Dear Editor
In the end of 2019, a series of pneumonia cases emerged in China, with clinical presentations greatly resembling viral pneumonia, caused by COVID‐19 or SARS‐CoV‐2. 1
Currently, several clinicians described an increasing number of cases of coronavirus‐positive patients reporting skin problems, either in early stage of infection or as late‐onset manifestation. 2 , 3 , 4
Recently, Dr. Sebastiano Recalcati analysed the cutaneous involvement in 148 COVID‐19 patients hospitalized in the Lecco Hospital, Lombardy, Italy. 5
Among them, 18 patients developed cutaneous involvement with erythematous rash, urticaria and chickenpox‐like vesicles. 5
In the light of these data, in the absence of a related histological analysis, it is not possible to determine whether these clinical manifestations are attributable to direct viral action or to other factors.
We report a patient with a history of COVID‐19 infection and a late‐onset cutaneous eruption, after healing.
A 47‐year‐old auxiliary hospital worker, with a history of hypertension and impaired glucose tolerance, in service at a hospital located in one of the Italian COVID‐19 red zones, had a syncope during his work shift, so urgent CT scan was performed.
The radiological report showed, unexpectedly, pulmonary ground‐glass opacifications, mainly involving the right lower lobe.
Consequently, nasopharyngeal and oropharyngeal swabs were performed for COVID‐19 on 25 March 2020: the tests were positive for SARS‐CoV‐2.
Pertinent laboratory results on admission revealed only elevated RCP (2.11 mg/dL).
Supportive, antibiotic, antiviral and anticoagulant (ceftriaxone, lopinavir/ritonavir, hydroxychloroquine and enoxaparin) care were carried with good clinical response.
Neither high fever nor severe respiratory symptoms were noticed.
Firstly on April 2, and once again on April 4, the control swabs were negative; therefore, given his health status, the patient was discharged from hospital on 8 April 2020.
Four days later, patient reported appearance of persistent, progressive, erythematous and itchy lesions, with craniocaudal displacement.
Symptoms get worse quickly, so he went to E.R. where he was given intravenous steroid and antihistamine agent, with mild benefit.
Blood test revealed an increase in white blood cells (22.27 × 103/μL) especially in neutrophils (19.52 × 103/μL).
Dermatologic consultation revealed multiple, raised erythematous weals, alone or in cluster, some of them with central purple hyperpigmentation, predominantly localized on head, trunk and upper arms (Fig. 1a).
Figure 1.
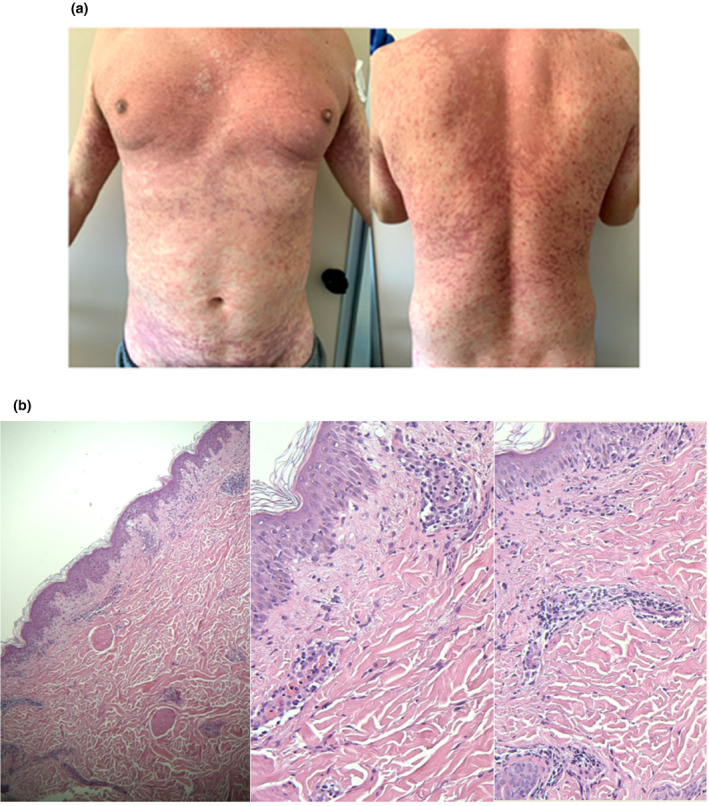
(a) Clinical pictures. (b) Histology pictures.
Patient complained of intense itching.
A diagnosis of suspected urticarial vasculitis has been made.
In an attempt to rule out if this clinical manifestation was linked to viral reactivation, nasopharyngeal and oropharyngeal swabs were executed again, resulting negative for SARS‐CoV‐2.
The blood test for autoimmune disease was negative (ANA, ENA screening, ANCA, antiphospholipid, C3, C4).
Punch biopsy was performed, and histological examination revealed orthokeratotic hyperkeratosis, spongiosis, focal vacuolar degeneration of basal keratinocytes and focal lymphocytic exocytosis. Slight inflammatory lymphomorphonuclear infiltrate of superficial dermis with minimal perivascular neutrophilic component was observed, with occasional aspects of vessel wall damage (Fig. 1b).
Thus, the histopathologic diagnosis of a plausible adverse drug reaction was established.
Therefore, the patient was treated as urticarial vasculitis due to adverse drug reaction with tapering prednisone, bilastine and pantoprazole with prior authorization of diabetes specialist, given the evidence of recent‐onset diabetes mellitus.
After 7 days, patient presented a complete symptom remission.
Currently, cases of different COVID‐19‐related skin manifestations are frequently described. 6 , 7
We recognize the limitations of this single case report; however, further experiences are required to distinguish how often skin involvement is closely related to virus and how frequently it could be related to anti‐COVID‐19 multidrug treatment.
Acknowledgement
The patient in this manuscript has given written informed consent to the publication of his case details.
Funding source
none to declare.
Conflict of interest
none to declare
References
- 1. Huang C, Wang Y, Li X et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet 2020; 395: 497–506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Joob B, Wiwanitkit V. Various forms of skin rash in COVID‐19: a reply. J Am Acad Dermatol 2020; S0190‐9622(20)30612‐5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Estébanez A, Pérez‐Santiago L, Silva E, Guillen‐Climent S, García‐Vázquez A, Ramón MD. Cutaneous manifestations in COVID‐19: a new contribution. J Eur Acad Dermatol Venereol 2020. 10.1111/jdv.16474 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Henry D, Ackerman M, Sancelme E, Finon A, Esteve E. Urticarial eruption in COVID‐19 infection. J Eur Acad Dermatol Venereol 2020. 10.1111/jdv.16472 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Recalcati S. Cutaneous manifestations in COVID‐19: a first perspective. J Eur Acad Dermatol Venereol 2020; 34: e212–e213. [DOI] [PubMed] [Google Scholar]
- 6. Mahé A, Birckel E, Krieger S, Merklen C, Bottlaender L. A distinctive skin rash associated with Coronavirus Disease 2019? J Eur Acad Dermatol Venereol 2020. 10.1111/jdv.16471 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Fernandez‐Nieto D, Ortega‐Quijano D, Segurado‐Miravalles G, Pindado‐Ortega C, Prieto‐Barrios M, Jimenez‐Cauhe J. Comment on: Cutaneous manifestations in COVID‐19: a first perspective, Safety concerns of clinical images and skin biopsies. J Eur Acad Dermatol Venereol 2020. 10.1111/jdv.16470 [DOI] [PMC free article] [PubMed] [Google Scholar]


