Abstract
Introduction
Synovial chondromatosis is a rare metaplastic disorder of the synovial membrane. Primary synovial chondromatosis of the shoulder joint is a rare localization and extra-articular localization around the shoulder is much less common.
Case Report
We report a rare case of a 13-year-old boy with primary synovial chondromatosis of the subscapular bursa. Computed tomography and magnetic resonance imaging showed that multiple cartilaginous loose bodies were found in the subscapular bursa and the glenohumeral joint. Arthroscopic removal of loose bodies and synovectomy of the subscapular bursa was performed through sublabral foramen.
Conclusion
Pre-operative investigation for the precise location of the lesions was important for the planning the operative procedure. Arthroscopic removal of loose bodies and synovectomy was useful treatment options for synovial chondromatosis of the subscapular bursa.
Keywords: Shoulder, synovial chondromatosis, subscapular bursa, arthroscopy
Learning Point of the Article:
Primary synovial chondromatosis of the subscapular bursa is a rare localization and arthroscopic treatment is an effective treatment option with satisfactory clinical outcome.
Introduction
Synovial chondromatosis is a rare metaplastic disorder of the synovial membrane. It is characterized by multiple cartilaginous loose bodies arising from the synovial membrane of the joint, synovial sheath, or bursae around the joint [1]. The disease most commonly affects the knee joint, followed by the hip, elbow, wrist, ankle, and shoulder joints. Extra-articular localization such as a bursa or tendon sheath is much less common. Cases of synovial chondromatosis of the periarticular bursa around the shoulder have rarely been reported in literature [2, 3, 4]. An extremely rare case of primary synovial chondromatosis of the subscapular bursa communicating with the glenohumeral joint through a sublabral foramen, which was successfully treated by arthroscopic surgery, is reported.
Case Report
A 13-year-old right-handdominant boy presented with pain and locking while moving the right shoulder during basketball activity and recurrent swelling around his right shoulder. There was no history of trauma, major illness, or surgery. His pain did not improve with conservative treatment, which included nonsteroidal anti-inflammatory drugs and physical therapy. On physical examination, he had a swollen right shoulder, but there were no signs of erythema, warmth, or muscle atrophy in his right shoulder. Active forward elevation of the right shoulder was 160°, external rotation was 70°, and internal rotation was at level T8. Plain radiographs of the right shoulder showed no abnormal findings (Fig. 1), but computed tomography (CT) and magnetic resonance imaging (MRI) showed several loose bodies in the axillary pouch and a large calcified mass lesion in the subscapular bursa (Fig. 2 and 3). Arthroscopy under general anesthesia in the beach chair position was performed through standard posterior and anterior portals. Arthroscopic examination showed several loose bodies in the glenohumeral joint (Fig. 4a). However, intrasynovial chondroid nodules were not seen in the glenohumeral joint. A sublabral foramen was found at the anterosuperior portion of the glenoid that communicated with the subscapular bursa (Fig. 4b). Multiple large calcified mass lesions and intrasynovial chondroid nodules were seen in the subscapular bursa, suggesting Milgram Stage 2 (transitional phase) (Fig. 4c). Loose bodies both in the glenohumeral joint and in the subscapular bursa were removed through a standard anterior portal, and proliferative thickened synovium of the subscapular bursa was also resected using a motorized shaver through the sublabral foramen. The histological examination of the loose bodies confirmed cartilaginous synovial metaplasia consistent with primary synovial chondromatosis (Fig. 5). The range of motion exercise was initiated from the day after surgery. Three weeks after the operation, he was symptom free with full range of motion and was able to return to sports. At follow-up after 5 years, he remained asymptomatic, and there was no clinical and radiographic evidence of recurrence.
Figure 1.
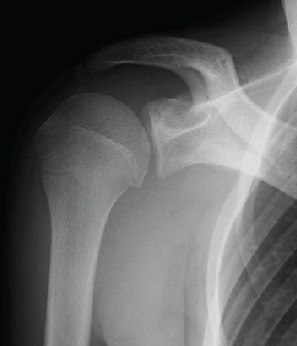
Anteroposterior radiograph shows no calcified lesion in the right shoulder.
