Background: The coronavirus disease 2019 (COVID-19) pandemic has challenged all of medicine. However, in recent weeks, the nation's need for more infectious disease (ID) expertise has become a clear focal point. As the virus swept across the country, distress over constraints—tests, swabs, personal protective equipment, and ventilators—dominated the discussion. There is more to the story. Following a decade-long trend, in 2019 to 2020, ID programs nationwide saw just 0.8 applicant for every open position; 38% of ID programs failed to fill training slots, and 19% could not fill any slots at all (1). Simply put, cognitive specialties, such as ID, have attracted fewer physicians to the field than other, high-income–generating specialties (2).
Objective: To examine how the distribution of ID specialists matches the needs of the COVID-19 pandemic across the United States.
Methods: We determined county-level ID physician densities—the number of ID physicians per 100 000 persons—by using 2017 Medicare Provider Utilization and Payment Data (3). We calculated the U.S. national average of ID physician density, assigning each county to 1 of 3 categories: ID physician density above the national average, ID physician density below the national average, and no ID physicians.
We then used USAFacts to aggregate data from the Centers for Disease Control and Prevention and public health agencies (4). Using the Geographic Information System tool, we plotted county-level COVID-19 confirmed case rates per 100 000 population (12 May 2020). Because of the skewed distribution of cases nationally, we divided counties into quartiles.
Findings: In 2017, the national average density was 1.76 ID physicians per 100 000 persons; the distribution is geographically skewed (Figure 1). Of the 3142 U.S. counties, 331 (10.5%) and 312 (9.9%) have above- and below-average ID physician densities, respectively; 2499 counties (79.5%) do not have a single ID physician. Therefore, 208 million citizens live in counties with no or below-average ID physician coverage.
Figure 1.
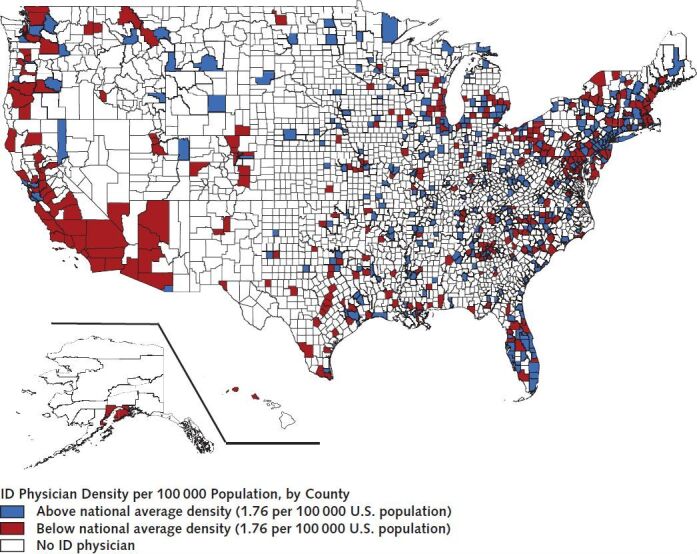
County-level ID physician density for the United States.
The average ID physician density in the United States is 1.76 per 100 000 persons. Counties with ID physicians above this national average density are shown in blue, those with below national average density are shown in red, and counties with no ID physicians are shown in white. ID = infectious disease.
Among the 785 counties with the highest quartile of COVID-19 disease burden (Figure 2), 147 (18.7%) and 117 (14.9%) have above- and below-average ID physician densities, respectively; 521 (66.4%) have no ID physician coverage. In the second highest quartile of counties, 88 (11.2%) and 110 (14.0%) have above- and below-average ID physician densities; 588 (74.8%) have no ID physicians. Among counties with the lowest COVID-19 burden, approximately 95% do not have a single ID physician.
Figure 2.
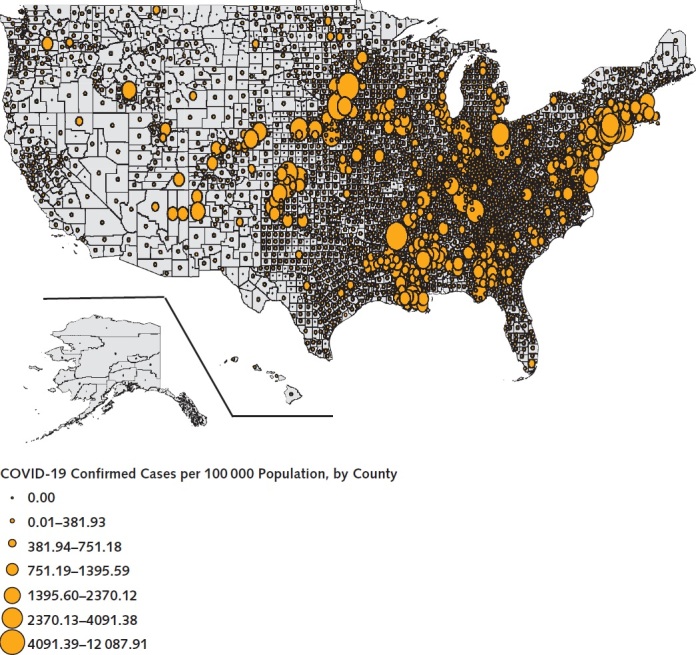
Confirmed COVID-19 cases reported per 100 000 population, by county, 12 May 2020.
