Summary
During the UK’s COVID‐19 pandemic lockdown there was national guidance to suspend routine dermatology work. As a consequence, over 800 patient appointments in a district general dermatology department were temporarily suspended. Remote consultations were carried out to triage and manage referrals, via telephone or video consultations. Data were prospectively recorded on 488 patient interactions. Outcomes included advice/treatment, discharge, surgery or clinic review; 25% of patients were either uncontactable or their problem had resolved. Over a third of referrals were discharged with advice/treatment initiated remotely; 56% of referred dermatoses required further clinical review; 25% of lesion referrals were booked directly to surgery. This process was time‐intensive for the clinicians involved, and triage mechanisms could be improved. Sufficient referral information allows remote diagnosis; implementation of management plans and appropriate discharge of patients. This process has been shown to be feasible, and may be a temporary solution for other COVID‐19 impacted dermatology departments.
When the UK entered lockdown in March 2020 amidst the COVID‐19 pandemic, routine dermatology work was suspended as per national guidance1 to allow for redeployment of staff to the front line and also to reduce risk of patient exposure and travel.
New patient referrals from primary care into dermatology services usually enter via one of three routes: (i) the 2‐week wait (2WW) for suspected serious skin malignancies, (ii) routine nonurgent cases and (iii) emergency referrals (via an on‐call service). All these patients are assessed via a face‐to‐face (F2F) consultation after various waiting times, depending on their urgency.
As a result of this suspension, just over 800 new routinely referred patients had their appointments temporarily suspended, covering a 6‐week period. Many of these patients had already waited up to 18 weeks for an initial assessment. Furthermore, with the dual challenge of a depleted dermatology workforce and the need for reduced F2F consultations during the lockdown, it became imperative to develop new solutions to ensure that this cohort of patients would receive care within an appropriate timeframe.
To evaluate our response to this challenge, we prospectively collected data, with the aim of investigating whether the strategy deployed was an efficient way of assessing this large number of referred patients. In this paper, we also initiate discussion as to whether this novel method of working could yield a framework for providing a future dermatology service in the event of prolonged social distancing.
Report
The national Electronic Booking System (ESR) identified the 816 routinely referred patients whose appointments were cancelled, between the dates of 23 March and 30 April 2020. This patient worklist was divided between 15 clinicians (consultants, associate specialists and registrars) working in the department, including those shielding at or working from home.
Referral letters were reviewed and patients were contacted via telephone or video calling (the Attend Anywhere platform; www.attendanywhere.com). For telephoned patients, each clinician decided if patient photographs would be useful. If so, the patient was directed to send good‐quality images to a secure National Health Service (NHS) email account. Follow‐up contact was made with the patient to relay the diagnosis and describe any further management required. A patient was deemed to be ‘uncontactable’ if they did not respond to three telephone calls on three separate occasions.
Data collected included patient demographics, whether the referral was for a lesion or dermatosis, if a visual element was used in assessing the case (photo or video consultation) and the clinicians’ opinion as to who could have made the first contact with the patient (doctor, nurse or administrator) to streamline any future processes. Outcomes recorded included urgent review, direct booking for nonurgent surgery, routine clinic review (with/without management initiated) and direct discharge (with/without treatment). In addition, opinions were gathered from the clinicians involved, to assess this system as a future method of working and to judge what elements were most or least effective.
Data were available for 488 patients contacted over the 2‐week period. Of these, 229 were referred with a dermatosis and 259 with a lesion. For 52 individuals the problem had resolved and they were discharged. A further 72 were uncontactable and were sent a standardized letter to arrange a re‐booking, if the patient felt it was required. These two groups comprised 25% (n = 124) of the total referrals. Over a third of referrals were discharged with advice/treatment initiated remotely.
Of the 259 lesions referred, 32 had received prior in‐house teledermatology advice and, of these, it was felt 17 could have been directly booked to surgery. Where requested, 118 (45.6%) were assessed by imaging (via emailed photograph or video consultation), while 22 (8.5%) patients were unable to provide imaging, either because of inability due to body location (e.g. scalp/back) or lack of equipment/capability. Of these 22 patients, 18 required clinical review.
For all lesion referrals, 88 patients (34.0%) were discharged after advice and/or treatment, and 129 (49.8%) were given advice and/or topical treatment and booked for clinical review or surgery. There were 66 (25.5%) lesions booked directly to surgery; of these, 52 were for routine surgery, 10 were for Mohs assessment and 4 were expedited on to the 2WW pathway (Fig. 1).
Figure 1.
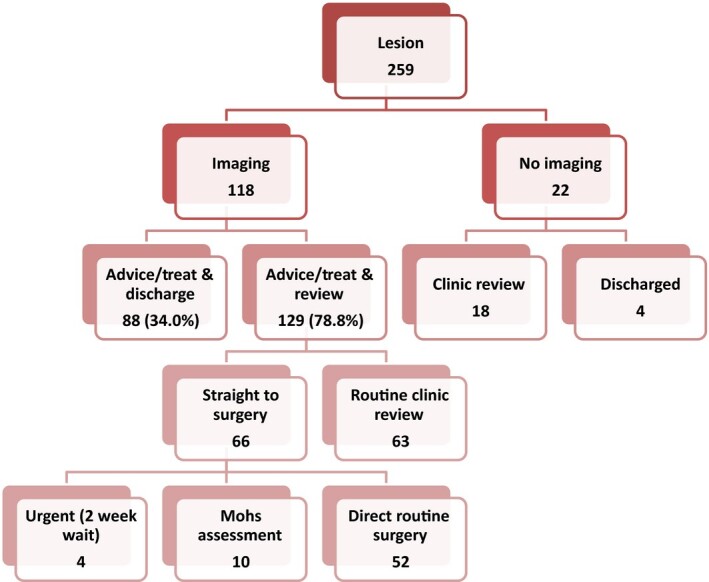
Outcomes for referred lesions.
