Abstract
Objective
This study aimed to assess the positional relationships between the maxillary sinus and the first and second molars in a western Chinese population by using cone-beam computed tomography.
Methods
This study included 212 patients (652 maxillary molars and 1956 roots). Patient demographics (sex and age) and cone-beam computed tomography data regarding the relationship between molar roots and the maxillary sinus were obtained. This relationship was stratified into four types for statistical analysis.
Results
Sex and side did not significantly influence the distance between maxillary molar roots and the maxillary sinus. However, the distance between maxillary molar roots and the maxillary sinus increased with age. The mesiobuccal root of the second molar was nearest to the maxillary sinus. The most common relationship type involved absence of root contact with the sinus border and presence of a maxillary sinus cross-section above the root apex.
Conclusions
Compared with other teeth, the maxillary posterior teeth have a complex anatomical structure and are closely related to the sinus. These findings may serve as reference information for root canal treatment, tooth extraction, dental implant, and other dental clinical procedures among patients in western China.
Keywords: cone-beam computed tomography, maxillary sinus, maxillary molar roots, relationship, dental implants, dental pulp cavity, tooth root, tooth extraction, China
Introduction
Surgical removal of maxillary molars is a routine procedure. In some instances, the close relationship of the maxillary sinus floor (MSF) and posterior molar roots (PMRs) leads to oroantral communication, maxillary sinusitis, cysts, or root collapse into the sinus.1 Notably, the maxillary sinus differs among physiological and pathological conditions.2 A thorough understanding of the relationships between the MSF and PMRs is critical for avoiding these complications.
The floor wall is most closely related to the maxillary posterior teeth. Previous studies have shown that the MSF may expand to the alveolar bone in nearly 50% of patients, forming alveolar crypts and extending between adjacent teeth or their roots.3 During ordinal eruption of molars, the sinus floor moves occlusally, covering the root apices of the first premolar to the third molar.4 The alveolar ridge height continues to reduce with age, as does the distance between the MSF and PMRs.5 Surgical procedures (e.g., root canal therapy, tooth extraction, or implant treatments) can cause sinusitis, oroantral fistulae, and root displacement.6 An understanding of the relationship between the MSF and PMRs may aid in prevention of complications.
The simplest method to assess the relationship between the MSF and PMRs involves proper imaging of the area. Periapical and panoramic radiography and cone-beam computed tomography (CBCT) are commonly used imaging techniques in dental procedures. Periapical and panoramic images can adequately depict the relationship between molar roots and MSF. However, when molar roots cling to the MSF, the root images overlap with MSF images; thus, their spatial relationships are unclear.7 More precise assessment of maxillary sinus conditions could be obtained by using CBCT, which provides additional data for comparison with periapical and panoramic images. The CBCT provides images without geometric distortion and avoids superimposition of adjacent structures.2 Accordingly, the three-dimensional images provided by CBCT enable rationalization of surgical plans and facilitate appropriate doctor-patient communication.8 In western China, CBCT examinations have not been popular in some counties, because of financial constraints. Thus, surgical risk is higher for patients with complicated pathologies in these counties.
This study explored the positional relationships of the maxillary MSF with the first and second molars by using CBCT images in a western Chinese population; it then classified and compared the prominent characteristics of these relationships, with the goal of providing additional reference information for root canal treatment, tooth extraction, dental implant treatment, and other dental procedures in this region.
Materials and methods
Ethical approval and sample size calculations
This was a retrospective imaging study, which did not involve identifying information for included patients. Hence, no written/verbal consent was obtained from patients or their guardians. This study was approved by the Ethics Committee of West China Hospital of Stomatology, Sichuan University (approval number: WCHSIRB-D-2014-074).
Statistical analysis in this study comprised comparisons of mean quantitative data; thus, the sample size calculation formula was n = . Considering the nearest distance between the molar roots and MSF, a mean difference of 0.25 mm was considered clinically meaningful; 2.17 mm was regarded as the variation, based on the findings in a previously published study.9 This study was designed to achieve 5% significance and 80% power. The size of the effect that was clinically meaningful (d) was 0.25; the standard deviation of the study population (σ) was 2.17; the probability of falsely rejecting a true null hypothesis (α) was 0.05, Z(α) = 1.96; and the probability of failing to reject a false null hypothesis (β) was 0.80, Z(β) = 0.84. Thus, this study was designed to include at least 560 roots.
Patients
The American Dental Association Council on Scientific Affairs advises use of CBCT only when the diagnostic yield will benefit patient care, enhance patient safety, or significantly improve clinical outcomes.10 Adult patients who underwent CBCT scans during various procedures at the West China Hospital of Stomatology from July 2016 to September 2016 were selected for this study. The inclusion criteria for the study sample were as follows:
age ≥18 years;
normally erupted maxillary second premolars and molars (except the third molar) with complete root development, absence of missing or deformed teeth, and absence of pulp periodontal lesions or apical shadows;
absence of pathological changes in the target region, including absence of maxillary sinus mucosal thickening, absence of maxillary sinus inflammation, absence of cyst or tumors, absence of malformations, and absence of maxillary fractures;
absence of septa in the sinus area containing molar apices;
clear, distortion-free, and deflection-free radiographic images containing a complete maxillary sinus and maxillary molars.
Scanning and analysis procedures
Computed tomography scans were all obtained using the same 3D Accuitomo CBCT scanner (MCT-1[EX-2F]; J Morita Manufacturing, Kyoto, Japan) with settings of 85 kV and 4 mA. Scanning was accomplished with a gray-scale image of 14 bits and a voxel size of 0.125 mm per side. CBCT images were viewed using INFINITT PACS software (INFINITT Healthcare Co., Ltd., Seoul, South Korea) on a Dell 24-inch LCD monitor (1920 × 1200 resolution) (Dell Computer Corp, Ron Droke, TX, USA). All evaluations were conducted by one examiner. Study images were evaluated twice with a 1-month interval between assessments. Cohen’s kappa was assessed to determine intraobserver reliability. The average value of the two length measurements was used for data analysis.
