Abstract
Glioblastoma is an aggressive primary tumor of the central nervous system. This review will focus on clinical developments and management of newly diagnosed disease, including a discussion about the incorporation of molecular features into the classification of glioblastoma. Such advances will continue to shape our thinking about the disease and how to best manage it. With regards to treatment, the role of surgical resection, radiotherapy, chemotherapy, and tumor-treating fields will be presented. Pivotal studies defining our current standard of care will be highlighted, as will key ongoing trials that may influence our management of glioblastoma in the near future.
Introduction
Glioblastoma, previously known as glioblastoma multiforme, is the most aggressive among infiltrative gliomas, a group of primary tumors arising from the central nervous system (CNS). Patients with this cancer type face significant morbidity and mortality, with over 13,000 deaths per year in the United States. Recent advances in our biological understanding of gliomas have led to important and substantive changes in their classification, in the identification of prognostic and predictive molecular markers, as well as in the therapeutic management of newly diagnosed glioma.
Classification
The term ‘glioblastoma multiforme’ was introduced in the 1926 classification system devised by Cushing and Bailey.[1] ‘Multiforme,’ which refers to a heterogenous, histological appearance and proliferation of multiple cell types, was abandoned from the revised nomenclature in the 2007 World Health Organization Classification of Tumors of the Central Nervous System, and is now simply called ‘glioblastoma’. [2] Glioblastoma is histologically defined by neoplastic cells with astrocytic characteristics and the presence of either endothelial proliferation—often in a glomeruloid morphology—and/or necrosis, which may resemble a pseudopalisading pattern (a false fence of neoplastic cells surrounding an area of necrotic tissue).
Due to its aggressive and highly proliferative course, glioblastoma is considered a grade IV astrocytoma. Molecular characterization has allowed for further refinement of the condition’s classification and is now an integral part of the diagnosis of malignant glioma.[3] Patients are classified into one of two distinct categories based on the presence or absence of mutations in the isocitrate dehydrogenase (IDH) 1 (IDH1) or IDH2 genes.
Primary glioblastoma/glioblastoma IDH wild-type (IDH-wt)
The majority of glioblastomas are IDH-wt and correspond to the longstanding clinical description of primary glioblastomas, which arise rapidly from non-neoplastic brain and progress quickly. In addition, a subgroup of lower-grade glioma may carry molecular features and signatures similar to glioblastoma, with a similarly aggressive natural course[4] for which an intensive treatment strategy is advocated. These facts stress that a microscopic histological diagnosis alone is insufficient to make informed and rational clinical decisions; therefore, it is essential that molecular alterations be integrated when diagnosing and managing glioma. This will potentially be of benefit in opening up appropriate clinical trial opportunities for this subset of patients in the future.[5]
Secondary glioblastoma/glioblastoma, IDH mutated
Up to 10% of patients with glioblastoma harbor a mutation in the IDH1 or IDH2 genes, an early event in gliomagenesis. Since these glioblastomas often arise from a prior, lower-grade glioma, they are considered secondary glioblastoma. In the past, both primary and secondary glioblastoma were considered to be the same clinical entity. However, recent studies clearly indicate that IDH-mutated glioblastoma has a more protracted natural course. As such, secondary glioblastomas are to be classified as a distinct biological and molecular entity for which different treatment strategies will ultimately be proposed. Former series of long-term survivors are commonly enriched for patients with IDH-mutated tumors.[3]
Epidemiology
Primary CNS tumors represent only 2% of adult cancer diagnoses; however, due to their location and often rapid clinical course, they are associated with high morbidity and mortality. About 50% of primary malignant CNS tumors are glioblastoma, with an incidence rate of 3.20 per 100,000 population. Incidence is higher in whites than in blacks (3.46 vs 1.79 per 100,000 population, respectively), with a 1.93:1 ratio (P < .05), a difference for which no biological explanation exists. Compared with whites, the incidence of glioblastoma is somewhat lower in Asians. The condition occurs more frequently in men than in women, with a 1.58:1 ratio (P < .05).[6] Over the last 3 decades, the incidence of glioblastoma in the United States has been relatively stable[7]; however, an aging population and better diagnostic tools may lead to a higher incidence of disease, as has been suggested in other countries[8]. Further study is needed to confirm changes in incidence, and, if present, to determine the causal factors.
Both environmental and patient-intrinsic factors may influence the risk of developing glioblastoma. An established risk factor is prior exposure to ionizing radiation to the CNS. The lag time between radiation and the development of glioblastoma may range from years to decades.[9–11] Unlike other cancers, there is no histologic or molecular signature that is pathognomonic for radiation-induced glioblastoma. The condition is observed in several hereditary cancer syndromes, including Lynch syndrome (with mutations in MSH2, MLH1, MSH6, PMS2) and Li-Fraumeni syndrome (with mutations in TP53).[7] While mutations in some tumor suppressor genes increase the risk of susceptibility, the presence of an allergic disorder appears to be associated with a decreased incidence of glioma, including glioblastoma, across a number of epidemiologic and preclinical studies.[7,12–14]
Pathophysiology
Despite extensive study, the cellular origin of glioblastoma and the pathophysiologic mechanism of gliomagenesis remain uncertain. Research on the cell of origin for glioblastoma often involves targeting different precursor cell populations in transgenic mouse models and explores the effects of these interventions on the development of glioma. However, contemporary thought favors primitive pluripotent cells, including neural stem cells, glial precursor cells, and oligodendrocyte precursor cells.[15] Numerous preclinical models have been conducted in this area, each with their favorable attributes and drawbacks.[16–19]
Research demonstrates that, amongst IDH-wt glioblastomas, there are spatial intratumoral differences in the mutational profile and clonality of tumor cells, with approximately half of the mutations being regionally exclusive. Distinct areas, found within these tumors, can exhibit a hypermutated phenotype. When present, mutations in the TERT gene appeared across all clones.[20] Recent studies utilizing xenografts in murine models have shown that these tumors consist of a slow-cycling population of stem-like cells which give rise to a rapidly dividing progenitor cell population, a proportion of whose daughter cells develop into terminal differentiated cells, supporting a hierarchical model of gliomagenesis. [21] A minority of the clonal population proves resistant to chemotherapy.[21] In turn, this cell population will require different treatments. When evaluated longitudinally, recurrent glioblastoma can accumulate additional mutations[22], and can appear similar to the primary tumor or may resemble a distinct subclonal population.[23,24] It is thought that this genomic heterogeneity is driven, at least in part, by the uneven cellular inheritance patterns of extra-chromosomal DNA. [25] As we garner a clearer understanding of the pathophysiology of gliomagenesis, new areas for potential therapeutic intervention will open up.

In glioblastoma, surgery plays an important diagnostic and therapeutic role: it offers tissue for diagnosis, immediate relief of the tumor-related mass effect and its associated symptoms, and potential cytoreduction.
In addition to the difficulties associated with treating heterogenous tumors, which evolve over the course of the disease and harbor treatment-resistant subpopulations of cells, the blood-brain barrier is another impediment to the effective treatment of these tumors. The blood-brain barrier is a dynamic, functional system which both precludes and modulates the traversing of systemically administered therapeutics into the CNS, including CNS tumors.[26] Numerous means have been utilized to overcome this obstacle. Thus far, the most successful have included systemically-administered drugs with adequate CNS penetration (eg, temozolomide) and locally delivered, alternating electrical fields (tumor-treating fields, TTFields). Direct intracranial application of both chemotherapy (eg, biodegradable carmustine–impregnated wafers) and radiation (eg, brachytherapy) has also been explored.
Intratumoral injection of oncolytic viruses and chimeric antigen receptor (CAR) T-cell therapies is a modern example of a similar strategy that is undergoing active investigation.[27,28] Disruption of the blood-brain barrier to facilitate transmission of a systemically-administered therapy has been under investigation for many decades. Initial studies utilized intra-arterially–administered agents.[29] A recent strategy being studied includes ultrasound to open up the barrier.[30] Another, which has had varying degrees of success, is avoiding the need to overcome the blood-brain barrier. The utilization of therapeutics whose direct activity occurs on the luminal side of the blood-brain barrier (eg, bevacizumab)[31]—or which act on the luminal side, with a goal of affecting function on the tumoral side of the barrier (eg, immune checkpoint inhibitors)—is another way to attempt to circumvent this obstacle. It is reasonable to surmise that more than one approach may prove to be successful.
Therapeutic Management
The therapeutic management of newly-diagnosed glioblastoma typically involves a four-pronged approach. First, surgical resection is completed to the maximal safe extent, thereby reducing the tumor load and establishing a histopathological and molecular diagnosis. Following surgery, adjuvant radiotherapy is given with concomitant and maintenance chemotherapy, as is treatment of alternating electrical fields.
