Abstract
Purpose
CSOM is a common disease in lower socio-economic set-ups. Its incidence has decreased over time due to improved hygiene status increased use of antibiotics. It can be associated with cholesteatoma or granulation tissue as far as unsafe ears are considered. Cholesteatoma is defined as a well demarcated noncancerous cystic lesion derived from an abnormal growth of keratinising squamous epithelium in the temporal bone, commonly characterised as skin in the wrong place. Granulations are defined as the inflammatory response of middle ear mucosa to toxic insults. Overtime the incidence of granulations has increased. This study aims to observe the incidence trends of cholesteatoma in comparison to granulation tissue as intraoperative finding in CSOM patients and the association of these two with the age of the patient and associated complications if present.
Materials and Methods
All the patients admitted to E.N.T ward of M.D.M. Hospital, Jodhpur, Rajasthan, India undergoing mastoid exploration surgery between the time period of 1 year from September 2017 to August 2018 were observed and their clinical findings along with patients data including age and sex were recorded and studied in regard with incidence of cholesteatoma, granulation tissue or both simultaneously along with associated complications.
Results
Majority of the patients who required mastoid exploration surgery had the presence of granulation tissue as intraoperative finding (55.07%). The incidence of cholesteatoma and both cholesteatoma and granulations together was (21.73%) and (23.18%) respectively. Complication percentage was highest with that of cholesteatoma patients (44.45%). Most of the patients presented in the 3rd–4th decade of their lives (63.77%) and the incidence was low amongst the children (30.43%) and the elderly (5.8%). The complication rate was higher in children (55.56%).
Conclusion
Granulation tissue showed an increased incidence trend as compared with cholesteatoma; although complication rate was higher in the latter. Incidence as a function of age was maximum in the middle ages but the complication rate was more amongst the children.
Keywords: Cholesteatoma, Granulation tissue, Chronic otitis media
Introduction
Being an ENT surgeon, one of the most common diseases we all have to deal with is chronic otitis media. It is defined as a permanent abnormality of the pars tensa or flaccida, most likely a result of earlier acute otitis media, negative middle ear pressure or otitis media with effusion. It is mostly a disease of lower socio-economic strata, more common in people living in rural areas with poor hygiene status [1].
The disease as such is divided into two counterparts, the mucosal and the squamosal types. The mucosal type being less aggressive these days due to excessive use of antibiotics; but the squamosal type is of more destructive variety, posing a problem to be dealt with at first hand as it can lead to what is called an unsafe ear.
Histopathologically, COM can be characterised by middle ear pathology associated with the disease that is either a cholesteatoma or granulation tissue or both together [2].
Cholesteatoma is defined as a well demarcated noncancerous cystic lesion derived from an abnormal growth of keratinising squamous epithelium in the temporal bone [3–5] which is commonly characterised as skin in the wrong place [6, 7]. It is locally invasive and capable of causing destruction of structures in the middle ear cleft. While granulation tissue is an inflammatory process occurring due to reactionary healing which results in fibroblast recruitment, neovascularisation and occasionally polyp formation [8].
Cholesteatoma and granulation tissue are both destructive pathologies and the incidence of both varies according to age and sex as does their association with complications.
The annual incidence of cholesteatoma is estimated at 3 per 1,00,000 in children and 9.2 per 1,00,000 in adults based on a study of Finnish and Danish individuals [9].
Along with incidence, the nature of spread and aggressiveness of cholesteatoma and granulations also differ between children and adults with pediatric cholesteatoma being more frequently infectious, more aggressive, more proliferative and associated with a less favourable prognosis [5, 10].
Bone erosion is present in the majority of mature cholesteatomas. Initially bone erosion is confined to the ossicular chain and scutum. As the cholesteatoma expands, erosion of otic capsule, fallopian canal and tegmen can occur.
Cholesteatoma may further be classified as congenital and acquired. Congenital which is specific to childhood and arises from epithelial tissue rests within or adjacent to temporal bone and acquired which affects children as well as adults [11]. Acquired cholesteatomas originate in the middle ear from the stratified squamous epithelium of the tympanic membrane or metaplasia of middle ear mucosa. In the pediatric population, cholesteatoma accounts for 10% of COM cases [12]. The incidence of acquired cholesteatoma has declined in the recent decades [13, 14] due to widespread use of ventilation tubes [15].
