Abstract
Aim
The COVID‐19 pandemic has resulted in society experiencing unprecedented challenges for health care practitioners and facilities serving at the frontlines of this pandemic. With regard to oral cancer, there is a complete absence of literature regarding the long‐term impact of pandemics on patients with oral potentially malignant disorders (OPMDs). The objective of this article is to put forth an institutional multidisciplinary approach for the evaluation and management of OPMDs.
Methods
A multidisciplinary approach was put formalized within our institution to risk stratify patients based on need for in‐person assessment vs telehealth assessment during the COVID‐19 pandemic.
Results
With judicious risk stratification of patients based on clinical features of their OPMD and with consideration of ongoing mitigation efforts and regional pandemic impact, providers are able to safely care for their patients.
Conclusions
The COVID‐19 pandemic has required health care practitioners to make novel decisions that are new to us with development of creative pathways of care that focused on patient safety, mitigation efforts, and clinical management of disease processes. The care of patients with OPMDs requires special considerations especially as patients at high risk for severe COVID‐19 illness are also higher risk for the development of OPMDs.
Keywords: COVID‐19, oral cancer, oral dysplasia, oral leukoplakia, oral potentially malignant disorders
1. INTRODUCTION
The novel coronavirus, severe acute respiratory syndrome coronavirus 2 (SARS‐CoV‐2), is a highly contagious enveloped single stranded sense RNA virus that results in a life‐threatening pulmonary illness known as COVID‐19. 1 Today, the COVID‐19 pandemic has resulted in society experiencing unprecedented challenges for health care practitioners and facilities serving at the frontlines of this pandemic. As health care practitioners, we are implementing measures that aim to mitigate the spread of the virus and to conserve resources including personal protective equipment (PPE) while still caring for patients. Currently, the majority of the mandates on health care practitioners have been to stratify patients based on risk for severe illness per the Centers for Disease Control and Prevention (CDC) guidelines (Figure 1) while also considering the necessity for patients to be evaluated in‐person in the outpatient setting and to assess the “urgency” of any surgical procedure(s) to be performed. 2
FIGURE 1.
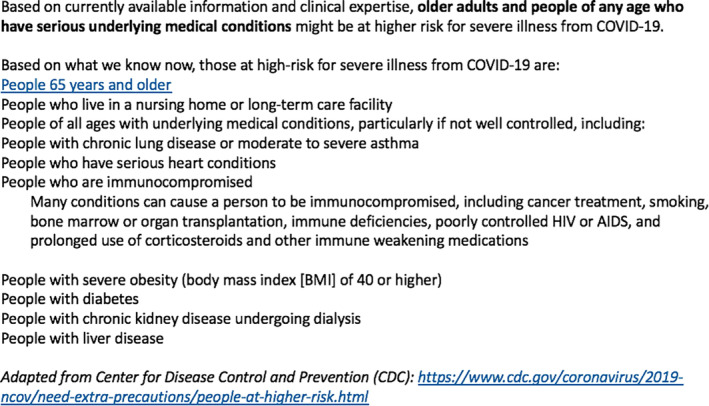
Centers for Disease Control and Prevention (CDC) categories of individuals at high risk for severe illness from COVID‐19 [Color figure can be viewed at wileyonlinelibrary.com]
Irrespective of the nature of any health care crisis, patients suffering from cancer always receive significant attention due to the morbidity and mortality rate associated with cancer, which is the leading cause of death in countries with developed economies. 3 Today, there is a paucity of literature on the impact of pandemics on the progression/evolution of cancer with most of the literature being devoted to the impact of viral illness on patients with cancer. 4 For example, Chemaly et al published a multicenter study evaluating the impact of the 2009 H1N1 influenza pandemic on adult patients with solid tumors and reported a mortality rate of 9.5% in these patients in comparison to the global mortality rate, which was 0.001% to 0.007%. 4 With regard to oral cancer, there is a complete absence of literature regarding the long‐term impact of pandemics on patients with oral potentially malignant disorders (OPMDs) and early‐stage oral cancer. Therefore, for practitioners who manage OPMDs and oral cancer, a great concern is the risk of progression of these lesions and the detriments patients will incur in the long term. Prior to this pandemic, even with readily available access for the majority of patients to a fully intact health care infrastructure, less than 50% of patients with oral cancer were diagnosed at an early stage. 5 Such concerns for delays in diagnosis and care of patients with oral cancer have been extensively addressed in the medical literature in the pre‐COVID‐19 era. Murphy et al reported that 25% of patients with head and neck cancer in the United States experienced treatment delay. 6 Furthermore, an increase in the time to treatment initiation (TTI) by 46 to 52 days resulted in an increased risk of death with the most detrimental impact once TTI extends beyond 60 days. 6 Therefore, early diagnosis and early time to treatment are mainstays for the care of patients with oral cancer to reduce such adverse outcomes, with the most opportune time to prevent and treat oral cancer in its earliest stage through the methodical evaluation and management of OPMDs.
