Dear Editor,
The outbreak of coronavirus disease (COVID-19) was first reported in Wuhan, the capital city of Hubei province, and may lead to severe pneumonia and acute respiratory distress syndrome (ARDS). Extracorporeal membrane oxygenation (ECMO), as a temporary life support technique for refractory respiratory or cardiac failure, has been applied in COVID-19 patients [1]. However, the impact of ECMO on outcomes from COVID-19 was controversial. Referring to the present case series and the COVID-19 cohort in China, the mortality of patients undergoing ECMO ranged from 42 to 83% [2, 3]. The Chinese Society of Extracorporeal Life Support (CSECLS) performed a survey of ECMO programs for COVID-19 in China, aimed at investigating the program organization and the potential factors associated with outcomes during the pandemic.
This voluntary survey was disseminated via e-mail and WeChat to 365 ECMO programs registered with the CSECLS on March 23, 2020. Through March 29, we had received 350 individual responses from 270 (74.0%) ECMO programs in total. When analyzing program characteristics, the program directors’ or coordinators’ responses were adopted.
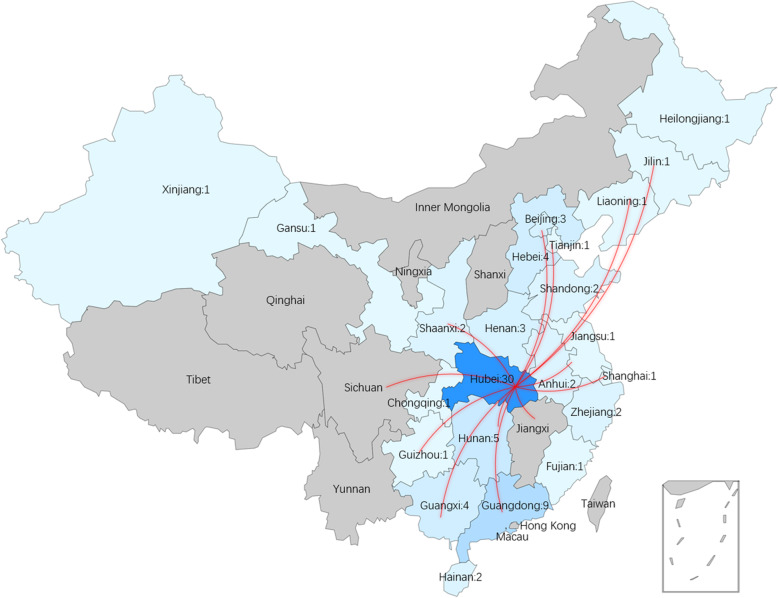
One hundred eleven individual responses from 79 ECMO programs (30 in Hubei and 49 outside Hubei) applied ECMO in patients with COVID-19 pneumonia and ARDS were analyzed. Respondents included those located in 25 provinces within China before COVID-19 outbroke. Twenty-seven respondents belonged to the medical assistance teams which were dispatched to aid Hubei and 39 respondents aided other hospitals in their original province, while 45 respondents managed COVID-19 patients with ECMO within their original hospitals. Fifty-one of 79 ECMO programs (15 in Hubei and 36 outside Hubei) were organized temporarily in response to the crisis. Thirty-two hospitals with temporary ECMO programs did not have any ECMO cases before. The geographic distribution of the 79 ECMO programs and responders’ aid to Hubei is shown in Fig. 1. Patient management characteristics are illustrated in Table 1. Compared with ECMO programs in Hubei, more programs outside Hubei initiated ECMO in older patients (36.7% vs 3.3% in age ≥ 75, p = 0.001; 55.1% vs 26.7% in age 65–74, p = 0.014).
Fig. 1.
The geography distribution of ECMO programs for COVID-19 in China. The total 79 ECMO programs for COVID-19 by province (with the number of ECMO programs in each province) and respondents’ aid to Hubei from other provinces (red lines) were shown
Table 1.
Patient management responded by ECMO programs
| Question | Total ECMO programs, n = 79 [n (%)] |
|---|---|
| ECMO cases for COVID-19 | |
| ≤ 5 | 68 (86.1%) |
| > 5 | 11 (13.9%) |
| The source of ECMO patients for COVID-19 | |
| In-hospital patient | 62 (78.5%) |
| Transferred from other hospitals, then initiated ECMO | 24 (30.4%) |
| Initiated ECMO in other hospitals, then transferred | 8 (10.1%) |
| Initiated ECMO in COVID-19 patients whose age | |
| < 65 | 54 (68.4%) |
| 65–74 | 35 (44.3%) |
| ≥ 75 | 19 (24.1%) |
| Therapy before ECMO initiation | |
| Recruitment maneuvers | 65 (82.3%) |
| Neuromuscular blockers | 64 (81.0%) |
| Prone position | 61 (77.2%) |
| Therapy after ECMO initiation | |
| Recruitment maneuvers | 56 (70.9%) |
| Neuromuscular blockers | 61 (77.2%) |
| Prone position | 61 (77.2%) |
| Bronchoscopy | 59 (74.7%) |
| CT scan | 40 (50.6%) |
ECMO extracorporeal membrane oxygenation, CT computer tomography
Our findings provide evidence of the current condition of ECMO programs for COVID-19 across China. Fifty-one ECMO programs were newly organized. It was most efficient to rearrange medical workers and resources rather than starting new ECMO programs amid the crisis, given that inexperienced ECMO programs and hospitals might lead to unfavorable outcomes. Since ECMO is a complicated and high-risk therapy, adequate training and high-volume experience are indispensable [4].
