
- 74.Tawfik DS, Profit J, Webber S, Shanafelt TD. Organizational Factors Affecting Physician Well-Being. Current Treatment Options in Pediatrics. 2019;5(1):11–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Barry JS, Baca MD, Parker TF. Neonatal Intensive Care Unit Medical Directors in Academic Institutions: Who Are They? J Pediatr. 2019;208:5–7 e1. [DOI] [PubMed] [Google Scholar]
- 76.Gordon EK, Baranov DY, Fleisher LA. The role of feedback in ameliorating burnout. Curr Opin Anaesthesiol. 2018;31(3):361–365. [DOI] [PubMed] [Google Scholar]
- 77.Gribben V, Bogetz A, Bachrach L, Blankenburg R. The Golden Ticket Project for peer recognition. Clin Teach. 2019;16(3):203–208. [DOI] [PubMed] [Google Scholar]
- 78.Leiter MP, Frank E, Matheson TJ. Demands, values, and burnout: relevance for physicians. Can Fam Physician. 2009;55(12):1224–1225, 1225 e1221–1226. [PMC free article] [PubMed] [Google Scholar]
- 79.Shanafelt T, Swensen S. Leadership and Physician Burnout: Using the Annual Review to Reduce Burnout and Promote Engagement. American journal of medical quality: the official journal of the American College of Medical Quality. 2017;32(5):563–565. [DOI] [PubMed] [Google Scholar]
- 80.Frankel A, Grillo SP, Pittman M, et al. Revealing and resolving patient safety defects: the impact of leadership WalkRounds on frontline caregiver assessments of patient safety. Health Serv Res. 2008;43(6):2050–2066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Sexton JB, Sharek PJ, Thomas EJ, et al. Exposure to Leadership WalkRounds in neonatal intensive care units is associated with a better patient safety culture and less caregiver burnout. BMJ Qual Saf. 2014;23(10):814–822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Taylor C, Xyrichis A, Leamy MC, Reynolds E, Maben J. Can Schwartz Center Rounds support healthcare staff with emotional challenges at work, and how do they compare with other interventions aimed at providing similar support? A systematic review and scoping reviews. BMJ Open. 2018;8(10):e024254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Pumped Grinberg C.. JAMA. 2018;320(10):977–978. [DOI] [PubMed] [Google Scholar]
- 84.Fassiotto M, Simard C, Sandborg C, Valantine H, Raymond J. An Integrated Career Coaching and Time-Banking System Promoting Flexibility, Wellness, and Success: A Pilot Program at Stanford University School of Medicine. Academic medicine: journal of the Association of American Medical Colleges. 2018;93(6):881–887. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Papazian L, Sylvestre A, Herridge M. Should all ICU clinicians regularly be tested for burnout? Yes. Intensive care medicine. 2018;44(5):681–683. [DOI] [PubMed] [Google Scholar]
- 86.Ricou B, Zampieri FG, Brown SM. Should all ICU clinicians regularly be tested for burnout? No. Intensive care medicine. 2018;44(5):684–686. [DOI] [PubMed] [Google Scholar]


