Editor
In the context of COVID‐19 pandemic, teledermatology is being favoured over in‐person consultation in order to avoid the possibility of virus transmission. 1 In France, COVID‐19 was not known to cause cutaneous manifestations before 6 April 2020, when an alert about possible associated skin symptoms was raised to the general public and the professional social network. 2 , 3 , 4 We aimed to assess the impact of alerting about COVID‐associated lesions on the activity of urgent teledermatology (TD) and the activity of dermatologic emergencies unit (DEU) of two university hospitals during this pandemic.
This study was conducted between 30 March and 10 April 2020. These two institutions provide urgent consultations via a DEU and a store‐and‐forward teledermatology, between dermatologists and other healthcare professionals, with rapid responses. All consultations in the DEU and urgent TD were retrieved, and the number of consultations for suspicious COVID‐associated lesions and non‐COVID lesions was collected before and after the alert. For TD cases, the suspicion was made by the referring physician. For the DEU cases, the suspicion was made by the patients after having heard about the possible COVID‐19‐associated lesions through the media. For both groups DEU and TD, the number of cases, the mean consultation per day and the proportion of suspicious COVID‐associated lesions per day, before and after the alert, were compared. Finally, the type of possible COVID‐associated lesions, after the dermatologists’ evaluation, was described.
The number of patients in both groups, before and after the signal, is seen in Figs 1 and 2. Among teledermatology consultations, before and after the alert, the proportions of the cases for suspicious COVID‐associated lesions are 2/65 (3%) and 89/182 (48.9%), respectively (P < 10−3). Moreover, the mean number of consultations per day, before and after the alert, increased from 9.28 ± 1.36 to 36.4 ± 2.52, respectively (P = 0.007). Among DEU consultations, neither the proportions of the cases for suspicious COVID‐associated lesions [3/46 (6.5%) and 9/66 (13.6%), respectively] nor the mean number of consultations (6.5 ± 1.1 and 13.2 ± 1.86, respectively) significantly differed before and after the alert (P = 0.35, P = 1). After a dermatologic evaluation, 80 patients in total had possible COVID‐associated lesions: mostly chilblains (58/80), vasculitic lesions (6/80), morbilliform rash (5/80), pityriasis rosea‐like lesions (3/80) and urticaria (3/80).
Figure 1.
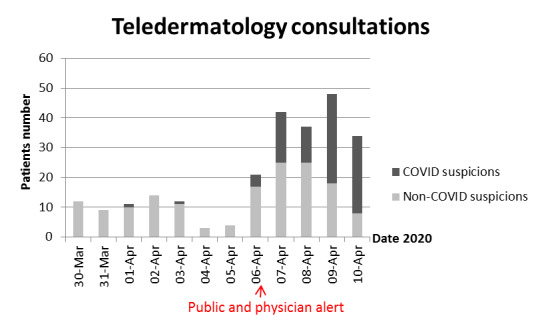
Number of patients with suspicious COVID‐associated lesions and non‐COVID lesions in teledermatology consultations.
Figure 2.
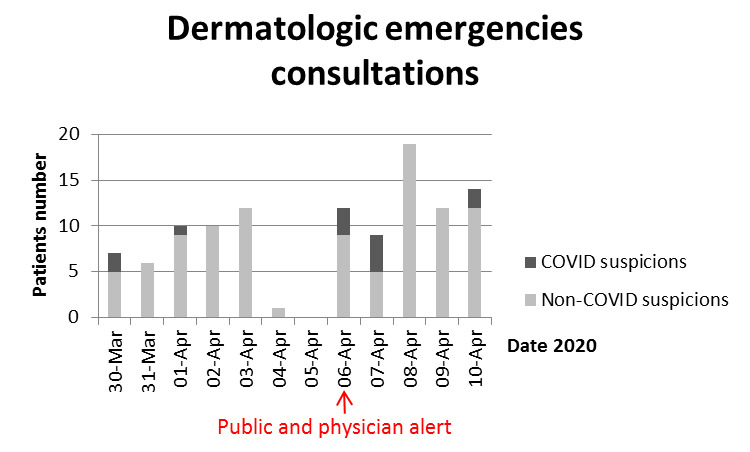
Number of patients with suspicious COVID‐associated lesions and non‐COVID lesions in the dermatologic emergencies unit.
COVID‐associated cutaneous signs were mainly described in pauci‐symptomatic patients for COVID‐19. 2 , 5 , 6 The alert on possible COVID‐associated cutaneous signs did not modify the activity of DEUs, but there was a significant increase in urgent TD’s activity. During the pandemic period, TD can thus act as a substitute of face‐to‐face visits to limit virus transmission in outpatients, whereas in normal settings, it is considered as a supplement to standard dermatological care. 7 As most of COVID‐associated lesions are considered mild and can be diagnosed and managed without in‐person visits, TD can be efficient for managing non‐COVID and COVID‐related skin conditions and reassuring patients through their primary care physicians. In a period where lockdown is among essential keys for COVID‐19 control, COVID patients might not have to consult in‐person for their skin lesions.
In conclusion, teledermatology is a weapon that dermatologists should use to play their indispensable role in controlling this pandemic.
Conflict of interest
None.
Funding sources
None.
Acknowledgements
Dr Camille Hua for her assistance IRB#00011558 approved study.
References
- 1. Kwatra SG, Sweren RJ, Grossberg AL. Dermatology practices as vectors for COVID‐19 transmission: a call for immediate cessation of nonemergent dermatology visits. J Am Acad Dermatol 2020; 82: e179–e180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Recalcati S. Cutaneous manifestations in COVID‐19: a first perspective. J Eur Acad Dermatol Venereol 2020; 34. [DOI] [PubMed] [Google Scholar]
- 3. Covid‐19: alerte sur les signes cutanés [Internet] . Le Quotidien du Pharmacien.fr. URL https://www.lequotidiendupharmacien.fr/formation/specialites‐medicales/covid‐19‐alerte‐sur‐les‐signes‐cutanes (last accessed 27 April 2020).
- 4. Duong TA, Velter C, Rybojad M et al. Did Whatsapp® reveal a new cutaneous COVID‐19 manifestation? J Eur Acad Dermatol Venereol 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Tammaro A, Adebanjo GAR, Parisella FR, Pezzuto A, Rello J. Cutaneous manifestations in COVID‐ 19: the experiences of Barcelona and Rome. J Eur Acad Dermatol Venereol 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Piccolo V, Neri I, Filippeschi C et al. Chilblain‐like lesions during COVID‐19 epidemic: a preliminary study on 63 patients. J Eur Acad Dermatol Venereol 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Villani A, Scalvenzi M, Fabbrocini G. Teledermatology: a useful tool to fight COVID‐19. J Dermatolog Treat 2020; 31: 325. [DOI] [PubMed] [Google Scholar]