Figure 2.
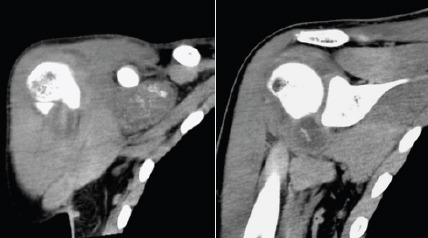
Computed tomography scan of the right shoulder shows a large calcified mass lesion in the subscapular bursa (a) and some free fragments in the glenohumeral joint (b).
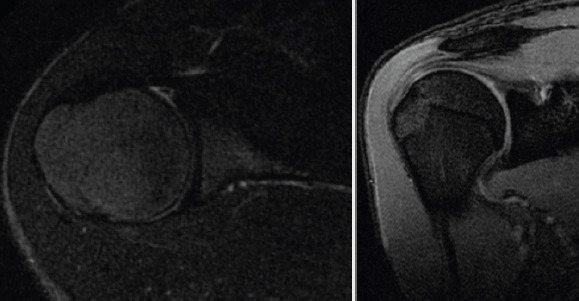
Figure 3.
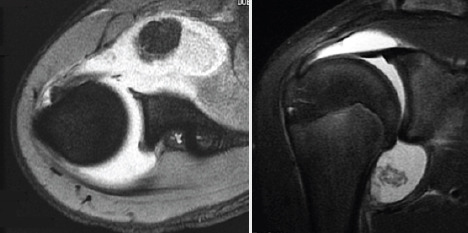
Fat-suppressed T2-weighted axial (a) and coronal oblique (b) magnetic resonance images of the right shoulder show a large mass lesion in the subscapular bursa and loose bodies in the axillary pouch.
Figure 4.

Arthroscopic view from the posterior portal shows free bodies in the axillary pouch (b), the sublabral foramen (arrows) at the anterosuperior portion of the glenoid (a), and multiplelarge calcified mass lesions and intrasynovial chondroid nodules in the subscapular bursa (c).
Figure 5.
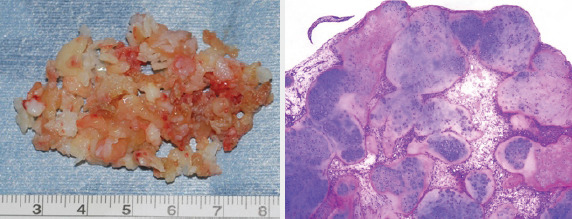
Macroscopic appearance of numerous cartilaginous loose bodies removed from the subscapular bursa (a).Photomicrograph of loose bodies shows multiple lobulated cartilaginous nodules within the synovial tissue (b).
Discussion
Synovial chondromatosis has been divided into primary and secondary forms [5]. Primary synovial chondromatosis is a benign metaplastic disorder of the synovial membrane with multiple cartilaginous loose bodies. In contrast, secondary synovial chondromatosis is caused by degenerative joint disease such as trauma, inflammatory and non-inflammatory arthropathies, avascular necrosis, and osteochondritis dissecans, which generally occurs at an older age than the primary form. The present case was thought to be a primary synovial chondromatosis due to the patient’s age and the absence of degenerative joint disease.
Primary synovial chondromatosis of the shoulder joint is a rare localization, with a reported incidence of approximately 5% [6]. Extra-articular localization of primary synovial chondromatosis is much less common. Extra-articular, intra-articular, and combined types at the shoulder joint have been documented in literature [7, 8, 9,10]. There have been only three reports of primary synovial chondromatosis of the glenohumeral joint including the subscapular recess and the biceps tendon sheath [8, 9, 10]. These reports demonstrated intrasynovial proliferation of cartilaginous nodules and the multiple loose bodies in the glenohumeral joint. Therefore, the origin of the loose bodies in the previous reports might be the glenohumeral joint. In the present case, both the subscapular bursa and glenohumeral joint were involved, which indicate the combined type of primary synovial chondromatosis. Arthroscopic and histological findings indicated that the origin of the loose bodies was primary synovial chondromatosis of the subscapular bursa.
