Abstract
To explore the multimorbidity prevalence and patterns among middle-aged and older adults from China. Data on thirteen chronic diseases were collected from 2,097,150 participants aged over 45 years between January 1st 2011 and December 31st 2015 from Beijing Medical Claim Data for Employees. Association rule mining and hierarchical cluster analysis were applied to assess multimorbidity patterns. Multimorbidity prevalence was 51.6% and 81.3% in the middle-aged and older groups, respectively. The most prevalent disease pair was that of osteoarthritis and rheumatoid arthritis (OARA) with hypertension (HT) (middle-aged: 22.5%; older: 41.8%). Ischaemic heart disease (IHD), HT, and OARA constituted the most common triad combination (middle-aged: 11.0%; older: 31.2%). Among the middle-aged group, the strongest associations were found in a combination of cerebrovascular disease (CBD), OARA, and HT with IHD in males (lift = 3.49), and CBD, OARA, and COPD with IHD in females (lift = 3.24). Among older patients, glaucoma and cataracts in females (lift = 2.95), and IHD, OARA, and glaucoma combined with cataracts in males (lift = 2.45) were observed. Visual impairment clusters, a mixed cluster of OARA, IHD, COPD, and cardiometabolic clusters were detected. Multimorbidity is prevalent among middle-aged and older Chinese individuals. The observations of multimorbidity patterns have implications for improving preventive care and developing appropriate guidelines for morbidity treatment.
Keywords: multimorbidity, prevalence, pattern, chronic diseases, China
1. Introduction
Multimorbidity, commonly defined as the cooccurrence of two or more chronic diseases, has gained increasing attention as a prominent public health issue worldwide [1]. Multimorbidity has been associated with poorer health outcomes including greater risk of disability and mortality among older populations [2]. Additionally, it complicates treatment and health care plans and increases the risk of psychiatric and somatic complications, thus leading to higher healthcare expenditures and resource utilization [3,4].
A large body of literature has reported multimorbidity prevalence and patterns worldwide. It was reported that the prevalence of multimorbidity ranged from 45% to 72% among older adults aged 50 years and over in nine countries [5] and ranged from 24% to 83% among those aged 60 years and older in South Asia [6]. In addition, the overall prevalence of multimorbidity among older adults is widely ranged from 6.4% to 86.9% in China [7]. Additionally, studies have observed different multimorbidity patterns, such as cardiometabolic patterns, mental health patterns, and musculoskeletal patterns, using cluster analysis, factor analysis, or Association rule mining (ARM) [8,9,10]. Nevertheless, multimorbidity patterns are expected to have unique characteristics for different countries because of a variance in factors such as environment, race/ethnicity, and lifestyles [11].
However, most research studies investigating multimorbidity in China have been conducted among community-dwelling populations and defined chronic conditions using self-reported questionnaires or face-to-face interviews, which can be affected by recall and selection bias [8,9,12,13,14]. The population-based estimates derived from claims data were very limited, especially in Asian countries [14,15,16]. Studies based on claims data defined multimorbidity using more objective clinical diagnoses without recall/non-response bias based on a patient-based population [17,18]. Furthermore, using International Classification of Diseases (ICD) codes in claims data also facilitated the international comparability of understanding multimorbidity [19].
In addition, current multimorbidity studies have mostly focused on older adults aged ≥60 years [20,21,22,23]. One recent study reported that multimorbidity had a greater impact on all-cause mortality in middle-aged populations than in older populations [24]. There was found to be a greater hospitalization burden among middle-aged people with multimorbidity than their older counterparts as well [25]. Middle-aged patients with multimorbidity represent a vulnerable group with distinct chronic care needs [25]. Studies on multimorbidity among middle-aged adults are therefore essential to address their need for personalized health care.
Better understanding of multimorbidity prevalence and patterns among different populations can help explore possible interactions between different diseases as well as improve population-specific approaches for managing multimorbidity to lessen the public health burden [26,27]. This study therefore aimed to evaluate the prevalence and patterns of multimorbidity (i.e., combinations and clustering of chronic diseases) among middle-aged and older Chinese adults using claims data accumulated through a mandatory insurance programme in Beijing, China.
2. Materials and Methods
2.1. Data Source
This study used data from the Beijing Medical Claim Data for Employees (BMCDE), a mandatory health insurance programme consisting of all working and retired workers in Beijing [28,29]. BMCDE included information on patients’ demographic characteristics (age and sex), inpatient and outpatient clinical diagnoses, and medications, with personal identifiers removed. All clinical visits of patients could be linked with their unique encrypted identification number. This study was considered exempt because BMCDE data were collected for administrative purposes with personal identifiers removed for research purposes.
2.2. Measurement of Multimorbidity and Study Population
For this study, the following thirteen chronic diseases were selected based on the most frequently mentioned diseases for multimorbidity measures by previous literatures that were considered to significantly impact long-term treatment and decrease functional performance and quality of life among the Chinese population [30,31]: malignancy, cerebrovascular disease (CBD), ischaemic heart disease (IHD), chronic obstructive pulmonary disease (COPD), diabetes mellitus (DM), depressive disorders (DD), chronic kidney disease (CKD), osteoarthritis and rheumatoid arthritis (OARA), peptic ulcer disease (PUD), cataracts, heart failure (HF), hypertension (HT), and glaucoma. Diseases were identified if they had been documented using inpatient or outpatient ICD-10 codes at least twice in individual medical records during the 5-year period from January 1, 2011 to December 31, 2015 [32,33]. For this study, a total of 2,097,150 people aged ≥45 years in 2015 were included. Table S1 lists all chronic medical diseases included and their corresponding ICD-10 codes. For this study, multimorbidity was defined as concurrently suffering from two or more chronic diseases.
2.3. Statistical Analyses
Age was categorized into the following two subgroups: 45–59 years (middle-aged group) and ≥60 years (older group). Continuous variables were examined using the mean (standard deviation, SD). Categorical variables were summarized with frequencies (percentages), and the X2 test was performed to compare these characteristics. Given the sufficiently large sample size in this study, all tests showed a significant p value (p < 0.001), which is not presented in the results [34].
