As the death toll from the COVID-19 pandemic caused by SARS-CoV-2 continues to mount globally, scientists, healthcare agencies, and pharmaceutical companies are trying hard to find a “cure” and devise treatment strategies to reduce mortality. “Repurposing” existing drugs to fight COVID-19 remains an important strategy. Since respiratory failure remains one of the leading causes of death in COVID-19 patients, in this commentary, we have critically discussed the potential benefit of neutrophil elastase inhibitors (NEIs) in patients hospitalised with severe COVID-19.
Around one in three COVID-19 patients admitted to a hospital develop systemic inflammatory conditions such as cytokine release syndrome (CRS) [1] and acute respiratory distress syndrome (ARDS) [2]. Since lymphocytopenia is often reported in severe COVID-19 patients, it suggests that systemic inflammatory complications, associated with disease severity and mortality, are likely to be mediated by leukocytes other than T cells [3]. The drop in lymphocyte count is accompanied by an increase in neutrophil count and a decrease in monocytes, eosinophils, and basophils [4, 5], indicating that, together with lymphocytopenia, increased neutrophil count and neutrophil-to-lymphocyte ratio may be important predictors of disease severity in COVID-19 patients [5]. A recent case study supported this hypothesis [6]. The patient’s deterioration on day 12 of illness was preceded by an elevation in his neutrophil count on day 11, while lymphocytes and monocytes remained low [6]. Given that there is often a short window between the time of hospital admission and development of ARDS in severe cases [3, 6], a rapid prophylactic therapy is warranted to effectively prevent complications and death.
Neutrophils play a pivotal role in the development of ARDS through the production of toxic mediators including reactive oxygen species and proteases, especially elastase [7]. Furthermore, neutrophils can produce interleukin 6 (IL-6) in response to viral infections, in particular single-stranded RNA viruses such as SARS-CoV-2 via a Toll-like receptor 8 (TLR8)-mediated mechanism [8]. These cells are also important sources of soluble IL-6 receptors (IL-6R) in the lungs and may contribute to pathogenic IL-6R trans-signaling in chronic respiratory diseases [9]. The importance of this kind of signaling for the development of CRS has been demonstrated in chimeric antigen receptor T cell (CART)-treated lymphoma patients [10]. These studies suggest that increased neutrophil count can contribute to CRS and lung damage in patients with ARDS. Additionally, elastase secreted by these cells is one of the key proteolytic enzymes shown to activate the spike (S) protein of coronaviruses and shift the viral entry to a low pH-independent route [11].
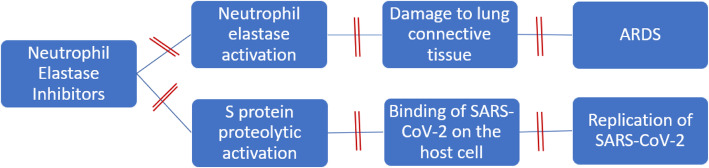
We advocate the use of NEIs such as sivelestat to alleviate neutrophil-induced damage in high-risk COVID-19 patients. Initiation of sivelestat will serve two strategic purposes; first, it will mitigate the damaging effect of neutrophil elastase on the lung connective tissue, and second, it will limit the virus spreading capabilities by preventing S protein proteolytic activation (Fig. 1). Sivelestat is approved in Japan and the Republic of Korea for the treatment of acute lung injury and ARDS. Although existing clinical data is somewhat conflicting, the severity of lung injury remains an important predictor for treatment outcomes in such patients [12, 13]. Clinical trials that reported positive outcomes of sivelestat treatment in patients with ARDS and ALI had recruited patients mainly with lung injury score (LIS) < 2.5. On the other hand, trials reporting negative outcomes particularly the STRIVE study had recruited patients mainly with LIS > 2.5 [12, 13] emphasizing the critical importance of an early intervention with sivelestat. Notably, patients enrolled in the STRIVE study were more heterogeneous than the other trials and included more cases with non-pulmonary organ failures, conditions that are not relevant to COVID-19 patients [12, 13]. Furthermore, post hoc analysis of patient subgroups from the STRIVE study with mean LIS < 2.5 and those with systemic inflammatory response syndrome revealed a positive outcome of sivelestat on mortality rate and ventilator-free days [12, 13]. More importantly, the STRIVE study failed to identify any evidence of drug-related toxicity and did not offer any plausible explanation for the increase in long-term mortality in sivelestat-treated groups [12].
Fig. 1.
Mechanism of action of neutrophil elastase inhibitors in COVID-19.  indicates block. ARDS acute respiratory distress syndrome
indicates block. ARDS acute respiratory distress syndrome
Although current evidence to support the use of NEIs in ARDS induced by COVID-19 is lacking, we hypothesize that early administration of these drugs to patients with lymphocytopenia and LIS < 2.5 may be of significant value to prevent disease progression. Future clinical trials should be designed to evaluate the effectiveness of sivelestat in COVID-19 patients admitted to hospital with high risk of respiratory failure.
