Abstract
Seventy one patients (43 children and 28 adults) of thyroglossal duct remnants (TGDRs) presented at a tertiary care institute from January 2001 to September 2017 were retrospectively analysed. The mean age of presentation was 7.15 years in children and 26.85 years in adults. The male to female ratio was 1.9:1 among children and 1.8:1 among adults. The most common presentation in children was a thyroglossal fistula (53.48%) whereas it was a painless cystic neck swelling (89.29%) in adults. All the children underwent a Sistrunk’s operation whereas 78.57% of the adult patients underwent simple excision of cyst/fistula using the modified incision (Yadav’s incision). Recurrence developed in one child and one adult patient who underwent Sistrunk’s operation and none in the modified incision, these cases were treated with a second stage procedure. In conclusion, compared with adults, more children presented with a discharging thyroglossal fistula. The thyroglossal duct remnants can be managed successfully by simple excision in adults.
Keywords: Thyroglossal duct remnants (TGDRs), Children, Adults, Sistrunk’s operation, Yadav’s incision
Introduction
Thyroglossal duct remnants usually present as a swelling in the neck called thyroglossal duct cyst. The thyroglossal duct cyst is the most common congenital midline swelling of the neck accounting for approximately 70% of the congenital neck anomalies [1, 2]. It is often diagnosed during childhood, about 7% of the lesions occur in the adult population [3]. The thyroglossal duct cyst can present at any site along the pathway of thyroglossal duct. The cyst moves with deglutition as well as protrusion of the tongue. Next common presentation of thyroglossal duct remnants is thyroglossal fistula, which is either due to spontaneous rupture of infected thyroglossal duct cyst, inadequate removal of thyroglossal tract or incision and drainage of infected cyst by quacks and sometimes unsuspecting physicians. Although Sistrunk operation is most commonly used procedure for thyroglossal duct remnants, simple excisions have also been used for the treatment [4]. The purpose of our study was to compare the clinical presentation, surgical treatment and outcome between children and adults. A new incision is proposed.
Materials and Methods
The present study included 71 patients of thyroglossal duct remnants which presented at a tertiary care centre, from January 2001 to September 2017. The records of the patients were retrieved and analysed to know their age, sex, presenting symptoms, family history, previous history of surgery, site and side of the lesion, radiological investigations, thyroid profile, fine needle aspiration cytology (FNAC), preoperative diagnosis, surgical treatment including surgical findings, postoperative complications, final histopathological report and outcome. One of the senior surgeon (SPSY) devised an incision (Yadav’s incision, Fig. 1) where the initial incision was given not at the mid level of the thyroglossal cyst/fistula. The incision was given just above the level of cyst or between the mid-point of the cyst and hyoid bone. The superior and inferior flaps were raised and the cyst/fistula was dissected and pulled up and it could be dissected easily upto the upper end of the thyroglossal tract. The advantage of this incision is that there is no need of additional incision which may sometimes be required when thyroglossal cyst is very low down. Further, the scar is not only in the skin crease but also under the chin shadow, so it is not visible.
Fig. 1.
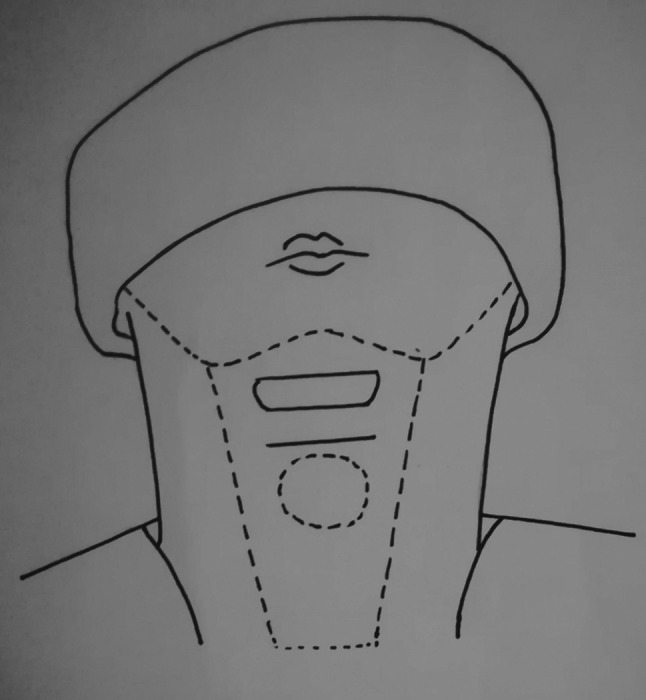
Showing modified incision given between the mid-point of the cyst and hyoid bone
Results