ARM was applied to determine common multimorbidity patterns that met a minimum requirement of measurement indicators among large sets of diagnoses. Association rules were relationships between sets of diseases from “antecedent” to “consequent” [35]. The following are the three common measurement indicators in ARM: support (the frequency of the disease combinations in the association rule), confidence (how frequently the antecedent diseases occur, conditional on the consequent diseases), and lift (how much more frequently the diseases set in the same association rule occur together compared with the expected prevalence under statistical independence). Lift was considered the main measure of significance in ARM [36]. The higher the lift, the higher the chance of co-occurrence of the consequent with the antecedent and the more significant the association [36]. For this study, the minimum thresholds of parameters in ARM were defined as follows: support > 2%, confidence > 10%, and lift > 1%. Hierarchical cluster analysis (HCA) was used to identify those diseases that were inclined to gather together according to their correlated structure and similarity patterns. Those that were strongly correlated or had similar diseases were classified into the same clusters using homogeneity criteria [37]. The homogeneity criterion of a cluster is defined as the sum of correlation ratios [37]. The function “hclustvar” in the R package “ClustOfVar” was used in the clustering analysis (www.r-project.org). All analyses were performed using R 3.2.2 (R Development Core Team).
3. Results
Table 1 shows the basic demographics and prevalence of chronic diseases in the studied population. This study included 2,097,150 people aged ≥45 years, with 50.0% (n = 1,048,575) aged 45–59 years (middle-aged group) and 50.0% (n = 1,048,575) aged ≥60 years (older group). The mean age was 52.8 years for those aged 45–59 years and 70.3 years for those aged ≥60 years.
Table 1.
Observed prevalence of chronic diseases by age and sex.
| 45 ≤ Age ≤ 59 | Age ≥ 60 | |||||
|---|---|---|---|---|---|---|
| All (n = 1,048,575) |
Male (n = 446,540) |
Female (n = 602,035) |
All (n = 1,048,575) |
Male (n = 508,717) |
Female (n = 539,858) |
|
| Age (yrs), mean (SD) | 52.8 (4.3) | 52.7 (4.3) | 52.9 (4.2) | 70.3 (8.0) | 70.5 (8.1) | 70.0 (8.0) |
| Chronic health disease, n (%) | ||||||
| Malignancy | 58,077 (5.5) | 28,112 (6.3) | 29,965 (5.0) | 94,008 (9.0) | 44,195 (8.7) | 49,813 (9.2) |
| CBD | 81,777 (7.8) | 39,936 (8.9) | 41,841 (6.9) | 263,451 (25.1) | 138,135 (27.2) | 125,316 (23.2) |
| IHD | 231,483 (22.1) | 112,274 (25.1) | 119,209 (19.8) | 587,596 (56.0) | 273,645 (53.8) | 313,951 (58.2) |
| COPD | 206,724 (19.7) | 100,081 (22.4) | 106,643 (17.7) | 394,699 (37.6) | 181,243 (35.6) | 213,456 (39.5) |
| DM | 216,014 (20.6) | 104,721 (23.5) | 111,293 (18.5) | 317,576 (30.3) | 163,205 (32.1) | 154,371 (28.6) |
| DD | 113,530 (10.8) | 55,000 (12.3) | 58,530 (9.7) | 128,534 (12.3) | 51,017 (10.0) | 77,517 (14.4) |
| CKD | 57,640 (5.5) | 27,944 (6.3) | 29,696 (4.9) | 130,281 (12.4) | 66,252 (13.0) | 64,029 (11.9) |
| OARA | 467,787 (44.6) | 226,943 (50.8) | 240,844 (40.0) | 707,436 (67.5) | 306,174 (60.2) | 410,262 (74.3) |
| PUD | 125,720 (12.0) | 61,089 (13.7) | 64,631 (10.7) | 190,506 (18.2) | 89,638 (17.6) | 100,868 (18.7) |
| Cataract | 37,363 (3.6) | 18,151 (4.1) | 19,212 (3.2) | 216,475 (20.6) | 88,028 (17.3) | 128,447 (23.8) |
| HF | 10,835 (1.0) | 5280 (1.2) | 5555 (0.9) | 48,672 (4.6) | 24,717 (4.9) | 23,955 (4.4) |
| HT | 520,324 (49.6) | 252,602 (56.6) | 267,722 (44.5) | 681,179 (65.0) | 335,584 (66.0) | 345,595 (64.0) |
| Glaucoma | 23,188 (2.2) | 11,212 (2.5) | 11,976 (2.0) | 51,695 (4.9) | 21,195 (4.2) | 30,500 (5.6) |
Abbreviations: SD, standard deviation; CBD, cerebrovascular disease; IHD, ischaemic heart disease; COPD, chronic obstructive pulmonary disease; DM, diabetes mellitus; DD, depressive disorders; CKD, chronic kidney disease; OARA, osteoarthritis and rheumatoid arthritis; PUD, peptic ulcer disease; HF, heart failure; HT, hypertension.
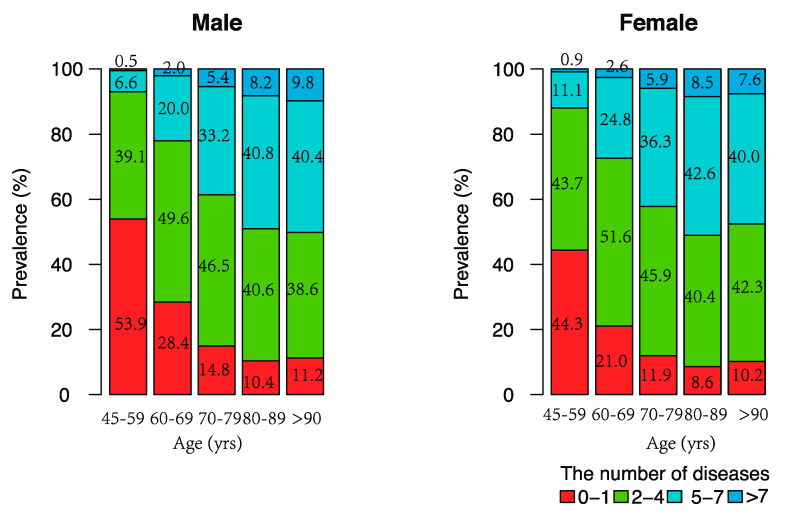
Figure 1 shows the multimorbidity prevalence by age and sex. The prevalence of multimorbidity was 51.6% (male: 46.1%; female: 55.7%) in the middle-aged group and 81.3% (male: 78.8%; female: 83.7%) in the older group. The overall proportion of people with multimorbidity increased from 51.6% for those aged 45–59 years to 89.3% for those over 90 years. Females had a higher prevalence than males for each age group.