Surgery
Surgery plays an important diagnostic and therapeutic role in the management of glioblastoma: it offers tissue for histological and molecular diagnosis, immediate relief of the tumor-related mass effect and its associated symptoms, and potential cytoreduction. However, due to the invariably infiltrative nature of the disease, even macroscopically complete resection is not curative. Numerous retrospective studies have evaluated the value of the extent of resection in glioblastoma. While early work suggested a dichotomous picture with a need for a substantial extent of resection of the contrast-enhancing tumor,[32] subsequent studies demonstrated the graded benefit of the extent of resection. [33,34] A more recent meta-analysis also supports a more extensive resection with improved 1- and 2-year survival rates as well as prolonged progression-free survival.[35] In low-grade glioma, the extent of resection is influenced by the area of increased signal on T2/fluid-attenuated inversion recovery (FLAIR) imaging.[36–39] Similarly, glioblastoma tumors are not limited to the area of enhancement but rather involve the area of increased T2/FLAIR signal. The extent of resection of this non-enhancing glioblastoma may also be of clinical impact, as demonstrated in a recent retrospective study.[40]
Although the association between extent of resection and survival has been reported and consistently confirmed in numerous studies, it is subject to several potential confounders, biases, and occult prognostic factors. While cytoreduction—the act of removing the bulk of tumor cells—may intuitively delay disease recurrence, the non-linear growth of tumor cells seen in glioblastoma could quickly recover the tumor burden that was removed during surgery, negating the survival benefit of small increments of cytoreduction. The durability of the effect of cytoreduction, and whether it leads to a survival benefit, is likely related to the rate of tumor cell proliferation. On the other hand, patients with neurological deficits have lower functional status, which ultimately impacts their overall survival. Thus, it is possible that relief of mass effect leading to improved functional status from resection might prolong survival in symptomatic patients, irrespective of cytoreduction. Finally, the tumor location may also reflect the underlying biology and dictate the natural history of the disease. Determination of the influence of these previously described variables on overall survival is complicated, as resectable tumors may have an overall better prognosis, regard-less of the actual extent of resection.
Resectable tumors often present in “silent areas of the brain” that tolerate injury for a long period of time prior to becoming symptomatic. In addition, resectable tumors, such as fronto-polar tumors, are more likely to harbor IDH1 mutations, which are associated with a better prognosis. In contrast, unresectable tumors, such as midline/diencephalic or brainstem tumors, often bear H3K27 mutations, which indicate an overall more aggressive biology and a worse prognosis.[41] Further dissection of the relationship between the extent of resection and survival requires controlling for tumor resectability per se. Yet, this complicated variable is difficult to capture by established scales, and is influenced by anatomical considerations as well as neurosurgeon-related factors.[42]
Maximizing extent of resection.
A number of technological advances have been developed to safely maximize the extent of resection, although their availability and usage may vary greatly. These techniques have become more widespread over time because, in addition to maximizing the extent of resection, they also optimize the safety of intra-axial brain tumor surgery. The major technological tools that surgeons use for improving the safety and accuracy of resection can be divided into three groups, as follows.
Intraoperative navigation technology.
This technology involves the use of volumetric imaging (eg, MRI or CT scan), which is used as a reference to locate a lesion/anatomical structure within the surgical field. Navigation involves an optical or electromagnetic system that uses a physical reference to register the location and position of a patient’s head in space, and allows real-time visualization of instruments within the images, which are loaded to a computer. These technologies help minimize the extent of the open craniotomy exposure; optimize a trajectory to access lesions that avoids critical neural structures, such as white matter pathways; and provides an anatomical reference during the operation. However, they are limited by the fact that the referenced images are not updated as resection progresses, and brain shift in space in relation to the skull makes this information less reliable as the case advances. To address this, several groups have introduced intraoperative MRI, which provides a real-time update of the field for navigation.[43,44] The true utility and cost-effectiveness ratio of intraoperative MRI remains a highly debated topic, as cost and added time during the procedure are not insignificant. The use of intraoperative ultrasound is a dynamic, easy to use, and affordable alternative for real-time imaging during surgery.
Electrophysiological monitoring and functional brain mapping.
Wilder Penfield and George Ojemann pioneered the use of electrodes to functionally map sensory and motor primary cortical regions and related subcortical circuits as the spinothalamic and corticospinal tracts to avoid postoperative deficits. [45–48] Over the last few decades, work by George Ojemann, Hugues Duffau, Mitchell Berger, and others has incorporated the routine use of awake brain mapping techniques, which have greatly improved the surveillance of motor circuits, language/comprehension, coordination, vision, and some higher cognitive functions by enabling them to be mapped and preserved.[49–53]
Fluorescent markers to maximize tumor visualization.
Fluorescent dyes—which are either metabolized by tumor cells, or accumulate in areas of blood-brain barrier breakdown—have been incorporated to maximize tumor tissue visualization in the operating room. This is helpful, as gross tumor tissue often has a similar texture or color as the surrounding edematous brain and is not always easy to distinguish under bright light. The use of 5-aminolevulinic acid under blue light allows the neurosurgeon to view residual tumor in real-time during surgery. A phase III trial demonstrated an improved rate of complete resection for contrast-enhancing tumor with 5-aminolevulinic acid compared with conventional microsurgery with white light (65% vs 36%; P < .0001) and 6-month progression-free survival (41% vs 21%; P = .0003). However, this did not translate into an improvement in overall survival.[54] Fluorescein has also been used to visualize enhancing tumor, as this dye leaks through areas with defective blood-brain barrier.[55,56] Here, no special light source is needed.
Radiation therapy
Radiotherapy has been shown to improve survival in glioblastoma and plays a key role in treatment. Modern conformal radiotherapy—which utilizes three-dimensional, computerized planning and multi-beam modulation—focally treats MRI-evident disease plus margin to a cumulative absorbed dose of 60 Gy. Given in daily doses of 1.8 to 2.0 Gy fractions, total treatment lasts approximately 6 weeks and is usually initiated 3 to 4 weeks after surgery. While some reports have suggested that delayed radiotherapy has a detrimental effect, other investigators have reported better outcomes; this question has yet to be definitively answered.[57,58]. Up to 6 to 7 weeks of postoperative recovery is considered acceptable as part of the established standard of care.
Earlier studies have examined doses of more than 60 Gy, some of which incorporated stereotactic radiosurgery. However, they failed to demonstrate improved outcomes with doses of up to 76 Gy.[59] An ongoing randomized phase II study, NRG BN001 (ClinicalTrials.gov identifier: NCT02179086), is evaluating dose escalation to 75 Gy compared with standard 60 Gy radiotherapy.[60] This study includes distinct cohorts utilizing photons or protons, and the primary endpoint is survival.
For elderly patients or those with sub-stantially altered performance status and poor prognosis, an abbreviated course of “hypofractionated” radiotherapy allows for a shortened overall treatment time. Long-term toxicity is of less concern in this population due to a commonly short survival. Hypofractionated radiation, which has been widely investigated, has been utilized to improve tolerability of radiotherapy (Table 1). Tumor volume often guides the selection of a radiation regimen because the risk of toxicity is theoretically greater with high vs low daily doses. Omitting radiotherapy (even less than the standard 60 Gy) leads to significantly worse survival compared with best supportive care alone.[61] Recent prospective data have demonstrated that abbreviated courses can also be safely and effectively combined with concurrent chemotherapy, as covered in the section below regarding treatment strategies for elderly patients.
Table 1.
Clinical Trials Investigating Various Radiation Dosing Regimens
| Author | Minimum Age | Fractional Dose | Total Dose | Duration | Concurrent Chemotherapy? | Median Survival |
|---|---|---|---|---|---|---|
| Baumann et al (1994)[83] | 65 y (or KPS ≤ 50) | 3.0 Gy | 30.0 Gy | 10 d | No | 6 mos |
| Roa et al (2004)[115] | 60 y | 2.67 Gy | 40.0 Gy | 15 d | No | 5.6 mos |
| Malmstrom et al (2012)[81] | 60 y | 3.4 Gy | 34.0 Gy | 10 d | No | 7.5 mos |
| Roa et al (2015)[84] | 65 y (or KPS 50–70) | 5.0 Gy | 25.0 Gy | 5 d | No | 7.9 mos |
| Perry et al (2017)[82] | 65 y | 2.67 Gy | 40.0 Gy | 15 d | Yes | 9.3 mos |
KPS = Karnofsky Performance Status.
A direct prospective comparison between full-course radiotherapy with concurrent and adjuvant chemotherapy vs abbreviated course radiotherapy with concurrent and adjuvant chemotherapy has not been conducted. In addition to an abbreviated course of radiotherapy, the shorter course also employs a shorter course of concomitant chemotherapy. This lack of direct comparison leaves an important question not fully answered. In many clinical practices, the full course of radiotherapy and chemotherapy will be utilized in elderly patients with good performance status.