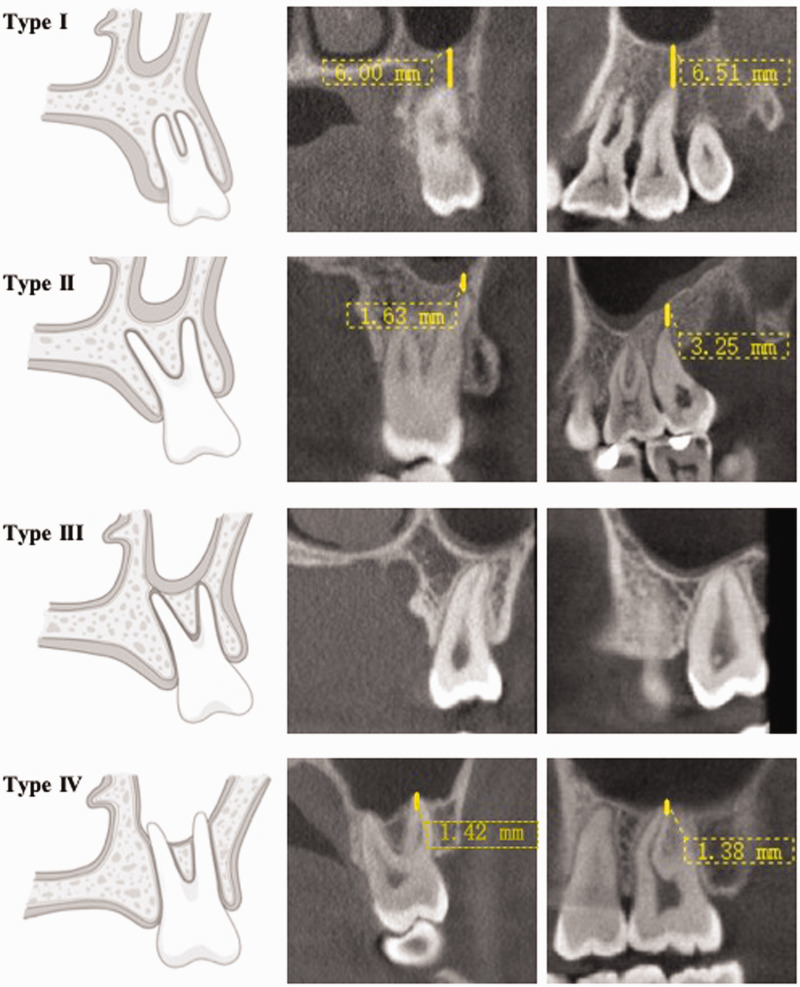
Each root of the molars was classified and measured in the sagittal, coronal, and axial planes. In accordance with the methods of previous studies9,11,12 and the images collected in this study, the positional relationships between the root apices and maxillary sinus were divided into the following four types: type I, absence of root contact with the sinus border and presence of maxillary sinus cross-section above the root apex; type II, absence of root contact with the sinus border, with lateral projection on the sinus cavity accompanied by an inferiorly curving sinus floor; type III, root apex contact with the maxillary sinus (touching or tangentially); and type IV, root apex intrusion into the maxillary sinus. To facilitate measurements of the distance between the molar root apex and the MSF, the images were classified and measured using i-Dixel One Data Viewer Plus software (J. Morita Corp., Osaka, Japan). The plane of the anterior nasal spine and posterior nasal spine on the axial plane was chosen as the palatal plane; sagittal and coronal images were observed and the distance was determined with the axial plane unchanged (Figures 1 and 2). Vertical lines were made from each molar root apex to the hard palatal plane; distances between the molar roots and MSF were recorded. This method avoided interference from individual root direction and maxillary shape at the extremities (Figure 3). Types I and II relationships were regarded as positive, type III relationships were regarded as neutral, and type IV relationships were regarded as negative.
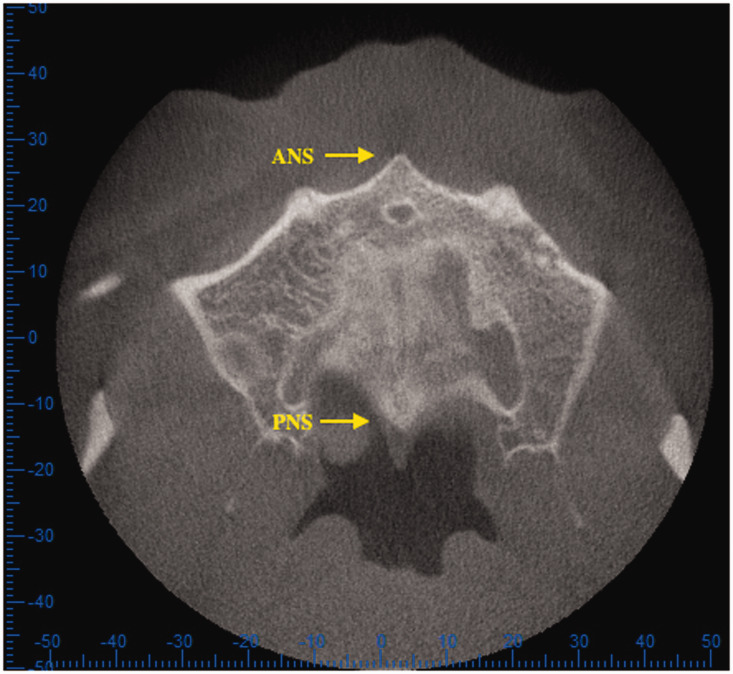
Figure 1.
Palatal plane, as defined by anterior nasal spine–posterior nasal spine using i-Dixel One Data Viewer Plus software.
Abbreviations: ANS, anterior nasal spine; PNS, posterior nasal spine.
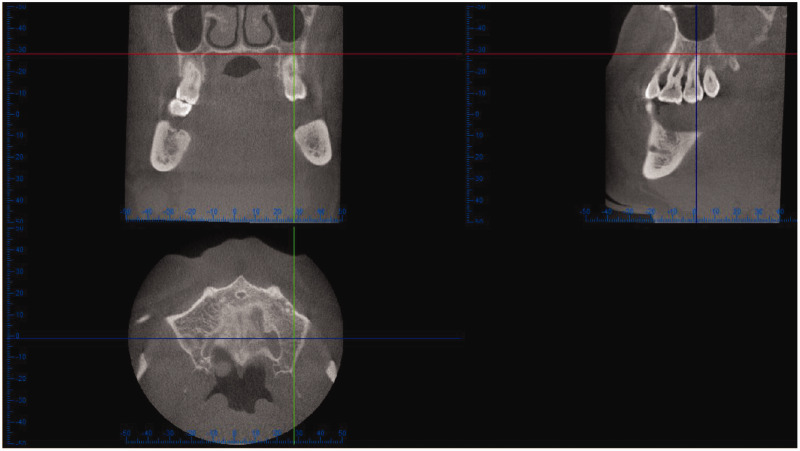
Figure 2.
Sagittal and coronal images were observed to determine distances while the axial plane (palatal plane) remained unchanged. Top left, coronal plane; top right, sagittal plane; bottom left, axial plane.
Figure 3.
Schematics and cone-beam computed tomography views of four types of relationships in coronal and sagittal planes. Yellow line indicates measurement of distance from molar to sinus floor. Type I, absence of root contact with the sinus border and presence of maxillary sinus cross-section above the root apex; type II, absence of root contact with the sinus border, with lateral projection on the sinus cavity accompanied by an inferiorly curving sinus floor; type III, root apex contact with the maxillary sinus (touching or tangentially); and type IV, root apex intrusion into the maxillary sinus.
In accordance with the classification proposed by Kwak et al.,13 types II, III, and IV in the coronal plane were divided into the following three sub-types, based on the positional relationships of buccal and palatal molar roots with the lowest point of the maxillary sinus: class 1, lowest point of maxillary sinus on buccal side of buccal root; class 2, lowest point of maxillary sinus between buccal root and palatal root; and class 3, lowest point of maxillary sinus on palatal side of palatal root.
