Abstract
Introduction
The global pandemic due to SARS‐CoV‐2 has resulted in an expansion of telemedicine. Measures of quality and barriers for rapid use by patients and physicians are not well described.
Objective
To describe results from a quality improvement initiative during a rapid adoptive phase of telemedicine during the pandemic.
Design
Patient and physician satisfaction with synchronous audiovisual telemedicine visits was measured during the early adoptive phase (6 April 2020‐17 April 2020) within the division of sports medicine in an academic Physical Medicine and Rehabilitation (PM&R) department. Patients were invited to participate in a quality improvement initiative by completing an online survey at the end of a telemedicine visit. Physicians completed a separate survey.
Primary Outcome Measures
Patient measures included visit type, duration of encounter, quality, and satisfaction. Physicians reported on experiences performed telemedicine.
Results
Surveys were completed by 119 patients (293 telemedicine encounters, response rate 40.6%) and 14 physiatrists. Telemedicine was utilized primarily for follow‐up visits (n = 74, 70.6%), and the most common duration was 15 to 29 minutes. Patients rated their telemedicine visit as “excellent” or “very good” across measures (91.6%‐95.0%) including addressing concerns, communication, developing a treatment plan, convenience, and satisfaction. Value of completing a future telemedicine visit was measured at 84.9%. Most reported estimated travel time saved was in excess of 30 minutes. Rate of no‐show was 2.7%. Most physicians (57.1%) had no prior experience with telemedicine visits, and most were comfortable performing these visits after completing 1 to 4 sessions (71%). Nearly all physicians (92.9%) rated their telemedicine experience as very good or excellent. The key barrier identified for telemedicine was technical issues. All physicians reported plans to perform telemedicine visits if reimbursement continues.
Conclusions
In summary, rapid expansion of telemedicine during the COVID‐19 pandemic was well‐received by a majority of patients and physicians. This suggests feasibility in rapid expansion of telemedicine for other outpatient sports medicine practices.
Introduction
The utilization of telemedicine has increased during SARS‐CoV‐2 pandemic (commonly referred to as COVID‐19). This form of health care delivery most commonly uses technology that allows for both video and auditory communication to conduct clinical care outside of the traditional in‐office or hospital setting. The use of telemedicine for physiatry includes both inpatient and outpatient health care delivery, and this may be particularly important for individuals with disability and travel limitations. 1 Visits can be synchronous (real‐time interaction between patient and provider) or asynchronous. Barriers to widespread use of telemedicine have included insurance payment models, access to telehealth technology, physician knowledge, malpractice insurance, and concerns regarding value. 2 , 3
The COVID‐19 pandemic has driven health care delivery to rapidly expand telemedicine. In an abrupt and unexpected fashion, hospital systems suspended or drastically reduced in‐person health care delivery for nonessential medical encounters to reduce the risk of virus spread. Telemedicine has become an alternative model to deliver patient care while maintaining social distancing and limiting contagion. During this time, areas of physiatric care that would not otherwise utilize telehealth were forced to move to this platform. Solutions have been proposed to assist physiatrists in conducting telemedicine encounters including effective documentation of physical examinations and incorporating prehabilitation strategies to improve telemedicine best practices. 4
The rapid expansion of telemedicine may provide continued access to care in outpatient practices. However, knowledge on how physicians and patients adapt to rapid expansion of telemedicine is limited, particularly in the setting of a pandemic. Although telemedicine has been proposed for multiple uses within physiatry practice and patient populations, reports on feasibility and quality are limited. Quality improvement measures will provide insight into patient populations, medical conditions, and types of outpatient encounters that can be effectively managed using telemedicine. The rationale for performing this type of investigation is to assist physiatrists and hospital systems that are suddenly adopting telemedicine in their medical practice. The purpose of this report is to describe a quality improvement initiative during the rapid adoptive phase of telemedicine in outpatient sports medicine practices during the COVID‐19 pandemic.