OPMDs are a heterogeneous group of lesions with varying clinical features, risk factors, biologic behavior, and malignant transformation rates (Figure 2A,B).4, 5 It is estimated that OPMDs affect about 2% of the world's population, with a combined malignant transformation rate of 7.9%.7, 8 Herein, we describe a collaborative and multidisciplinary (oral and maxillofacial surgery, otorhinolaryngology, and oral medicine) perspectives on our approach for the evaluation and management of OPMDs during the COVID‐19 pandemic.
FIGURE 2.
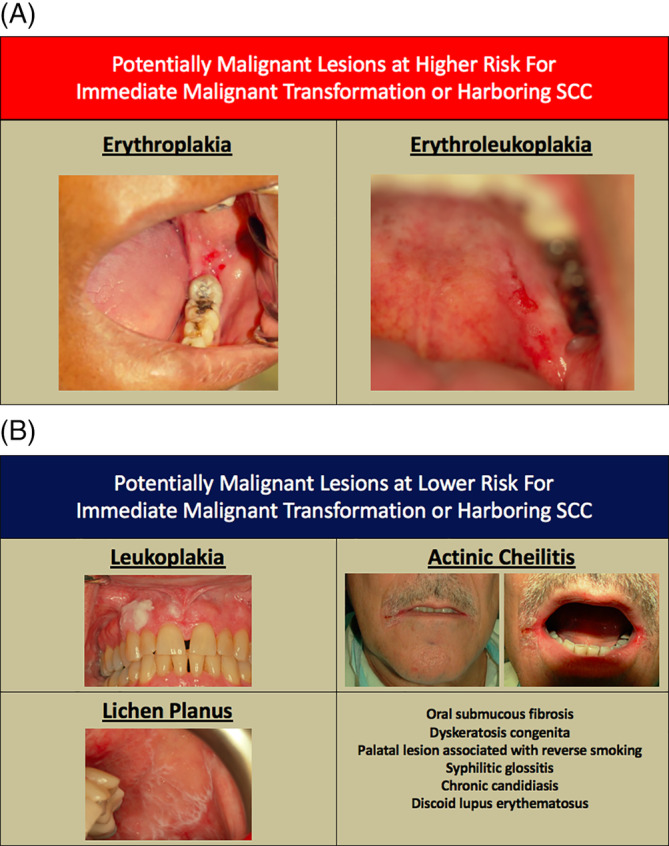
Clinical photographs of lesions considered high risk, A, and low risk, B, for immediate malignant transformation or harboring oral squamous cell carcinoma (OSCC) [Color figure can be viewed at wileyonlinelibrary.com]
1.1. Considerations for the evaluation of new and established patients
The emerging data on COVID‐19 pandemic clearly identify that the presence of comorbidities (ie, diabetes, hypertension, cardiac disease, and pulmonary disease) are responsible for a significantly greater risk of mortality. 9 Similarly, chronic diseases have been identified to be more common in patients with OPMDs; for instance, dyslipidemia and asthma have been identified as being more prevalent in patients with oral leukoplakia in comparison to case‐controls. 10 Furthermore, elderly patients (≥75 years of age) who develop oral leukoplakia have a higher 5‐year cumulative incidence (3.21%) for the development of oral cancer. 5 Tobacco use has also been identified in increasing the risk for adverse events in patients with COVID‐19. 11 Such data is additionally troubling with regard to patients with OPMDs and oral cancer as tobacco use is the main risk factor for the development of the majority of cases of OPMDs and oral squamous cell carcinoma. Similarly, the CDC also considers immunosuppressed patients at being high risk for serious illness from COVID‐19 including patients with “prolonged use of corticosteroids and other immune weakening medications” (Figure 1). 2 This is also concerning for patients with severe cases of oral lichen planus with long‐standing systemic corticosteroid use, or other immunosuppressing agents (eg, tacrolimus, cyclosporine, azathioprine, mycophenolate mofetil, cyclophosphamide, or methotrexate). Therefore, one must consider the patient's risk in developing severe illness with COVID‐19 in deciding the timing of their in‐person evaluation. Additionally, a major part of mitigation efforts surrounding the COVID‐19 pandemic have been focused on social distancing and decreased patient visits to health care facilities unless medically necessary. This is for the benefits of patients and health care professionals, as health care workers represent anywhere from 3.8% to 20% of infected individuals, with approximately 15% developing severe illness or death. 12 The specific impact on oral health providers has yet to be identified, but based on the aerosolization involved with assessing the oral cavity and performing invasive procedures within the oral cavity, one must seriously consider the higher risk of exposure for oral health providers as well as the patients.