Of the 229 dermatoses referred, 64 (27.9%) had imaging available. With imaging for assessment, 23 (35.9%) were discharged following advice and/or treatment, 34 (53.1%) were given advice and/or treatment and booked for clinic review and 7 (10.9%) were given open access, if needed.
Of the dermatoses without imaging available (n = 165), following advice and/or treatment, 47 (28.5%) patients were discharged, 96 (58.2%) were booked for clinic review, and 22 (13.3%) were given open access, if needed. In total, 56% of referred dermatoses required further clinical review (Fig. 2).
Figure 2.
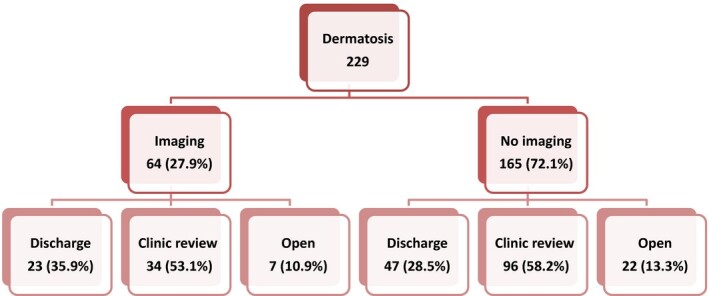
Outcomes for referred dermatoses.
The overall feedback from clinicians was positive, as it was felt a large proportion of referrals were pragmatically, safely and effectively managed through remote consulting (Fig. 3). Just over a third of patients were discharged with advice/treatment given, reducing the need for further outpatient clinic appointment slots. One clinician largely used video consulting, predominantly for dermatoses, negating the need for repeat calls and emails for photographs, and reported high patient satisfaction. A future review of patient satisfaction with this process is required to compare this process with our standard practice.
Figure 3.
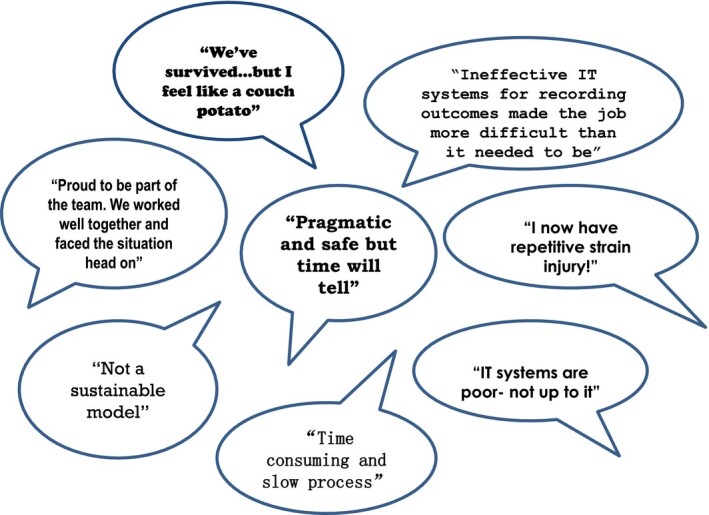
Feedback from clinicians.
Limitations encountered include variation in opinions between clinicians, and also that data could only be collected within an acceptable timeframe for 488 out of the 816 referrals.
This process was felt to be time‐consuming by clinicians. Alternatively, administrative staff could triage the referrals, and arrange with the patient or referring general practitioner to submit the necessary images ahead of the clinician call. Otherwise, a standardized letter, email or multimedia message could be sent to patients to request that they send their own images to an appropriate platform, prior to their remote consultation. Inevitably, there will be some patients without the knowledge or capabilities to do this, as for video calls.
Managing new patient referrals via remote consulting is set to remain in place for the near future, and possibly longer for vulnerable patient groups during the COVID‐19 pandemic. Reflection on our performance and actions taken at this stage will enable us to institute immediate improvements to address this challenge. We look forward to a broader national and international discussion on strategies for managing the challenges faced both by dermatology and the wider healthcare service.
Learning points.
Remote consultations are an effective process to manage a large volume of referrals efficiently and reduce the need for F2F clinic appointments.
Patients were receptive to remote dermatology consultations.
Patient‐sourced photographs of lesions were mostly sufficient to allow diagnosis, advice and/or treatment and/or booking of surgery.
The majority of lesions assessable by imaging and requiring surgical intervention were booked directly from remote consultation, removing the need for an additional clinic appointment prior to surgery.
Arrangement for images to be submitted ahead of a clinician’s call, via administrative staff, a standardized letter, email or multimedia message would improve time management.
Video consulting may be especially useful for assessment of dermatoses.
Contributor Information
E. Corden, Department of Dermatology Portsmouth Hospitals NHS Trust Portsmouth Hampshire UK.
A. K. Rogers, Department of Dermatology Portsmouth Hospitals NHS Trust Portsmouth Hampshire UK
W. A. Woo, Department of Dermatology Portsmouth Hospitals NHS Trust Portsmouth Hampshire UK
R. Simmonds, Faculty of Science School of Pharmacy and Biomedical Sciences University of Portsmouth Portsmouth Hampshire UK
C. D. Mitchell, Department of Dermatology Portsmouth Hospitals NHS Trust Portsmouth Hampshire UK
Reference
- Stevens S. Important and urgent – next steps on NHS response to COVID‐19. Available at: https://www.england.nhs.uk/coronavirus/wp‐content/uploads/sites/52/2020/03/urgent‐next‐steps‐on‐nhs‐response‐to‐covid‐19‐letter‐simon‐stevens.pdf (accessed 13 May 2020).