Methods
The context of this quality improvement project was to measure patient and physician responses during the rapid adoption of telemedicine during the COVID‐19 pandemic. The methodology was reviewed and approved by our academic department quality improvement committee, and the project was determined to be exempt from institutional review board (IRB) approval. The report conforms to SQUIRE 2.0 (Standards for QUality Improvement Report Excellence) guidelines. 5 Participants in this quality improvement project were from a population of patients and physicians who completed a telemedicine visit at four different hospital systems (Brigham and Women's Hospital, Massachusetts General Hospital, Newton Wellesley Hospital, and Spaulding Rehabilitation Hospital) within a single academic department of Physical Medicine and Rehabilitation (PM&R). Fourteen physiatrists participated from Spaulding Rehabilitation Hospital Department of Physical Medicine and Rehabilitation, from 6 April 2020 to 17 April 2020. Patients were seen for a variety of acute and chronic musculoskeletal conditions under nonsurgical treatment and for concussion management. All patients seen by physicians for telemedicine visits during this interval were invited at the conclusion of the visit to complete an online quality improvement survey consisting of 15 items (Appendix, Figure 1). The survey was provided on the same day of visit through use of electronic communication, including electronic medical record, chat function of telemedicine platform, and rarely through electronic mail. To our knowledge, there are no standardized measures that have been developed for telemedicine visits to measure quality or patient satisfaction. 6 Therefore, we used group consensus to develop the survey and measures of interest. This included questions that were descriptive of the patient population (gender, age category, insurance status), telemedicine encounter (new vs. follow‐up, reason for visit, duration of visit, participation of family, typical travel time for visit), and experience during encounter using a Likert scale with five values (excellent to poor). A free text option was included to record any additional comments on patient experience or difficulties with the encounter.
All physiatrists who completed one or more telemedicine visits during the dates of 6 April 2020 to 17 April 2020 were instructed to complete a separate quality improvement survey (Appendix Figure 2). The provider questionnaire contained 12 items and included measures of experience with telemedicine prior to the COVID‐19 pandemic. Questions about the type of digital platform, number of visits to become comfortable delivering care, and satisfaction with performing telemedicine visits were included. Billing practice and barriers in telemedicine delivery prior to and during COVID‐19 were also measured. The total number of visits as well as missed visits were recorded to determine patient participation and no‐show rates. Additional questions on utility for future encounters were recorded. Physicians were similarly provided free text to describe any adverse events or comment on personal experience with telehealth virtual visits.
The quality improvement survey was recorded using an online survey tool through REDCap (Research Electronic Data Capture) electronic data capture tools hosted at Partners Healthcare server. 7 , 8 REDCap is a secure, web‐based software platform designed to support data capture for research studies, providing (1) an intuitive interface for validated data capture, (2) audit trails for tracking data manipulation and export procedures, (3) automated export procedures for seamless data downloads to common statistical packages, and (4) procedures for data integration and interoperability with external sources.
During the time of this quality improvement project, telemedicine platforms used by the institution incorporated audio and visual input and included both InTouch and Zoom. Both software platforms were HIPAA Compliant and were able to provide screen sharing. Training on these platforms was provided by the hospital system with a brief tutorial delivered electronically. Staff training, superusers, and help desk phone number were provided to address questions from physiatrists and patients.
The data were evaluated in aggregate with an a priori plan to evaluate using descriptive statistics. Given the nonparametric distribution of categorical data, the Fisher's exact test was used to analyze the relationship between patient satisfaction (dependent variable) and age category, gender, duration of visit, and type of visit (independent variables). For all statistical analyses, patient satisfaction was categorized into three groups: excellent, very good, or good/fair/poor. Data were combined to two groups (excellent and very good; good, fair, or poor) as few total measurements noted in the latter categories. Significance level was set to a threshold of 0.05.