A sublabral foramen is a normal anatomic variant of the anterosuperior glenoid labrum without any clinical importance. The reported prevalence of sublabral foramen is ranging from 7.7% to 13.4% in shoulder arthroscopies [11, 12]. The sublabralforamen is clinically asymptomatic and should be treated non-operatively. Recent reports have shown that anatomic variants of the anterosuperior labrum are associated with the development of superior labrum anterior-posterior lesions by altering the intra-articular biomechanics [11, 12]. A case in which the sublabral foramen was arthroscopically repaired after the removal of loose bodies in a sublabral recess to prevent reaccumulation of additional loose bodies has been reported [13]. However, it is unclear whether the labral variations should be repaired. In the present case, the sublabral foramen was diagnosed as normal anatomic variant and was not repaired to prevent increased pain and restricted range of motion. The patient achieved early functional recovery and a satisfactory clinical outcome without recurrence.
Clinical diagnosis is based on history, physical examination, radiographic examination, and histological examination. The symptoms of primary synovial chondromatosis are generally non-specific, including pain, swelling, locking, and limited range of motion of the affected joint. In the present study, the pain and locked joint movement originated from the loose bodies in the glenohumeral joint, which had migrated from the subscapular bursa through the sublabral foramen. Recurrent hemarthrosis, as seen in the present case, was an atypical manifestation for primary synovial chondromatosis and may be caused by irritation or mechanical stress affecting the subscapular bursa including large calcified mass lesions during sports activity. Plain radiography is not always helpful for the diagnosis of primary synovial chondromatosis, as shown in the present case. The previous report showed that calcifications were not present in 5–55% of primary synovial chondromatosis cases [14].In the present case, CT or MRI is useful for detecting uncalcified lesions and evaluating the precise localization of extra-articular forms of primary synovial chondromatosis.
The treatment decision is made according to the patient’s age, symptoms, and the disease stage. Traditional treatment for primary synovial chondromatosis consists of the surgical removal of the loose bodies and synovectomy in an open manner or arthroscopically. Recently, the arthroscopic surgery has been an effective treatment method with many advantages over open surgery, although some cases of recurrence have been reported with both techniques. The advantages of this procedure include better visualization during surgery, decreased post-operative pain, and earlier functional recovery than with open treatment [6, 7, 8, 10, 13, 15]. A disadvantage of arthroscopy is the possibility of limited synovectomy and residual loose bodies. In the present case, the patient was successfully treated by arthroscopic removal of loose bodies and synovectomy because the subscapular bursa communicated with the glenohumeral joint through a sublabral foramen. The patient had a satisfactory clinical outcome and the range of motion of his shoulder was symmetric to that of the uninvolved side. No evidence of recurrence was found in 5-year follow-up MRI (Fig. 6).
Figure 6.
Fat-suppressed T2-weighted axial (a) and coronal oblique (b) magnetic resonance images of the right shoulder at 5-year follow-up show no loose bodies in the subscapular bursa and the axillary pouch.
Conclusion
We described a rare case of primary synovial chondromatosis of the subscapular bursa communicating with the glenohumeral joint through a sublabral foramen. Pre-operative investigation for the precise location of the lesions by CT or MRI was important for planning the operative procedure. Arthroscopic treatment, which provided good visualization and early functional recovery, was a useful treatment option for primary synovial chondromatosis of the subscapular bursa.
Clinical Message.
Although primary synovial chondromatosis of the subscapular bursa is a rare localization, careful analysis of the lesion including intrasynovial chondroid nodules and loose bodies is important to prevent recurrence of disease. Arthroscopic treatment is an effective treatment option with early functional recovery and satisfactory clinical outcome.
Biography




Footnotes
Conflict of Interest: Nil
Source of Support: Nil
Consent: The authors confirm that Informed consent of the patient is taken for publication of this case report
References
- 1.Milgram JW. Synovial osteochondromatosis:A histopathological study of thirty cases. J Bone Joint Surg Am. 1977;59:792–801. [PubMed] [Google Scholar]
- 2.Neumann JA, Garrigues GE. Synovial chondromatosis of the subacromial bursa causing a bursal-sided rotator cuff tear. Case Rep Orthop2015. 2015:259483. doi: 10.1155/2015/259483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Dwidmuthe SC, Nemade AS, Agrawal S, Pathak A. Rare case of extra-articular synovial chondromatosis of biceps tendon sheath in 8 years male child. J Orthop Case Rep. 2014;4:33–6. doi: 10.13107/jocr.2250-0685.221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Xu C, Yang X, Zhao J. Arthroscopic treatment for synovial chondromatosis of the subacromial bursa associated with partial rotator cuff tear. Knee Surg Sports Traumatol Arthrosc. 2015;23:600–2. doi: 10.1007/s00167-014-3308-7. [DOI] [PubMed] [Google Scholar]
- 5.Ji JH, Shafi M, Jeong DS. Secondary synovial chondromatosis of the shoulder. Knee Surg Sports Traumatol Arthrosc. 2015;23:2624–7. doi: 10.1007/s00167-014-3024-3. [DOI] [PubMed] [Google Scholar]
- 6.Raval P, Vijayan A, Jariwala A. Arthroscopic retrieval of over 100 loose bodies in shoulder synovial chondromatosis:A case report and review of literature. Orthop Surg. 2016;8:511–5. doi: 10.1111/os.12294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.ElRassi G, Matta J, Hijjawi A, Khair OA, Fahs S. Extra-articular synovial chondromatosis eroding and penetrating the acromion. Arthrosc Tech. 2015;4:e443–8. doi: 10.1016/j.eats.2015.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Tokis AV, Andrikoula SI, Chouliaras VT, Vasiliadis HS, Georgoulis AD. Diagnosis and arthroscopic treatment of primary synovial chondromatosis of the shoulder. Arthroscopy. 2007;23:1023–e1-5. doi: 10.1016/j.arthro.2006.07.009. [DOI] [PubMed] [Google Scholar]
- 9.Chalasani P, Koduru S, Mikkineni K. A rare case of multiple rice bodies in glenohumeral joint, subscapular recess and along long head of biceps. J Orthop Case Rep. 2016;6:53–5. doi: 10.13107/jocr.2250-0685.504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Fowble VA, Levy HJ. Arthroscopic treatment for synovial chondromatosis of the shoulder. Arthroscopy. 2003;19:E2. doi: 10.1053/jars.2003.50019. [DOI] [PubMed] [Google Scholar]
- 11.Kanatli U, Ozturk BY, Bolukbasi S. Anatomical variations of the anterosuperior labrum:Prevalence and association with type II superior labrum anterior-posterior (SLAP) lesions. J Shoulder Elbow Surg. 2010;19:1199–203. doi: 10.1016/j.jse.2010.07.016. [DOI] [PubMed] [Google Scholar]
- 12.Rao AG, Kim TK, Chronopoulos E, McFarland EG. Anatomical variants in the anterosuperior aspect of the glenoid labrum:A statistical analysis of seventy-three cases. J Bone Joint Surg Am. 2003;85:653–9. doi: 10.2106/00004623-200304000-00011. [DOI] [PubMed] [Google Scholar]
- 13.Kaplan K, Sahajpal DT, Jazrawi L. Loose bodies in a sublabral recess:Diagnosis and treatment. Bull Hosp Jt Dis. 2006;63:161–5. [PubMed] [Google Scholar]
- 14.Kirchhoff C, Buhmann S, Braunstein V, Weiler V, Mutschler W, Biberthaler P. Synovial chondromatosis of the long biceps tendon sheath in a child:A case report and review of the literature. J Shoulder Elbow Surg. 2008;17:e6–e10. doi: 10.1016/j.jse.2007.06.012. [DOI] [PubMed] [Google Scholar]
- 15.Duymus TM, Yucel B, Mutlu S, Tuna S, Mutlu H, Komur B. Arthroscopic treatment of synovial chondromatosis of the shoulder:A case report. Ann Med Surg (Lond) 2015;4:179–82. doi: 10.1016/j.amsu.2015.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]


