A 53-year-old man underwent circumferential endoscopic submucosal dissection (ESD) in our hospital for a superficial esophageal neoplasm 10 cm in circumference and approximately 29 to 39 cm from the incisors. To prevent postoperative esophageal stenosis, we performed implantation of autologous esophageal mucosa with polyglycolic acid (PGA) and placed a temporary stent to fill the artificial ulcer in the esophagus.
The circumferential early esophageal squamous cell carcinoma was treated by ESD. After ESD, we used a Duette kit (HX-20Q-1; Olympus, Tokyo, Japan) to excise several pieces of autologous esophageal mucosal tissue by multiband mucosectomy from a normal esophagus site away from the lesion. These normal sections of mucosa were cut into 3- to 5-mm pieces. They were structured onto an absorbable PGA felt (Neoveil, 100 × 50 × 0.15 mm; Gunze Co, Tokyo, Japan) by absorbable lines (VCP738D; Johnson & Johnson, New Brunswick, NJ, USA). The mucosal side was attached against the PGA felt so that the submucosal side was in contact with the ESD ulcer. Every mucosal patch was separated 1.0 cm vertically and horizontally from the others.
Next, the felt was structured onto a covered metal mesh stent (MTN-SE-S-20/120-A-8/650; Micro-Tech Co, Ltd, Nanjing, China) by absorbable lines (VCP738D; Johnson & Johnson) and then attached to the ulcer surface. The endoscope was put through the stent, and the grasping forceps were passed through the biopsy channel to grasp the distal steel lasso loop of the stent (Figs. 1 and 2; Video 1, available online at www.VideoGIE.org). We also placed an overtube (MD-48618; Sumitomo Bakelite Co, Ltd, Tokyo, Japan) orally before placement of the stent; the overtube facilitated the passage of the stent and protected the digestive mucosa from injury. Finally, the stent was placed at the ulcer surface.
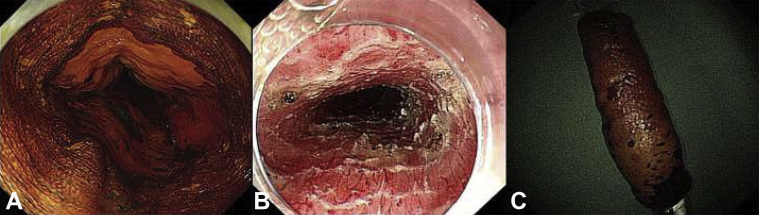
Figure 1.
A, Lugol iodine staining revealed a lesion that was wholly circumferential within the esophageal lumen. B, C, The circumferential endoscopic submucosal dissection resulted in a wholly circumferential mucosal defect.
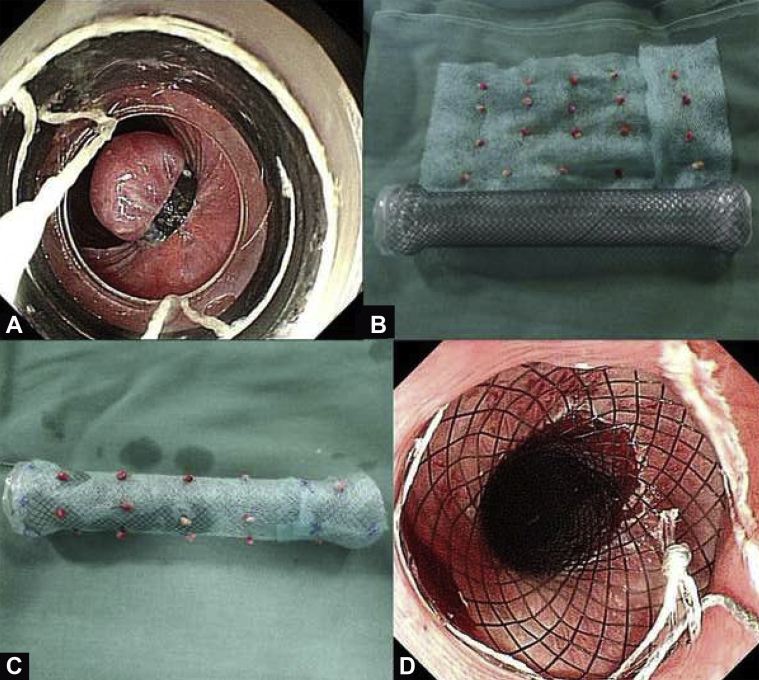
Figure 2.