Results
A group of 14 sports and musculoskeletal medicine physiatrists conducted a total of 293 telemedicine visits over the study period (mean 22.5 ± 17 visits per physician, range 4‐54). There were eight no‐show visits (2.7%) during the study period. A total of 119 patients completed the survey (40.6% response rate) and were included in this study (Table 1). The majority of patients were female and the most common age range was 35‐ to 64–years‐old. All patients were insured. Estimated travel time to and from appointments varied widely among patients, with most travel times estimated to exceed 30 minutes. Telehealth visits were most commonly follow‐ups (70%) lasting 15 to 29 minutes and rarely included a family member, friend, or other patient advocate. The reason for visit varied widely, most commonly related to musculoskeletal and sports injuries, followed by pain and spine issues.
Table 1.
Patient demographics and telehealth visit characteristics, n (%)
| Gender | Type of visit | ||
| Female | 73 (61.3) | New | 35 (29.4) |
| Male | 44 (37.0) | Follow‐up, established issue | 74 (62.2) |
| Transman | 2 (1.7) | Follow‐up, new issue | 10 (8.4) |
| Age (years) | Duration of visit (minutes) | ||
| 8‐12 | 0 | 5‐14 | 14 (11.8) |
| 13‐17 | 3 (2.5) | 15–29 | 67 (56.3) |
| 18‐34 | 38 (31.9) | 30‐60 | 34 (28.6) |
| 35–64 | 63 (52.9) | 60+ | 4 (3.4) |
| 65+ | 15 (12.6) | ||
| Insurance status | Reason for visit | ||
| Insured | 119 (100) | Spine issue | 23 (19.3) |
| Uninsured | 0 | Sports injury | 35 (29.4) |
| Typical travel time (minutes) | Concussion | 2 (1.7) | |
| 5–14 | 16 (13.4) | Other musculoskeletal issue | 49 (41.2) |
| 15–29 | 27 (22.7) | Other pain issue | 29 (24.4) |
| 30‐59 | 35 (29.4) | Review imaging result | 5 (4.2) |
| 60‐89 | 21 (17.6) | Review non‐imaging result | 1 (0.8) |
| 90‐120 | 20 (16.8) | Medication question | 3 (2.5) |
| Family or friend involvement | Procedure question | 6 (5.0) | |
| Yes, present | 8 (6.7) | Return to activity/exercise | 12 (10.1) |
| Yes, remote | 4 (3.4) | Other | 11 (9.2) |
| No | 107 (89.9) | ||
Patient satisfaction was independent of age category (P = .20), gender (P >.99), duration of visit (P = .95), and type of visit (P = .35). Overall, patients appeared to be highly satisfied (defined as “excellent” or “very good” responses) with their telehealth visits across all patient‐centered outcome measures (Figure 1): addressing my concerns and questions (92.4%), communication with my provider (94.1%), developing a treatment plan (92.4%), convenience (95.0%), overall visit satisfaction (91.6%), and value in having a future telehealth visit (84.9%). Qualitatively, many patients expressed gratitude for access to their physicians at a time when they would otherwise not be able to receive medical care. Similar to physicians, however, many felt that telehealth visits worked best for follow‐up encounters where more limited physical examination was adequate for management recommendations. Of note, one patient reported difficulty with navigating the telehealth visit platform due to visual impairment and one patient had a hearing deficit and was aided by his wife during the encounter.
Figure 1.
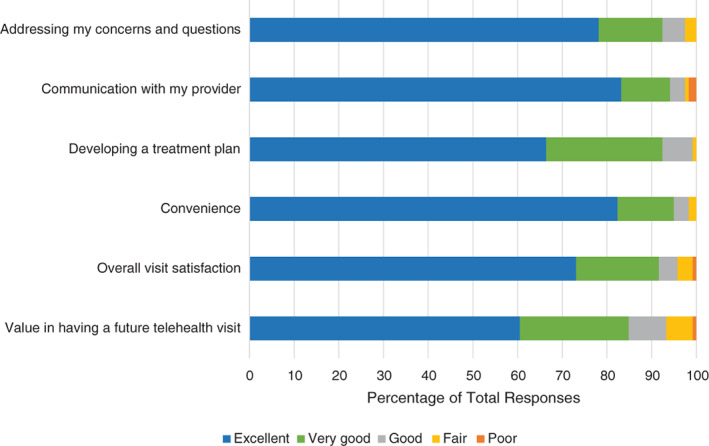
Patient responses across 119 telemedicine encounters, divided by question. Each question response was “excellent,” “very good,” “good,” “fair,” or “poor.” Most patients reported “excellent” or “very good” to their experience with telemedicine visit.