Figure 1.
Multimorbidity prevalence by age and sex among middle-aged and older Chinese.
The most frequent (top 3) combinations, stratified by age, sex, and total number of chronic diseases, are presented in Table 2. Among patients with at least two chronic conditions, OARA combined with HT was the most prevalent disease pair for patients of all ages (male: 29.6%; female: 37.6%), male middle-aged patients (male: 16.0%; female: 27.3%), and male older patients (35.1%). Among older females, IHD combined with OARA was the most prevalent disease pair (49.2%). Furthermore, IHD, HT, and OARA was the most common triad combination among patients with at least three chronic conditions (middle-aged male: 8.0%; middle-aged female: 13.2%; older male: 26.4%; older female: 36.6%).
Table 2.
Top three frequent unique combination clusters for patients with multimorbidity, stratified by total number of chronic diseases and by sex.
| Age Group | Rank | Dyads of Morbidities | Triads of Morbidities | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Male | Female | Male | Female | ||||||
| Combination | n (%) | Combination | n (%) | Combination | n (%) | Combination | n (%) | ||
| All ages; male: n = 955,257, female: n = 1,141,893 | |||||||||
| 1 | OARA + HT | 282,995 (29.6) | OARA + HT | 429,553 (37.6) | IHD + OARA + HT | 194,735 (20.4) | IHD + OARA + HT | 276,928 (24.3) | |
| 2 | IHD + HT | 272,230 (28.5) | IHD + OARA | 383,889 (33.6) | COPD + OARA + HT | 132,923 (13.9) | COPD + OARA + HT | 204,352 (17.9) | |
| 3 | IHD + OARA | 255,872 (26.8) | IHD + HT | 324,411 (28.4) | IHD + COPD + OARA | 130,557 (13.7) | IHD + COPD + OARA | 198,311 (17.4) | |
| 45–59 years; male: n = 446,540, female: n = 602,035 | |||||||||
| 1 | OARA + HT | 71,626 (16.0) | OARA + HT | 164,234 (27.3) | IHD + OARA + HT | 35,719 (8.0) | IHD + OARA + HT | 79,290 (13.2) | |
| 2 | DM + HT | 65,518 (14.7) | COPD + OARA | 120,912 (20.1) | DM + OARA + HT | 24,719 (5.5) | COPD + OARA + HT | 70,249 (11.7) | |
| 3 | IHD + HT | 63,979 (14.3) | IHD + OARA | 118,355 (19.7) | COPD + OARA + HT | 24,367 (5.5) | IHD + COPD + OARA | 58,021 (9.6) | |
| ≥60 years; male: n = 602,035, female: n = 539,858 | |||||||||
| 1 | OARA + HT | 211,369 (35.1) | IHD + OARA | 265,534 (49.2) | IHD + OARA + HT | 159,016 (26.4) | IHD + OARA + HT | 197,638 (36.6) | |
| 2 | IHD + HT | 208,251 (34.6) | OARA + HT | 265,319 (49.1) | IHD + COPD + OARA | 110,904 (18.4) | IHD + COPD + OARA | 140,290 (26.0) | |
| 3 | IHD + OARA | 206,397 (34.3) | IHD + HT | 230,795 (42.8) | COPD + OARA + HT | 108,556 (18.0) | COPD + OARA + HT | 134,103 (24.8) | |
Abbreviations: IHD, ischaemic heart disease; COPD, chronic obstructive pulmonary disease; DM, diabetes mellitus; OARA, osteoarthritis and rheumatoid arthritis; HT, hypertension.
The ARM results illustrated the associations between these diseases. The top 10 association rules among the included diseases according to lift are shown in Table 3. Among the middle-aged patients, the strongest association was found between the combination of CBD, OARA, HT, and IHD in males where the lift was 3.49, whereas the highest lift for females was 3.24 for the combination of CBD, OARA, COPD, and IHD, making these diseases occur together with 3.49- or 3.24-times higher likelihoods, respectively, than would be expected if they were independent. Among older adults, the strongest associations were observed between glaucoma and cataracts in females (lift = 2.952) and the combination of IHD, OARA, and glaucoma with cataracts in males (lift = 2.450), indicating that these antecedent combinations positively correlated with the occurrence of cataracts. Moreover, in the middle-aged group, IHD tended to be comorbid with others that occurred in 9 association rules in males and 10 in females among the top 10 rules. In contrast, among the older males, cataracts and diabetes were the most common comorbidities, and both occurred in 5 association rules.
Table 3.
The top 10 association rules in the order of lift.
| Middle-Aged | Older | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Male | Female | Male | Female | ||||||||
| Antecedent | Consequent | Lift | Antecedent | Consequent | Lift | Antecedent | Consequent | Lift | Antecedent | Consequent | Lift |
| CBD + OARA + HT | IHD | 3.487 | CBD + OARA + COPD | IHD | 3.237 | IHD + OARA + Glaucoma | Cataract | 2.450 | Glaucoma | Cataract | 2.952 |
| CBD + OARA | IHD | 3.321 | CBD + COPD | IHD | 3.169 | IHD + Glaucoma | Cataract | 2.419 | OARA + PUD + CKD | COPD | 2.008 |
| OARA + HT + PUD | IHD | 3.020 | CBD + OARA + HT | IHD | 3.134 | HT + Glaucoma | Cataract | 2.417 | IHD + DD + OARA + HT | IHD | 2.006 |
| COPD + OARA + HT | IHD | 2.981 | CBD + OARA | IHD | 2.992 | OARA + Glaucoma | Cataract | 2.382 | IHD + COPD + DD | IHD | 1.997 |
| DM + OARA + HT | IHD | 2.945 | CBD + HT | IHD | 2.874 | Glaucoma | Cataract | 2.311 | IHD + CKD + PUD | COPD | 1.992 |
| COPD + DM | IHD | 2.781 | COPD + DM + OARA + HT | IHD | 2.821 | CBD + CKD + HT | DM | 2.062 | CKD + PUD + HT | COPD | 1.961 |
| COPD + HT | IHD | 2.692 | COPD + PUD + OARA + HT | IHD | 2.764 | IHD + CKD + HT | DM | 1.953 | IHD + DM + OARA + PUD + HT | IHD | 1.957 |
| PUD + HT | IHD | 2.637 | COPD + DM + HT | IHD | 2.736 | CBD + IHD + CKD | DM | 1.946 | CBD + IHD + CKD + OARA + HT | COPD | 1.956 |
| COPD + PUD | OARA | 2.623 | COPD + PUD + HT | IHD | 2.711 | IHD + CKD + OARA + HT | DM | 1.937 | IHD + DD + HT | IHD | 1.952 |
| CBD + HT | IHD | 2.593 | CBD | IHD | 2.692 | CBD + CKD | DM | 1.933 | CKD + OARA + Cataract | COPD | 1.945 |
Abbreviations: CBD, cerebrovascular disease; IHD, ischaemic heart disease; COPD, chronic obstructive pulmonary disease; DM, diabetes mellitus; DD, depressive disorders; CKD, chronic kidney disease; OARA, osteoarthritis and rheumatoid arthritis; PUD, peptic ulcer disease; HT, hypertension.