We also found a difference in age between ECMO patients in Hubei and outside Hubei. Seventy-five percent of COVID-19 cases in China were diagnosed in Hubei [5]. With limited medical resources in Hubei, patients with a higher likelihood of survival were chosen to receive ECMO, namely younger patients. However, medical resources were adequate outside Hubei. That might be the main reason for more ECMO programs outside Hubei applied ECMO in older patients (age > 65), aiming at minimizing the local mortality of COVID-19. Age is a key driver of mortality, helping clinicians to select the most appropriate candidates for ECMO among severe ARDS patients [6]. However, age should be reconsidered in the discussions of indications for ECMO in COVID-19. To the limitation, the patient’s detailed characteristic was not obtained in the present study. Further multicenter registry on COVID-19 patients receiving ECMO support would be performed.
To summarize, our large national survey provided detailed information regarding the organization of ECMO programs for COVID-19 in China. To improve outcomes with ECMO during the pandemic, it is key to provide information about ECMO experience, patient selection, and resource allocation to ECMO programs throughout the world.
Abbreviations
- COVID-19
Coronavirus disease 2019
- CSECLS
Chinese Society of Extracorporeal Life Support
- CT
Computer tomography
Authors’ contributions
CL and XH, manuscript writing; XH, study design; CL, data collection and analysis; TZ, QH, LY, and LA, manuscript revision. The authors read and approved the final manuscript.
Funding
This work was supported by the National Key Research and Development Program of China (No. 2016YFC1301001).
Availability of data and materials
The datasets used in the present study are available from the first author and corresponding authors on reasonable request.
Ethics approval and consent to participate
Institutional ethics oversight was considered unnecessary since the present study was a voluntary survey.
Consent for publication
Not applicable.
Competing interests
None.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.MacLaren G, Fisher D, Brodie D. Preparing for the most critically ill patients with COVID-19: the potential role of extracorporeal membrane oxygenation. JAMA. 2020;323(13):1245–1246. doi: 10.1001/jama.2020.2342. [DOI] [PubMed] [Google Scholar]
- 2.Yang X, Yu Y, Xu J, Shu H, Xia J, Liu H, Wu Y, Zhang L, Yu Z, Fang M, et al. Clinical course and outcomes of critically ill patients with SARS-CoV-2 pneumonia in Wuhan, China: a single-centered, retrospective, observational study. Lancet Respir Med. 2020;8(5):475–81. [DOI] [PMC free article] [PubMed]
- 3.Zeng Y, Cai Z, Xianyu Y, Yang BX, Song T, Yan Q. Prognosis when using extracorporeal membrane oxygenation (ECMO) for critically ill COVID-19 patients in China: a retrospective case series. Crit Care. 2020;24(1):148. doi: 10.1186/s13054-020-2840-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Barbaro RP, Odetola FO, Kidwell KM, Paden ML, Bartlett RH, Davis MM, Annich GM. Association of hospital-level volume of extracorporeal membrane oxygenation cases and mortality. Analysis of the extracorporeal life support organization registry. Am J Respir Crit Care Med. 2015;191(8):894–901. doi: 10.1164/rccm.201409-1634OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wu Z, McGoogan JM. Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China: summary of a report of 72314 cases from the Chinese Center for Disease Control and Prevention. JAMA. 2020;323(13):1239–1242. doi: 10.1001/jama.2020.2648. [DOI] [PubMed] [Google Scholar]
- 6.Schmidt M, Bailey M, Sheldrake J, Hodgson C, Aubron C, Rycus PT, Scheinkestel C, Cooper DJ, Brodie D, Pellegrino V, et al. Predicting survival after extracorporeal membrane oxygenation for severe acute respiratory failure. The Respiratory Extracorporeal Membrane Oxygenation Survival Prediction (RESP) score. Am J Respir Crit Care Med. 2014;189(11):1374–1382. doi: 10.1164/rccm.201311-2023OC. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets used in the present study are available from the first author and corresponding authors on reasonable request.