Physicians were also highly satisfied with their telehealth visits, with 92.9% reporting either “excellent” or “very good” overall satisfaction. Most physicians had not used telehealth platforms prior to the ongoing pandemic, but all reported comfort with use after 10 visits. Just over 70% were comfortable after 1 to 4 visits. Many of the physician‐reported barriers to telehealth use prior to the pandemic, including concerns regarding reimbursement, time, and lack of knowledge or training, diminished with use during the pandemic. Further barriers in health care delivery (staff coordinating visits, incorporating the electronic medical record, and platform for documentation and orders) were cited. All physicians billed by time for telehealth visits. All physicians reported that they would continue to use telehealth in the future if reimbursement continued, more so for follow‐up visits than for new patient evaluations (Table 2). Qualitative responses indicate that preference for performing telemedicine for follow‐up visits is likely due to lack of ability to perform a comprehensive physical examination and concern regarding development of patient rapport.
Table 2.
Physician characteristics and outcome measures, n (%)
| Prior telehealth use | ||
| Yes, frequently | 3 (21.4) | |
| Yes, infrequently | 3 (21.4) | |
| No | 8 (57.1) | |
| Number of visits until comfortable | ||
| 1–4 | 10 (71.4) | |
| 5–10 | 4 (28.6) | |
| 11+ | 0 | |
| Platform use | ||
| InTouch | 5 (35.7) | |
| Zoom | 14 (100) | |
| Facetime | 3 (21.4) | |
| Other | 2 (14.3) | |
| Billing method | ||
| By time | 14 (100) | |
| By medical complexity | 0 | |
| Barriers to use | Pre‐pandemic | During pandemic |
| Reimbursement concern | 6 (42.9) | 1 (7.1) |
| Lack of knowledge/training | 5 (35.7) | 1 (7.1) |
| Time | 3 (21.4) | 1 (7.1) |
| Technology concern | 9 (71.4) | 8 (64.3) |
| None | 2 (14.3) | 5 (35.7) |
| Future use | ||
| Yes | 14 (100) | |
| No | 0 | |
| Future reason for use | ||
| New patient evaluations | 3 (21.4) | |
| Follow‐up visits | 12 (85.7) | |
| Follow‐up of imaging | 13 (92.9) | |
| Follow‐up test results | 13 (92.9) | |
| Patient education | 13 (92.9) | |
| Improved access | 12 (85.7) | |
One adverse event was noted due to unanticipated vasovagal syncope. The event was limited to 15 seconds and fortunately the patient fell onto her bed where she was sitting at the time of the encounter. She reported no injury and returned to her baseline status. She was called by her provider again that day and reported no return of prior symptoms.
Discussion
The purpose of this study was to report patient and provider experience with the delivery of telemedicine visits during the COVID‐19 pandemic. Within a patient population of various ages and health concerns, a majority reported high satisfaction with their experience using telemedicine. Likewise, a majority of physiatrists reported high satisfaction with performing telemedicine visits and interest in future use. Limitations in technology, inaccessibility for patients with sensory disability or non‐English speakers, and inability to perform a face‐to‐face physical examination were recognized barriers.
Patients reported high quality and satisfaction across ages and genders. This included addressing concerns and developing a treatment plan, consistent with a prior large review for in‐home use of telemedicine. 9 Notably high satisfaction was recorded in a mixed population of new and follow‐up telemedicine encounters. Our findings of both high satisfaction across new and follow‐up telemedicine encounters expands on a prior report of telemedicine follow‐up encounters performed by 254 patients and 61 physicians in an overlapping hospital system. 10 In this report, no differences in the “overall quality of the visit” were reported between patients (62.6%) and clinicians (59%). 10 Our population saved over 30 minutes of travel time on average. Decreased travel time is recognized as a value of telemedicine, 11 especially for those living in remote or rural areas. 6 In‐person visits have costs to patients, employers, and the environment due to the need for travel. Clear inefficiencies, defined as the small fraction total time for an in‐person encounter to total time accounting for travel, is well documented in the literature. 12 , 13 Although speculative, the no‐show rate of 2.7% across the 289 telemedicine visits in our report may be explained by reducing barriers to complete these visits; no‐show rates for sports medicine subspecialty visits has been identified in one report at 13.3%. 14
Physiatrists reported satisfaction with telemedicine visits. Our institution created an iterative approach to evaluate and discuss barriers for use of telemedicine. A priority to rapidly complete telemedicine visits for all traditional face‐to‐face encounters was communicated by leadership. Notably rapid expansion of telemedicine visits for physicians was aided by having appropriate support staff to contact patients and coordinate visits. Incorporating telemedicine into existing workflow may reduce clinician burden and has been a reported predictor of physician acceptance. 15 There are recognized limitations in telemedicine for performing aspects of the physical examination,11 although recent solutions have been proposed to improve this aspect of care. 4 Regardless, telemedicine may not be appropriate for all patient populations. For example, patients with new‐onset neurological symptoms including weakness would still benefit from an in‐person examination to help establish a diagnosis.
Our report, and the use of telemedicine, is not without limitations. We performed this quality improvement initiative within our department that focused on outpatient musculoskeletal and sports medicine practices; other physicians or providers and patient populations may have different health care needs that would be better served with face‐to‐face visits. Our response rate for a quality improvement initiative was adequate, but we cannot exclude the potential for bias in patients and physiatrists who participated. It is important to recognize that adoption of telemedicine was not universally accepted, with one physiatrist rating the experience as “fair” and a small number of patients describing different aspects of the telemedicine visits as “fair” or “poor.” Telemedicine may be used to review or determine need for imaging or laboratory testing, and to prescribe medications or physical therapy, and to discuss overall treatment plan including procedures; however, procedures require in‐person visits to perform. In addition, the use of telemedicine still presents systemic barriers to patients with sensory disability (eg, blind, deaf, hard of hearing), cognitive deficits, those challenged in using technology or without necessary electronic devices, as well as those who require use of a medical interpreter. Providing appropriate resources such as use of interpreter services or incorporating other assistive technology is important to help address and reduce risk for worsening preexisting disparities in health care access for individuals with disabilities or underserved populations.
Findings from our report have practical implications for physiatrists. Rapid expansion of telemedicine can be performed with high patient and provider satisfaction. Use of platforms that are supported by smartphones may be most practical, given that 81% of the United States population has a smartphone. 16 The physiatrist should have adequate support staff to arrange logistics prior to the telemedicine visit. Education and training should be provided with recognition that physiatrists are likely to feel most comfortable delivering telemedicine by their fourth encounter, on average. Patients should be advised to complete the encounter in a location that provides appropriate privacy. Barriers in performing the physical examination should be recognized, although recent strategies have been proposed that can assist with effective documentation. 4 Adverse events are uncommon, but our experience suggests that patient comfort should be accounted for when performing the visits, including sitting for prolonged discussion or assessing the safety of surrounding environment (to perform balance testing, for example).
Conclusion
In summary, this quality improvement report describes experience in the rapid expansion of telemedicine during the COVID‐19 pandemic. A majority of patients and physiatrists reported high satisfaction and value in the use of telemedicine for evaluation and management of conditions seen in outpatient musculoskeletal and sports medicine practice. Clinical support staff for the physiatrist and patients may help optimize its use. Limitations in technology and the ability to perform a physical examination are recognized barriers that should be considered. Our report suggests that physiatrists may consider using telemedicine in practice with good overall patient and physician experience.