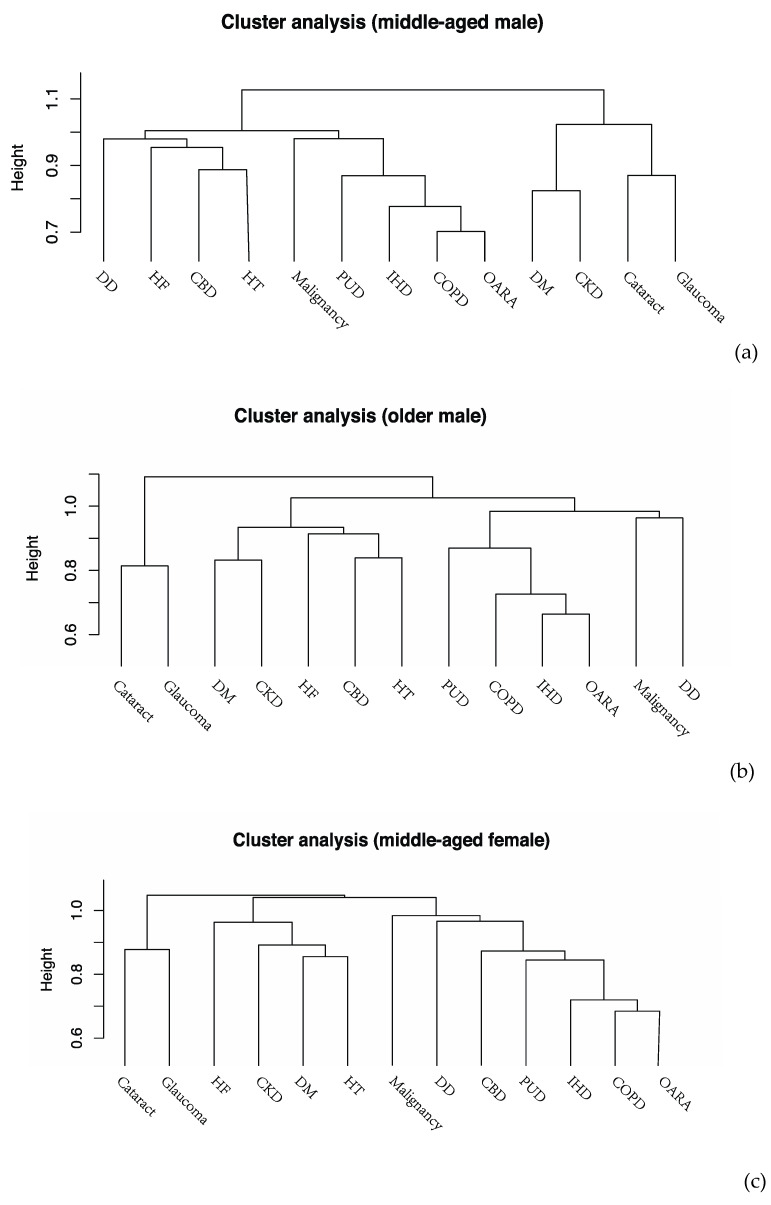
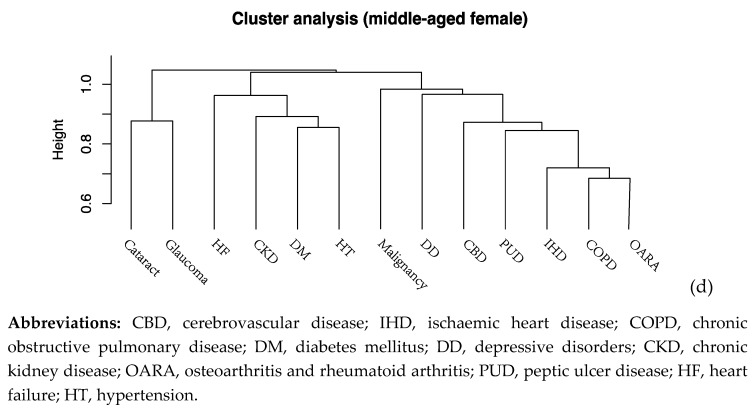
Disease clusters derived from HCA stratified by age and sex are shown in Figure 2a–d. Common disease clusters observed in the four subgroups included a visual impairment cluster consisting of glaucoma and cataract and a mixed cluster of OARA, IHD, and COPD. Furthermore, a cardiometabolic cluster, including HF, HT, DM and CKD, was detected among middle-aged female individuals and the older group.
Figure 2.
Dendrograms of cluster analysis showing the distribution and aggregation of chronic diseases in (a) middle-aged males, (b) middle-aged females, (c) older males, and (d) older females.
4. Discussion
To the best of our knowledge, this study was among the first to explore multimorbidity prevalence and patterns based on large medical claims data among a middle-aged and older Chinese population. The prevalence of multimorbidity increased with age. Females had a higher prevalence of multimorbidity than males. OARA, combined with HT, was the most prevalent disease pair for patients of all ages. IHD, HT, and OARA was the most common triad combination. In addition, several disease clusters were identified in our study including a visual impairment cluster, a mixed cluster of OARA, IHD, and COPD, and a cardiometabolic cluster. There were strong associations between CBD, OARA, and IHD among the middle-aged group and between glaucoma and cataracts among the older group.