A, B, C, Normal autologous esophageal mucosae were harvested from the patient and sutured onto the polyglycolic acid (PGA) sheet. Finally, the PGA sheet was sutured onto the fully covered esophageal stent. D, The stent was placed at the location of the artificial ulcer in the esophagus.
After finishing the procedure, we placed a gastric tube. The transplantation procedure took approximately 50 minutes. An R0 resection was achieved, and the specimen was pathologically confirmed to be squamous cell carcinoma.
Outcome
Circumferential ESD and stent implantation were successfully performed in this patient. The patient was hospitalized for 1 week and experienced occasional thoracalgia, which was caused by the stent. The patient was allowed a clear liquid diet on the fourth day after the operation, and the gastric tube was removed on the seventh day after the procedure. The patient underwent endoscopy every week, which showed the stent in place.
The stent was removed 8 weeks after the procedure when the PGA and absorbable lines were totally absorbed. The patient had still not experienced stenosis and dysphagia at 7-month follow-up (5 months after removal of the stent) (Figs. 3, 4, and 5; Video 1, available online at www.VideoGIE.org). No adverse events occurred, including perforation, bleeding, wound infection, or stent migration.
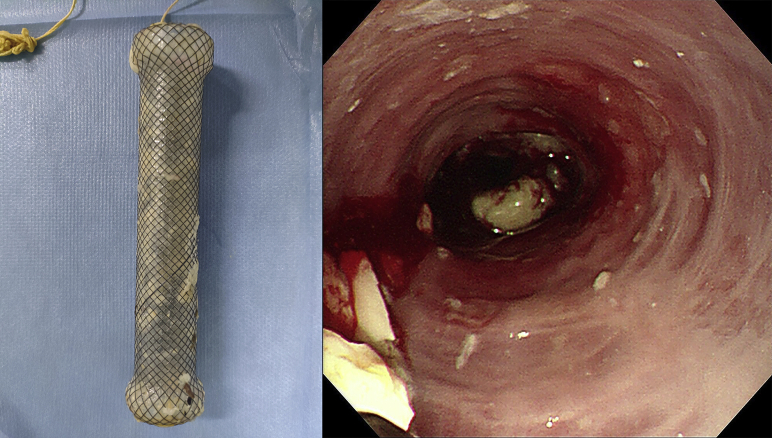
Figure 3.
Endoscopic follow-up every week showed the stent in place.
Figure 4.
The stent was removed 8 weeks after the procedure.
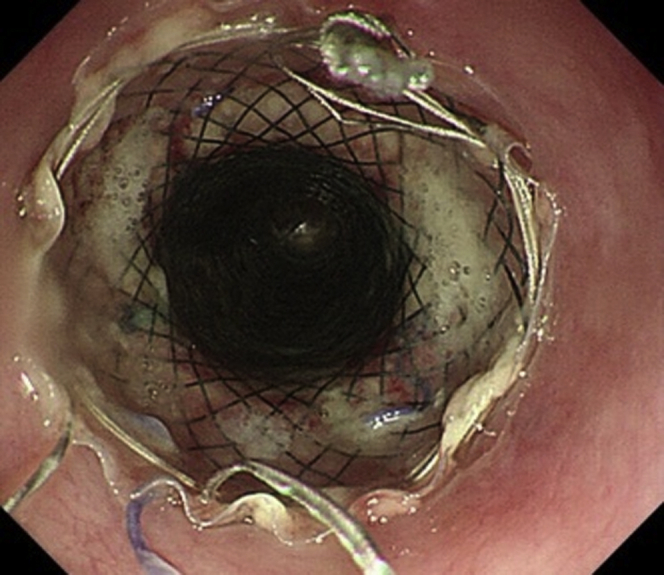
Figure 5.
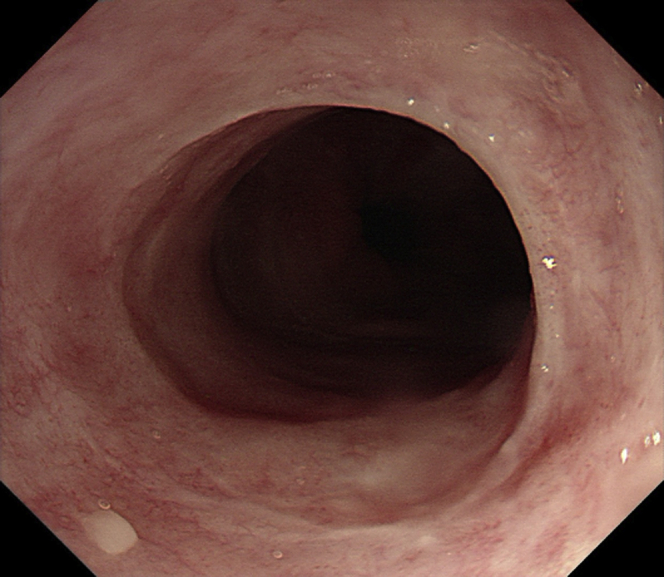
The patient had still not experienced stenosis and dysphagia at 7-month follow-up (5 months after removal of the stent).