Data analysis
Sex, age, and side of evaluation were analyzed to determine whether these characteristics were associated with radiographic measurements. Only images with bilateral molars were evaluated with respect to the side factor. Statistical analysis was performed using SPSS Statistics, version 22.0 (IBM Corp., Armonk, NY, USA). The independent-samples t-test, paired t-test, and rank-sum test were respectively applied to detect significant differences in distances from molar apices to the maxillary sinus border with respect to sex, side, and age. Lengths of root apices and the sinus floor were compared by one-way analysis of variance. The prevalences of first molar and second molar classifications were analyzed using the chi-squared test. P values < 0.05 were considered statistically significant.
Results
Overall patient characteristics
In total, 652 maxillary molars (first molars, 50%; second molars, 50%) with 1956 roots from 212 patients (88 men, 124 women; mean age, 33.5 ± 12.5 years; range, 18–83 years) met the criteria and were included in this study (Table 1). The Cohen’s kappa value for intraobserver reliability was 0.87. The distances between PMRs and the MSF were greater in men than in women in the coronal and sagittal planes, but these differences were not statistically significant (Tables 2 and 3). Most distances between PMRs and the MSF were shorter on the left side than on the right side, but these differences were not statistically significant (Table 4).
Table 1.
Distribution of evaluated situations.
| Tooth | Right | Left | Total (%) |
|---|---|---|---|
| 16 and 26 (first molar) | 158 | 168 | 326 (50) |
| 17 and 27 (second molar) | 160 | 166 | 326 (50) |
| Total | 318 | 334 | 652 (100) |
Table 2.
Sex-related distances between the root apex and the maxillary sinus floor on the right side.
| Tooth | Sex | N | Sagittal |
Coronal |
||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Mean ± SD | Min | Max | P value | Mean ± SD | Min | Max | P value | |||
| 16 and 26 | ||||||||||
| MB | M | 71 | 2.16 ± 3.39 | −1.26 | 12.01 | 0.40 | 2.98 ± 4.27 | −1.46 | 13.25 | 0.22 |
| F | 87 | 1.73 ± 2.99 | −4.08 | 13.43 | 2.19 ± 3.54 | −2.77 | 11.54 | |||
| DB | M | 71 | 2.27 ± 3.40 | −1.20 | 13.53 | 0.34 | 2.75 ± 4.00 | −1.65 | 13.49 | 0.61 |
| F | 87 | 1.79 ± 2.84 | −2.75 | 12.10 | 2.44 ± 3.48 | −4.12 | 18.11 | |||
| P | M | 71 | 2.20 ± 3.98 | −4.07 | 14.81 | 0.99 | 2.27 ± 3.63 | −4.03 | 10.94 | 0.55 |
| F | 87 | 2.20 ± 3.23 | −3.02 | 11.48 | 2.61 ± 3.62 | −2.44 | 12.30 | |||
| 17 and 27 | ||||||||||
| MB | M | 71 | 1.22 ± 2.90 | −3.29 | 8.37 | 0.50 | 1.37 ± 2.94 | −2.33 | 9.56 | 0.49 |
| F | 89 | 0.94 ± 2.17 | −2.76 | 8.77 | 1.08 ± 2.22 | −2.46 | 8.62 | |||
| DB | M | 71 | 1.92 ± 3.27 | −2.37 | 8.37 | 0.22 | 2.10 ± 3.18 | −1.41 | 9.56 | 0.26 |
| F | 89 | 1.34 ± 2.49 | −2.03 | 10.72 | 1.57 ± 2.58 | −1.59 | 10.01 | |||
| P | M | 71 | 3.08 ± 3.81 | −1.69 | 11.88 | 0.40 | 3.12 ± 3.68 | −1.10 | 11.73 | 0.80 |
| F | 89 | 2.60 ± 3.11 | −2.55 | 12.24 | 2.98 ± 3.20 | −2.65 | 11.57 | |||
Distances are shown in mm.
Abbreviations: MB, mesiobuccal root; DB, distobuccal root; P, palatal root; N, number; M, male; F, female; SD, standard deviation; Min, minimum; Max, maximum.
Table 3.
Sex-related distances between the root apex and the maxillary sinus floor on the left side.
| Tooth | Sex | N | Sagittal |
Coronal |
|||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Mean ± SD | Min | Max | P value | Mean ± SD | Min | Max | P value | ||||
| 16 and 26 | |||||||||||
| MB | M | 65 | 2.26 ± 3.55 | −1.86 | 14.06 | 0.23 | 3.16 ± 4.03 | −1.20 | 13.96 | 0.24 | |
| F | 103 | 1.65 ± 3.00 | −4.19 | 10.19 | 2.43 ± 3.82 | −3.17 | 13.61 | ||||
| DB | M | 65 | 2.11 ± 3.53 | −1.36 | 14.24 | 0.50 | 2.92 ± 3.87 | −1.51 | 16.01 | 0.20 | |
| F | 103 | 1.75 ± 2.90 | −2.16 | 11.23 | 2.18 ± 3.05 | −2.89 | 12.74 | ||||
| P | M | 65 | 2.08 ± 3.60 | −2.72 | 10.52 | 0.65 | 2.52 ± 3.54 | −2.39 | 11.12 | 0.74 | |
| F | 103 | 2.35 ± 3.89 | −3.70 | 13.44 | 2.34 ± 3.44 | −2.75 | 13.11 | ||||
| 17 and 27 | |||||||||||
| MB | M | 63 | 0.84 ± 2.84 | −2.77 | 13.15 | 0.72 | 1.04 ± 2.73 | −1.60 | 13.02 | 0.91 | |
| F | 103 | 0.99 ± 2.54 | −2.56 | 9.72 | 0.99 ± 2.49 | −4.18 | 7.87 | ||||
| DB | M | 63 | 1.44 ± 3.31 | −2.56 | 13.15 | 0.69 | 1.75 ± 3.31 | −2.80 | 13.02 | 0.65 | |
| F | 103 | 1.33 ± 2.72 | −2.52 | 10.87 | 1.52 ± 3.90 | −4.18 | 11.87 | ||||
| P | M | 63 | 2.15 ± 3.62 | −2.40 | 13.15 | 0.56 | 3.05 ± 3.87 | −1.13 | 13.02 | 0.43 | |
| F | 103 | 2.48 ± 3.46 | −2.52 | 13.73 | 2.60 ± 3.07 | −1.55 | 10.74 | ||||
Distances are shown in mm.
Abbreviations: MB, mesiobuccal root; DB, distobuccal root; P, palatal root; N, number; M, male; F, female; SD, standard deviation; Min, minimum; Max, maximum.
Table 4.