Systemic therapy
We recently reviewed in detail the pivotal, late-phase trials that led to the current standard of care for patients with newly diagnosed glioblastoma.[62] These trials are summarized in Table 2. Temozolomide is a DNA-alkylating chemotherapy agent that is designed to readily cross the blood-brain barrier to achieve therapeutic concentrations in the brain. In 2005, a large, international, randomized, phase III trial (European Organisation for Research and Treatment of Cancer [EORTC] 26098/National Cancer Institute of Canada [NCIC] CE3) demonstrated prolonged survival when daily temozolomide chemotherapy (75 mg/m2 daily × 40–49 days) is added concomitantly to radiotherapy followed by 6 cycles of maintenance temozolomide (150–200 mg/m2 × 5/28 days). Based on this landmark trial, temozolomide/radiotherapy followed by maintenance temozolomide has become the world-wide standard of care for patients with a newly diagnosed glioblastoma.[63,64] Temozolomide adds a methyl group to the DNA residues at the O6, N3, and N7 positions that, if unrepaired, leads to DNA strand breaks and cytotoxicity. More than one-third of glioblastomas are deficient in methylguanine methyltransferase (MGMT), a repair protein that removes the methyl adduct from the O6 guanine position. This MGMT deficiency is via methylation (silencing) of the MGMT gene promoter, which leads to downregulated transcription. Glioblastoma patients with a silenced MGMT gene who are treated with an alkylating agent chemotherapy have a longer survival than those with an unmethylated MGMT and those treated with radiotherapy alone.[65] In studies of paired tissue samples, MGMT promoter methylation is relatively conserved from the newly diagnosed to progressive disease settings, with the majority of tumors maintaining an unchanged profile over time.[66,67] In mismatch repair–deficient conditions, the O6 guanine methyl adduct is tolerated and can be mutagenic. This may be a key mechanism in the development of glioma mutations due to temozolomide, and is described in low-grade glioma progressing to higher grade tumors as well as potentially in the development of a hypermutated phenotype.[68,69] The methyl adducts at N3 and N7 are addressed by the base excision repair mechanism.[70] Inhibition of this mechanism continues to undergo investigation in trials of poly (ADP-ribose) polymerase-1 (PARP) inhibitors.
Table 2.
Key Late-Phase Clinical Trials for Newly Diagnosed Glioblastoma
| Trial Designation | Author | Year | Phase | n | Age | Study Design | Median OS | Median PFS |
|---|---|---|---|---|---|---|---|---|
| N/A | Walker[116] | 1978 | III | 222 | NR |
HGG patients BCNU/RT+ BCNU vs BCNU vs RT vs Supportive care |
34.5 wks vs 18.5 wks vs 35 wks vs 14 wks | NR |
| N/A | Westphal[117] | 2003 | III | 240 | 18–65 y |
HGG patients BCNU-wafers + RT vs Placebo-wafers + RT |
13.9 mo vs 11.6 mo in HGG patients 13.5 mo vs 11.4 mo in GBM subgroup |
5.9 mo vs 5.9 mo in HGG patients |
| EORTC 26981/22981; NCIC CE3 |
Stupp[63–64] | 2005 | III | 573 | 18–71 y | RT/TMZ + TMZ vs RT | 14.6 mo vs 12.1 mo | 6.9 mo vs 5.1 mo |
| N/A | Keime-Guibert[61] | 2007 | N/A | 85 | ≥ 70y | RT/supportive care vs Supportive care | 29.1 wks vs 16.9 wks | 14.9 wks vs 5.4 wks |
| RTOG 0525 | Gilbert[72] | 2013 | III | 833 | ≥ 18 y | RT/TMZ + TMZ [150–200 mg/m2/d for 5/28 d) vs RT/TMZ + TMZ (75 mg/m2/d for 21/28 d] | 16.6 mo vs 14.9 mo | 5.5 mo vs 6.7 mo |
| RTOG 0825 | Gilbert[73] | 2014 | III | 637 | ≥ 18 y | RT/TMZ/bev + TMZ/bev vs RT/TMZ + TMZ | 15.7 mo vs 16.1 mo | 10.7 mo vs 7.3 mo |
| AVAglio | Chinot[74] | 2014 | III | 921 | ≥ 18 y | RT/TMZ/bev + TMZ/bev vs RT/TMZ + TMZ | 16.8 mo vs 16.7 mo | 10.6 mo vs 6.2 mo |
| CENTRIC EORTC 26071–22072 | Stupp[118] | 2014 | III | 545 | ≥ 18 y |
MGMT methylated RT/TMZ/cilengitide + TMZ/cilengitide vs RT/TMZ + TMZ |
26.3 mo vs 26.3 mo | 10.6 mo vs 7.9 mo |
| GLARIUS | Herrlinger[107] | 2016 | II | 182 | NR | RT/bev + bev/CPT11 vs RT/TMZ + TMZ | 16.6 mo vs 17.5 mo | 9.7 mo vs 5.99 mo |
| TMZ/rindopepimut vs TMZ | 21.1 mo vs 20.0 mo | 8.0 mo vs 7.4 mo | ||||||
| TMZ/TTFields vs TMZ | 20.9 mo vs 16.0 mo | 6.7 mo vs 4.0 mo | ||||||
| CCTG CE.6, EORTC 26062–22061, TROG 08.02 | Perry[82] | 2017 | III | 562 | ≥ 65 y | Short-course RT/TMZ + TMZ vs Short-course RT | 9.3 mo vs 7.6 mo | 5.3 mo vs 3.9 mo |
| RT/TMZ + TMZ vs RT/CCNU/TMZ + CCNU/TMZ | 31.4 mo vs 48.1 mo | 16.7 mo vs 16.7 mo |
bev = bevacizumab; BCNU-wafers = carmustine wafers; CCNU = lomustine; CCTG = Canadian Cancer Trials Group; CPT11 = irinotecan; EORTC = European Organisation for Research and Treatment of Cancer; GBM = glioblastoma; HGG = high-grade glioma, including glioblastoma; N/A = not available; NCIC = National Cancer Information Center; NR = not reported; OS = overall survival; PFS = progression-free survival; RT = radiotherapy; RTOG = Radiation Therapy Oncology Group; TMZ = temozolomide; TROG = Trans Tasman Radiation Oncology Group; TTFields = tumor-treating fields.
Optimal duration of adjuvant temozolomide chemotherapy.
The pivotal EORTC/NCIC study established a regimen of up to 6 adjuvant chemotherapy cycles. However, in the United States, the duration of chemotherapy may still extend for up to 12 cycles or more in non-progressive patients. While early treatment discontinuation is a concern due to the disease’s poor prognosis, cumulative toxicity, impaired bone marrow reserve for subsequent second-line chemotherapy, and increased risk of secondary malignancies are concerns with prolonged treatment. In some trials, treatment was allowed per local practice to be extended to up to 12 cycles. A pooled meta-analysis of individual patient outcomes data stemming from four randomized trials compared the duration of maintenance temozolomide chemotherapy (6 cycles vs 7+ cycles) among individuals who were non-progressive after 6 cycles.[71] While there was a slight improvement in progression-free survival, no difference in survival was seen for those who received 6 cycles vs more than 6 cycles of chemotherapy. This suggests that prolonged administration and dose intensification do not improve disease control. At this time, the value of temozolomide during radiotherapy, independent of adjuvant temozolomide in the treatment of glioblastoma, is unknown.
Alternative temozolomide dosing schedules.
Alternative dosing schedules have been investigated in the newly-diagnosed and recurrent disease settings. However, none of these regimens have been shown to be superior to the standard temozolomide dosing schedule. The randomized RTOG0525 study found no benefit with intensified maintenance chemotherapy. Patients were randomized at the end of chemoradiotherapy to either standard maintenance therapy (150–200 mg/m2/day × 5/28 days) or an intensified daily regimen (75 mg/m2/day × 21/28 days), effectively doubling the cumulative dose of chemotherapy. No difference in outcomes was noted, and a higher incidence of grade 3/4 toxicities was observed in the investigational arm.[72]
Hopes and disappointments with bevacizumab.
The addition of the antiangiogenic agent bevacizumab to radiotherapy and temozolomide has been explored in two phase III trials focusing on newly diagnosed glioblastoma[73,74] and one phase III trial focusing on recurrent glioblastoma[75]. The observed and expected improvement in progression-free survival based on imaging did not translate into any improvement in overall survival when bevacizumab was added. Unplanned post-hoc analyses found an association of improved overall survival in a molecularly-defined subset of patients.[76] The addition of bevacizumab to hypofractionated radiotherapy demonstrated no improvement in overall survival compared with hypofractionated radiotherapy alone in elderly (≥ 65 years) patients with newly diagnosed glioblastoma.[77] Based on the results of these trials, bevacizumab should not be administered as part of primary treatment of glioblastoma. Of note, some physicians utilize bevacizumab as a corticosteroid-sparing agent to decrease cerebral edema, so that treatment with standard radiotherapy and chemotherapy is feasible without high doses or prolonged use of corticosteroids.