CME Question.
In an outpatient survey of practicing musculoskeletal physiatrists, the most commonly cited barrier to use of telemedicine was lack of:
Reimbursement
Knowledge/training
Time
Technology
Answer online at http://me.aapmr.org
Appendix A 1.
Figure 1. Telehealth patient satisfaction and quality improvement.
- Age (in years)
- 8‐12, 13‐17, 18‐34, 35‐64, 65 and older
- Gender
- Female, Male, Transman, Transwoman, Non‐binary, Other
- Health Care Insurance Status
- Insured, Uninsured, Prefer not to answer
- Incorporated family, friend, or caregiver during visit
- Yes ‐ with me during visit, Yes ‐ joined remotely, No
- Visit type
- New (no prior face‐to‐face provider visit), Follow‐up (previously seen provider), Follow‐up with new issue (previously seen provider)
- Reason for visit (select all that apply)
- Spine condition, Sports injury, Concussion, Other condition (tendon, joint, or bone injury), Other pain, Other reason for visit (not listed), Review imaging results (eg, MRI, X‐ray), Review results of non‐imaging tests (ex. lab studies), Medication question, Procedure question, Return to activity/exercise
- Estimated time of visit (in minutes)
- 5‐14, 15‐29, 30‐60, +60
-
Estimated round trip travel time to complete a typical in‐person visit with this provider (hypothetical for new patient or time required for a prior visit with same provider in minutes including parking)
- 5‐14, 15‐29, 30‐59, 60‐89, 90‐120
Please rate your experience in relation to this telehealth visit. Please answer each question using the measures: excellent, very good, good, fair, poor.
Addressing my concerns and questions
Communication with my provider
Developing a treatment plan
Convenience
Overall visit satisfaction
Value in having a future telehealth visit
Optional question: Please feel free to provide feedback on anything that you found particularly helpful or limitations to your telehealth experience
Figure 2. Telehealth quality improvement outcomes sports–physician survey.
Please refer only to your experience with combined audio + video telehealth encounters as you answer the following questions.
- Did you use telehealth prior to COVID‐19, defined as combined audio + visual communication (such as InTouch, Zoom)?
- Yes – frequently Yes – infrequently No
- This question refers to performing telehealth during April 6‐17: What platforms did you use to complete visits (select all that apply)?
- InTouch, Zoom, Facetime, Other
- Indicate the number of visits you completed to feel comfortable performing telehealth:
- 1‐4, 5‐10, 11+, I do not feel comfortable.
- Satisfaction with telehealth:
- Excellent, Very good, Good, Fair, Poor
- In general, I determined my level of billing:
- by time, by medical complexity
- Key barriers to use of telehealth prior to COVID‐19 (select all that apply):
- Concern about reimbursement, Knowledge, Time, Technology, None
- Key barriers to use of telehealth during COVID‐19 (select all that apply):
- Concern about reimbursement, Knowledge, Time, Technology, None
Number of telehealth visits conducted since April 6 (Please review your Epic schedule; This is necessary for total denominator for responses)
Number of no‐shows for telehealth visits conducted since April 6 (Please review your Epic schedule)
- Based on experiences, if reimbursement for telehealth continues do you plan to use telehealth in the future after this pandemic has subsided?
- ‐Yes, No
- Based on experiences, how do you plan to utilize telehealth (choose all that apply):
- Follow‐up of imaging, Follow‐up test results, Patient education, New patient evaluations, Follow‐up visits, Complete visits for those living remotely or with limited access to transportation
Please provide any additional comments regarding your experience with telehealth visits (ie, issues, benefits, adverse events, etc).
Disclosure: none.
All financial disclosures and CME information related to this article can be found on the mē ® site (http://me.aapmr.org/) prior to accessing the activity.
Footnotes
This journal‐based CME activity is designated for 1.0 AMA PRA Category 1 Credit and can be completed online at http://www.me.aapmr.org. This activity is FREE to AAPM&R members and available to nonmembers for a nominal fee. For assistance with claiming CME for this activity, please contact (847) 737‐6000.