Distances between the root apex and the maxillary sinus floor on different sides.
| Tooth | Side | N | Sagittal |
Coronal |
||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Mean ± SD | Min | Max | P value | Mean ± SD | Min | Max | P value | |||
| 16 and 26 | ||||||||||
| MB | R | 117 | 1.81 ± 3.10 | −4.08 | 13.43 | 0.24 | 2.44 ± 3.75 | −3.10 | 16.06 | 0.13 |
| L | 117 | 2.03 ± 3.43 | −4.08 | 13.43 | 2.82 ± 4.20 | −3.17 | 13.96 | |||
| DB | R | 117 | 1.93 ± 3.09 | −2.81 | 13.53 | 0.53 | 2.40 ± 3.52 | −4.12 | 18.11 | 0.31 |
| L | 117 | 2.04 ± 3.42 | −2.16 | 14.24 | 2.62 ± 3.68 | −2.89 | 16.01 | |||
| P | R | 117 | 2.23 ± 3.76 | −4.07 | 14.88 | 0.58 | 2.28 ± 3.54 | −4.03 | 12.69 | 0.41 |
| L | 117 | 2.40 ± 3.98 | −3.70 | 13.44 | 2.49 ± 3.61 | −2.75 | 13.11 | |||
| 17 and 27 | ||||||||||
| MB | R | 116 | 0.90 ± 2.48 | −3.29 | 10.13 | 0.63 | 1.07 ± 2.53 | −2.46 | 9.56 | 0.93 |
| L | 116 | 0.97 ± 2.70 | −3.54 | 13.15 | 1.06 ± 2.60 | −4.18 | 13.02 | |||
| DB | R | 116 | 1.26 ± 2.60 | −2.37 | 12.91 | 0.46 | 1.53 ± 2.69 | −2.06 | 12.40 | 0.48 |
| L | 116 | 1.39 ± 2.99 | −3.54 | 13.15 | 1.67 ± 3.14 | −4.18 | 13.02 | |||
| P | R | 116 | 2.54 ± 3.28 | −2.55 | 16.97 | 0.49 | 2.85 ± 3.36 | −2.65 | 16.02 | 0.63 |
| L | 116 | 2.36 ± 3.54 | −3.54 | 13.73 | 2.72 ± 3.46 | −2.45 | 13.02 | |||
Distances are shown in mm.
Abbreviations: MB, mesiobuccal root; DB, distobuccal root; P, palatal root; N, number; SD, standard deviation; Min, minimum; Max, maximum.
Group characteristics
The 212 patients were divided into three groups on the basis of age: ≤20 years, 21 to 40 years, and 41 to 60 years. This evaluation excluded three patients who were older than 60 years of age because this number of patients was insufficient to allow meaningful analysis. In the sagittal and coronal planes, the distance between each root of the first molar and the sinus increased with age. In addition, there were significant intergroup differences (P < 0.05 for all), except between the mesiobuccal and palatal roots in the first and second groups (Table 5). The distance between each root of the second molar and the MSF also increased with age, with significant differences observed for all distances (P < 0.05 for all) except those involving distobuccal and palatal roots in the first and second groups (Table 6).
Table 5.
Age-related distances between the root apex and the maxillary sinus floor in the first molar.
| Tooth | Age | N | Sagittal |
Coronal |
||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Mean ± SD | Min | Max | P value | Mean ± SD | Min | Max | P value | |||
| MB | ≤20① | 62 | 0.39 ± 1.76 | −1.77 | 6.45 | P(①,②) =0.533 | 0.59 ± 2.08 | −3.10 | 6.31 | P(①,②) = 0.634 |
| 21–40② | 82 | 1.41 ± 2.76 | −4.84 | 10.73 | P(②,③) <0.001 | 2.10 ± 3.41 | −3.11 | 16.06 | P(②,③) < 0.001 | |
| 41–60③ | 67 | 3.48 ± 3.45 | −3.77 | 13.04 | P(①,③) < 0.001 | 4.54 ± 4.05 | −2.38 | 14.34 | P(①,③) < 0.001 | |
| DB | ≤20① | 62 | 0.35 ± 1.65 | −1.10 | 7.47 | P(①,②) = 0.044 | 0.62 ± 1.92 | −2.91 | 6.91 | P(①,②) = 0.035 |
| 21–40② | 82 | 1.49 ± 2.72 | −2.46 | 11.35 | P(②,③) < 0.001 | 2.03 ± 3.10 | −2.71 | 16.16 | P(②,③) < 0.001 | |
| 41–60③ | 67 | 3.33 ± 3.26 | −2.81 | 13.89 | P(①,③) < 0.001 | 4.33 ± 3.70 | −2.27 | 14.75 | P(①,③) < 0.001 | |
| P | ≤20① | 62 | 0.32 ± 1.99 | −2.93 | 5.62 | P(①,②) = 0.759 | 0.60 ± 2.18 | −2.94 | 9.23 | P(①,②) = 0.697 |
| 21–40② | 82 | 1.75 ± 3.14 | −3.39 | 10.26 | P(②,③) < 0.001 | 2.14 ± 3.36 | −2.56 | 12.69 | P(②,③) = 0.001 | |
| 41–60③ | 67 | 3.82 ± 3.57 | −2.67 | 13.04 | P(①,③) < 0.001 | 3.94 ± 3.25 | −3.28 | 9.82 | P(①,③) < 0.001 | |
Distances are shown in mm. Circled numbers indicate age groups as shown in “Age” column.
Abbreviations: MB, mesiobuccal root; DB, distobuccal root; P, palatal root; N, number; SD, standard deviation; Min, minimum; Max, maximum.
Table 6.
Age-related distances between root apex and the maxillary sinus floor in the second molar.
| Tooth | Age | N | Sagittal |
Coronal |
||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Mean ± SD | Min | Max | P value | Mean ± SD | Min | Max | P value | |||
| MB | ≤20① | 62 | −0.16 ± 2.16 | −2.92 | 10.27 | P(①,②) = 0.017 | −0.23 ± 1.98 | −2.03 | 9.38 | P(①,②) = 0.003 |
| 21–40② | 82 | 0.75 ± 2.23 | −3.54 | 8.78 | P(②,③) = 0.001 | 0.88 ± 2.24 | −3.29 | 8.14 | P(②,③) < 0.001 | |
| 41–60③ | 66 | 2.06 ± 2.74 | −1.72 | 10.76 | P(①,③) < 0.001 | 2.21 ± 2.69 | −1.02 | 11.29 | P(①,③) < 0.001 | |
| DB | ≤20① | 62 | 0.40 ± 2.42 | −2.47 | 10.33 | P(①,②) = 0.648 | 0.48 ± 2.46 | −1.88 | 9.66 | P(①,②) = 0.583 |
| 21–40② | 82 | 1.13 ± 2.66 | −3.54 | 10.80 | P(②,③) < 0.001 | 1.36 ± 2.64 | −2.74 | 10.94 | P(②,③) < 0.001 | |
| 41–60③ | 66 | 2.88 ± 3.01 | −1.72 | 12.91 | P(①,③) < 0.001 | 3.07 ± 2.99 | −0.96 | 12.40 | P(①,③) < 0.001 | |
| P | ≤20① | 62 | 1.03 ± 2.26 | −2.10 | 10.40 | P(①,②) = 0.624 | 1.44 ± 2.33 | −1.33 | 9.22 | P(①,②) = 0.657 |
| 21–40② | 82 | 2.39 ± 3.24 | −3.54 | 10.96 | P(②,③) < 0.001 | 2.83 ± 3.16 | −2.45 | 11.54 | P(②,③) = 0.039 | |
| 41–60③ | 66 | 3.88 ± 3.58 | −1.72 | 16.97 | P(①,③) < 0.001 | 3.96 ± 3.35 | −1.02 | 16.02 | P(①,③) < 0.001 | |
Distances are shown in mm. Circled numbers indicate age groups as shown in “Age” column.