Cholesteatoma can remain undetected for years remaining non-aggressive and undiscovered until they get dangerously large and threaten to spread intracranially and intratemporally leading to a number of intra and extra cranial complications which include labyrinthine fistula, labyrinthitis, facial nerve palsy, brain abscess, hearing loss, meningitis, lateral sinus thrombosis [16].
An observation was made by us recently towards a decreasing incidence of cholesteatoma. The consistency of cholesteatoma matrix is quite variable, ranging from a relatively thick and well defined capsule to loose squamous debris without any visible capsule. To minimise the risk of leaving residual disease, the matrix should be resected as completely as possible, elevating it as an intact sheet if possible. The sac is usually not uniformly adherent to the underlying mucosa or bone; rather, it is often in loose contact and fixed only intermittently by mucosal adhesions. Thus cholesteastoma removal seems to be surgically less challenging than operating on ears with extensive granulation extension into various recesses and crevices of middle ear cleft spaces. Thus this study was undertaken to observe the incidence trends of cholesteatoma and granulation tissue and their association with complications. Also the age association of both the pathologies were evaluated and studied (Fig. 1).
Fig. 1.
Clinical photographs showing presence of granulation tissue in the mastoid cavity
Materials and Methods
All the patients admitted to E.N.T ward of M.D.M. Hospital, Jodhpur, Rajasthan, India undergoing mastoid exploration surgery between the time period of 1 year from September 2017 to August 2018 were observed and their clinical findings along with patients data including age and sex were recorded and studied retrospectively-prospectively in regard with incidence of cholesteatoma, granulation tissue or both simultaneously along with associated complications.
Study design: It was a hospital based descriptive type of observational study.
Study period: September 2017 to August 2018 (1 year).
Study area: Department of Otorhinolaryngology and Head and Neck Surgery, Dr.S.N. Medical College and M.D.M. Hospital, Jodhpur, Rajasthan, India.
Inclusion criteria:
All patients diagnosed to suffer from CSOM (mucosal or squamosal who required and underwent mastoid exploration surgery).
Those who gave written and informed consent.
Exclusion criteria:
Patients unfit for general anaesthesia.
Patients previously operated for the same complain (revision surgeries).
Methodology
The study was carried out by means of information obtained through patients who underwent Mastoidectomy surgery in the service of Otorhinolaryngology department of Dr. S.N. Medical College, Jodhpur. The patients were analysed by age (children taken to be those less than 18 years of age in this study), intraoperative disease pathology and the complications associated with the primary disease. The patients were selected for mastoid surgery after thorough evaluation of the disease process and general and E.N.T examination.
ENT examination: A thorough history was taken to determine the onset, duration and cause of the discharge and/or hearing loss or any other complain. A detailed otological examination was done including otoscopy and microscopic examination. Along with this, nose and throat examination was also done in detail. A diagnosis of CSOM and its division into cholesteatoma and granulation tissue groups was made on the basis of history, otoscopic finding and post-operative histopathology reports obtained from middle ear tissue taken during surgery.
Imaging: A HRCT-temporal bone was performed in all cases pre-operatively.
Audiology: A pure tone audiogram was obtained for all cases before surgery.
Ophthalmologic references were done for fundus examination in cases with suspected intracranial complication for increased intracranial pressure and neurosurgical help was taken whenever required both pre and intra-operatively in cases of intracranial complication.
Operative procedure: All the patients were operated by the classical post aural approach to mastoidectomy by Wilde’s incision. The procedures were started as Intact Canal Wall and converted to Canal Wall Down whenever deemed necessary for disease clearance.
The surgery was performed under complete sterile conditions and with all aseptic precautions under General Anaesthesia.
Post-operative and follow up: The patients were kept under observation for 2–4 days and dressings done on day 2nd and 4th, follow up was made on regular intervals after discharge for the HPE report and ear status post surgery (Fig. 2).