De-escalation of treatment in the elderly.
De-escalation of therapeutic interventions has been extensively explored in the elderly and in frail populations with glioblastoma. This interest is driven by the overall brief survival of elderly glioblastoma patients, and thus the desire to shorten the duration of medical intervention. This topic has recently been reviewed in detail.[78,79] Several studies have prospectively evaluated abbreviated courses of radiotherapy in these patients (as covered earlier in the “Radiation Therapy” section).
Two large randomized trials have evaluated the exclusive administration of temozolomide chemotherapy in the elderly. Consistently, both trials demonstrated that withholding radiotherapy and instead treating patients with temozolomide alone may be an option for elderly patients with tumors harboring a methylated MGMT gene promoter, while this strategy is detrimental in the absence of MGMT methylation.[80,81] Monotherapy with temozolomide offers the advantage of an oral treatment regimen without the need for daily radiotherapy. The utilization of a short-course, hypofractionated radiotherapy regimen (of 40 Gy in 15 treatments) with concomitant temozolomide, followed by adjuvant temozolomide, was shown to improve outcomes in the elderly, which is consistent with the observed benefit reported 10 years earlier by the EORTC/NCIC in patients up to age 70 years. [82] The clinical circumstances, including chronologic age, performance status, concurrent medical problems, MGMT promoter methylation status, and logistical concerns should all be weighed during therapeutic decision-making for elderly patients with glioblastoma. In healthy, MGMT-methylated elderly patients with good performance status, a more aggressive approach, including full-course radiotherapy and temozolomide, can be considered.
Poor performance status.
Both de-escalation and escalation of care for patients with poor performance status have been considered. Many of these evaluations have been performed specifically in the elderly population, thus potentially limiting their generalizability to younger patients. De-escalation approaches attempt to limit the toxicity of treatment in a patient population that may not tolerate and is less likely to benefit from therapy. These approaches also attempt to shorten treatment duration as well as the amount of travel to the treatment facility, particularly for patients with limited mobility. The previously discussed abbreviated radiotherapy courses for elderly patients are also often used in the frail population with a poorer performance status; some prospective studies on abbreviated radiotherapy included patients on the basis of performance status alone.[83,84] The use of temozolomide chemotherapy alone has been studied in patients with poor performance status (Karnofsky Performance Score [KPS] of < 70); it was shown to be associated with an improvement in performance status or an improvement to the level of self-care (KPS ≥ 70) in one-third and one-fourth of patients, respectively. [85] Increasing the number of concomitant therapeutics has been performed with the goals of extending survival and improving functionality. One treatment intensification approach adds bevacizumab to the standard of care, relying on the corticosteroid-sparing effects described earlier. This approach has demonstrated only a transient improvement in performance status, and the data thus far do not justify its routine employment, as median overall survival remained short at 5.6 months (95% CI, 4.4–6.4).[86]
The addition of tumor-treating fields to maintenance temozolomide chemotherapy for newly-diagnosed glioblastoma patients has recently been incorporated as a new standard of care.
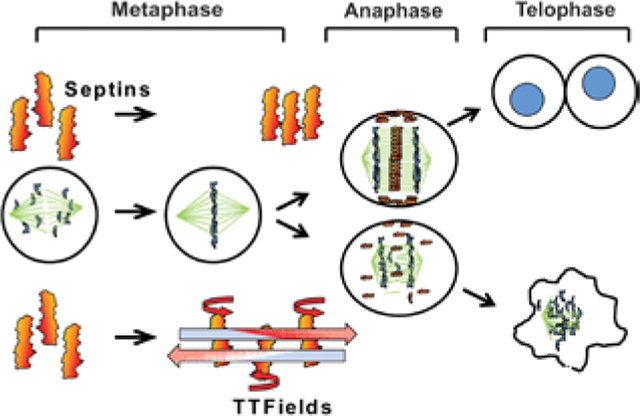
TTFields
The addition of TTFields to maintenance temozolomide chemotherapy for newly-diagnosed glioblastoma patients has recently been incorporated as a new standard of care.[87–89] TTFields are applied via multiple electrodes that are directly fixed to the scalp. These low-intensity, alternating electrical fields of 200 Hz interfere with polar organelles (eg, tubulins), which are required for normal cell division. Mitotic disruption ultimately leads to cell cycle arrest, aneuploidy, and apoptosis.[90,91] Additional mechanisms potentially contributing to therapy-associated effects include a disruption of organelles and an induction or modulation of the anti-glioma immune response.[92]
The effect of TTFields was evaluated in two large prospective, non-blinded randomized trials. In recurrent disease, TTFields failed to show superiority over best physicians’ choice (chemo)therapy in patients with recurrent glioblastoma. [93] In a pivotal large, randomized, phase III trial, 695 patients with newly diagnosed glioblastoma were randomized to receive adjuvant temozolomide and TTFields or standard maintenance therapy of temozolomide alone after the end of initial treatment with temozolomide/radiotherapy. Patients who received adjuvant temozolomide and TTFields fared much better than those treated with temozolomide alone. Survival was prolonged with a hazard ratio of 0.63 (95% CI, 0.52–0.76; P < .001), and durable survival was achieved in some patients. [88] This improvement was observed without a measurable negative impact on health-related quality of life (HRQL). [94] In the real-world setting, the rate of compliance among patients utilizing TTFields is high.[95] The primary toxicity noted in the trials was mild-to-moderate cutaneous toxicity, which typically resolves with minimal intervention.[96]
Impact of Other Medications
It has been hypothesized that certain medications commonly used to treat other conditions may potentially benefit patients with glioblastoma. These range from those prescribed for tumor-related conditions—such as epilepsy[97,98] and cerebral edema—to those which are independent of the neoplastic disease, including hypertension, hyperlipidemia, and venous thromboembolism[99,100]. Thus far, none have been proven to be beneficial. When thoroughly evaluated, none of the associations observed in several studies could be validated in larger cohorts, underscoring the importance of prospective (rather than retrospective) trials with strong biological hypotheses.
Corticosteroids
Corticosteroids are frequently used to decrease cerebral edema. Their off-target effects also lead to the suppression of immune system activity. Recent preclinical and clinical work suggests that these unfavorable effects contribute to shortened survival.[101] This is of particular importance as we evaluate the role of immunotherapeutic approaches for the treatment of glioma.[102] Despite the lack of a clear benefit in survival, bevacizumab has been shown to decrease the utilization of corticosteroids in patients with glioblastoma in numerous trials.[73,74,103–105] In routine clinical practice, functional improvement is often seen in association with radiographic improvement; however, it has not been proven to correlate with improved overall survival.
Future Directions
Efforts are continuously being undertaken to improve outcomes for patients with newly diagnosed glioblastoma. The diminishing return of second-and subsequent-line oncologic therapies supports the testing of promising new therapeutic approaches in the newly diagnosed population. This is underscored by the strong survival benefit seen among patients treated with TTFields in the newly diagnosed setting compared with those with progressive disease. A number of novel regimens are being studied in the newly diagnosed setting (Table 3). While many contemporary trials for newly diagnosed glioblastoma build upon the standard of care, as previously described, trials for patients with unmethylated MGMT promoter may omit temozolomide without losing treatment efficacy.[106–108]
Table 3.
Ongoing Late-Phase Clinical Trials for Newly Diagnosed Glioblastoma
| Trial Designation | NCT Number | Phase | Planned n | Novel Treatment | Treatment Regimen | Status |
|---|---|---|---|---|---|---|
| RTOG 3508A (Intellancel) | NCT02573324[111] | IIb/III | 640 | ABT-414, an EGFR-targeting antibody-drug conjugate |
EGFR amplified or EGFRvlll mutated RT/TMZ + TMZ vs RT/TMZ/ABT-414 + TMZ/ABT-414 |
Completed accrual |
| A071102 | NCT02152982[120] | II/III | 440 | Veliparib, a PARP inhibitor |
MGMT promoter methylated Post-RT/TMZ enrollment TMZ +/− TTFa vs TMZ/veliparib +/− TTFa |
Completed accrual |
| N/A | NCT00045968[121,122] | III | 348 | DCVax®-L, an autologous dendritic cell vaccine | Post-RT/TMZ enrollment TMZ/placebo vs TMZ/DCVax®-L |
Completed accrualb |
| CheckMate-548 | NCT02667587[112] | III | 693 | Nivolumab, a PD-1 antibody |
MGMT promoter methylated RT/TMZ + TMZ vs RT/TMZ/nivolumab + TMZ/nivolumab |
Completed accrual |
| CheckMate-498 | NCT02617589[111] | III | 550 | Nivolumab, a PD-l antibody |
MGMT promoter unmethylated RT/TMZ + TMZ vs RT/nivolumab + nivolumab |
Completed accrual |
| N/A | NCT03345095[123] | III | 750 | Marizomib, a proteasome inhibitor | RT/TMZ + TMZ vs RT/TMZ/marizomib + TMZ/marizomib | Open to accrual |
Decision to use TTFields is made prior to enrollment but is then continued throughout study treatment.