Abbreviations: MB, mesiobuccal root; DB, distobuccal root; P, palatal root; N, number; SD, standard deviation; Min, minimum; Max, maximum.
Sagittal plane analysis
Among all 1956 maxillary molar roots analyzed, in the sagittal plane, the distances between the roots and the sinus were in the following order (from nearest to farthest): second molar mesiobuccal root; second molar distobuccal root; second molar palatal root; first molar mesiobuccal root; first molar distobuccal root; and first molar palatal root (Table 7). These findings implied that the second molar mesiobuccal root was nearest to the maxillary sinus; this difference was statistically significant, in comparison with the other roots (P < 0.05). The second molar distobuccal root was second nearest to the maxillary sinus; this difference was also statistically significant, in comparison to the other roots (P < 0.05).
Table 7.
Distances between different roots and the maxillary sinus.
| Tooth | N | Sagittal |
Coronal |
||||
|---|---|---|---|---|---|---|---|
| Mean ± SD | Min | Max | Mean ± SD | Min | Max | ||
| 16 and 26 | |||||||
| MB | 326 | 1.90 ± 3.20 | -4.84 | 14.06 | 2.63 ± 3.89 | -3.17 | 16.06 |
| DB | 326 | 1.94 ± 3.12 | -2.81 | 14.24 | 2.52 ± 3.54 | -4.12 | 18.11 |
| P | 326 | 2.04 ± 3.36 | -4.07 | 14.88 | 2.43 ± 3.54 | -4.03 | 13.11 |
| 17 and 27 | |||||||
| MB | 326 | 0.99* ± 2.58 | -3.54 | 13.15 | 1.11Δ ± 2.56 | -4.18 | 13.02 |
| DB | 326 | 1.45# ± 2.85 | -3.54 | 13.15 | 1.68 ± 2.91 | -4.18 | 13.02 |
| P | 326 | 1.81 ± 3.09 | -3.54 | 13.15 | 2.86 ± 3.32 | -2.65 | 13.02 |
Distances are shown in mm.
*In the sagittal plane, the distance between the indicated root and the maxillary sinus is shortest in comparison with the other roots with P value < 0.05.
#In the sagittal plane, the distance between the indicated root and the maxillary sinus is second shortest in comparison with the other roots with P value < 0.05.
Δ In the coronal plane, the distance between the indicated root and the maxillary sinus is shortest in comparison with the other roots with P value < 0.05, except for the second molar DB.
Abbreviations: MB, mesiobuccal root; DB, distobuccal root; P, palatal root; N, number; SD, standard deviation; Min, minimum; Max, maximum.
Coronal plane analysis
Among all 1956 maxillary molar roots analyzed, in the coronal plane, the distances between the roots and sinuses were in the following order (from nearest to farthest): second molar mesiobuccal root; second molar distobuccal root; first molar palatal root; first molar distobuccal root; first molar mesiobuccal root; and second molar palatal root (Table 7). The second molar mesiobuccal root remained nearest root to the maxillary sinus; it exhibited a significant difference in distance to the maxillary sinus relative to other roots, except the second molar distobuccal root. The second molar distobuccal root remained the second nearest root; it exhibited significant differences relative to the first molar distobuccal root and first molar palatal root (P = 0.040 and P = 0.014, respectively) (Table 7).
Common relationships in the sagittal plane
In the sagittal plane, the most common relationship between maxillary molar roots and the maxillary sinus was type I, which was observed in 866 roots (44.3%). Type III relationships and type IV relationships were observed in 425 (21.7%) and 406 roots (20.8%), respectively. In contrast, type II was the rarest relationship; it was observed in 259 roots (13.2%). In total, 491 first molar roots (50.2%) and 375 second molar roots (38.3%) exhibited type I relationships. Type II relationships were present in 92 first molar roots (9.4%) and 167 second molar roots (17.1%). Type III and IV relationships both constituted approximately 20% of the first and second molar roots. The differences in type constituent ratio between first and second molar roots were statistically significant (P < 0.001) (Table 8).
Table 8.
Classification of roots in the sagittal plane.
| Tooth | Type |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| I |
II |
III |
IV |
Total |
||||||
| N | % | N | % | N | % | N | % | N | % | |
| 16 and 26 | ||||||||||
| MB | 153 | 46.9 | 44 | 13.5 | 68 | 20.9 | 61 | 18.7 | 326 | 100 |
| DB | 172 | 52.8 | 24 | 7.4 | 70 | 21.5 | 60 | 18.4 | 326 | 100 |
| P | 166 | 50.9 | 24 | 7.4 | 61 | 18.7 | 75 | 23.0 | 326 | 100 |
| Total* | 491 | 50.2 | 92 | 9.4 | 199 | 20.3 | 196 | 20.0 | 978 | 100 |
| 17 and 27 | ||||||||||
| MB | 112 | 34.4 | 39 | 12.0 | 86 | 26.4 | 89 | 27.3 | 326 | 100 |
| DB | 123 | 37.7 | 43 | 13.2 | 82 | 25.2 | 78 | 23.9 | 326 | 100 |
| P | 140 | 42.9 | 85 | 26.1 | 58 | 17.8 | 43 | 13.2 | 326 | 100 |
| Total* | 375 | 38.3 | 167 | 17.1 | 226 | 23.1 | 210 | 21.5 | 978 | 100 |
| Total | 866 | 44.3 | 259 | 13.2 | 425 | 21.7 | 406 | 20.8 | 1956 | 100 |
*P < 0.001 for differences in type constituent ratio between first and second molar roots Abbreviations: MB, mesiobuccal root; DB, distobuccal root; P, palatal root; N, number.
Common relationships in the coronal plane
In the coronal plane, type I remained the most common relationship (907 roots, 46.4%); the incidences of types III, IV, II were in descending order, respectively, 474 roots (24.2%), 341 roots (17.4%), and 234 roots (12.0%). With respect to the distribution of types, the first and second molars showed similar distributions (Table 9). In the coronal plane, 311 teeth with type II, III, and IV roots could be divided into sub-types, including 149 first molars and 162 second molars. The distribution of sub-types was as follows: class 1, 61 teeth (19.6%); class 2, 233 teeth (74.9%); and class 3, 17 teeth (5.5%) (Table 10).
Table 9.
Classification of roots in the coronal plane.
| Tooth | Type |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| I |
II |
III |
IV |
Total |
||||||
| N | % | N | % | N | % | N | % | N | % | |
| 16 and 26 | ||||||||||
| MB | 161 | 49.4 | 43 | 13.2 | 64 | 19.6 | 58 | 17.8 | 326 | 100 |
| DB | 173 | 53.1 | 32 | 9.8 | 72 | 22.1 | 49 | 15.0 | 326 | 100 |
| P | 134 | 41.1 | 51 | 15.6 | 81 | 24.8 | 60 | 18.4 | 326 | 100 |
| Total | 468 | 47.9 | 126 | 12.9 | 217 | 22.2 | 167 | 17.1 | 978 | 100 |
| 17 and 27 | ||||||||||
| MB | 128 | 29.3 | 21 | 6.4 | 95 | 29.1 | 82 | 25.2 | 326 | 100 |
| DB | 146 | 44.8 | 22 | 6.7 | 96 | 29.4 | 62 | 19.0 | 326 | 100 |
| P | 165 | 50.6 | 65 | 19.9 | 66 | 20.2 | 30 | 9.2 | 326 | 100 |
| Total | 439 | 44.9 | 108 | 11.0 | 257 | 26.3 | 174 | 17.8 | 978 | 100 |
| Total | 907 | 46.4 | 234 | 12.0 | 474 | 24.2 | 341 | 17.4 | 1956 | 100 |
Abbreviations: MB, mesiobuccal root; DB, distobuccal root; P, palatal root; N, number.
