Introduction
This report describes a case of a bronchopleural fistula occurring after concurrent chemoradiation therapy. This rare and major complication has not been previously described in the literature. Surgical options are limited, and even after surgery the prognosis is poor. The aim of this case report is to increase awareness of this rare, life-threatening complication and to discuss the options for defect closure.
Case Report
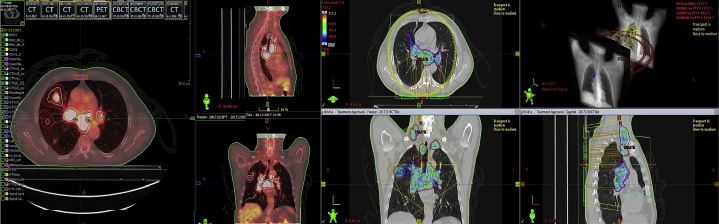
A 63-year old man with a history of smoking, hypertension, and vascular disease received a diagnosis of a clinically T3 (satellites in same lobe), N3 (1R, 1L, 2R, 2L, 4R, 4L, 7, 10R), M0, poorly differentiated adenocarcinoma in the right upper lobe, stadium IIIB, in December 2017. After a multidisciplinary team meeting, it was decided to treat the patient according to international guidelines with concurrent chemoradiation, with curative intent. He received 3 courses carboplatin/etoposide chemotherapy and 60 Gy radiation therapy in 30 fractions with a 4-dimensional volumetric-modulated arc therapy technique. The target volume for irradiation consisted of the primary tumor and all involved lymph node stations, without elective nodal irradiation (Fig 1). The mean lung dose was 19.3 Gy and the mean heart dose 10.8 Gy, in line with EORTC guidelines.1 The maximal dose to the mediastinal structures was 69.2 Gy in 30 fractions.
Figure 1.
Overview of radiation treatment volume.
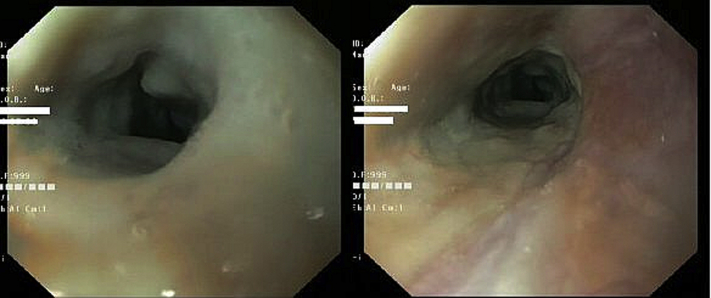
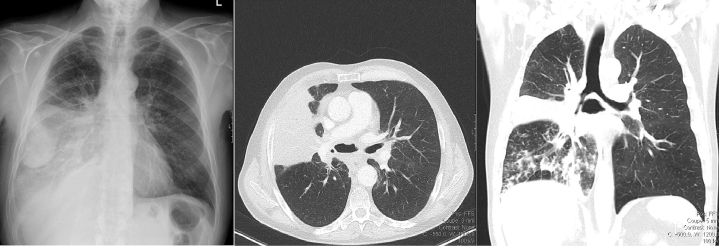
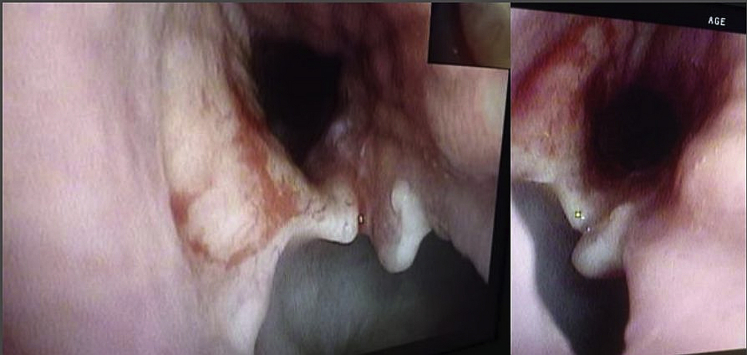
After chemoradiation, the patient developed dysphagia grade 3 including weight loss. Gastroscopy was performed because of persistent complaints despite adequate medication and showed a radiation esophagitis with stenosis (Fig 2). A nasogastric tube was placed for tube feeding. In April 2018, the patient presented at the emergency room with signs of sepsis, acute dyspnea, right sided thoracic pain with reduced right sided airflow, tachycardia (155 bpm), hypotension (92/58 mm Hg), saturation of 85%, C-reactive protein of 348 mg/L, and leukocytosis of 24.8 × 109/L. Conventional chest x-ray showed atelectasis and right sided pleural effusion (Fig 3). Additionally, computed tomography (CT) scan of the chest showed a mediastinal air configuration of 3.5 cm in possible continuation with the right main stem bronchus (Fig 3). The patient was admitted to the intensive care unit with acute respiratory failure and sepsis owing to pneumonia and empyema. He was treated with noninvasive ventilation, intravenous broad-spectrum antibiotics, and fluid resuscitation. Bronchoscopy revealed a bronchopleural fistula of 2 centimeters in the right intermediate bronchus (Fig 4). A 20 French chest tube was placed for drainage of the right-sided empyema. Repeated CT scan after 10 days showed a decrease of empyema and consolidations. The mediastinal air configuration remained unchanged. No signs of cancer recurrence were detected.