Preliminary results
DCVax®-L = lysate-pulsed dendritic cell vaccine; NCT = National Clinical Trial; PD-1 = programmed death ligand 1; RT = radiotherapy; RTOG = Radiation Therapy Oncology Group; TMZ = temozolomide; TTFields = tumor-treating fields.
EGFR remains an attractive therapeutic target, as it is frequently upregulated in glioblastoma, and its expression is associated with a worse prognosis; it is constitutionally activated in 30% of glioblastomas with a VIII variant. However, randomized trials targeting EGFR have repeatedly failed.[109,110] The addition of a novel peptide vaccine, rindopepimut, to the standard of care has been studied in a phase III trial. While the preclinical and early-phase studies held substantial promise, the phase III trial failed to demonstrate improved survival.[110] Phase III trial evaluation of the antibody drug conjugate depatuxizumab mafodotin (ABT-414) in combination with standard of care treatment for patients with EGFR-amplified, newly diagnosed glioblastoma is eagerly awaited.[111] Finally, the results of two separate trials evaluating the anti-PD1 monoclonal antibody nivolumab in newly diagnosed glioblastoma patients with unmethylated (CheckMate-498)[112] and methylated (CheckMate-548)[113] MGMT promoter are anticipated. Biomarkers that may help predict benefit from immuno-therapies[114] will require prospective evaluation, but may provide insight into the role of immunotherapeutic approaches in glioblastoma.
Conclusion
The therapeutic management of newly diagnosed glioblastoma is well-defined and includes surgery, radiation, temozolomide, and TTFields. Nuances to management in the elderly or frail exist; in these populations, treatment de-escalation is often considered on a patient-specific basis. The addition of other systemic therapies—such as antiangiogenic agents or other routinely administered medications, such as anti-epileptic or blood pressure agents—has not been shown to improve survival in newly diagnosed glioblastoma. Concerns exist, substantiated by both preclinical and clinical data, that corticosteroid utilization may negatively impact outcomes of immunotherapeutic approaches for the treatment of these patients. This will need to be carefully considered in the design, administration, and interpretation of clinical trials for this disease. As outcomes in glioblastoma remain poor, continued investigation into promising therapeutics is necessary.
FINANCIAL DISCLOSURE:
Dr. Lukas, Dr. Wainwright, Dr. Sonabend, and Dr. Stupp receive funding support from P50CA221747 SPORE for Translational Approaches to Brain Tumors. Dr. Wainwright receives funding support from the NIH/National Institute of Neurological Disorders and Stroke R01NS097851 grant. Dr. Lukas is a consultant for AbbVie, and has served as a consultant for NewLink Genetics and ReNeuron; he has also served on an advisory board for Monteris Medical; served as a medical editor for EBSCO and MedLink Neurology; and has presented CME board review courses for the American Physician Institute. Dr. Sonabend is a consultant for AbbVie. Dr. Stupp receives travel support from NovoCure; he also served on one-time advisory boards for Boehringer Ingelheim, Celgene, and Northwest Biotherapeutics.
Biographies

Dr. Lukas is an Associate Professor in the Department of Neurology and Associate Chief of Neuro-Oncology at the Lou and Jean Malnati Brain Tumor Institute at Robert H. Lurie Comprehensive Cancer Center of Northwestern University in Chicago, Illinois.

Dr. Wainwright is an Assistant Professor in the Department of Neurological Surgery at the Lou and Jean Malnati Brain Tumor Institute at Robert H. Lurie Comprehensive Cancer Center of Northwestern University in Chicago, Illinois.

Dr. Ladomersky is a Postdoctoral Fellow in the Department of Neurological Surgery at Northwestern University in Chicago, Illinois.

Dr. Sachdev is an Assistant Professor in the Department of Radiation Oncology at the Lou and Jean Malnati Brain Tumor Institute at Robert H. Lurie Comprehensive Cancer Center of Northwestern University in Chicago, Illinois.

Dr. Sonabend is an Assistant Professor in the Department of Neurological Surgery at the Lou and Jean Malnati Brain Tumor Institute at Robert H. Lurie Comprehensive Cancer Center of Northwestern University in Chicago, Illinois.

Dr. Stupp is a Professor in the Departments of Neurology, Neurological Surgery, and Medicine (Hematology & Oncology), and Chief of Neuro-Oncology, at the Lou and Jean Malnati Brain Tumor Institute at Robert H. Lurie Comprehensive Cancer Center of Northwestern University in Chicago, Illinois.
Contributor Information
Rimas V. Lukas, Department of Neurology and Associate Chief of Neuro-Oncology at the Lou and Jean Malnati Brain Tumor Institute at Robert H. Lurie Comprehensive Cancer Center of Northwestern University in Chicago, Illinois..
Derek A. Wainwright, Department of Neurological Surgery at the Lou and Jean Malnati Brain Tumor Institute at Robert H. Lurie Comprehensive Cancer Center of Northwestern University in Chicago, Illinois..
Erik Ladomersky, Department of Neurological Surgery at Northwestern University in Chicago, Illinois..
Sean Sachdev, Department of Radiation Oncology at the Lou and Jean Malnati Brain Tumor Institute at Robert H. Lurie Comprehensive Cancer Center of Northwestern University in Chicago, Illinois..
Adam M. Sonabend, Department of Neurological Surgery at the Lou and Jean Malnati Brain Tumor Institute at Robert H. Lurie Comprehensive Cancer Center of Northwestern University in Chicago, Illinois..
Roger Stupp, Departments of Neurology, Neurological Surgery, and Medicine (Hematology & Oncology), and Chief of Neuro-Oncology, at the Lou and Jean Malnati Brain Tumor Institute at Robert H. Lurie Comprehensive Cancer Center of Northwestern University in Chicago, Illinois..
References
- 1.Bailey P, Cushing H. A classification of the tumours of the glioma group on a histogenetic basis, with a correlated study of prognosis. Br J Surg. 1926;14:554–5. [Google Scholar]
- 2.Louis DN, Ohgaki H, Wiestler OD, et al. The 2007 WHO classification of tumors of the central nervous system. Acta Neuropathol. 2007;114:97–109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Louis DN, Perry A, Reifenberger G, et al. The 2016 World Health Organization classification of tumors of the central nervous system: a summary. 2016;131:803–20. [DOI] [PubMed] [Google Scholar]
- 4.Brat DJ, Aldape K, Colman H, et al. cIMPACT-NOW update 3: recommended diagnostic criteria for “diffuse astrocytic glioma, IDH-wildtype, with molecular features of glioblastoma, WHO grade IV”. Acta Neuropathol. 2018;136:805–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Velázquez Vega JE, Brat DJ. Incorporating advances in molecular pathology into brain tumor diagnostics. Adv Anat Pathol. 2018;25:143–71. [DOI] [PubMed] [Google Scholar]
- 6.Ostrum QT, Gittleman H, Liao P, et al. CBTRUS statistical report: primary brain and other central nervous system tumors diagnosed in the United States in 2010–2014. Neuro Oncol. 2017;19(suppl 5):v1–88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ostrum QT, Bauchet L, Davis FG, et al. The epidemiology of glioma in adults: a “state of the science” review. Neuro Oncol. 2014;16:896–913. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Philips A, Henshaw DL, Lamburn G, O’Carroll M. Brain tumors: rise in glioblastoma multiforme incidence in England 1995–2015 suggests an adverse environmental or lifestyle factor. J Environ Public Health. 2018. June 24 [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Elsamadicy AA, Babu R, Kirkpatrick JP, Adamson DC. Radiation-induced malignant gliomas: a current review. World Neurosurg. 2015;83:530–42. [DOI] [PubMed] [Google Scholar]
- 10.Taylor AJ, Little MP, Winter DL, et al. Population based risks of CNS tumors in survivors of childhood cancer. J Clin Oncol. 2010;28:5287–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Neglia JP, Robison LL, Stovall M, et al. New primary neoplasms of the central nervous system in survivors of childhood cancer: a report from the Childhood Cancer Survivor Study. J Natl Cancer Inst. 2006;98:1528–37. [DOI] [PubMed] [Google Scholar]