Table 10.
Sub-types of roots in the coronal plane.
| Tooth | Type |
|||||||
|---|---|---|---|---|---|---|---|---|
| 1 |
2 |
3 |
Total |
|||||
| N | % | N | % | N | % | N | % | |
| 16 | 8 | 9.4 | 76 | 89.4 | 1 | 1.2 | 85 | 100 |
| 26 | 21 | 32.8 | 39 | 60.9 | 4 | 6.3 | 64 | 100 |
| Total | 29 | 19.5 | 115 | 77.2 | 5 | 3.4 | 149 | 100 |
| 17 | 9 | 10.6 | 72 | 84.7 | 4 | 4.7 | 85 | 100 |
| 27 | 23 | 29.9 | 46 | 59.7 | 8 | 10.4 | 77 | 100 |
| Total | 32 | 19.6 | 118 | 72.8 | 12 | 7.41 | 162 | 100 |
| Total | 61 | 19.6 | 233 | 74.9 | 17 | 5.5 | 311 | 100 |
Abbreviation: N, number.
Discussion
Rationale for exclusion criteria used in this study
Although most of the maxillary sinus is bilaterally symmetrical, there are large individual differences in the size and shape of the sinus.14 Zaman et al.15 reviewed the maxillary sinus morphology among individuals of different ages and in different populations, which revealed that the development pattern of the maxillary sinus may differ according to age and sex. Langford et al.16 also found that the growth rate of the sinus differs significantly according to age. Thus, to exclude the impact of maxillary sinus decline during development, the present study included patients aged ≥18 years.
In addition, pathological changes in the maxillary posterior regions such as apical periodontitis and chronic periodontitis can cause mucosal thickening and other changes in the maxillary sinus.17,18 Sharan and Madjar12 proposed that maxillary molar extraction can lead to maxillary sinus pneumatization, bringing the remaining root apices closer to the maxillary sinus. This finding is more obvious when intruding roots are extracted or the second molar is extracted,19 which indicates that this phenomenon may be induced by the loss of chewing stimulation for alveolar bone after tooth extraction, as well as osteoclast activity and reconstruction of the alveolar bone and maxillary sinus. Therefore, to eliminate interference, the present study excluded target teeth without adjacent teeth.
Sex-related differences in maxillary sinus relationships
The findings in this experiment showed that, irrespective of side or plane, the molar roots were closer to the sinus in women than in men, but these differences were not statistically significant. In an analysis of premolars and the maxillary sinus, Von Arx et al.20 revealed that premolars were closer to the sinus in men than in women, presumably because men have longer roots and a broader fully developed maxillary sinus. However, considering the longer roots in men, as well as the greater bone volume and mass, the present study’s finding that maxillary molars in men are relatively far from the maxillary sinus is reasonable.
Age-related differences in maxillary sinus relationships
Age analysis in this study showed that the distance between molar apex and the maxillary sinus increases with age. The distance between each root and the MSF increases by approximately 1 mm with each 20-year increase in age. Previous studies had presented limited data regarding the relationship of age with the distance between PMRs and MSF. In the study by Von Arx et al.,20 age did not affect the distance between the maxillary premolars and the sinus; moreover, no significant differences were observed among age groups. Tian et al.21 showed that mean distances between PMRs and MSF, as well as the frequency of type IV relationships, decreased with increasing age in the Chinese population. Moreover, in all roots of posterior teeth from Chinese patients, Gu et al.22 found that distances between root apices and the MSF increased with age. With improvements in the quality of life, the younger generation has higher indexes of height and weight, relative to older individuals; this difference has presumably resulted in intergroup errors in cross-sectional studies. To investigate whether the distance between PMRs and MSF exhibits any associations with age, as well as the specific reasons for these associations, a longitudinal study is needed for a fixed experimental group of individuals.
Furthermore, physiological tooth attrition increases with age. To compensate for reduction in the clinical crown, the formation of secondary cementum in root apices can increase the distance between the PMRs and the MSF. Some scholars have proposed that, after development of the maxillary sinus, the maxillary sinus volume will be reduced and the sinus floor will move upwards, unless interference is encountered (e.g., tooth extractions that cause sinus pneumatization).23–25 The present study revealed that the distance between molar roots and MSF increased with age, which indicated that the risks of molar extraction, endodontic therapy, or implantation were also relatively greater in adolescents. This conclusion indicates the need to protect molars from childhood onwards, by means of dental examinations or the pit and fissure sealant technique.
Maxillary sinus relationships with specific teeth
Purmal et al.26 found that the lowest position of the sinus is in between the right molars and the highest position is in between the left premolars. Most studies have shown that maxillary second molar buccal roots are nearest to the maxillary sinus.9,11,13,21,22,27,28 Eberhardt et al.,27 Georgescu et al.,28 and Jung and Cho11 reported that the second molar mesiobuccal root was nearest to the maxillary sinus. In studies of Chinese individuals, Tian et al.,21 Gu et al.,22 and Zhang et al.29 also found that the root nearest to the MSF was generally the second molar mesiobuccal root. However, Kilic et al.9 found that the second molar distobuccal root was nearest to the MSF. In a study of 33 skull images measured via computed tomography, Kwak et al.13 revealed that the second molar distobuccal root was nearest to the sinus (2.74 mm). The results of the present study, which used two coronal and sagittal cross-sectional measurements, showed that the mesiobuccal root of the second molar was nearest to the maxillary sinus; this was consistent with the findings of the previous studies in Chinese individuals. In the sagittal plane, the average distance between the maxillary second molar mesiobuccal root and the sinus was 0.99 ± 2.58 mm; in the coronal plane, this distance was 1.11 ± 2.56 mm. Furthermore, the second molar distobuccal root was the second nearest.
Comparisons with prior studies
The results of the present study differed from those of some previous studies. Possible explanations may be ethnicity-related differences in molar characteristics; notably, the results of the present study were similar to those of previous studies involving Chinese individuals.21,22,29 In addition, the methods adopted in this study to examine distance differed from those of prior studies; specifically, a hard palate datum plane was established for distance measurement to obtain more accurate data. The results of the present study may also be explained with reference to the report by Mustian,30 who wrote that the lowest point of the MSF is in the second molar region; this is consistent with the type IV positional relationship between the root and maxillary sinus, whereby the second molar mesiobuccal root has the highest proportion.