In order to reduce density of patients within a health care facility we have incorporated Telehealth into our daily office workflow for the evaluation of new patients with oral mucosal lesions and re‐evaluation of known patients with OPMDs. While the convenience and social distancing afforded by Telehealth are well aligned with ongoing mitigation efforts, the limitations of Telehealth in the evaluation of oral mucosal lesions become readily apparent, such as, the inability to address the texture of a lesion, clearly delineate the borders of a lesion, and evaluate for the presence of an endophytic component to a lesion. Therefore, the use of Telehealth in the evaluation and management of oral mucosal lesions is best suited for easily visible lesions (ie, lip, tip of tongue, and anterior facial gingiva of the maxilla or mandible) and is significantly limited in other locations of the oral cavity (ie, lingual gingiva of mandible, posterior floor of mouth, maxillary vestibule, and mandibular vestibule). From our experience thus far, Telehealth plays an instrumental role in triaging patients and minimizing the number of visits to the clinic for both new and established patients (Figure 3). Below are individual considerations that we are currently employing in the evaluation of new and established patients that are summarized in Figure 3.
FIGURE 3.
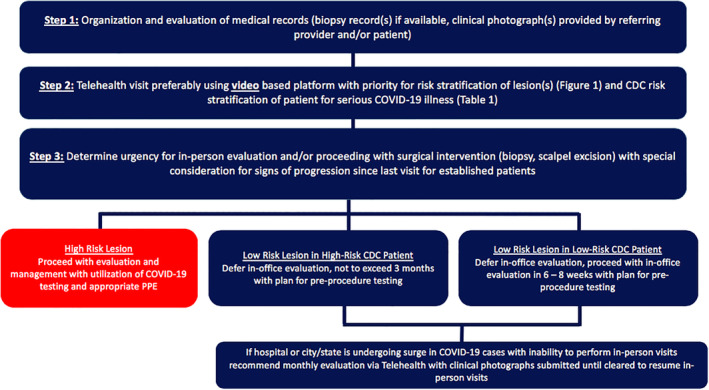
Pathway of care for the evaluation and management of new and established patients with oral potentially malignant disorders (OPMDs) during the COVID‐19 pandemic [Color figure can be viewed at wileyonlinelibrary.com]
1.2. New and established patient evaluation
Acquisition of medical and dental records: Key records to obtain are clinical photographs (ideally from referring provider) and/or photographs provided by the patient (Figure 3) of the lesion(s) of interest; copy of biopsy report(s).
Telehealth consultation: This ideally should be video‐based, and at our institution, we are currently utilizing BlueJeans (Mountain View, California) and Doximity (San Francisco, California) as video conferencing platforms. A greater amount of details is obtained in assessing a lesion via a photograph(s) than through video conferencing; however, through video a greater spatial appreciation of a lesion is achieved and better assessment for cervical lymphadenopathy through video, which adds a greater degree of human touch to the visit.
Determine urgency/timing of in‐person visit: This decision is the most critical decision as one must balance social mitigation efforts, reducing exposure risks to patients especially those deemed as high risk per CDC, and also providing medically appropriate care. The timing of an in‐person visit is largely predicated on the likelihood of lesion being cancer (Figure 2A,B) and ongoing mitigation efforts and surge capacity. One of the most critical considerations from a clinical perspective is the progression (development of symptoms and/or taking on high‐risk clinical features; Figure 4) of the lesion of interest. Any clinical indications for progression must escalate care and proceed with in‐person evaluation. Should an institution lacks the resources or capacity for care of the patient, then collaboration with colleagues with familiarity and resources to care for a patient with a OPMD will become necessary. We cannot overemphasize the importance of absence or presence of progression of a lesion in part of this algorithm.