Acknowledgements
Not applicable
Authors’ contributions
MMAM, IAE, and MAH conceived the idea. MMAM and IAE wrote the initial draft. MAH critically reviewed the paper. All authors have read the final version and agreed to submit for publication in the journal.
Funding
No funding was obtained from any governmental and non-governmental source in the preparation of this manuscript.
Availability of data and materials
Not applicable
Ethics approval and consent to participate
Not applicable
Consent for publication
Not applicable
Competing interests
None declared.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Mahmoud M. A. Mohamed and Ismail Amr El-Shimy contributed equally to this work.
References
- 1.Zhang C, Wu Z, Li J-W, Zhao H, Wang GQ. The cytokine release syndrome (CRS) of severe COVID-19 and interleukin-6 receptor (IL-6R) antagonist tocilizumab may be the key to reduce the mortality. Int J Antimicrob Agents. 2020. 10.1016/j.ijantimicag.2020.105954. [DOI] [PMC free article] [PubMed]
- 2.Huang C, Wang Y, Li X, Ren L, Zhao J, Hu Y, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395:497–506. doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Shi Y, Wang Y, Shao C, Huang J, Gan J, Huang X, et al. COVID-19 infection: the perspectives on immune responses. Cell Death Differ. 2020. 10.1038/s41418-020-0530-3. [DOI] [PMC free article] [PubMed]
- 4.Qin C, Zhou L, Hu Z, Zhang S, Yang S, Tao Y, et al. Dysregulation of immune response in patients with COVID-19 in Wuhan, China. Clin Infect Dis. 2020. 10.1093/cid/ciaa248. [DOI] [PMC free article] [PubMed]
- 5.Zhang B, Zhou X, Zhu C, Feng F, Qiu Y, Feng J, et al. Immune phenotyping based on neutrophil-to-lymphocyte ratio and IgG predicts disease severity and outcome for patients with COVID-19. medRxiv. 2020. 10.1101/2020.03.12.20035048. [DOI] [PMC free article] [PubMed]
- 6.Xu Z, Shi L, Wang Y, Zhang J, Huang L, Zhang C, et al. Pathological findings of COVID-19 associated with acute respiratory distress syndrome. Lancet Respir Med. 2020;8:420–422. doi: 10.1016/S2213-2600(20)30076-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Donnelly SC, MacGregor I, Zamani A, Gordon MW, Robertson CE, Steedman DJ, et al. Plasma elastase levels and the development of the adult respiratory distress syndrome. Am J Respir Crit Care Med. 1995;151:1428–1433. doi: 10.1164/ajrccm.151.5.7735596. [DOI] [PubMed] [Google Scholar]
- 8.Zimmermann M, Arruda-Silva F, Bianchetto-Aguilera F, Finotti G, Calzetti F, Scapini P, et al. IFNα enhances the production of IL-6 by human neutrophils activated via TLR8. Sci Rep. 2016;6:19674. doi: 10.1038/srep19674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Farahi N, Paige E, Balla J, Prudence E, Ferreira RC, Southwood M, et al. Neutrophil-mediated IL-6 receptor trans-signaling and the risk of chronic obstructive pulmonary disease and asthma. Hum Mol Genet. 2017;26:1584–1596. doi: 10.1093/hmg/ddx053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Li C, Zhang C, Chen X, Zhang Y, Chen J, Kang L, et al. Relative depletion of soluble interleukin 6 receptors abolished the development of cytokine release syndrome after CART19/22 and lenalidomide treatment for lymphoma. Blood. 2019;134(Supplement 1):5313. doi: 10.1182/blood-2019-126821. [DOI] [Google Scholar]
- 11.Belouzard S, Madu I, Whittaker GR. Elastase-mediated activation of the severe acute respiratory syndrome coronavirus spike protein at discrete sites within the S2 domain. J Biol Chem. 2010;285:22758–22763. doi: 10.1074/jbc.M110.103275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Zeiher BG, Artigas A, Vincent JL, Dmitrienko A, Jackson K, Thompson BT, et al. Neutrophil elastase inhibition in acute lung injury: results of the STRIVE study. Crit Care Med. 2004;32:1695–1702. doi: 10.1097/01.CCM.0000133332.48386.85. [DOI] [PubMed] [Google Scholar]
- 13.Aikawa N, Kawasaki Y. Clinical utility of the neutrophil elastase inhibitor sivelestat for the treatment of acute respiratory distress syndrome. Ther Clin Risk Manag. 2014;10:621–629. doi: 10.2147/TCRM.S65066. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable