The outbreak of coronavirus disease 2019 (COVID‐19) in December 2019 in Wuhan, China, rapidly became a pandemic across the world, including the USA. Since March 2020, we started to receive peripheral blood smear review consults for patients who were admitted with COVID‐19. We reviewed 15 peripheral blood smears from the 15 most recently admitted patients Table I. These patients ranged in age from 26 to 90 years and included eight males and seven females. The reasons for peripheral blood smear consult were primarily concerns for haemolysis (nine of the 15 cases), followed by anaemia, thrombocytopenia and pancytopenia.
Table I.
Full blood count of the 15 patients with COVID‐19 accompanying the blood smear review in Fig 1.
| ID no. | Age, years |
Location/ disposition |
% atypical Lympho. | WBC, K/μl | RBC, M/μl | Hb, g/l | Hct, % | MCV, fl | MCH, pg | MCHC,% | RDW, % | PLT, K/μl | MPV, fl | Absolute neutrophil, K/μl | Absolute lymphocyte, K/μl | Absolute monocyte, K/μl | Absolute eosinophil, K/μl | Absolute basophil, K/μl |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 72 | ICU | 10 | 16 | 2·03 | 68 | 21·6 | 106 | 33·5 | 31·5 | 14·6 | 287 | 11·2 | 11·4 | 3 | 0·2 | 0·2 | 0·2 |
| 2 | 43 | Medicine Floor | 0·5 | 3·9 | 2·93 | 83 | 27·5 | 94 | 28·3 | 30·2 | 12·1 | 228 | 10·6 | 1·8 | 1·5 | 0·5 | 0 | 0 |
| 3 | 37 | ED | 14 | 7·5 | 4·45 | 118 | 35·4 | 80 | 26·5 | 33·3 | 15·6 | 73 | 12·6 | 6·2 | 0·7 | 0·4 | 0 | 0·1 |
| 4 | 66 | ICU | 9 | 14·6 | 2·36 | 71 | 24·5 | 104 | 30·1 | 29 | 16·9 | 407 | 11·2 | 11·1 | 0·6 | 2 | 0 | 0·1 |
| 5 | 68 | ICU | 2 | 10·6 | 2·41 | 71 | 22·3 | 92 | 29·5 | 31·8 | 13·7 | 232 | 11 | 8·8 | 1 | 0·7 | 0·1 | 0 |
| 6 | 54 | ICU | 13·5 | 13·5 | 2·58 | 73 | 23·1 | 90 | 28·3 | 31·6 | 16·4 | 229 | 11·1 | 11·2 | 0·5 | 1·1 | 0·1 | 0·1 |
| 7 | 58 | Medicine Floor | 12 | 8·4 | 5·7 | 166 | 49·1 | 86 | 29·1 | 33·8 | 12·9 | 315 | 10·7 | 6·4 | 1·5 | 0·5 | 0 | 0 |
| 8 | 75 | ICU | 6 | 9·6 | 3·73 | 108 | 29·8 | 80 | 29 | 36·2 | 15 | 144 | 10·9 | 8 | 1·1 | 0·3 | 0·1 | 0 |
| 9 | 42 | ICU | 4 | 23·7 | 2·56 | 78 | 24·5 | 96 | 30·5 | 31·8 | 15·8 | 158 | 12·9 | 20·4 | 1·2 | 2·1 | 0 | 0 |
| 10 | 65 | ICU | 9 | 18·8 | 2·96 | 74 | 24·5 | 83 | 25 | 30·2 | 18·2 | 443 | 11·7 | 15·6 | 1·5 | 1·7 | 0 | 0 |
| 11 | 70 | Medicine Floor | 6 | 2·3 | 5·56 | 125 | 41·9 | 75 | 22·5 | 29·8 | 16·7 | 76 | N/A | 1·6 | 0·5 | 0·2 | 0·1 | 0 |
| 12 | 26 | Medicine Floor | 3 | 1·6 | 3·46 | 107 | 31·9 | 92 | 30·9 | 33·5 | 12·8 | 207 | 10·3 | 0·8 | 0·4 | 0·4 | 0 | 0 |
| 13 | 90 | ICU | 4 | 17·1 | 4·2 | 113 | 35·7 | 85 | 26·9 | 31·7 | 16·7 | 65 | N/A | 15·7 | 0·5 | 0·3 | 0 | 0 |
| 14 | 54 | Medicine Floor | 10 | 1·9 | 2·65 | 84 | 24·4 | 92 | 31·7 | 34·4 | 11·9 | 122 | 10·7 | 1·3 | 0·2 | 0·2 | 0 | 0 |
| 15 | 72 | ICU | 0 | 4 | 3·94 | 117 | 34·7 | 88 | 29·7 | 33·7 | 12·2 | 97 | 9·5 | 2·2 | 1·5 | 0·2 | 0 | 0 |
Hb, haemoglobin; Hct, haematocrit; ICU, intensive care unit; ID, identification; MCH(C), mean corpuscular Hb (concentration); MCV, mean corpuscular volume; MPV, mean platelet volume; RBC, red blood cell; PLT, platelets; RDW, red cell distribution width; WBC, white blood cell.