We found that the prevalence of multimorbidity was 51.6% for middle-aged adults aged 45–59 and 81.3% for older adults aged ≥60 years. One study using claims data from Taiwan in 2013 showed a similar prevalence of multimorbidity, which was 56.8%, 74.6%, and 82.6% in people aged 60–69, 70–79, and 80–89 years, respectively [16]. Additionally, two European studies based on claims data also reported that the multimorbidity prevalence among adults aged ≥60 years old was 85% in Germany [14] and 77% in Switzerland [15]. Consistent with previous studies, we observed a higher prevalence of multimorbidity among females than among males, which may be partially due to the relatively higher prevalence of select chronic diseases in females [8,38,39,40]. One study conducted in six low- and middle-income countries among adults aged ≥50 years reported a higher overall prevalence of six chronic diseases, including angina, arthritis, asthma, chronic lung disease, depression, and HT, in females [41]. Moreover, the incidence of chronic inflammatory diseases in females after menopausal age, as a result of hormonal changes, exceeded that observed in males [42]. One alternative explanation might be that females were generally more aware of their own health status and had more healthcare-seeking behaviours, which might lead to a higher probability of being diagnosed with diseases [43].
According to the frequency, we found that the most prevalent disease pair was OARA combined with HT, and the most common triad combination was IHD, HT, and OARA. A multi-country study reported similar results: comorbid diseases of HT and arthritis were highly prevalent in China, Finland, Ghana, Poland, Russia, South Africa, and Spain [5]. A study in Belgium also detected the most prevalent pair as HT-OA [44]. Moreover, the lift in ARM discovered interesting combinations of comorbidities that were occurring more frequently than expected. In our study, the ranked lift indicated that there were strong associations between vascular and musculoskeletal disorders, including CBD, IHD, and HT with OARA. A cross-sectional study conducted in Europe observed that HT was one of the most common comorbidities among individuals with osteoarthritis (OA) [45]. In addition, a meta-analysis showed that there was a significant relationship between cardiovascular disease (CVD) and OA [46,47]. Possible explanations for the relationship between CVD and OARA include shared biological mechanisms, such as ageing and obesity [48,49,50]. For example, obesity can induce chronic inflammation and endothelial dysfunction, which are simultaneously implicated in cartilage degradation, atherosclerosis, and a higher CVD risk [51]. Overweight and obese people also have reduced levels of physical activity and functional limitations, which are concomitant risk factors for CVD, joint pain and OARA [52]. Moreover, individuals with nonsteroidal anti-inflammatory medication treatments could contribute substantially to the OA–CVD association [53]. The observations of prevalent disease combinations could have implications for health prevention, where measurements targeting a specific factor may benefit two or more related diseases.
Furthermore, strong associations between IHD, OARA, and COPD were also detected by ARM and HCA. Our findings were consistent with those from a study using medical record data in Sweden which reported significantly associated comorbidities, including IHD and OA, among COPD patients [54]. Similarly, a population-based cohort in Canada also observed COPD and HT as prevalent comorbidities among people with OA [55]. Moreover, a systematic review confirmed that the prevalence of OA was high among individuals with COPD [56]. The potential mechanisms might include increased systemic inflammatory mediators and some adverse effects, such as physical inactivity, which are also risk factors for other diseases [56]. Compared to a study conducted in rural China, it observed the most prevalent multimorbidity pattern for CBD, HT, and DM, which might be attributed to an imbalance in the delivery of primary care services, such as the lack of blood pressure and blood glucose monitoring, and availability of essential medicines in rural districts [57]. Moreover, in older females, strong associations between IHD, OARA, glaucoma, and cataracts were observed, partially owing to the high prevalence of these diseases [58]. The ARM results also reported common comorbidities, including IHD among middle-aged individuals and DM in males. Survival bias may explain the age and gender difference for the comorbidity, as IHD and DM were linked to higher mortality in older [59] and female [60] patients, respectively.
The main strength of this study was the large sample size of the administrative data used to illustrate multimorbidity prevalence and patterns among a middle-aged and older Chinese population. The multimorbidity measures defined by the ICD codes, including a broad range of chronic diseases, can help detect specific patterns potentially left out in survey-based studies. This study also had several limitations. First, the BMCDE database only included people who had been employed, leading to limited generalizability to a general population. Additionally, although claims data included ICD-10 codes recorded by well-trained doctors in certified hospitals, we could not necessarily ensure exclusion of inaccurate or underreporting diagnoses. Finally, the dataset did not include patients’ socioeconomic status, anthropometric parameters, detailed clinical information, as well as health-related behaviours. We therefore could not investigate potential confounding factors and take disease severity into consideration.
5. Conclusions
Multimorbidity was prevalent among middle-aged and older Chinese individuals. Females had a higher prevalence than males. The most prevalent disease pair was OARA combined with HT. The most common triad combination consisted of IHD, HT, and OARA. CVDs (including CBD, IHD, and HT), OARA and COPD were more likely to co-occur. The observations of the multimorbidity pattern, including the most frequent comorbidities, associations, and clusters in our study, provide evidence for the priority of disease clusters for further research and encourage healthcare providers to develop healthcare plans towards a multiple-condition framework among patients with multimorbidity. Deep understanding of the complexity of multimorbidity based on large administrative datasets can improve the quality and efficiency of patient-centred care.
Abbreviations
| ICD | International Classification of Diseases |
| BMCDE | Beijing Medical Claim Data for Employees |
| SD | standard deviation |
| ARM | association rule mining |
| HCA | hierarchical cluster analysis |
| CBD | cerebrovascular disease |
| IHD | ischaemic heart disease |
| COPD | chronic obstructive pulmonary disease |
| DM | diabetes mellitus |
| DD | depressive disorders |
| CKD | chronic kidney disease |
| OARA | osteoarthritis and rheumatoid arthritis |
| PUD | peptic ulcer disease |
| HF | heart failure |
| HT | hypertension |
| CVD | cardiovascular disease |
Supplementary Materials
The following are available online at https://www.mdpi.com/1660-4601/17/10/3395/s1, Table S1: The ICD-10 codes for the select diseases included.