- 12.Krishnamachari B, Il’yasova D, Scheurer ME, et al. A pooled multisite analysis of the effects of atopic medical conditions in glioma risk in different ethnic groups. Ann Epidemiol. 2015;25:270–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Amirian ES, Zhou R, Wrensch MR, et al. Approaching a scientific consensus on the association between allergies and glioma risk: a report from the Glioma International Case-Control Study. Cancer Epidemiol Biomarkers Prev. 2016;25:282–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Schwartzbaum JA, Hwang K, Lawler S, et al. Allergy and inflammatory transcriptome is predominantly negatively correlated with CD133 expression in glioblastoma. Neuro Oncol. 2010;12:320–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Shao F, Liu C. Revisit the candidacy of brain cell types as the cell(s) of origin for human high-grade glioma. Front Mol Neurosci. 2018;11:48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Miyami M, Tomita H, Soeda A, et al. Current trends in mouse models of glioblastoma. J Neurooncol. 2017;135:423–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lei L, Sonabend AM, Guarnieri P, et al. Glioblastoma models reveal the connection between adult glial progenitors and the proneural phenotype. PLoS One. 2011. May 23 [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Sonabend AM, Bansal M, Guarnieri P, et al. The transcriptional regulatory network of proneural glioma determines the genetic alterations selected during tumor progression. Cancer Res. 2014;74:1440–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Verhaak RG, Hoadley KA, Purdom E, et al. Integrated genomic analysis identifies clinically relevant subtypes of glioblastoma characterized by abnormalities in PDGFRA, IDH1, EGFR, and NF1. Cancer Cell. 2010;17:98–110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Mahlokozera T, Vellimana AK, Li T, et al. Biological and therapeutic implications of multisector sequencing in newly diagnosed glioblastoma. Neur Oncol. 2018;20:472–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Lan X, Jorg DJ, Cavalli FMG, et al. Fate mapping of human glioblastoma reveals an invariant stem cell hierarchy. Nature. 2017;549:227–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Wang J, Cazzato E, Ladewig E, et al. Clonal evolution of glioblastoma under therapy. Nat Gent. 2016;48:768–76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kim H, Zheng S, Amini SS, et al. Whole-genome and multisector exome sequencing of primary an post-treatment glioblastoma reveals patterns of tumor evolution. Genome Res. 2015;25:316–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Neilsen BK, Sleightholm R, McComb R, et al. Comprehensive genetic alteration profiling in primary and recurrent glioblastoma. J Neurooncol. 2018. December 9 [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 25.deCarvalho AC, Kim H, Poisson LM, et al. Discordant inheritance of chromosomal and extrachromosomal DNA elements contributes to dynamic disease evolution in glioblastoma. Nat Genet. 2018;50:708–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Banks WA. From blood-brain barrier to blood-brain interface: new opportunities for CNS drug delivery. Nat Rev Drug Discov. 2016;15:275–92. [DOI] [PubMed] [Google Scholar]
- 27.Panek WK, Kane JR, Young JS, et al. Hitting the nail on the head: combining adenovirus-mediated virotherapy and immunomodulation for the treatment of glioma. Oncotarget. 2017;8:89391–405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Maxwell R, Luksik AS, Garzon-Muvdi T, Lim M. The potential of cellular- and viral-based immunotherapies for malignant glioma-dendritic cell vaccines, adoptive cell transfer, and oncolytic viruses. Curr Neurol Neurosci Rep. 2017;17:50. [DOI] [PubMed] [Google Scholar]
- 29.Joshi S, Ellis JA, Ornstein E, Bruce JN. Intrarterial drug delivery for glioblastoma multiforme: will the phoenix rise again? J Neurooncol. 2015;124:333–43. [DOI] [PubMed] [Google Scholar]
- 30.Carpentier A, Canney M, Vignopt A, et al. Clinical trial of blood-brain barrier disruption by pulsed ultra-sound. Sci Transl Med. 2016;8:343re2. [DOI] [PubMed] [Google Scholar]
- 31.Hundsberger T, Reardon DA, Wen PY. Angiogenesis inhibitors in tackling recurrent glioblastoma. Expert Rev Anticancer Ther. 2017;17:507–15. [DOI] [PubMed] [Google Scholar]
- 32.Lacroix M, Abi-Said D, Fourney DR, et al. A multivariate analysis of 416 patients with glioblastoma multiforme: prognosis, extent of resection, and survival. J Neurosurg. 2001;95:190–8. [DOI] [PubMed] [Google Scholar]
- 33.Sanai N, Polley MY, McDermott MW, et al. An extent of resection threshold for newly diagnosed glioblastoma. J Neurosurg. 2011;115:3–8. [DOI] [PubMed] [Google Scholar]
- 34.Chaichana KL, Jusue-Torres I, Navarro-Ramirez R, et al. Establishing percent resection and residual volume thresholds affecting survival and recurrence for patients with newly diagnosed intracranial glioblastoma. Neuro Oncol. 2014;16:113–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Brown TJ, Brennan MC, Li M, et al. Association of the extent of resection with survival in glioblastoma: a systematic review and meta-analysis. JAMA Oncol. 2016;2:1460–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Jakola AS, Myrmel KS, Kloster R, et al. Comparison of a strategy favoring early surgical resection vs a strategy favoring watchful waiting in low-grade gliomas. JAMA. 2012;308:1881–8. [DOI] [PubMed] [Google Scholar]
- 37.Xia L, Fang C, Chen G, Sun C. Relationship between the extent of resection and the survival of patients with low-grade gliomas: a systematic review and meta-analysis. BMC Cancer. 2018;18:48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Duffau H Long-term outcomes after supratotal resection of diffuse low-grade gliomas: a consecutive series with 11-year follow-up. Acta Neurochir (Wien). 2016;158:51–8. [DOI] [PubMed] [Google Scholar]
- 39.Smith JS, Chang EF, Lamborn KR, et al. Role of extent of resection in the long-term outcome of low-grade hemispheric gliomas. J Clin Oncol. 2008;26:1338–45. [DOI] [PubMed] [Google Scholar]
- 40.Kotrotsou A, Elakkad A, Sun J, et al. Multi-center study finds postoperative residual non-enhancing component of glioblastoma as a new determinant of patient outcome. J Neurooncol. 2018;139:125–33. [DOI] [PubMed] [Google Scholar]
- 41.Beiko J, Suki D, Hess KR, et al. IDH1 mutant malignant astrocytomas are more amenable to surgical resection and have a survival benefit associated with maximal surgical resection. Neuro Oncol. 2014;16:81–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Sonabend AM, Zacharia BE, Cloney MB, et al. Defining glioblastoma resectability through the wisdom of the crowd: a proof-of-principle study. Neurosurgery. 2017;80:590–601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Napolitano N, Vaz G, Lawson TM, et al. Glioblastoma surgery with and without intraoperative MRI at 3.0T. Neurochirurgie. 2014;60:143–50. [DOI] [PubMed] [Google Scholar]
- 44.Kuhnt D, Becker A, Ganslandt O, et al. Correlation of the extent of tumor volume resection and patient survival in surgery of glioblastoma multiforme with high field intraoperative MRI guidance. Neuro Oncol. 2011;13:1339–48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Penfield W The electrode, the brain and the mind. Z Neurol. 1972;201:297–309. [DOI] [PubMed] [Google Scholar]
- 46.Penfield W Combined regional and general anesthesia for craniotomy and cortical exploration. Part I. Neurosurgical considerations. Int Anesthesiol Clin. 1986;24:1–11. [DOI] [PubMed] [Google Scholar]
- 47.Keles GE, Lundin DA, Lamborn KR, et al. Intraoperative subcortical stimulation mapping for hemispherical perirolandic gliomas located within or adjacent to the descending motor pathways: evaluation of morbidity and as-sessment of functional outcomes in 294 patients. J Neurosurg. 2004;100:369–75. [DOI] [PubMed] [Google Scholar]
- 48.Farrell DF, Leeman S, Ojemann GA. Study of the human visual cortex: direct cortical evoked potentials and stimulation. J Clin Neurophysiol. 2007;24:1–10. [DOI] [PubMed] [Google Scholar]
- 49.Ojemann G, Ojemann J, Lettich E, Berger MS. Cortical language localization in left, dominant hemisphere. An electrical stimulation mapping investigation in 117 patients. 1989. J Neurosurg. 2008;108:411–21. [DOI] [PubMed] [Google Scholar]
- 50.Engel AK, Moll CK, Fried I, Ojemann GA. Invasive recordings from the human brain: clinical insights and beyond. Nat Rev Neurosci. 2005;6:35–47. [DOI] [PubMed] [Google Scholar]
- 51.Duffau H Mapping the connectome in awake surgery for gliomas: an update. J Neurosurg Sci. 2017;61:612–30. [DOI] [PubMed] [Google Scholar]
- 52.Southwell DG, Riva M, Jordan K, et al. Language outcomes after resection of dominant inferior parietal lobule gliomas. J Neurosurg. 2017;127:781–9. [DOI] [PubMed] [Google Scholar]
- 53.Sanai N, Mirzadeh Z, Berger MS. Functional outcome after language mapping for glioma resection. N Engl J Med. 2008;358:18–27. [DOI] [PubMed] [Google Scholar]
- 54.Stummer W, Pichelmeier U, Meinel T, et al. Fluorescence-guided surgery with 5-aminolevulinic acid for resection of malignant glioma: a randomized controlled multicentre phase III trial. Lancet Oncol. 2006;7:392–401. [DOI] [PubMed] [Google Scholar]
- 55.Bowden SG, Neira JA, Gill BJA, et al. Sodium fluorescein facilitates guided sampling of diagnostic tumor tissue in nonenhancing gliomas. Neurosurgery. 2018;82:719–27. [DOI] [PubMed] [Google Scholar]
- 56.Catapano G, Sgulò FG, Seneca V, et al. Fluorescein-guided surgery for high-grade glioma resection: an intraoperative “contrast enhancer”. World Neurosurg. 2017;104:239–47. [DOI] [PubMed] [Google Scholar]
- 57.Han SJ, Englot DJ, Birk H, et al. Impact of timing of concurrent chemoradiation for newly diagnosed glioblastoma: a critical review of current evidence. Neurosurgery. 2016;62(suppl 1):160–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Han SJ, Rutledge WC, Molinaro AM, et al. The effect of timing of concurrent chemoradiation in patients with newly diagnosed glioblastoma. Neurosurgery. 2015;77:248–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Kirkpatrick JP, Laack NN, Shih HA, Gondi V. Management of GBM: a problem of local recurrence. J Neurooncol. 2017;134:487–93. [DOI] [PubMed] [Google Scholar]
- 60.NIH U.S. National Library of Medicine, ClinicalTrials.gov. Dose-escalated photon IMRT or proton beam radiation therapy versus standard-dose radiation therapy and temozolomide in treating patients with newly diagnosed glioblastoma. ClinicalTrials.gov identifier: NCT02179086. https://clinicaltrials.gov/ct2/show/NCT02179086. Ac-cessed February 7, 2019.
