During the early stages of the COVID‐19 pandemic, hospitals in London, the UK epicentre, reported an unusually high number of people presenting with COVID‐19 disease developing diabetic ketoacidosis, hyperosmolar hyperglycaemic state, or a combination of both. Very high doses of insulin were often needed to manage the hyperglycaemia. It has been proposed that these metabolic disturbances may result from severe insulin resistance combined with decreased insulin secretion due to beta cell dysfunction [1]. The increased demand for pumps to deliver inotropes has led to concerns of possible shortages of infusion pumps and/or 50 ml syringes being available for insulin infusions to manage these hyperglycaemic emergencies. Concerns were also raised about the potential risk of exacerbating ‘lung leak’ in COVID‐19 positive patients using the traditional rates of fluid replacement for the management of DKA. Clinicians therefore requested that a subcutaneous insulin regimen be made available as a backup strategy for managing diabetic ketoacidosis and guidance on the fluid replacement regimen.
In response to these requests the National Diabetes Inpatient COVID‐19 Response Group has developed guidance on the management of DKA using subcutaneous insulin based on a regimen developed by Umpierrez and colleagues in the US [2], accompanied by two alternative fluid replacement regimens. The first is that from the Joint British Diabetes Societies [3] guidance for managing typical DKA. The second is a more cautious regimen for COVID‐19 positive/suspected patients with consideration of a higher rate of fluid replacement if there is significant hypovolaemia or acute kidney injury (Figure 1). Importantly, clinical judgement, frequent senior review, and regular monitoring of fluid balance and oxygen saturations are advised. The regimen recommends using rapid acting insulin analogues. Given the need to reduce the time the health professional is in direct contact with the patient a 4 hourly dosing schedule has been recommended with the dose calculated on body weight to equate to a similar quantity of insulin that would have been delivered by an insulin infusion. Finally, as with other guidance we recommend continuing or starting a basal insulin alongside.
Figure 1.
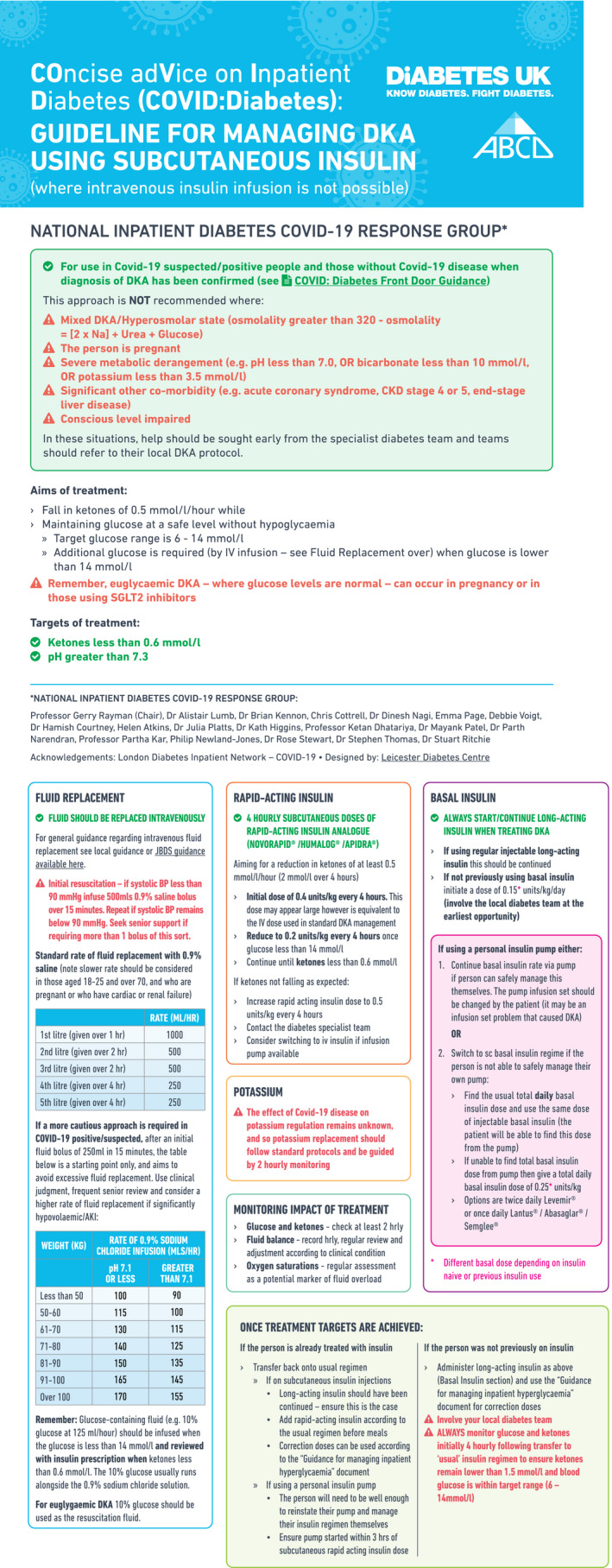
Guideline graphic
We hope that most teams will not find it necessary to use the subcutaneous insulin route to manage DKA, but we understand that this regimen has been welcomed by some working in less well‐resourced countries.
Diabet. Med. 37, 1214–1216(2020)
References
- 1. Bornstein SR, Rubino F, Khunti K, Mingrone G, Hopkins D, Birkenfeld AL et al. Practical recommendations for the management of diabetes in patients with COVID‐19. Lancet Diabetes Endocrinol 2020 Published Online, April 23, 2020, 10.1016/:S2213-8587(20)30152-2 [DOI] [PMC free article] [PubMed]
- 2. Andrade‐Castellanos CA, Colunga‐Lozano LE, Delgado‐Figueroa N, Gonzalez‐Padilla DA. Subcutaneous rapid‐acting insulin analogues for diabetic ketoacidosis. Cochrane Database Syst Rev 2016. Jan 21;(1). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Savage MW, Dhatariya KK, Kilvert A, Rayman G et al. Joint British Diabetes Societies Guideline for the Management of Diabetic Ketoacidosis. Diabetic Medicine 2011; 28(5): 508–515. [DOI] [PubMed] [Google Scholar]