Author Contributions
Conceptualization, X.W., B.X. and Y.H.; Data curation, S.Y.; Formal analysis, X.W. and S.Y.; Funding acquisition, B.X. and Y.H.; Investigation, X.W., M.W. and G.C.; Methodology, X.W. and M.W.; Project administration, Y.H.; Resources, Y.H.; Supervision, B.X. and Y.H.; Validation, Z.C. and Z.H.; Visualization, X.W.; Writing—original draft, X.W.; Writing—review and editing, X.W., S.Y., M.W., G.C., Z.C., Z.H., Y.W., L.H., B.X. and Y.H. All authors have read and agreed to the published version of the manuscript.
Funding
This work was supported by the Key Project of Natural Science Funds of China (No. 81230066) and the National Natural Science Fund Projects of China (No. 81473043, 81703304, and 81973130). The funding sources were not involved in the conception and design of this study; the assessment, analysis and interpretation of data; the writing of the report; or the decision to submit the article for publication.
Conflicts of Interest
The authors declare no conflict of interest.
References
- 1.Xu X., Mishra G.D., Jones M. Evidence on multimorbidity from definition to intervention: An overview of systematic reviews. Ageing Res. Rev. 2017;37:53–68. doi: 10.1016/j.arr.2017.05.003. [DOI] [PubMed] [Google Scholar]
- 2.Di Angelantonio E., Kaptoge S., Wormser D., Willeit P., Butterworth A.S., Bansal N., Danesh J. Association of cardiometabolic multimorbidity with mortality. Jama. 2015;314:52–60. doi: 10.1001/jama.2015.7008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.McPhail S.M. Multimorbidity in chronic disease: Impact on health care resources and costs. Risk Manag. Healthc Policy. 2016;9:143–156. doi: 10.2147/RMHP.S97248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Riano D., Peleg M., Ten Teije A. Ten years of knowledge representation for health care (2009–2018): Topics, trends, and challenges. Artif. Intell. Med. 2019;100:101713. doi: 10.1016/j.artmed.2019.101713. [DOI] [PubMed] [Google Scholar]
- 5.Garin N., Koyanagi A., Chatterji S., Tyrovolas S., Olaya B., Leonardi M., Haro J.M. Global multimorbidity patterns: A cross-sectional, population-based, multi-country study. J. Gerontol. A Biol. Sci. Med. Sci. 2016;71:205–214. doi: 10.1093/gerona/glv128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Pati S., Swain S., Hussain M.A., van den Akker M., Metsemakers J., Knottnerus J.A., Salisbury C. Prevalence and outcomes of multimorbidity in south asia: A systematic review. BMJ Open. 2015;5 doi: 10.1136/bmjopen-2014-007235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hu X., Huang J., Lv Y., Li G., Peng X. Status of prevalence study on multimorbidity of chronic disease in china: Systematic review. Geriatr. Gerontol. Int. 2015;15:1–10. doi: 10.1111/ggi.12340. [DOI] [PubMed] [Google Scholar]
- 8.Yao S.S., Cao G.Y., Han L., Chen Z.S., Huang Z.T., Gong P., Xu B. Prevalence and patterns of multimorbidity in a nationally representative sample of older chinese: Results from charls. J. Gerontol. A Biol. Sci. Med. Sci. 2019 doi: 10.1093/gerona/glz185. [DOI] [PubMed] [Google Scholar]
- 9.Zhang R., Lu Y., Shi L., Zhang S., Chang F. Prevalence and patterns of multimorbidity among the elderly in china: A cross-sectional study using national survey data. BMJ Open. 2019;9:e024268. doi: 10.1136/bmjopen-2018-024268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Prados-Torres A., Calderon-Larranaga A., Hancco-Saavedra J., Poblador-Plou B., van den Akker M. Multimorbidity patterns: A systematic review. J. Clin. Epidemiol. 2014;67:254–266. doi: 10.1016/j.jclinepi.2013.09.021. [DOI] [PubMed] [Google Scholar]
- 11.Violan C., Foguet-Boreu Q., Flores-Mateo G., Salisbury C., Blom J., Freitag M., Valderas J.M. Prevalence, determinants and patterns of multimorbidity in primary care: A systematic review of observational studies. PLoS ONE. 2014;9 doi: 10.1371/journal.pone.0102149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lai F.T.T., Guthrie B., Wong S.Y.S., Yip B.H.K., Chung G.K.K., Yeoh E.K., Chung R.Y. Sex-specific intergenerational trends in morbidity burden and multimorbidity status in hong kong community: An age-period-cohort analysis of repeated population surveys. BMJ Open. 2019;9:e023927. doi: 10.1136/bmjopen-2018-023927. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Gu J., Chao J., Chen W., Xu H., Wu Z., Chen H., Zhang R. Multimorbidity in the community-dwelling elderly in urban china. Arch. Gerontol. Geriatr. 2017;68:62–67. doi: 10.1016/j.archger.2016.09.001. [DOI] [PubMed] [Google Scholar]
- 14.Bahler C., Huber C.A., Brungger B., Reich O. Multimorbidity, health care utilization and costs in an elderly community-dwelling population: A claims data based observational study. BMC Health Serv. Res. 2015;15:23. doi: 10.1186/s12913-015-0698-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kostev K., Jacob L. Multimorbidity and polypharmacy among elderly people followed in general practices in germany. Eur. J. Intern. Med. 2018;55:66–68. doi: 10.1016/j.ejim.2018.07.014. [DOI] [PubMed] [Google Scholar]