Most of the patients showed normocytic anaemia with mild anisopoikilocytosis. None of the reviewed cases showed morphological evidence of haemolysis, regardless of their clinical presentation. Seven patients had neutrophilia and two had neutropenia, while the neutrophil counts were normal in six patients. The lymphocyte count was at a lower normal range in eight patients (normal range 1·0–4·0 K/μl) and seven patients had lymphopenia. Besides these findings, the most common observation was the presence of atypical lymphocytes in most of the smears (14/15, 93·3%). These lymphocytes are medium to large in size with loosely condensed chromatin, and moderate to deep basophilic cytoplasm Fig 1A. Some of these cells demonstrate plasmacytoid morphology with eccentric nuclei and perinuclear hof Fig 1B. Some show visible nucleoli resembling immunoblasts Fig 1C. The atypical lymphocytes comprised 6·94 ± 4·30% of the total lymphocytes Fig 1D. It appears that the percentage of atypical lymphocytes in total lymphocytes does not correlate with the severity of the disease Table I. Additionally, two cases of bronchial alveolar lavage smears from two patients (no accompanying blood smear review) were reviewed due to the presence of numerous atypical lymphocytes with the same morphology as those found in the blood smear Fig 1E.
Fig 1.
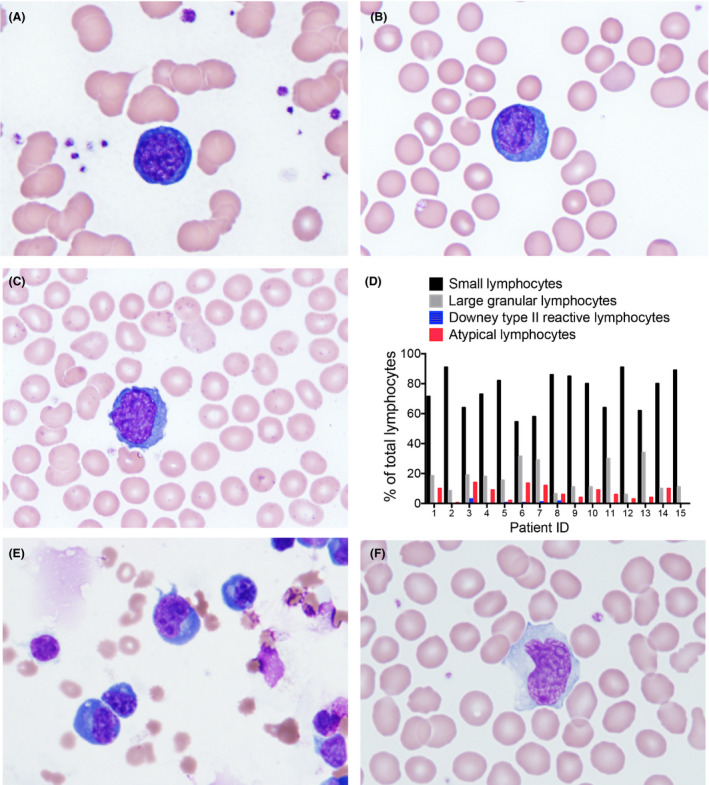
Atypical lymphocytes in patients with COVID‐19. (A–C) Wright‐Giemsa stained peripheral blood smear showing representative forms of atypical lymphocytes observed in 15 cases of smear review (×100). (D) Percentages of indicated lymphocytes out of total lymphocytes in the patients with COVID‐19. Differential count of the indicated lymphocytes was performed; 200 lymphocytes were counted in each patient. (E) Wright‐Giemsa stained bronchial alveolar lavage smear from a patient with COVID‐19 (×60). (F) Wright‐Giemsa stain of the peripheral blood smear from a patient with infectious mononucleosis caused by Epstein–Barr virus infection (×100).
These atypical lymphocytes are likely reactive to severe acute respiratory syndrome coronavirus 2 (SARS‐CoV‐2) infection. Their morphology is different from Downey type II reactive lymphocytes Fig 1F that are commonly seen in other viral infections such as Epstein–Barr virus. In our reviewed 15 patients, Downey type II reactive lymphocytes were seen, but with a much lower frequency (0·50 ± 0·85% of the total lymphocytes). Additionally, lymphopenia is frequently seen in SARS and influenza and in both diseases has been recognised as a negative predictor of outcomes. 1 , 2 . However, presence of atypical lymphocytes is not a laboratory feature of influenza. 3 The relative commonality of these cells compared to other viral infections, together with lymphopenia observed in many patients, may provide an important clue to further evaluate patients for COVID‐19. Future studies in the characterisation of these cells could be helpful in our understanding of the pathophysiology of the disease.
Acknowledgements
This work was partially supported by National Institute of Diabetes and Digestive and Kidney Diseases (R01 DK124220) and National Heart, Lung and Blood Institute (R01 HL148012). Peng Ji is a scholar of the Leukemia and Lymphoma Society and the Harrington Discovery Institute.
References
- 1. He Z, Zhao C, Dong Q, Zhuang H, Song S, Peng G, et al. Effects of severe acute respiratory syndrome (SARS) coronavirus infection on peripheral blood lymphocytes and their subsets. Int J Infect Dis. 2005;9:323–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Mendez R, Menendez R, Amara‐Elori I, Feced L, Piro A, Ramirez P, et al. Lymphopenic community‐acquired pneumonia is associated with a dysregulated immune response and increased severity and mortality. J Infect. 2019;78:423–31. [DOI] [PubMed] [Google Scholar]
- 3. Cunha BA, Connolly JJ, Irshad N. Are atypical lymphocytes present with viral influenza‐like illnesses (ILIs) in hospitalized adults? Eur J Clin Microbiol Infect Dis. 2016;35:1399–401. [DOI] [PubMed] [Google Scholar]