- 61.Keime-Guibert F, Chinot O, Taillandier L, et al. Radiotherapy for glioblastoma in the elderly. N Engl J Med. 2007;356:1527–35. [DOI] [PubMed] [Google Scholar]
- 62.Lukas RV, Mrugala MM. Pivotal therapeutic trials for infiltrating gliomas and how they affect clinical practice. Neurooncol Pract. 2017;4:209–19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Stupp R, Mason WP, van den Bent MJ, et al. Radiotherapy plus concomitant and adjuvant temozolomide for glioblastoma. N Engl J Med. 2005;352:987–96. [DOI] [PubMed] [Google Scholar]
- 64.Stupp R, Hegi ME, Mason WP, et al. Effects of radiotherapy with concomitant and adjuvant temozolomide versus radiotherapy alone on survival in glioblastoma in a randomised phase III study: 5-year analysis of the EORTC-NCIC trial. Lancet Oncol. 2009;10:459–66. [DOI] [PubMed] [Google Scholar]
- 65.Hegi ME, Diserens AC, Gorlia T, et al. MGMT gene silencing and benefit from temozlomide in glioblastoma. N Engl J Med. 2005;352:997–1003. [DOI] [PubMed] [Google Scholar]
- 66.Felsberg J, Thon N, Eigenbrod S, et al. Promoter methylation and expressionof MGMT and the DNA mismatch repair genes MLH1, MSH2, MSH6, and PMS2 in paired primary and recurrent glioblastomas. Int J Cancer. 2011;129:659–70. [DOI] [PubMed] [Google Scholar]
- 67.O’Regan CJ, Kearney H, Beausang A, et al. Temporal stability of MGMT promoter methylation in glioblastoma patients undergoing STUPP regimen. J Neurooncol. 2018;137:233–240. [DOI] [PubMed] [Google Scholar]
- 68.Choi S, Yu Y, Grimmer MR, et al. Temozlomide-associated hypermutation in gliomas. Neuro Oncol. 2018;20:1300–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Van Thuijl HF, Mazor T, Johnson BE, et al. Evolution of DNA repair defects during malignant progression of low-grade gliomas after temozolomide treatment. Acta Neuropathol. 2015;129:597–607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Zhang J, Stevens MF, Bradshaw TD. Temozolomide: mechanisms of action, repair, and resistance. Curr Mol Pharmacol. 2012;5:102–14. [DOI] [PubMed] [Google Scholar]
- 71.Blumenthal DT, Gorlia T, Gilbert MR, et al. Is more better? The impact of extended adjuvant temozolomide in newly diagnosed glioblastoma: a secondary analysis of EORTC and NRG Oncology/RTOG. Neuro Oncol. 2017;19:1119–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Gilbert MR, Wang M, Aldape KD, et al. Dose-dense temozolomide for newly diagnosed glioblastoma: a randomized phase III clinical trial. J Clin Oncol. 2013;31:4085–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Gilbert MR, Dignan JJ, Armstrong TS, et al. A randomized trial of bevacizumab for newly diagnosed glioblastoma. N Engl J Med. 2014;370:699–708. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Chinot OL, Wick W, Mason W, et al. Bevacizumab plus radiotherapy-temozolomide for newly diagnosed glioblastoma. N Engl J Med. 2014;370:709–22. [DOI] [PubMed] [Google Scholar]
- 75.Wick W, Gorlia T, Bendszus M, et al. Lomustine and bevacizumab in progressive glioblastoma. N Engl J Med. 2017;377:1954–63. [DOI] [PubMed] [Google Scholar]
- 76.Sandmann T, Bourgon R, Garcia J, et al. Patients with proneural glioblastoma may derive overall survival benefit from the addition of bevacizumab to first-line radiotherapy and temozolomide: a retrospective analysis of the AVAglio trial. J Clin Oncol. 2015;33:2735–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Wirsching HG, Tabatabai G, Roelcke U, et al. Bevacizumab plus hypofractionated radiotherapy versus radiotherapy alone in elderly patients with glioblastoma: the randomized, open-label, phase II ARTE trial. Ann Oncol. 2018;29:1423–30. [DOI] [PubMed] [Google Scholar]
- 78.Young JS, Chmura SJ, Wainwright DA, et al. Management of glioblastoma in elderly patients. J Neurol Sci. 2017;380:250–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Das S, Kim AH, Chang S, Berger MS. Management of elderly patients with glioblastoma after CE.6. Front Oncol. 2017;7:196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Wick W, Platten M, Meisner C, et al. Temozolomide chemotherapy alone versus radiotherapy alone for malignant astrocytoma in the elderly: the NOA-08 randomised, phase III trial. Lancet Oncol. 2012;13:707–15. [DOI] [PubMed] [Google Scholar]
- 81.Malmstrom A, Gronberg BH, Marosi C, et al. Temozolomide versus standard 6 week radiotherapy versus hypofractionated radiotherapy in patients older than 60 years with glioblastoma: the Nordic, randomized phase 3 trial. Lancet Oncol. 2012;13:916–26. [DOI] [PubMed] [Google Scholar]
- 82.Perry JR, Laperriere N, O’Callaghan CJ, et al. Short-course radiation plus temozolomide in elderly patients with glioblastoma. N Engl J Med. 2017;376:1027–37. [DOI] [PubMed] [Google Scholar]
- 83.Bauman GS, Gaspar LE, Fisher BJ, et al. A prospective study of short-course radiotherapy in poor prognosis glioblastoma multiforme. Int J Radiat Oncol Biol Phys. 1994;29:835–9. [DOI] [PubMed] [Google Scholar]
- 84.Roa W, Kepka L, Kumar N, et al. International Atomic Energy Agency randomized phase III study of radiation therapy in elderly and/or frail patients with newly diagnosed glioblastoma multiforme. J Clin Oncol. 2015;33:4145–50. [DOI] [PubMed] [Google Scholar]
- 85.Gallego Perez-Larraya J, Ducray F, Chinot O, et al. Temozolomide in elderly patients with newly diagnosed glioblastoma and poor performance status: an ANOCEF phase II trial. J Clin Oncol. 2011;29:3050–5. [DOI] [PubMed] [Google Scholar]
- 86.Reyes-Botero G, Cartalat-Carel S, Chinot OL, et al. Temozolomide plus bevacizumab in elderly patients with newly diagnosed glioblastoma and poor performance status: an ANOCEF phase II trial (ATAG). Oncologist. 2018;23:524–e44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Stupp R, Taillibert S, Kanner AA, et al. Maintenance therapy with tumor-treating fields plus temozlomide alone for glioblastoma: a randomized clinical trial. JAMA. 2015;314:2535–43. [DOI] [PubMed] [Google Scholar]
- 88.Stupp R, Taillibert S, Kanner A, et al. Effect of tumor-treating fields plus maintenance temozolomide vs maintenance temozolomide alone on survival in patients with glioblastoma: a randomized clinical trial. JAMA. 2017;318:2306–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Nabors LB, Portnow J, Ammiraiti M, et al. NCCN Guidelines Insights: Central Nervous System Cancers, Version 1.2017. J Natl Compr Canc Netw. 2017;15:1331–45. [DOI] [PubMed] [Google Scholar]
- 90.Mrugala MM, Ruzevick J, Zlomanczuk P, Lukas RV. Tumor treating fields in neuro-oncological practice. Curr Oncol Rep. 2017;19:53. [DOI] [PubMed] [Google Scholar]
- 91.Hottinger AF, Pacheco P, Stupp R. Tumor treating fields: a novel treatment modality and its use in brain tumors. Neuro Oncol. 2016;18:1338–49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Zhu P, Zhu JJ. Tumor treating fields: a novel and effective therapy for glioblastoma: mechanism, efficacy, safety, and future perspectives. Chin Clin Oncol. 2017;6:41. [DOI] [PubMed] [Google Scholar]
- 93.Stupp R, Wong ET, Kanner AA, et al. NovoTTA-100A versus physicians’ choice chemotherapy in recurrent glioblastoma: a randomized phase III trial of a novel treatment modality. Eur J Cancer. 2012;48:2192–202. [DOI] [PubMed] [Google Scholar]