A total of 71 patients (43 children and 28 adults) of thyroglossal duct remnants were studied retrospectively. The youngest patient in our study was 4 days old, while the oldest patient was 45 years old. The mean age of presentation was 7.15 years in children and 26.85 years in adults. The male to female ratio was 1.9:1 among children and 1.8:1 among adults. There was no statistical difference between the two groups (p > 0.05). The most common presentation (53.48%) in children was a thyroglossal fistula with or without discharge from the cervical opening. Among adult patients the most common presentation was a painless cystic swelling in the neck (89.29%) which moved with deglutition as well as protrusion of the tongue. Sistrunk operation was carried out in all the children and 21.43% of adults, the procedure involved radical excision of the tract, along with the body of hyoid bone. In most of the adult patients (78.57%), excision was carried out using the modified incision. The thyroglossal tract was followed upwards which terminated before reaching hyoid bone in all of these patients, thus the hyoid bone was not excised. The termination of tract was observed as loss of firmness and fanning of soft tissues at the upper end of the tract. There was no recurrence where modified incision was used.
In our series, the most common immediate postoperative complications observed was wound infection in both children (4.65%) and adult patients (7.14%). Recurrence developed in one child and one adult patient who underwent Sistrunk’s operation.
Discussion
The thyroid gland originates from the foramen caecum located at the junction of the anterior two-third and posterior one-third of the tongue. During further development the thyroid gland descends to its final destination in the lower neck [5]. Thyroglossal duct which lies along the path of thyroid gland remains patent until the eighth week of development [6]. Failure of the thyroglossal tract to involute may give rise to thyroglossal duct cyst. Because the thyroglossal duct does not communicate with ectoderm during development, thyroglossal fistula the second most common presentation of thyroglossal duct remnants is either the result of spontaneous rupture of thyroglossal cyst, infection or a prior drainage procedure [7].
In our study, the mean age at presentation was 7.15 and 26.85 years in children and adult patients respectively. In a study by Brosseau et al the mean age was 6 years among children and 45 years among adults [6]. There was a male predominance in our study, in both children as well as adults, the male:female ratio was 1.9:1 and 1.8:1 respectively. Thompson et al also reported a male predominance among children (males:females; 1.4:1) while there was a female preponderance in adults (males:females; 1:1.2) [8].
Careful history and physical examination are the most important elements in the diagnosis of thyroglossal duct remnants, however high index of suspicion and clinical awareness is equally important. Dermoid cyst, brachial cleft cyst, ectopic thyroid, lipoma, sebaceous cyst, metastatic thyroid carcinoma and enlarged lymphnodes are the important differential diagnosis of thyroglossal cyst [9]. Brosseau et al reported that the most common presenting features was a cervical mass both in children and adult patients, thyroglossal fistula was diagnosed in one adult patient only [6]. Thompson et al also reported that a neck swelling was the most common presentation, in both children and adult patients. Skin fistula was diagnosed in 9.78% patients; the fistula was twice as common in pediatric patients as adult patients [8]. However, in the present study, the most common presentation in children was a thyroglossal fistula (53.48%) whereas it was a painless cystic neck mass (80%) in adults.
Preoperative evaluation of the patients in our study included ultrasound (USG) neck, CT scan neck and fine-needle aspiration cytology. These investigations help to narrow down the differential diagnosis of thyroglossal duct cyst. Ultrasound neck was used in all of the children. Advantages of USG are that it is easily available, inexpensive, does not require sedation or ionizing radiations [10]. Radiological demonstration of a normal thyroid gland is necessary to exclude ectopic thyroid in patients with thyroglossal duct cyst. Computed tomography of neck was used in all of the adult patients. It gives useful information about the cyst location, size and relations to the surrounding structures. Fine needle aspiration cytology (FNAC) was also used in adult patients only. With concern to the possible injury FNAC is not so popular for diagnosing thyroglossal duct cysts in children [4]. Accordingly, FNAC was not used in any of the children.