The incidence of esophageal stenosis after resection of wholly circumferential lesions ranges from 75% to 100%.1,2 In 2014, Sakaguchi et al3 reported that the use of PGA sheets can reduce the incidence of stricture after circumferential ESD to 37.5%. However, the limitation of this method is that the PGA sheet shifts easily. Ohki et al4 transplanted tissue-engineered autologous oral mucosal epithelial cell sheets by endoscopy. Nevertheless, the fabrication of cell sheets to prevent the formation of strictures after ESD remains technically difficult and costly.
Recently, some researchers reported transplantation of autologous gastric mucosa5 or skin.6 However, the gastric antral mucosa can secrete gastric acid, which may cause symptoms or even ulceration. The skin may secrete sweat.
To the best of our knowledge,6, 7, 8 this is the first reported application of autologous esophageal mucosa with PGA transplantation and temporary stent implantation to prevent post-ESD esophageal stenosis. However, further follow-up of this case is required to determine the long-term efficacy of this technique in preventing postoperative esophageal stenosis.
Informed consent for publication of these images was obtained from the patient.
Disclosure
All authors disclosed no financial relationships.
Acknowledgment
This work is supported by grants from National Key R&D Program of China (2016YFC1302800 and 2016YFC0901402) and the CAMS Innovation Fund for Medical Sciences (CIFMS) (2016-I2M-1-001).
Supplementary data
A case of transplantation of autologous esophageal mucosa with polyglycolic acid and temporary stent implantation.
References
- 1.Ono S., Fujishiro M., Niimi K. Long-term outcomes of endoscopic submucosal dissection for superficial esophageal squamous cell neoplasms. Gastrointest Endosc. 2009;70:860–866. doi: 10.1016/j.gie.2009.04.044. [DOI] [PubMed] [Google Scholar]
- 2.Yu J., Liu Y., Tao Y. Prevention of esophageal stricture after endoscopic submucosal dissection: a systematic review. World J Surg. 2015;39:2955–2964. doi: 10.1007/s00268-015-3193-3. [DOI] [PubMed] [Google Scholar]
- 3.Sakaguchi Y., Tsuji Y., Ono S. Polyglycolic acid sheets with fibrin glue can prevent esophageal stricture after endoscopic submucosal dissection. Endoscopy. 2015;47:336. doi: 10.1055/s-0034-1390787. [DOI] [PubMed] [Google Scholar]
- 4.Ohki T., Yamato M., Ota M. Prevention of esophageal stricture after endoscopic submucosal dissection using tissue-engineered cell sheets. Gastroenterology. 2012;143:582–588.e2. doi: 10.1053/j.gastro.2012.04.050. [DOI] [PubMed] [Google Scholar]
- 5.Hochberger J., Koehler P., Wedi E. Transplantation of mucosa from stomach to esophagus to prevent stricture after circumferential endoscopic submucosal dissection of early squamous cell. Gastroenterology. 2014;146:906–909. doi: 10.1053/j.gastro.2014.01.063. [DOI] [PubMed] [Google Scholar]
- 6.Chai N., Zou J., Linghu E. Autologous skin-grafting surgery to prevent esophageal stenosis after complete circular endoscopic submucosal tunnel dissection for superficial esophageal neoplasms. Am J Gastroenterol. 2019;114:822–825. doi: 10.14309/ajg.0000000000000169. [DOI] [PubMed] [Google Scholar]
- 7.Liao Z., Liao G., Yang X. Transplantation of autologous esophageal mucosa to prevent stricture after circumferential endoscopic submucosal dissection of early esophageal cancer (with video) Gastrointest Endosc. 2018;88:543–546. doi: 10.1016/j.gie.2018.04.2349. [DOI] [PubMed] [Google Scholar]
- 8.Shi P., Ding X. Progress on the prevention of esophageal stricture after endoscopic submucosal dissection. Gastroenterol Res Pract. 2018;2018:1–8. doi: 10.1155/2018/1696849. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
A case of transplantation of autologous esophageal mucosa with polyglycolic acid and temporary stent implantation.