FIGURE 4.

Clinical parameters of a lesion that impact risk for malignant transformation [Color figure can be viewed at wileyonlinelibrary.com]
Of note, our rational for the use of the 3‐month time point in low‐risk lesions is based on literature that indicates 0.7% of patients with oral leukoplakia who go on to develop oral squamous cell carcinoma do so within 3 months of diagnosis. 5
1.3. Considerations for necessary oral mucosal procedures
From a health care professional exposure perspective, oral‐based examinations and procedures are of great concern. Per the CDC, “potential routes of close‐range transmission include splashes and sprays of infectious material onto mucous membranes and inhalation of infectious virions exhaled by an infected person. The relative contribution of each of these is not known for SARS‐Co‐V‐2.” 13 Furthermore, there is mounting evidence that SARS‐CoV‐2 may be transmitted through fomites and contact. 14 An oral health professionals points of contact during a patient interaction could be both direct and indirect, including but not limited to the following: (a) contact with human fluids, (b) contaminated surfaces and instrumentation, and (c) patient materials. 14 While strict hygiene measures are able to significantly reduce the risk of exposure from indirect routes, due to the contact with oral mucosal surfaces in the assessment of an OPMD and need to violate oral mucosal surfaces should an incisional or excisional biopsy become necessary, one must incorporate added protective measures to ensure the safety of the entire health care team. Below is a summary of such measures:
PPE: Conservation of PPEs has been one of the hallmarks of this pandemic. Our approach has been to use a level 3 surgical mask with face shield and/or goggles during the in‐person evaluation of a patient who is known to be SARS‐CoV‐2 negative based on testing within 24 hours. If the patient was unable to be tested or should the patient present for a surgical procedure, then a higher level of PPE is employed (N95, face shield, disposable medical safety gown, and disposable working cap).
SARS‐CoV‐2 testing: Globally testing continues to be a major challenge of this crisis; however, it is becoming more readily available. It is our recommendation that should a patient require a biopsy or surgical excision of their OPMD, testing be obtained within 24 hours of the planned procedure with consideration for the aforementioned PPE options. With regard to testing stewardship, this is where Telehealth evaluation allows for optimization of the efficiency of the in‐person visit. For instance if a patient requires a biopsy/surgical excision the testing is obtained prior to the visit with allocation for the necessary PPE. Additionally, during the Telehealth visit we address any medications or conditions that require special considerations (ie, management of antiplatelet agents/anticoagulants) and obtaining any necessary “clearances” to avoid any complicating factors and cancelation of procedures and need for the patient to return to the office.
Topical preparation of oral mucosal surfaces with povidone‐iodine (PVP‐I): Based on mounting evidence of the ability of PVP‐I to inactive SARS coronavirus prior to the biopsy or resection of an oral mucosal lesion we are currently topicalizing the oral mucosal surfaces with PVP‐I (1%‐7.5%) for 2 minutes prior to delivering local anesthesia and performing tissue excision. 15
Technical considerations for tissue handling: For incisional biopsies, our recommendation is for use of either a surgical scalpel or a tissue biopsy technique with avoidance of use of laser technologies due to concern for viral disease transmission by laser‐generated plume until more robust testing guidelines are established. Furthermore, our recommendation is for the use of absorbable sutures to avoid risk of bleeding from an open biopsy wound with return of patient to the office or having to visit an emergency department secondary to bleeding. Additional benefit of absorbable sutures is patients do not have to return for suture removal. Furthermore, should patient require excision of lesion in the operating room we are minimizing use of smoking‐generating cautery to minimize vaporization of viral particles.
Procedure setting: If the patient is SARS‐CoV‐2 negative, it is appropriate for the procedure to be performed in the outpatient clinic setting if the lesion is easily accessible. However, if the patient's SARS‐CoV‐2 status is unknown and a biopsy is warranted, our preference is to perform the procedure in the clinic setting. However, if a critical biopsy is necessary and in the absence of testing and if the lesion is difficult to access (secondary to location or other factors such as trismus) our preference is to perform the procedure in the operating room. Should the patient require the procedure in the operating room, preference should be given to excision of lesion in its entirety with/without use of frozen sections prior to lesion excision based on the specialists preference.