The positional relationship of PMRs and MSF is determined by the maxillary bone mass between them. For type I relationships with adequate bone, clinical treatment is relatively safe. Type II relationships can be treated safely in the vertical direction, but often require complex assessment. For example, the molar furcation causative agent can invade the maxillary sinus;31 extraction of residual molar roots may cause horizontal displacement, introducing the risk of root entry into the maxillary sinus.32 In such instances, there is insufficient vertical distance for the implant.33
Occasionally, the MSF expands within the alveolar process and extends between roots, such that the apex clings to the sinus covering only a very thin bone plate or a single layer of mucous membrane.5 Such instances, which are classified as types III and IV relationships, are considered high-risk. If the apex in either of these relationships exhibits pathology, the disease can easily spread to the maxillary sinus, where it causes inflammation and infection; inappropriate tooth extraction can lead to oral sinus fistula and foreign matter in the sinus.
Previous studies regarding the positional relationship of maxillary molars and the sinus showed that the separation of molar roots and maxillary sinus from bone was most common.9,12,27 However, Themkumkwun et al.34 analyzed CBCT images of 354 roots and concluded that molar roots extending beyond the sinus floor was most common. In Chinese individuals, Zhang et al.35 found that one-half of molar roots protrude into the maxillary sinus or touch the sinus floor without bony interaction. Jung and Cho11 also found that the most common type of molar buccal root involved root apex intrusion into the maxillary sinus. The present study included 1956 molar roots for classification in both sagittal and coronal planes. Type I relationships were most common in both planes. Generally, nearly half of the measured roots exhibited a more secure relationship with the maxillary sinus. The relatively dangerous type III and IV roots each constituted approximately 20%. Thus, approximately 40% of the roots were very close to the maxillary sinus; these required additional clinical attention. The rarest relationship was type II, which constituted approximately 10%.
In the vertical direction (i.e., the coronal plane), types II, III, and IV were further subdivided into classes 1, 2, and 3. In total, 311 teeth (149 first molars and 162 second molars) were included in the study. Class 2 was the most common vertical relationship (74.9%), followed by class 1 (19.6%); the rarest vertical relationship was class 3 (5.5%). These results are consistent with the findings of most previous studies.11,13 An accurate assessment of the lowest point in the vertical direction of the maxillary sinus is useful for selection of implant position.
Measurement data from this analysis indicated that the positional classification and distance between the maxillary molar roots and maxillary sinus exhibited no significant deviations in the sagittal and coronal planes; in CBCT scans, the two planes exhibited high consistency. Von Arx et al.20 found that when the distance between the root and maxillary sinus was measured, the sagittal plane did not comprise a horizontal section along the major axis of the tooth; thus, an angle between the root and maxillary sinus causes projection distortions. To avoid this measurement error, the same palatine plane was introduced for both sagittal and coronal planes in the measurement procedure, thereby reducing differences. In the clinic, when CBCT image data are available, dentists should be encouraged to perform a comprehensive and integrated analysis for the diagnosis and treatment area in each plane.
Limitations
The main limitation of this analysis was that it used sample collection from a single region over a short period of time. An additional cohort investigation with data from a wide geographical area may be necessary to achieve a better understanding of factors that influence the relationship between the maxillary molar roots and maxillary sinus, such as age and region.
Conclusion
The following conclusions can be drawn from this retrospective study:
There were no significant differences in the distance between the maxillary molars and MSF, according to sex and side. There was a statistically significant age-related difference in distance between the maxillary molars and the MSF.
The second molar mesiobuccal root was nearest to the maxillary sinus; the second molar distobuccal root was second nearest to the maxillary sinus.
The most common relationship between maxillary molar roots and the maxillary sinus was type I, which comprises absence of root contact with the sinus border and presence of maxillary sinus cross-section above the root apex.
This study assessed the physiological relationship between the maxillary molars and maxillary sinus in a group of patients from western China and provided theoretical reference data that could aid in clinical assessment and treatment of maxillary molars in this region. In comparison with other teeth, the maxillary posterior teeth exhibit a complex anatomical structure and are closely related to the sinus. Preoperative analysis and preparation should be performed before treatment, and CBCT should be used reasonably to achieve individualized and precise treatment.
Acknowledgements
The authors thank Dr. Feng Bo and Dr. Qiu Ling for advice regarding statistical analysis.
Declaration of conflicting interest
The authors declare that there is no conflict of interest.
Funding
This work was supported by the Scientific Research Foundation of the Science and Technology Department of Sichuan Province, China (grant no. 2017SZ0108).
ORCID iD
References
- 1.Racic A, Dotlic J, Janosevic L. [ Oral surgery as risk factor of odontogenic maxillary sinusitis]. Srp Arh Celok Lek 2006; 134: 191–194. DOI: 10.2298/sarh0606191r. [DOI] [PubMed] [Google Scholar]
- 2.Al-Zoubi I, Patil S, Kato I, et al. 3D CBCT assessment of incidental maxillary sinus abnormalities in a Saudi Arabian population. J Hard Tissue Biol 2017; 26: 369–372. DOI: 10.2485/jhtb.26.369. [Google Scholar]
- 3.Kottoor J, Velmurugan N, Surendran S. Endodontic management of a maxillary first molar with eight root canal systems evaluated using cone-beam computed tomography scanning: a case report. J Endod 2011; 37: 715–719. DOI: 10.1016/j.joen.2011.01.008. [DOI] [PubMed] [Google Scholar]
- 4.Tsai HH, Tan CT. Positional changes of the upper canine and posterior teeth, hard palate, and sinus floor from primary to permanent dentition. J Dent Child (Chic) 2004; 71: 48–53. [PubMed] [Google Scholar]
- 5.Valentini P, Abensur DJ. Maxillary sinus grafting with anorganic bovine bone: a clinical report of long-term results. Int J Oral Maxillofac Implants 2003; 18: 556–560. [PubMed] [Google Scholar]
- 6.Maillet M, Bowles WR, McClanahan SL, et al. Cone-beam computed tomography evaluation of maxillary sinusitis. J Endod 2011; 37: 753–757. DOI: 10.1016/j.joen.2011.02.032. [DOI] [PubMed] [Google Scholar]