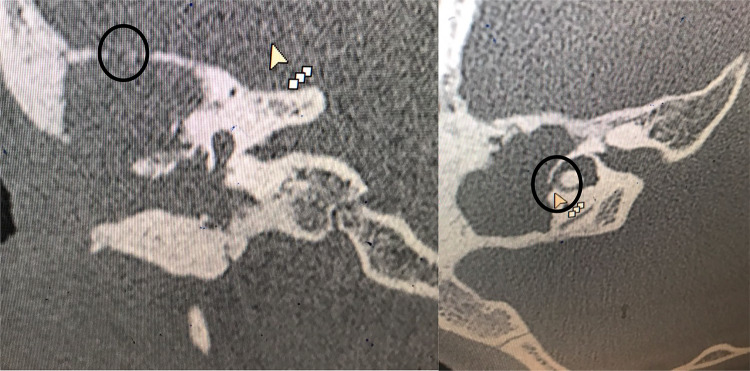
Fig. 2.
Complications like tegmen erosion and lateral semi-circular canal fistula as visualised on HRCT scan of temporal bone (encircled)
Results
Total number of cases in our study was 69. Majority of these patients who underwent mastoid exploration surgery had the presence of granulation tissue as intraoperative finding (55.07%). The incidence of cholesteatoma and both cholesteatoma and granulations together was (21.73%) and (23.18%) respectively. Complication percentage was highest with that of cholesteatoma patients (44.45%). Most of the patients presented in the 3rd–4th decade of their lives (63.77%) and the incidence was low amongst the children (30.43%) and the elderly (5.8%). The complication rate was higher in children (55.56%). These findings can be better understood by the following figures (Tables 1, 2, 3; Fig. 3).
Table 1.
Association of age with intra-operatively observed COM pathology and their individual overall incidences
| Age group | Pathology | |||
|---|---|---|---|---|
| Cholesteatoma | Granulations | Cholesteatoma with granulation | Total | |
| 0–18 years | 6 | 7 | 8 | 21 |
| 18–40 years | 9 | 27 | 8 | 44 |
| > 40 years | – | 4 | – | 4 |
| Total | 15 | 38 | 16 | 69 |
Table 2.
Complications association with age
| Age group | Complications | Percentage (%) |
|---|---|---|
| 0–18 years |
Dead labyrinth Labyrinthine fistula Cerebellar abscess Mastoid abscess Superior SCC fistula |
23.8% (5 out of 21 cases) |
| 18–40 years |
Facial nerve palsy-3 Lateral SCC fistula |
9% (4 out of 44 cases) |
| > 40 years | – | – |
Table 3.
Complication association with type of disease pathology found intra-operatively
| COM pathology | Complication associated | Percentage (%) |
|---|---|---|
| Cholesteatoma |
Dead labyrinth Labyrinthine fistula Facial nerve palsy Lateral SCC fistula |
26.66% (4 out of 15 cases) |
| Granulations |
Cerebellar abscess Facial nerve palsy |
5.26% (2 out of 38 cases) |
| Cholesteatoma with granulations |
Mastoid abscess Superior SCC fistula Facial nerve palsy |
18.75% (3 out of 16 cases) |
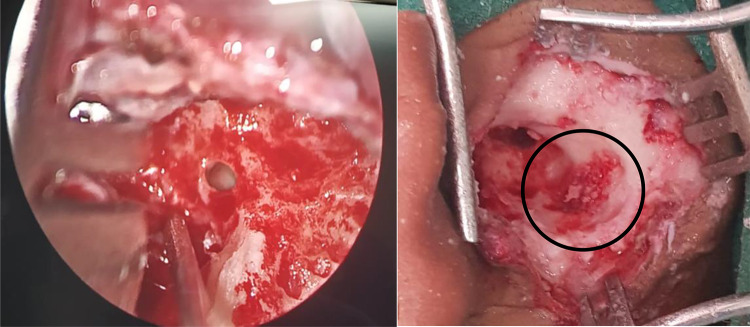
Fig. 3.
Clinical photographs showing absence of stapes footplate and other ossicles due to erosion and granulations adherent to the wall of sigmoid sinus (encircled)
Discussion
In our study we found the incidence of granulations to be higher than and almost more than twice of that of both cholesteatoma and granulations and cholesteatoma combined. This is in contrast with a study done by Gupta et al. [17] who found that incidence of cholesteatoma was about thrice of that both granulations and both cholesteatoma and granulations combined. This was a study done in 1998 and might indicate a changing incidence trend. Increase in granulation tissue might also be due to increased use of antibiotics in the recent era—both systemic and topical which lead to a healing response.
