Editor
Hogan1 reported in their correspondence that they ‘endeavour, as always, to provide the highest level of patient care within the framework of imposed constraints and to preserve the health of the surgical workforce providing this care’ and that ‘there is minimal evidence regarding emergency surgical care in the COVID-19 era’1. We agree, especially for tracheostomy. Severe COVID-19 causes acute respiratory distress syndrome requiring mechanical ventilation for a prolonged period, needing tracheostomy in some patients. However, percutaneous and surgical tracheostomy are aerosol-generating medical procedures putting medical personnel, even those wearing optimized personal protective equipment (PPE), at risk2. During this pandemic, preserving the health of the healthcare workforce and avoiding nosocomial spread of the virus are priorities2–4.
Here, we describe a hybrid surgical tracheostomy using a percutaneous kit under a customized insulated field with the patient in a supine position using a thyroid drape (Fig. 1). Two surgical arches protected with sterile camera covers were placed and covered by a transparent surgical vertical isolation drape in which a large suction tube was placed to create negative pressure. The goal was to avoid any leakage of viral particles through openings in the drape (made for the operator's hands). A Seldinger technique with a guidewire was used to dilate the tract. Ventilation was suspended prior to each dilator removal, and the open extremity of the in-place dilators was closed with a surgeon's finger to avoid any leak each time ventilation was resumed. The tracheostomy tube, armed with corresponding hard-rubber stylet with cone-shaped tips, was inserted when ready.
Fig. 1.
Hybrid surgical tracheostomy
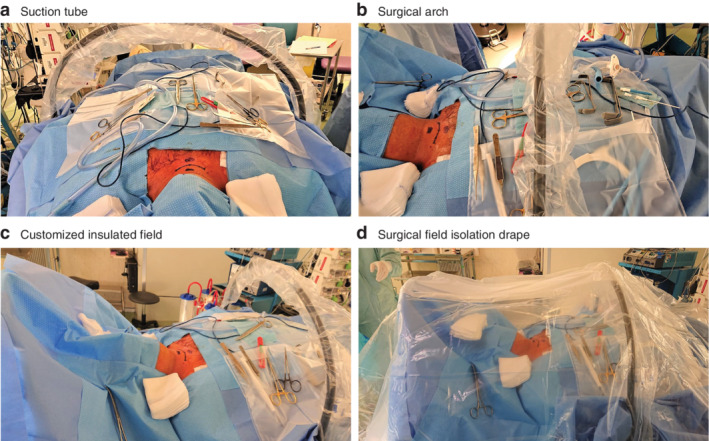
a Hybrid surgical tracheostomy using a large suction tube to create negative pressure. b Surgical arch protected with sterile camera cover and percutaneous tracheostomy kit. c Two surgical arches: one arch placed over the head under the surgical drape and one over the abdomen. d A surgical field isolation drape prevented leakage of viral particles.
Recommendations on the timing and location of surgery, and optimal PPE have been published previously2,4–5. Adding a customized insulated field and the hybrid technique, which avoids having to perform a fibreoptic bronchoscopy to check the tracheal puncture location or the final position of the canula, minimizes the aerosolization risk to provide extra security for the staff.
References
- 1. Hogan A. COVID-19 and emergency surgery. Br J Surg 2020; 10.1002/bjs.11640 [Epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Di Marzo F, Sartelli M, Cennamo R, Toccafondi G, Coccolini F, La Torre G et al. Recommendations for general surgery activities in a pandemic scenario (SARS-CoV-2). Br J Surg 2020; 10.1002/bjs.11652 [Epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Spinelli A, Pellino G. COVID-19 pandemic: perspectives on an unfolding crisis. Br J Surg 2020; 10.1002/bjs.11627 [Epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Søreide K, Hallet J, Matthews J, Schnitzbauer A, Line P, Lai P. Immediate and long-term impact of the COVID-19 pandemic on delivery of surgical services. Br J Surg 2020; 10.1002/bjs.11670 [Epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. COVIDSurg Collaborative . Global guidance for surgical care during the COVID-19 pandemic. Br J Surg 2020; 10.1002/bjs.11646 [Epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]