COVID-19 = coronavirus disease 2019.
Discussion: The distribution of ID physicians in the United States is geographically skewed. In the counties with the top quartile of COVID-19 cases today, 80% have below-average ID physician density or no ID physicians at all. Furthermore, nearly two thirds of all Americans live in the 90% of counties with below-average or no ID physician access, and these counties encompass vast—largely rural—parts of the country.
Data demonstrating the association between ID physician care and COVID-19 clinical outcomes have yet to emerge. However, for many other infectious diseases, a robust evidence base supports the association between ID physician intervention and improved outcomes, including lower mortality, shorter length of stay, fewer readmissions, and lower total health care spending (5). The current analysis did not account for other professions capable of delivering public health or ID-specific care (such as epidemiologists, advanced practice providers, pharmacists, and infection preventionists) or shortages in other cognitive specialties collaborating with ID physicians to manage patients with COVID-19. Although limited literature informs the “right” number of ID physicians in a population, our current distribution during pandemic times is probably far too sparse.
The deficits in our ID physician workforce today have left us poorly prepared for the unprecedented demand ahead. Telehealth stretches the reach of constrained ID expertise, extending clinical and public health management into underserved rural areas, but can succeed only if the Centers for Medicare & Medicaid Services and other payers fully embrace this tool.
While urban centers move toward the identification, containment, and treatment strategies required in the absence of herd immunity or an effective vaccine, rural counties offer fertile ground for the spread of severe acute respiratory syndrome coronavirus 2. Faced with a surge of patients with COVID-19, these rural counties will be left wanting for the public health and clinical care activities ID physicians provide. The current experience with an overextended ID workforce is a cautionary tale. Our nation's health and future clearly depend on a long-term strategic ID workforce plan.
Biography
Financial Support: The work was supported by awards from the Massachusetts General Hospital Executive Committee on Research (Steve and Deborah Gorlin Research Scholars Award to Dr. Walensky).
Disclosures: Disclosures can be viewed at www.acponline.org/authors/icmje/ConflictOfInterestForms.do?msNum=M20-2684.
Reproducible Research Statement: Study protocol: Available at https://usafacts.org/visualizations/coronavirus-covid-19-spread-map and www.cms.gov/Research-Statistics-Data-and-Systems/Statistics-Trends-and-Reports/Medicare-Provider-Charge-Data/Physician-and-Other-Supplier. Statistical code: Available from Dr. Shahbazi (e-mail, sshahbazi@mgh.harvard.edu). Data set: Available at https://usafacts.org/visualizations/coronavirus-covid-19-spread-map and https://data.cms.gov/Medicare-Physician-Supplier/Medicare-Physician-and-Other-Supplier-National-Pro/n5qc-ua94.
Corresponding Author: Rochelle P. Walensky, MD, MPH, Division of Infectious Diseases, Massachusetts General Hospital, 55 Fruit Street, Bul130, Boston, Massachusetts 02114; e-mail, rwalensky@mgh.harvard.edu.
Footnotes
This article was published at Annals.org on 3 June 2020.
References
- 1. The National Resident Matching Program. Match results statistics: 2019 MSMP match results report. Accessed at www.nrmp.org/fellowships/medical-specialties-matching-program. on 29 April 2020.
- 2. doi: 10.1093/cid/cix173. Walensky RP, Del Rio C, Armstrong WS. Charting the future of infectious disease: anticipating and addressing the supply and demand mismatch. Clin Infect Dis. 2017;64:1299-1301. [PMID: 28387806] doi:10.1093/cid/cix173. [DOI] [PubMed]
- 3. U.S. Census Bureau. County population totals: 2010-2019. Accessed at www.census.gov/data/tables/time-series/demo/popest/2010s-counties-total.html#par_textimage. on 29 April 2020.
- 4. USAFacts. Coronavirus locations: COVID-19 map by county and state. Accessed at https://usafacts.org/visualizations/coronavirus-covid-19-spread-map. on 29 April 2020.
- 5. doi: 10.1093/cid/ciy494. Schmitt S, MacIntyre AT, Bleasdale SC, et al. Early infectious diseases specialty intervention is associated with shorter hospital stays and lower readmission rates: a retrospective cohort study. Clin Infect Dis. 2019;68:239-246. [PMID: 29901775] doi:10.1093/cid/ciy494. [DOI] [PubMed]