Also it was found that cholesteatoma was about 1.5 times more common in adults than in children (taken as less than 18 years in this study) up to 40 years of age and no incidence was found in patients above 40 years. This can also be because patients above 40 years might not prefer to get a surgery done for an ear disease until some serious complication warrants.
Alongside this granulation tissue occurrence in COM was also most common in the 3rd and 4th decades of life but as was the incidence of COM. This incidence association with age is similar to previous studies done in this regard by Baig et al. [18].
Amongst the complications recorded, the incidence of both intra and extracranial complications combined was higher amongst the cholesteatoma group of patients and if taken as a ratio of number of patients then association of complications with cholesteatoma was about five times that of granulation tissue. Also was found that the incidence of complications associated with COM was about 1.5 times more in children than adults but the overall incidence was low as adult age group included more number of cases.
Many reasons can be cited for increased complication rate in children. Cholesteatoma in pediatric patients contains a greater proportion of cellular than fibrotic perimatrix than that found in adult cholesteatoma which might indicate that pediatric cholesteatoma in more invasive and less reparative [19]. Also, the temporal bone in children is more pneumatised and extensive pneumatisation provides adequate space allowing the disease to spread, exacerbating the aggressive behaviour of pediatric cholesteatoma [15, 20]. This finding of increased complication rate in children is similar to as found out by Kuo et al. [21].
Conclusion
Thus even though COM has been studied and its various managements considered exhaustively, the pattern of disease progression and presentation continues to change.
An ear with cholesteatoma which was the expected finding in COM with mastoiditis cases has decreased these days and more and more intraoperative incidence of granulations is seen. Overall the complications associated with granulations are less but increasing incidence should warrant a surgeon to be more careful as granulation in difficult areas pose a more challenging situations to clear and get a dry ear as it is not as in the case of cholesteatoma in which the disease can be removed en bloc with the cholesteatoma sac.
Lipopolysaccahrides, the primary component of bacterial cell walls, have been found in higher concentrations in patients with cholesteatoma and active bone destruction [22]. Destruction of these by frequent use of topical and systemic antibiotics might play a role in decreasing cholesteatoma incidence and increasing granulations.
At the last, a higher complication rate in children and that too with cholesteatoma should alert all of us as any delay in the diagnosis and/or treatment of cholesteatoma can have profound effects on language development, learning performance, and academic comprehension as a direct result of hearing loss [20]. Early intervention increases the chances of preserving or reclaiming the hearing of the patients and thus improve the quality of life post-surgery.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not for profit sectors.
Compliance with Ethical Standards
Conflict of interest
Bharti Solanki and Shivam Sharma declare that they have no conflict of interest.
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed Consent
Informed consent was obtained from all individual participants included in the study.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Bharti Solanki, Email: drbhartisolanki@gmail.com.
Shivam Sharma, Email: shivam92@hotmail.com.
References
- 1.Chaudhri MA, Alaudin M. Comparative study between tubotympanic and atticoantral type of chronic suppurative otitis media. Bangladesh Med Res Counc Bull. 2002;28(1):36–44. [PubMed] [Google Scholar]
- 2.Daly K, Hunter L, Giebank G. Chronic otitis media with effusion. Paediatr Rev. 1999;20:85–94. doi: 10.1542/pir.20-3-85. [DOI] [PubMed] [Google Scholar]
- 3.Isaacson G. Diagnosis of pediatric cholesteatoma. Pediatrics. 2007;120(3):603–608. doi: 10.1542/peds.2007-0120. [DOI] [PubMed] [Google Scholar]