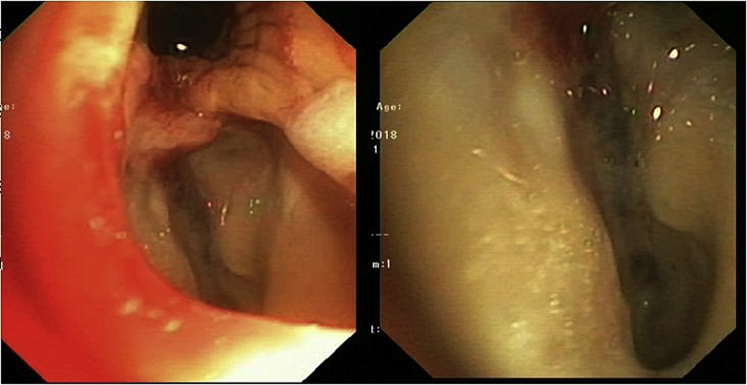
Figure 2.
Gastroscopy showing radiation esophagitis with stenosis.
Figure 3.
On the left conventional chest x-ray showing atelectasis and right sided pleural effusion, and on the right computed tomography–thorax showing extensive, presumably infectious consolidations in the right lower lobe and a mediastinal air configuration of 3.5 cm in communication with the mainstem bronchus.
Figure 4.
Bronchoscopy showing a bronchopleural fistula with a defect of 2 cm in the right intermediate bronchus.
Pros and cons of conservative treatment and surgical treatment were carefully presented in a multidisciplinary consultation with the radiologist, oncologist, 4 thoracic surgeons and radiotherapist after which the options were shared with the patient. It was decided to optimize the patient’s condition by enteral feeding, antibiotics to treat the intrapulmonary consolidations, and surgical coverage of the fistula with a pedicled latissimus dorsi flap. Before surgery, the condition of the patient was improved: he no longer required any respiratory support, he had no fever, and had low infection parameters and better nutritional status.
The operation was performed under general anesthesia with a double lumen tube for ventilation. First, the latissimus dorsi muscle flap was harvested. Subsequently, a thoracotomy was performed in the fifth intercostal space. When entering the thoracic cavity, the lung was completely adhesive to the thoracic wall. Amidst an area of extensive inflammation and fibrosis of the mediastinum, the defect was reached. A salvage pneumonectomy was considered but deemed unfeasible owing to the impossibility to safely mobilize the main stem bronchus and pulmonary artery embedded in fibrosis due to scar tissue from radiation and infection.
The pedicled latissimus dorsi flap was draped and fixated dorsally to the bronchus to cover the defect (Fig 5). The ventilator showed only an insignificant air leak, and bronchoscopy showed full coverage of the defect. A 28 French intrathoracic chest tube was placed via a distal stab incision. Under direct vision the lung was reinsufflated and showed no signs of air leakage. The wound was closed.
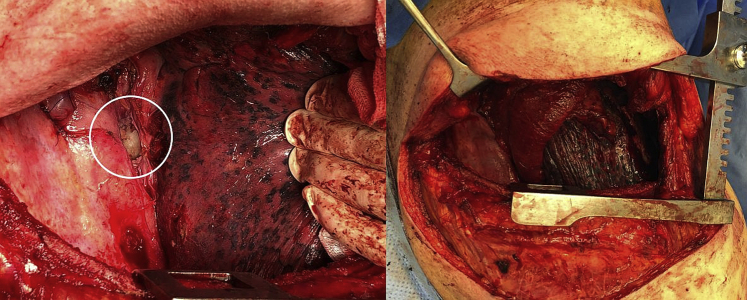
Figure 5.
Bronchopleural fistula in the first picture. Flap draped dorsally to the bronchus to cover the defect and fill the created space between esophagus and bronchus in the second picture.
The patient recovered well. After 6 days at the intensive care unit, he was transferred to the surgical ward. Limited air leakage persisted for 8 days after surgery. The drain was removed 10 days postoperatively, and on day 15 the patient was dismissed to a rehabilitation center.
Ten weeks after surgery the patient was readmitted. He had hemoptysis, pneumonia, and anemia. Bronchoscopy showed a large defect of the intermediate bronchus (Fig 6). No additional surgical options were left, and palliative care was started. The patient died 3.5 months after surgery.
Figure 6.
Bronchoscopy showing a large defect of the intermediate bronchus.
Discussion
Treatment of primary lung carcinoma depends on the general condition of the patient, staging, comorbidities, and pulmonary and cardiac function. Treatment of stage III non-small cell lung carcinoma mainly consists of concurrent chemoradiation.2
Chemoradiation therapy can cause severe complications, although to the best of our knowledge, the occurrence of a bronchopleural fistula after concurrent chemoradiation alone has not been described in literature. Pulmonary fistulas are mostly seen postsurgery after lung resection. A meta-analysis showed a much higher incidence after neoadjuvant chemoradiation and surgery, which was mainly driven by Asian studies.3,4 The mortality rate after development of a bronchopleural fistula is high, ranging from 18% to 50%.4
Bronchopleural fistula causes empyema and mediastinitis and cannot be averted when treated conservatively, eventually leading to death. Appropriate treatment consists of infection control and closure of the defect. Small fistulas from 1 to 3 mm can be treated using a flexible fiberoptic bronchoscopy under conscious sedation. Different substances are shown to be effective for closure of these small fistulas such as coils, glues (eg, fibrin glue or acrylic glue), sealants, ethanol injection, silver nitrate, spongy calf bone, or surgical sponges.3,5 In larger fistulas up to 5 mm, plugs or double disc Amplatzer devices are more effective.3,5,6 Motus et al also used this device for fistulas up to 24 mm with promising results. The Amplatzer device is made of fine metallic mesh and is placed through the defect by flexible fiberoptic bronchoscopy. It expands into 2 discs: one on the inside of the bronchus and one on the outside that will be assessed by video-assisted thoracoscopy or through a window thoracostomy from the pleural cavity. Granulation of the mesh and scar tissue effectuates airtightness, resulting in fistula closure. Limitations of this study are a small study population and short follow-up. These patients did not receive radiation therapy.7
For fistulas located in the trachea or mainstem bronchi the use of airway stents such as a Dumon silicone stent or covered self-expandable metallic stent can be used. A straight stent can be used for defects of the upper or mid trachea, and a Y-shaped stent is best suited for defects of the lower trachea or carina. Both stents are mainly used for airway obstruction but have also been used for treating fistulas. Mortality rate remains high and complications like stent migration and mucous impaction can occur.8,9 Airway stents can also be used as bridge to surgery, allowing patient optimization.
In our case the patient received concurrent chemoradiation without any prior surgery. The defect was approximately 2 cm located in the right intermediate bronchus, so surgical intervention was needed. Surgically there are 2 options: the defect can either be closed or a salvage pneumonectomy can be considered. Surgical closure of the defect can be established by using pedicled muscle flaps like a latissimus dorsi or pectoralis major, intercostal muscle, a rectus abdominis myocutaneous flap, or free flap surgery.10,11 A case report has been described using an omental flap for a bronchopleural fistula after lobectomy with optimal short-term outcome.12 However, no chemoradiation was administered, which suggests that surrounding tissue was vital and outcome is expected to be favorable. The choice of treatment depends on the location and size of the defect, comorbidities, and a history of radiation therapy. In our case a pedicled latissimus dorsi flap was considered the best option because a big muscle flap was needed to cover the defect and establish airtight closure. An intercostal muscle flap or pectoralis major flap would have been too small. Performing an operation in previously irradiated tissue has a higher perioperative and postoperative complication rate due to radiation damage, fibrosis, and poor wound healing leading to a poor prognosis of a bronchopleural fistula after radiation therapy.4,13
Bronchopleural fistula after concurrent chemoradiotherapy without surgery has never been described in literature before. In our case, an assembly of multiple factors caused the bronchopleural fistula. The tumor itself can cause a tissue defect, which, after tumor regression by chemoradiotherapy may lead to a bronchopleural fistula. Infection may precipitate these severe reactions.14 Moreover, this patient developed severe and persisting dysphagia, which is the case in less than 1% of patients, pointing to a possible higher sensitivity of this patient to chemoradiation and to possible late consequential damage.14 The goal of this case report was to increase awareness of the potentially severe complications caused by chemoradiation and the treatment options. A multidisciplinary approach is needed to strive for the best possible outcome.