The definite treatment for thyroglossal duct remnants is early and complete surgical excision. The unresected thyroglossal cysts have a high incidence of infection. In children, Sistrunk’s operation was performed in all cases, which involved resection of the body of hyoid bone together with the whole length of thyroglossal tract. In adults, cystectomy/fistula excision was performed in 78.57% of cases, in these patients we observed that the thyroglossal tract terminated before reaching the hyoid bone, the termination of tract was observed as loss of firmness and fanning out of the soft tissues of the tract. We could not find any logical explanation of this early termination of tract. This may be due to fibrosis of long standing thyrogossal tract with age as it was observed in adults only.
In our series, postoperative complications observed in children were wound infections (4.65%) and recurrence (2.32%). The most common complication observed in adults was wound infection which occurred in 7.14% cases and recurrence in 3.57%. Lin et al reported that among children recurrence was the most common complication, it developed in 6.25% cases (all patients underwent cyst excision), wound infection developed in 3.12% cases, among adults recurrence developed in 5.8% cases (all cases underwent Sistrunk’s operation), wound hematoma developed in 3.84% cases [4].
Conclusion
In conclusion, children are more likely to present with a discharging fistula than adults. Early surgical excision of thyroglossal duct cyst is the treatment of choice to prevent the development of thyroglossal fistula. Sistrunk’s operation is gold standard in children whereas the thyroglossal duct remnants can be managed by simple excision in adults, if macroscopically thyroglossal tract ends before reaching the hyoid bone.
Compliance with Ethical Standards
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical Approval
This study is a retrospective analysis of operated patients. The investigations (CT scan) and surgery is routinely done in our hospital and worldwide, so no ethical aspect is involved in this study.
Informed Consent
Informed consent was taken at the time of surgery.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Shahin A, Burroughs FH, Kirby JP, Ali SZ. Thyrogossal duct cyst: a cytopathologic study of 26 cases. Diagn Cytopathol. 2005;33:365–369. doi: 10.1002/dc.20346. [DOI] [PubMed] [Google Scholar]
- 2.Mandana J, Yolmo D, Saxena SK, Gopalakrishnan S. True thyroglossal fistula. Laryngoscope. 2009;119:2345–2347. doi: 10.1002/lary.20628. [DOI] [PubMed] [Google Scholar]
- 3.Dedivitis RA, Camargo DL, Peixoto GL, Weissman L, Guimaraes AV. Thyroglossal duct: a review of 55 cases. J Am Coll Surg. 2002;194:274–277. doi: 10.1016/S1072-7515(01)01171-1. [DOI] [PubMed] [Google Scholar]
- 4.Lin ST, Tseng FY, Hsu CJ, Yeh TH, Chen YS. Thyroglossal duct cyst: a comparison between children and adults. Am J Otolaryngol Head Neck Surg. 2008;29:83–87. doi: 10.1016/j.amjoto.2007.02.003. [DOI] [PubMed] [Google Scholar]
- 5.Chou J, Walters A, Hage R, Zurada A, Michalak M, Tubbs RS, et al. Thyroglossal duct cysts: anatomy, embryology and treatment. Surg Radiol Anat. 2013;35:11–25. doi: 10.1007/s00276-013-1115-3. [DOI] [PubMed] [Google Scholar]
- 6.Brousseau VJ, Solares CA, Xu M, Krakovitz P, Koltai PJ. Thyroglossal duct cysts: presentation and management in children versus adults. Int J Pediatr Otorhinolaryngol. 2003;67:1285–1290. doi: 10.1016/j.ijporl.2003.07.006. [DOI] [PubMed] [Google Scholar]
- 7.Lillehai C. Neck cysts and sinuses. In: Coran AG, Caldamone N, Adzick NS, Krummel TM, Laberge JM, Shamberger R, editors. Paediatric surgery. 7. Amsterdam: Elsevier; 2012. pp. 753–761. [Google Scholar]
- 8.Thompson LDR, Herrera HB, Lau SK. A clinicopathologic series of 685 thyroglossal duct remnant cysts. Head Neck Pathol. 2016;10:465–474. doi: 10.1007/s12105-016-0724-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Moorthy SN, Arcot R. Thyroglossal duct cyst—more than just an embryological remnant. Indian J Surg. 2011;73:28–31. doi: 10.1007/s12262-010-0171-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ahuja AT, King AD, Metriweli C. Sonographic evaluation of thyroglossal duct cysts in children. Clin Radiol. 2000;55:770–774. doi: 10.1053/crad.2000.0514. [DOI] [PubMed] [Google Scholar]