References
- 1. Tenforde AS, Hefner JE, Kodish‐Wachs JE, Iaccarino MA, Paganoni S. Telehealth in physical medicine and rehabilitation: a narrative review. PM R. 2017;9(5S):S51‐S58. [DOI] [PubMed] [Google Scholar]
- 2. Scott Kruse C, Karem P, Shifflett K, Vegi L, Ravi K, Brooks M. Evaluating barriers to adopting telemedicine worldwide: a systematic review. J Telemed Telecare. 2018;24(1):4‐12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Adler‐Milstein J, Kvedar J, Bates DW. Telehealth among US hospitals: several factors, including state reimbursement and licensure policies, influence adoption. Health Aff (Millwood). 2014;33(2):207‐215. [DOI] [PubMed] [Google Scholar]
- 4. Verduzco‐Gutierrez M, Bean AC, Tenforde AS, Tapia RN, Silver JK. How to conduct an outpatient telemedicine rehabilitation or prehabilitation visit. PM R. 2020. 10.1002/pmrj.12380. [Epub ahead of print]. [DOI] [PubMed] [Google Scholar]
- 5. Ogrinc G, Davies L, Goodman D, Batalden P, Davidoff F, Stevens D. SQUIRE 2.0 (Standards for QUality Improvement Reporting Excellence): revised publication guidelines from a detailed consensus process. BMJ Qual Saf. 2016;25(12):986‐992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Orlando JF, Beard M, Kumar S. Systematic review of patient and caregiversʼ satisfaction with telehealth videoconferencing as a mode of service delivery in managing patientsʼ health. PLoS One. 2019;14(8):e0221848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)–a metadata‐driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42(2):377‐381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Harris PA, Taylor R, Minor BL, et al. The REDCap consortium: building an international community of software platform partners. J Biomed Inform. 2019;95:103208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Almathami HKY, Win KT, Vlahu‐Gjorgievska E. Barriers and facilitators that influence telemedicine‐based, real‐time, online consultation at patientsʼ homes: systematic literature review. J Med Internet Res. 2020;22(2):e16407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Donelan K, Barreto EA, Sossong S, et al. Patient and clinician experiences with telehealth for patient follow‐up care. Am J Manag Care. 2019;25(1):40‐44. [PubMed] [Google Scholar]
- 11. Thiyagarajan A, Grant C, Griffiths F, Atherton H. Exploring patientsʼ and cliniciansʼ experiences of video consultations in primary care: a systematic scoping review. BJGP Open. 2020;4(1). 10.3399/bjgpopen20X101020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Abbott DE, Macke RA, Kurtz J, et al. Financial and temporal advantages of virtual consultation in veterans requiring specialty care. Mil Med. 2018;183(1–2):e71‐e76. [DOI] [PubMed] [Google Scholar]
- 13. Soegaard Ballester JM, Scott MF, Owei L, Neylan C, Hanson CW, Morris JB. Patient preference for time‐saving telehealth postoperative visits after routine surgery in an urban setting. Surgery. 2018;163(4):672‐679. [DOI] [PubMed] [Google Scholar]
- 14. Lee SR, Dix DB, McGwin G, et al. Correlation of appointment times and subspecialty with the no‐show rates in an orthopedic ambulatory clinic. J Healthc Manag. 2018;63(6):e159‐e169. [DOI] [PubMed] [Google Scholar]
- 15. Kissi J, Dai B, Dogbe CS, Banahene J, Ernest O. Predictive factors of physiciansʼ satisfaction with telemedicine services acceptance. Health Informatics J. 2019;1460458219892162. 10.1177/1460458219892162. [Epub ahead of print]. [DOI] [PubMed] [Google Scholar]
- 16. PEW Research Center . Mobile facts sheet. https://www.pewresearch.org/internet/factsheet/mobile/. Published June 2019. Accessed April 19, 2019.