- 4.Semaan MT, Megerian CA. The pathophysiology of cholesteatoma. Otolaryngol Clin N Am. 2006;39(6):1143–1159. doi: 10.1016/j.otc.2006.08.003. [DOI] [PubMed] [Google Scholar]
- 5.Dornelles C, da Costa SS, Meurer L, Schweiger C. Some considerations about acquired adult and pediatric cholesteatomas. Rev Bras Otorrinolaringol. 2005;71(4):536–546. doi: 10.1590/S0034-72992005000400023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Robinson JM. Cholesteatoma: skin in the wrong place. J R Soc Med. 1997;90(2):93–96. doi: 10.1177/014107689709000212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Gray JD. The chronic ear. The treatment of cholesteatoma in children. Proc R Soc Med. 1964;57:769–771. doi: 10.1177/003591576405700903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Roland PS. The formation and management of middle ear granulation tissue in chronic ear disease. Ear Nose Throat J. 2004;83(Suppl 1):5–8. doi: 10.1177/014556130408301s02. [DOI] [PubMed] [Google Scholar]
- 9.Kemppainen HO, Puhakka JH, Laippala PJ, Sipila MM, Manninen MP, Karma PH. Epidemiology and aetiology of middle ear cholesteatoma. Acta Otolarygol. 1999;119:568–572. doi: 10.1080/00016489950180801. [DOI] [PubMed] [Google Scholar]
- 10.Bujia J, Holly A, Antoli-Candela F, Tapia MG, Kastenbauer E. Immunobiological peculiarities of cholesteatoma in children: quantification of epithelial proliferation by MIB 1. Laryngoscope. 1996;106(7):865–868. doi: 10.1097/00005537-199607000-00015. [DOI] [PubMed] [Google Scholar]
- 11.Nevoux J, Lenoir M, Roger G, Denoyelle F, Le Pointe HD, Garabedian E-N. Childhood cholesteatoma. Eur Ann Otorhinolaryngol Head Neck Dis. 2010;127(4):143–150. doi: 10.1016/j.anorl.2010.07.001. [DOI] [PubMed] [Google Scholar]
- 12.Triglia JM, Gillot JC, Giovanni A, Cannoni M. Cholesteatoma of the middle ear in children. Apropos of 80 cases and review of the literature. Ann d’Oto-Laryngol Chir Cerv-Fac. 1993;110(8):437–443. [PubMed] [Google Scholar]
- 13.Bennett M, Warren F, Jackson GC, Kaylie D. Congenital cholesteatoma: theories, facts, and 53 patients. Otolaryngol Clin N Am. 2006;39(6):1081–1094. doi: 10.1016/j.otc.2006.08.001. [DOI] [PubMed] [Google Scholar]
- 14.Shohet JA, de Jong AL. The management of pediatric cholesteatoma. Otolaryngol Clin N Am. 2002;35(4):841–851. doi: 10.1016/S0030-6665(02)00052-X. [DOI] [PubMed] [Google Scholar]
- 15.Dornhoffer JL, Friedman AB, Gluth MB. Management of acquired cholesteatoma in the pediatric population. Curr Opin Otolarynol Head Neck Surg. 2013;21(5):440–445. doi: 10.1097/MOO.0b013e32836464bd. [DOI] [PubMed] [Google Scholar]
- 16.Singh B, Maharaj TJ. Radical mastoidectomy: its place in otitic intracranial complications. J Laryngol Otol. 1993;107(12):1113–1118. doi: 10.1017/S0022215100125435. [DOI] [PubMed] [Google Scholar]
- 17.Gupta A, Agarwal SR. A study of prevalence of cholesteatoma in complications of suppurative otitis media. IJO HNS. 1998;50(2):140–146. doi: 10.1007/BF02991677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Baig MM, Ajmal M, Saeed I, Fatima S. Prevalence of cholesteatoma and its complications in patients of chronic suppurative otitis media. J Rawalpindi Med Coll. 2011;15(1):16–17. [Google Scholar]
- 19.Bassiouny M, Badour N, Omran A, Osama H. Histopathological and immunohistochemical characterstics of acquired cholesteatoma in children and adults. Egypt J Ear Nose Throat Allied Sci. 2012;13(1):7–12. doi: 10.1016/j.ejenta.2012.02.007. [DOI] [Google Scholar]
- 20.Hildmann H, Sudhoff H. Cholesteatoma in children. Int J Pediatr Otorhinolaryngol. 1999;49(supplement 1):S81–S86. doi: 10.1016/S0165-5876(99)00138-X. [DOI] [PubMed] [Google Scholar]
- 21.Kuo CL, An-S Shiao, Yung M, Sakagami M, Sudhoff H, Wang CH, Hsu CH, Lien CF. Updates and knowledge gaps in cholesteatoma research. Biomed Res Int. 2015;2015:854024. doi: 10.1155/2015/854024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Jung J, Pashia M, Nishimoto S, Faddis Chole R. A possible role for nitric oxide in osteoclastogenesis associated with choletseatoma. Otol Neurotol. 2004;25:661–668. doi: 10.1097/00129492-200409000-00003. [DOI] [PubMed] [Google Scholar]