- 16.Hu R.H., Hsiao F.Y., Chen L.J., Huang P.T., Hsu W.W. Increasing age- and gender-specific burden and complexity of multimorbidity in taiwan, 2003–2013: A cross-sectional study based on nationwide claims data. BMJ Open. 2019;9:e028333. doi: 10.1136/bmjopen-2018-028333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hunger M., Schwarzkopf L., Heier M., Peters A., Holle R. Official statistics and claims data records indicate non-response and recall bias within survey-based estimates of health care utilization in the older population. BMC Health Serv. Res. 2013;13:1. doi: 10.1186/1472-6963-13-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lujic S., Simpson J.M., Zwar N., Hosseinzadeh H., Jorm L. Multimorbidity in australia: Comparing estimates derived using administrative data sources and survey data. PLoS ONE. 2017;12:e0183817. doi: 10.1371/journal.pone.0183817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Calderon-Larranaga A., Vetrano D.L., Onder G., Gimeno-Feliu L.A., Coscollar-Santaliestra C., Carfi A., Fratiglioni L. Assessing and measuring chronic multimorbidity in the older population: A proposal for its operationalization. J. Gerontol. A Biol. Sci. Med. Sci. 2017;72:1417–1423. doi: 10.1093/gerona/glw233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Yarnall A.J., Sayer A.A., Clegg A., Rockwood K., Parker S., Hindle J.V. New horizons in multimorbidity in older adults. Age Ageing. 2017;46:882–888. doi: 10.1093/ageing/afx150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Beard J.R., Officer A., de Carvalho I.A., Sadana R., Pot A.M., Michel J.P., Chatterji S. The world report on ageing and health: A policy framework for healthy ageing. Lancet. 2016;387:2145–2154. doi: 10.1016/S0140-6736(15)00516-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Taylor A.W., Price K., Gill T.K., Adams R., Pilkington R., Carrangis N., Wilson D. Multimorbidity—Not just an older person’s issue. Results from an australian biomedical study. BMC Public Health. 2010;10:718. doi: 10.1186/1471-2458-10-718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ding D., Rogers K., van der Ploeg H., Stamatakis E., Bauman A.E. Traditional and emerging lifestyle risk behaviors and all-cause mortality in middle-aged and older adults: Evidence from a large population-based australian cohort. PLoS Med. 2015;12:e1001917. doi: 10.1371/journal.pmed.1001917. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Jani B.D., Hanlon P., Nicholl B.I., McQueenie R., Gallacher K.I., Lee D., Mair F.S. Relationship between multimorbidity, demographic factors and mortality: Findings from the uk biobank cohort. BMC Med. 2019;17:74. doi: 10.1186/s12916-019-1305-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Lai F.T.T., Wong S.Y.S., Yip B.H.K., Guthrie B., Mercer S.W., Chung R.Y., Yeoh E.K. Multimorbidity in middle age predicts more subsequent hospital admissions than in older age: A nine-year retrospective cohort study of 121,188 discharged in-patients. Eur. J. Intern. Med. 2019;61:103–111. doi: 10.1016/j.ejim.2018.12.001. [DOI] [PubMed] [Google Scholar]
- 26.Wang L., Si L., Cocker F., Palmer A.J., Sanderson K. A systematic review of cost-of-illness studies of multimorbidity. Appl. Health Econ. Health Policy. 2018;16:15–29. doi: 10.1007/s40258-017-0346-6. [DOI] [PubMed] [Google Scholar]
- 27.National Institute for Health and Care Excellence . Multimorbidity: Assessment, Prioritisation and Management of Care for People with Commonly Occurring Multimorbidity. National Institute for Health and Care Excellence (UK); London, UK: 2016. Clinical Guidelines. [PubMed] [Google Scholar]
- 28.Wang X., Cao Y., Wu Y., Yang C., Song J., Tian Y., Hu Y. The prescription pattern of initial treatment for type 2 diabetes in beijing from 2011 to 2015. Medicine. 2019;98:e14370. doi: 10.1097/MD.0000000000014370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Wu Y., Yang C., Xi H., Zhang Y., Zhou Z., Hu Y. Prescription of antibacterial agents for acute upper respiratory tract infections in beijing, 2010–2012. Eur. J. Clin. Pharmacol. 2016;72:359–364. doi: 10.1007/s00228-015-1997-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Diederichs C., Berger K., Bartels D.B. The measurement of multiple chronic diseases–A systematic review on existing multimorbidity indices. J. Gerontol. A Biol. Sci. Med. Sci. 2011;66:301–311. doi: 10.1093/gerona/glq208. [DOI] [PubMed] [Google Scholar]
- 31.Global, regional, and national disability-adjusted life-years (DALYs) for 359 diseases and injuries and healthy life expectancy (HALE) for 195 countries and territories, 1990–2017: A systematic analysis for the global burden of disease study 2017. Lancet. 2018;392:1859–1922. doi: 10.1016/S0140-6736(18)32335-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Schubert I., Ihle P., Koster I. Internal confirmation of diagnoses in routine statutory health insurance data: Concept with examples and case definitions. Gesundheitswesen. 2010;72:316–322. doi: 10.1055/s-0030-1249688. [DOI] [PubMed] [Google Scholar]
- 33.Gellert P., von Berenberg P., Zahn T., Neuwirth J., Kuhlmey A., Drager D. Multimorbidity profiles in german centenarians: A latent class analysis of health insurance data. J. Aging Health. 2017 doi: 10.1177/0898264317737894. [DOI] [PubMed] [Google Scholar]
- 34.Sullivan G.M., Feinn R. Using effect size-or why the p value is not enough. J. Grad. Med. Educ. 2012;4:279–282. doi: 10.4300/JGME-D-12-00156.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Global, regional, and national incidence, prevalence, and years lived with disability for 354 diseases and injuries for 195 countries and territories, 1990–2017: A systematic analysis for the global burden of disease study 2017. Lancet. 2018;392:1789–1858. doi: 10.1016/S0140-6736(18)32279-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Zhang C., Zhang S. Association Rule Mining: Models and Algorithms. Springer-Verlag; Berlin, Germany: 2002. p. 228. [Google Scholar]
- 37.Chavent M., Kuentz-Simonet V., Liquet B., Saracco J. Clustofvar: An r package for the clustering of variables. J. Stat. Softw. 2012;50:16. doi: 10.18637/jss.v050.i13. [DOI] [Google Scholar]
- 38.Jin L., Guo X., Dou J., Liu B., Wang J., Li J., Yao Y. Multimorbidity analysis according to sex and age towards cardiovascular diseases of adults in northeast china. Sci. Rep. 2018;8:8607. doi: 10.1038/s41598-018-25561-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Zemedikun D.T., Gray L.J., Khunti K., Davies M.J., Dhalwani N.N. Patterns of multimorbidity in middle-aged and older adults: An analysis of the uk biobank data. Mayo Clin. Proc. 2018;93:857–866. doi: 10.1016/j.mayocp.2018.02.012. [DOI] [PubMed] [Google Scholar]