- 94.Taphoorn MJB, Dirven L, Kanner AA, et al. Influence of treatment of tumor-treating fields on health-related quality of life of patients with newly diagnosed glioblastoma: a secondary analysis of a randomized clinical trial. JAMA Oncol. 2018. April 1 [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Onken J, Staub-Bartlett F, Vajkocy P, Misch M. Acceptance and compliance of TTFields treatment among high-grade glioma patients. J Neurooncol. 2018;139:177–84. [DOI] [PubMed] [Google Scholar]
- 96.Lukas RV, Ratterman KL, Wong ET, Villano JL. Skin toxicities associated with tumor treating fields: case based review. J Neurooncol. 2017;135:593–9. [DOI] [PubMed] [Google Scholar]
- 97.Weller M, Gorlia T, Cairncross JD, et al. Prolonged survival with valproic acid use in the EORTC/NCIC temozolomide trial of glioblastoma. Neurology. 2011;77:1156–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Happold C, Gorlia T, Chinot O, et al. Does valproic acid or levitaracetam improve survival in glioblastoma? A pooled analysis of prospective clinical trials in newly diagnosed glioblastoma. J Clin Oncol. 2016;34:731–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Happold C, Gorlia T, Nabors LB, et al. Do statins, ACE inhibitors, or sartans improve outcome in primary glioblastoma? J Neurooncol. 2018;138:163–71. [DOI] [PubMed] [Google Scholar]
- 100.Le Rhun E, Genbrugge E, Stupp R, et al. Associations of anticoagulant use with outcome in newly diagnosed glioblastoma. Eur J Cancer. 2018;101:95–104. [DOI] [PubMed] [Google Scholar]
- 101.Pitter KL, Tamagno I, Alikhanyan K, et al. Corticosteroids compromise survival in glioblastoma. Brain. 2016;139(pt 5):1458–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Giles AJ, Hutchinson MND, Sonnemann HM, et al. Dexamethasone-induced immunosuppression: mechanisms and implications for immunotherapy. J Immunother Cancer. 2018;6:51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Vredenburgh JJ, Cloughesy T, Samant M, et al. Corticosteroid use in patients with glioblastoma at first or second relapse treated with bevacizumab in the BRAIN study. Oncologist. 2010;15:1329–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Ananthnarayan S, Bahng J, Roring J, et al. Time course of imaging changes of GBM during extended bevacizumab treatment. J Neurooncol. 2008;88:339–47. [DOI] [PubMed] [Google Scholar]
- 105.Ellingson BM, Cloughesy TF, Lai A, et al. Quantitative volumetric analysis of conventional MRI response in recurrent glioblastoma treated with bevacizumab. Neuro Oncol. 2011;13:401–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Hegi ME, Stupp R. Witholding temozlomide in glioblastoma patients with unmethylated MGMT promoter—still a dilemma? Neuro Oncol. 2015;17:1425–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Herrlinger U, Schafer N, Steibach JP, et al. Bevacizumab plus irinotecan versus temozolomide in newly diagnosed O6-methylguanine-DNA methylatransferase nonmethylated glioblastoma: the randomized GLARIUS trial. J Clin Oncol. 2016;34:1611–9. [DOI] [PubMed] [Google Scholar]
- 108.Wick W, Gorlia T, Bady P, et al. Phase II study of radiotherapy and temsirolimus versus radiochemotherapy with temozolomide in patients with newly diagnosed glioblastoma without MGMT promoter hypermethylation (EORTC 26082). Clin Cancer Res. 2016;22:4797–4806. [DOI] [PubMed] [Google Scholar]
- 109.Westphal M, Heese O, Steinbach JP, et al. A randomized, open label phase 3 trial of nimotuzumab, an anti-epidermal growth factor receptor monoclonal antibody in the treatment of newly diagnosed adult glioblastoma. Eur J Cancer. 2015;51:522–32. [DOI] [PubMed] [Google Scholar]
- 110.Weller M, Butowski N, Tran DD, et al. Rindopepimut and temozolomide for patients with newly diagnosed, EGFRvIII-expressing glioblastoma (ACT IV): a randomised, double blind, international phase 3 trial. Lancet Oncol. 2017;18:1373–85. [DOI] [PubMed] [Google Scholar]
- 111.NIH U.S. National Library of Medicine, ClinicalTrials.gov. A study of ABT-414 in subjects with newly diagnosed glioblastoma (GBM) with epidermal growth factor receptor (EGFR) amplification (Intellance1). https://clinicaltrials.gov/ct2/show/NCT02573324. Accessed February 26, 2019.
- 112.NIH U.S. National Library of Medicine, ClinicalTrials.gov. An investigational immuno-therapy study of nivolumab compared to temozolomide, each given with radiation therapy, for newly-diagnosed patients with glioblastoma (GBM, a malignant brain cancer) (CheckMate 498). https://clinicaltrials.gov/ct2/show/NCT02617589. Accessed February 26, 2019.
- 113.NIH U.S. National Library of Medicine, ClinicalTrials.gov. An investigational immuno-therapy study of temozolomide plus radiation therapy with nivolumab or placebo, for newly diagnosed patients with glioblastoma (GBM, a malignant brain cancer) (CheckMate548). https://clinicaltrials.gov/ct2/show/NCT02667587. Accessed February 26, 2019.
- 114.Zhao J, Chen AX, Gartell RD, et al. Immune and genomic correlates of response to anti-PD-1 immunotherapy in glioblastoma. Nat Med. 2019. February 11 [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Roa W, Brasher PM, Bauman G, et al. Abbreviated course of radiation therapy in older patients with glioblastoma multiforme: a prospective randomized clinical trial. J Clin Oncol. 2004;22:1583–8. [DOI] [PubMed] [Google Scholar]
- 116.Walker MD, Alexander E Jr, Hunt WE, et al. Evaluation of BCNU and/or radiotherapy in the treatment of anaplastic gliomas. A cooperative clinical trial. J Neurosurg. 1978;49:333–43. [DOI] [PubMed] [Google Scholar]
- 117.Westphal M, Hilt DC, Bortey E, et al. A phase 3 trial of local chemotherapy with biodegradable carmustine (BCNU) wafers (Glaidel wafers) in patients with primary malignant glioma. Neuro Oncol. 2003;5:79–88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Stupp R, Hegi ME, Gorlia T, et al. Cilengitide combined with standard treatment for patients with newly diagnosed glioblastoma with methylated MGMT promoter (CENTRIC EORTC 26071–22072 study): a multicentre, randomized, open-label, phase 3 trial. Lancet Oncol. 2014;15:1100–8. [DOI] [PubMed] [Google Scholar]
- 119.Herrlinger U, Tzaridis T, Mack F, et al. Phase III trial of CCNU/temozolomide (TMZ) combination therapy vs. standard TMZ therapy for newly diagnosed MGMT-methylated glioblastoma patients: the randomized, open-label CeTeG/NOA-09 trial. Lancet. 2019;393:678–88. [DOI] [PubMed] [Google Scholar]
- 120.NIH U.S. National Library of Medicine, ClinicalTrials.gov. Temozolomide with or without veliparib in treating patients with newly diagnosed glioblastoma multiforme. https://clinicaltrials.gov/ct2/show/NCT02152982. Accessed February 26, 2019.
- 121.Liau LM, Ashkan A, Tran DD, et al. First results on survival from a large phase 3 clinical trial of an autologous dendritic cell vaccine in newly diagnosed glioblastoma. J Transl Med. 2018;16:142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Liau LM, Ashkan K, Tran DD, et al. Correction to: First results on survival from a large phase 3 clinical trial of an autologous dendritic cell vaccine in newly diagnosed glioblastoma. J Transl Med. 2018;16:179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.NIH U.S. National Library of Medicine, ClinicalTrials.gov. A phase III trial of with marizomib in patients with newly diagnosed glioblastoma. https://clinicaltrials.gov/ct2/show/NCT03345095. Accessed February 26, 2019.