Footnotes
Sources of support: Publication fee was funded by Zuyderland Medical Center, Heerlen, the Netherlands.
Disclosures: none.
References
- 1.De Ruysscher D., Faivre-Finn C., Moeller D. European Organization for Research and Treatment of Cander (EORTC) recommendations for planning and delivery of high-dose, high precision radiotherapy for lung cancer. Radiother Oncol. 2017;124:1–10. doi: 10.1016/j.radonc.2017.06.003. [DOI] [PubMed] [Google Scholar]
- 2.Midthun D.E. Overview of the initial evaluation, treatment and prognosis of lung cancer. UpToDate. https://www.uptodate.com/contents/overview-of-the-initial-treatment-and-prognosis-of-lung-cancer?search=lung%20cancer&source=search_result&selectedTitle=3∼150&usage_type=default&display_rank=3 Available at:
- 3.Cusumano G., Alifano M., Lococo F. Endoscopic and surgical treatment for bronchopleural fistula after major lung resection: An enduring challenge. J Thorac Dis. 2019;11:1351–1356. doi: 10.21037/jtd.2019.03.102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Li S., Fan J., Zhou J. Neoadjuvant therapy and risk of bronchopleural fistula after lung cancer surgery: A systematic meta-analysis of 14912 patients. Jpn J Clin Oncol. 2016;46:534–546. doi: 10.1093/jjco/hyw037. [DOI] [PubMed] [Google Scholar]
- 5.Lois M., Noppen M. Bronchopleural fistulas. An overview of the problem with a special focus on endoscopic management. Chest. 2005;128:3955–3965. doi: 10.1378/chest.128.6.3955. [DOI] [PubMed] [Google Scholar]
- 6.Klotz L.V., Gesierich W., Schott-Hildebrand S. Endobronchial closure of bronchopleural fistula using Amplatzer device. J Thorac Dis. 2015;7:1478–1482. doi: 10.3978/j.issn.2072-1439.2015.08.25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Motus I.Y., Bazhenov A.V., Basyrov R.T., Tsvirenko A.S. Endoscopic closure of a bronchopleural fistula after pneumonectomy with the Amplatzer occluder: A step forward? Interact Cardiovasc Thorac Surg. 2019 doi: 10.1093/icvts/ivz241. ivz241. [DOI] [PubMed] [Google Scholar]
- 8.Sehgal I.S., Dhooria S., Madan K. Placement of tracheobronchial silicone Y-stents: Multicenter experience and systematic review of the literature. Lung India. 2017;34:311–317. doi: 10.4103/0970-2113.209241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sökücü SN, Özdemir C, Tural Önür S, et al. Comparison of silicon and metallic bifurcated stents in patients with malignant airway lesions [e-pub ahead of print]. Clin Respir J. 10.1111/crj.13114. Accessed January 31, 2020. [DOI] [PubMed]
- 10.Fricke A., Bannasch H., Klein H.F. Pedicled and free flaps for intrathoracic fistula management. Eur J Cardiothorac Surg. 2017;52:1211–1217. doi: 10.1093/ejcts/ezx216. [DOI] [PubMed] [Google Scholar]
- 11.Huang J.W., Lin Y.Y. Transverse rectus abdominis myocutaneous flap for postpneumonectomy bronchopleural fistula: A case report. Medicine (Baltimore) 2017;96:e6688. doi: 10.1097/MD.0000000000006688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Endoh H., Yamamoto R., Nishizawa N., Satoh Y. Thoracoscopic surgery using omental flap for bronchopleural fistula. Surg Case Rep. 2019;5:5. doi: 10.1186/s40792-019-0563-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Chargari C., Riet F., Mazevet M., Morel E., Lepechoux C., Deutsch E. Complications of thoracic radiotherapy. Presse Med. 2013;42:e342–e351. doi: 10.1016/j.lpm.2013.06.012. [DOI] [PubMed] [Google Scholar]
- 14.De Ruysscher D., Niedermann G., Burnet N.G. Radiotherapy toxicity. Nat Rev Dis Primers. 2019;5:13. doi: 10.1038/s41572-019-0064-5. [DOI] [PubMed] [Google Scholar]