- 40.Alimohammadian M., Majidi A., Yaseri M., Ahmadi B., Islami F., Derakhshan M., Malekzadeh R. Multimorbidity as an important issue among women: Results of a gender difference investigation in a large population-based cross-sectional study in west asia. BMJ Open. 2017;7:e013548. doi: 10.1136/bmjopen-2016-013548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Arokiasamy P., Kowal P., Capistrant B.D., Gildner T.E., Thiele E., Biritwum R.B., Yawson A.E., Mensah G., Maximova T., Wu F., et al. Chronic noncommunicable diseases in 6 low- and middle-income countries: Findings from wave 1 of the world health organization’s study on global ageing and adult health (sage) Am. J. Epidemiol. 2017;185:414–428. doi: 10.1093/aje/kww125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Jones C.M., Boelaert K. The endocrinology of ageing: A mini-review. Gerontology. 2015;61:291–300. doi: 10.1159/000367692. [DOI] [PubMed] [Google Scholar]
- 43.Thompson A.E., Anisimowicz Y., Miedema B., Hogg W., Wodchis W.P., Aubrey-Bassler K. The influence of gender and other patient characteristics on health care-seeking behaviour: A qualicopc study. BMC Fam. Pract. 2016;17:38. doi: 10.1186/s12875-016-0440-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Boeckxstaens P., Peersman W., Goubin G., Ghali S., De Maeseneer J., Brusselle G., De Sutter A. A practice-based analysis of combinations of diseases in patients aged 65 or older in primary care. BMC Fam. Pract. 2014;15:159. doi: 10.1186/1471-2296-15-159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Kovari E., Kaposi A., Bekes G., Kiss Z., Kurucz R., Mandl P., Balint P.V. Comorbidity clusters in generalized osteoarthritis among female patients: A cross-sectional study. Semin. Arthritis Rheum. 2019 doi: 10.1016/j.semarthrit.2019.09.001. [DOI] [PubMed] [Google Scholar]
- 46.Zhang Y.M., Wang J., Liu X.G. Association between hypertension and risk of knee osteoarthritis: A meta-analysis of observational studies. Medicine. 2017;96:e7584. doi: 10.1097/MD.0000000000007584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Hall A.J., Stubbs B., Mamas M.A., Myint P.K., Smith T.O. Association between osteoarthritis and cardiovascular disease: Systematic review and meta-analysis. Eur. J. Prev. Cardiol. 2016;23:938–946. doi: 10.1177/2047487315610663. [DOI] [PubMed] [Google Scholar]
- 48.Fernandes G.S., Valdes A.M. Cardiovascular disease and osteoarthritis: Common pathways and patient outcomes. Eur. J. Clin. Invest. 2015;45:405–414. doi: 10.1111/eci.12413. [DOI] [PubMed] [Google Scholar]
- 49.Ricci G., Pirillo I., Tomassoni D., Sirignano A., Grappasonni I. Metabolic syndrome, hypertension, and nervous system injury: Epidemiological correlates. Clin. Exp. Hypertens. 2017;39:8–16. doi: 10.1080/10641963.2016.1210629. [DOI] [PubMed] [Google Scholar]
- 50.Ortega F.B., Lavie C.J., Blair S.N. Obesity and cardiovascular disease. Circ. Res. 2016;118:1752–1770. doi: 10.1161/circresaha.115.306883. [DOI] [PubMed] [Google Scholar]
- 51.Van Gaal L.F., Mertens I.L., De Block C.E. Mechanisms linking obesity with cardiovascular disease. Nature. 2006;444:875–880. doi: 10.1038/nature05487. [DOI] [PubMed] [Google Scholar]
- 52.Kadam U.T., Jordan K., Croft P.R. Clinical comorbidity in patients with osteoarthritis: A case-control study of general practice consulters in england and wales. Ann. Rheum. Dis. 2004;63:408–414. doi: 10.1136/ard.2003.007526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Atiquzzaman M., Karim M.E., Kopec J., Wong H., Anis A.H. Role of nonsteroidal antiinflammatory drugs in the association between osteoarthritis and cardiovascular diseases: A longitudinal study. Arthritis Rheumatol. 2019;71:1835–1843. doi: 10.1002/art.41027. [DOI] [PubMed] [Google Scholar]
- 54.Stallberg B., Janson C., Larsson K., Johansson G., Kostikas K., Gruenberger J.B., Lisspers K. Real-world retrospective cohort study arctic shows burden of comorbidities in swedish copd versus non-copd patients. NPJ Prim. Care Respir. Med. 2018;28:33. doi: 10.1038/s41533-018-0101-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Marshall D.A., Liu X., Barnabe C., Yee K., Faris P.D., Barber C., Lix L. Existing comorbidities in people with osteoarthritis: A retrospective analysis of a population-based cohort in alberta, canada. BMJ Open. 2019;9:e033334. doi: 10.1136/bmjopen-2019-033334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Wshah A., Guilcher S.J., Goldstein R., Brooks D. Prevalence of osteoarthritis in individuals with copd: A systematic review. Int. J. Chronic Obstr. Pulm. Dis. 2018;13:1207–1216. doi: 10.2147/COPD.S158614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Wang R., Yan Z., Liang Y., Tan E.C., Cai C., Jiang H., Qiu C. Prevalence and patterns of chronic disease pairs and multimorbidity among older chinese adults living in a rural area. PLoS ONE. 2015;10:e0138521. doi: 10.1371/journal.pone.0138521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Chen X., Zhou D., Shen J., Wu Y., Sun Q., Dong J., Yu J. Prevalence and causes of visual impairment in adults in binhu district, wuxi, china. Med. Sci. Monit. 2018;24:317–323. doi: 10.12659/MSM.908218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Yazdanyar A., Newman A.B. The burden of cardiovascular disease in the elderly: Morbidity, mortality, and costs. Clin. Geriatr. Med. 2009;25:563–577. doi: 10.1016/j.cger.2009.07.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Norhammar A. Diabetes and cardiovascular mortality: The impact of sex. Lancet Diabetes Endocrinol. 2018;6:517–519. doi: 10.1016/S2213-8587(18)30111-6. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.