- 7.Douglass CW, Valachovic RW, Wijesinha A, et al. Clinical efficacy of dental radiography in the detection of dental caries and periodontal diseases. Oral Surg Oral Med Oral Pathol 1986; 62: 330–339. DOI: 10.1016/0030-4220(86)90017-4. [DOI] [PubMed] [Google Scholar]
- 8.Marmulla R, Wortche R, Muhling J, et al. Geometric accuracy of the NewTom 9000 cone beam CT. Dentomaxillofac Radiol 2005; 34: 28–31. DOI: 10.1259/dmfr/31342245. [DOI] [PubMed] [Google Scholar]
- 9.Kilic C, Kamburoglu K, Yuksel SP, et al. An assessment of the relationship between the maxillary sinus floor and the maxillary posterior teeth root tips using dental cone-beam computerized tomography. Eur J Dent 2010; 4: 462–467. [PMC free article] [PubMed] [Google Scholar]
- 10.The American Dental Association Council on Scientific Affairs. The use of cone-beam computed tomography in dentistry. J Am Dent Assoc 2012; 143: 899–902. DOI: 10.14219/jada.archive.2012.0295. [DOI] [PubMed] [Google Scholar]
- 11.Jung YH, Cho BH. Assessment of the relationship between the maxillary molars and adjacent structures using cone beam computed tomography. Imaging Sci Dent 2012; 42: 219–224. DOI: 10.5624/isd.2012.42.4.219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Sharan A, Madjar D. Correlation between maxillary sinus floor topography and related root position of posterior teeth using panoramic and cross-sectional computed tomography imaging. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2006; 102: 375–381. DOI: 10.1016/j.tripleo.2005.09.031. [DOI] [PubMed] [Google Scholar]
- 13.Kwak HH, Park HD, Yoon HR, et al. Topographic anatomy of the inferior wall of the maxillary sinus in Koreans. Int J Oral Maxillofac Surg 2004; 33: 382–388. DOI: 10.1016/j.ijom.2003.10.012. [DOI] [PubMed] [Google Scholar]
- 14.Maspero C, Farronato M, Bellincioni F, et al. Three-dimensional evaluation of maxillary sinus changes in growing subjects: a retrospective cross-sectional study. Materials (Basel) 2020; 13: 1007. DOI: 10.3390/ma13041007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Zaman S, Alam M, Enezei H, et al. Mental foramen, inferior alveolar canal and morphology of maxillary sinus: a review. Int J Pharma Bio Sci 2015; 6: 1222–1228. [Google Scholar]
- 16.Langford RJ, Sgouros S, Natarajan K, et al. Maxillary volume growth in childhood. Plast Reconstr Surg 2003; 111: 1591–1597. DOI: 10.1097/01.Prs.0000057971.87632.37. [DOI] [PubMed] [Google Scholar]
- 17.Arias-Irimia O, Barona-Dorado C, Santos-Marino JA, et al. Meta-analysis of the etiology of odontogenic maxillary sinusitis. Med Oral Patol Oral Cir Bucal 2010; 15: e70–e73. DOI: 10.4317/medoral.15.e70. [DOI] [PubMed] [Google Scholar]
- 18.Lee KC, Lee SJ. Clinical features and treatments of odontogenic sinusitis. Yonsei Med J 2010; 51: 932–937. DOI: 10.3349/ymj.2010.51.6.932. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hameed S, Bakhshalian N, Alwazan E, et al. Maxillary sinus floor and alveolar crest alterations following extraction of single maxillary molars: a retrospective CBCT analysis. Int J Periodontics Restorative Dent 2019; 39: 545–551. DOI: 10.11607/prd.3865. [DOI] [PubMed] [Google Scholar]
- 20.Von Arx T, Fodich I, Bornstein MM. Proximity of premolar roots to maxillary sinus: a radiographic survey using cone-beam computed tomography. J Endod 2014; 40: 1541–1548. DOI: 10.1016/j.joen.2014.06.022. [DOI] [PubMed] [Google Scholar]
- 21.Tian XM, Qian L, Xin XZ, et al. An analysis of the proximity of maxillary posterior teeth to the maxillary sinus using cone-beam computed tomography. J Endod 2016; 42: 371–377. DOI: 10.1016/j.joen.2015.10.017. [DOI] [PubMed] [Google Scholar]
- 22.Gu Y, Sun C, Wu D, et al. Evaluation of the relationship between maxillary posterior teeth and the maxillary sinus floor using cone-beam computed tomography. BMC Oral Health 2018; 18: 164. DOI: 10.1186/s12903-018-0626-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ariji Y, Ariji E, Yoshiura K, et al. Computed tomographic indices for maxillary sinus size in comparison with the sinus volume. Dentomaxillofac Radiol 1996; 25: 19–24. DOI: 10.1259/dmfr.25.1.9084281. [DOI] [PubMed] [Google Scholar]
- 24.Ikeda A, Ikeda M, Komatsuzaki A. A CT study of the course of growth of the maxillary sinus: normal subjects and subjects with chronic sinusitis. ORL J Otorhinolaryngol Relat Spec 1998; 60: 147–152. DOI: 10.1159/000027584. [DOI] [PubMed] [Google Scholar]
- 25.Kim HY, Kim MB, Dhong HJ, et al. Changes of maxillary sinus volume and bony thickness of the paranasal sinuses in longstanding pediatric chronic rhinosinusitis. Int J Pediatr Otorhinolaryngol 2008; 72: 103–108. DOI: 10.1016/j.ijporl.2007.09.018. [DOI] [PubMed] [Google Scholar]
- 26.Purmal K, Alam M, Pohchi A, et al. 3D measurement of maxillary sinus height for multidisciplinary benefit. J Hard Tissue Biol 2015; 24: 225–228. DOI: 10.2485/jhtb.24.225. [Google Scholar]
- 27.Eberhardt JA, Torabinejad M, Christiansen EL. A computed tomographic study of the distances between the maxillary sinus floor and the apices of the maxillary posterior teeth. Oral Surg Oral Med Oral Pathol 1992; 73: 345–346. DOI: 10.1016/0030-4220(92)90133-b. [DOI] [PubMed] [Google Scholar]
- 28.Georgescu CE, Rusu MC, Sandulescu M, et al. Quantitative and qualitative bone analysis in the maxillary lateral region. Surg Radiol Anat 2012; 34: 551–558. DOI: 10.1007/s00276-012-0955-6. [DOI] [PubMed] [Google Scholar]
- 29.Zhang X, Li Y, Zhang Y, et al. Investigating the anatomical relationship between the maxillary molars and the sinus floor in a Chinese population using cone-beam computed tomography. BMC Oral Health 2019; 19: 282. DOI: 10.1186/s12903-019-0969-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Mustian W. The floor of the maxillary sinus and its dental, oral and nasal relations. J Am Dent Assoc 1933; 20: 2175–2218. [Google Scholar]
- 31.Dagassan-Berndt DC, Zitzmann NU, Lambrecht JT, et al. Is the Schneiderian membrane thickness affected by periodontal disease? A cone beam computed tomography-based extended case series. J Int Acad Periodontol 2013; 15: 75–82. [PubMed] [Google Scholar]
- 32.Barclay JK. Root in the maxillary sinus. Oral Surg Oral Med Oral Pathol 1987; 64: 162–164. DOI: 10.1016/0030-4220(87)90083-1. [DOI] [PubMed] [Google Scholar]
- 33.Ananda GK, Phrabhakaran Nambiar, Sunil Mutalik, et al. Anatomical considerations for implant placements in first maxillary molar extracted sites in East Asian patients. Surg Radiol Anat 2015; 37: 1099–1108. DOI: 10.1007/s00276-015-1473-0. [DOI] [PubMed] [Google Scholar]
- 34.Themkumkwun S, Kitisubkanchana J, Waikakul A, et al. Maxillary molar root protrusion into the maxillary sinus: a comparison of cone beam computed tomography and panoramic findings. Int J Oral Maxillofac Surg 2019; 48: 1570–1576. DOI: 10.1016/j.ijom.2019.06.011. [DOI] [PubMed] [Google Scholar]
- 35.Zhang YQ, Yan XB, Meng Y, et al. Morphologic analysis of maxillary sinus floor and its correlation to molar roots using cone beam computed tomography. Chin J Dent Res 2019; 22: 29–36. DOI: 10.3290/j.cjdr.a41772. [DOI] [PubMed] [Google Scholar]