2. CONCLUSION
The COVID‐19 pandemic has required health care practitioners to make novel decisions that are new to us with development of creative pathways of care that focused on patient safety, mitigation efforts, and clinical management of disease processes. The care of patients with OPMDs requires special considerations especially as patients at high risk for severe COVID‐19 illness are also higher risk for the development of OPMDs.
Shanti RM, Stoopler ET, Weinstein GS, et al. Considerations in the evaluation and management of oral potentially malignant disorders during the COVID‐19 pandemic. Head & Neck. 2020;42:1497–1502. 10.1002/hed.26258
REFERENCES
- 1. Wu F, Zhao S, Yu B, et al. A new coronavirus associated with human respiratory disease in China. Nature. 2020;579(7798):265‐269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Centers for Disease Control and Prevention . Coronavirus Disease 2019 (COVID‐19); 2020. https://www.cdc.gov/coronavirus/2019-ncov/need-extra-precautions/people-at-higher-risk.html. Accessed April 29, 2020.
- 3. Gorji HA, Jafari H, Heidari M, Seifi B. Cancer patients during and after natural and man‐made disasters: a systematic review. Asian Pac J Cancer Prev. 2018;19(10):2695‐2700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Chemaly RF, Vigil KJ, Saad M, et al. A multicenter study of pandemic influenza A (H1N1) infection in patients with solid tumors in 3 countries: early therapy improves outcomes. Cancer. 2012;118(18):4627‐4633. [DOI] [PubMed] [Google Scholar]
- 5. Yanik EL, Katki HA, Silverberg MJ, et al. Leukoplakia, oral cavity cancer risk, and cancer survival in the U.S. elderly. Cancer Prev Res. 2015;8(9):867‐963. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Arduino PG, Bagan J, El‐Naggar AK, et al. Urban legends series: oral leukoplakia. Oral Dis. 2013;19(7):642‐659. [DOI] [PubMed] [Google Scholar]
- 7. Iocca O, Sollecito TP, Alawi F, et al. Potentially malignant disorders of the oral cavity and oral dysplasia: a systematic review and meta‐analysis of malignant transformation rate by subtype. Head Neck. 2020;42(3):539‐555. [DOI] [PubMed] [Google Scholar]
- 8. Murphy CT, Galloway TJ, Handorf EA, et al. Survival impact of increasing time to treatment initiation for patients with head and neck cancer in the United States. J Clin Oncol. 2016;34(2):169‐178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Singh AK, Gupta R, Misra A. Comorbidities in COVID‐19: outcomes in hypertensive cohort and controversies with renin angiotensin system blockers. Diabetes Metab Syndr. 2020;14(4):283‐287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Giudice LW, Graff EA, Haripersad Y, et al. Chronic disease comorbidity in patients with oral leukoplakia: a matched case‐controls tudy. Oral Dis. 2020. 10.1111/odi.13315. [DOI] [PubMed] [Google Scholar]
- 11. Vardavas CI, Nikitara K. COVID‐19 and smoking: a systematic review of the evidence. Tob Induc Dis. 2020;18. 10.18332/tid/119324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Kowalski LP, Sanabria A, Ridge JA, et al. COVID‐19 pandemic: effects and evidence‐based recommendations for otolaryngology and head and neck surgery practice. Head Neck. 2020. 10.1002/hed.26164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Centers for Disease Control and Prevention . Coronavirus Disease 2019 (COVID‐19); 2020. https://www.cdc.gov/coronavirus/2019-ncov/hcp/infection-control-faq.html. Accessed April 29, 2020.
- 14. Peng X, Xu X, Li Y, Cheng L, Zhou X, Ren B. Transmissin routes of 2019‐nCoV and controls in dental practice. Int J Oral Sci. 2020;12(1):9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Kariwa H, Fujii N, Takashima I. Inactivation of SARS coronavirus by means of povidone‐iodine, physical conditions and chemical reagents. Dermatology (Basel). 2006;212(suppl 1):119‐123. 10.1159/000089211. [DOI] [PMC free article] [PubMed] [Google Scholar]


