Abstract
To manage the spread of coronavirus, health entities have urged the public to take preventive measures such as social distancing and handwashing. Yet, many appear reluctant to take these measures. Research is needed to understand factors underlying such reluctance, with the aim of developing targeted health interventions. We identify associating coronavirus with death as one such factor.
590 participants completed surveys in mid-March 2020, which included attitudes toward coronavirus, preventive behavioral intentions, and sociodemographic factors.
Associating coronavirus with death negatively predicted intentions to perform preventive behaviors. Further, associating coronavirus with death was not evenly distributed throughout the sample and was related with a number of sociodemographic factors including age, race, and availability of sick leave.
Following recommended preventive measures to slow the spread of coronavirus appears to relate to the degree to which people associate coronavirus with death. These findings can be used by public health researchers and practitioners to identify those for whom targeted health communication and interventions would be most beneficial, as well as to frame health messaging in ways that combat fatalism.
Keywords: COVID-19, Fatalism, Preventive behavior
Highlights
-
•
Age, race, and ability to take sick leave predict associating coronavirus with death.
-
•
Such associations are negatively correlated with preventive behaviors such as handwashing and social distancing.
-
•
The findings inform resistance to preventive behaviors and point to the need for targeted health communication.
Introduction
On March 11, 2020, the World Health Organization classified COVID-19, commonly referred to as coronavirus, as a global pandemic (Ghebreyesus, 2020). Since its first report in December 2019, coronavirus has spread to over 180 countries, taking thousands of lives (Coronavirus Map: Tracking, 2020). In the US, day-to-day life has been interrupted to an unprecedented degree as a result of precautionary measures given the widespread nature of coronavirus transmission: businesses and schools have closed, jobs have been lost, people have begun working from home, community gatherings have been cancelled, travel has been restricted, and some areas have experienced food and toiletry shortages. Worryingly, the U.S. health care system is unprepared to handle the number of coronavirus cases projected to be seen in the near future. As one stark example of this, a moderate projection in which 40% of the U.S. population contracts coronavirus during 2020 would see a shortage of hospital beds by half (Waldman, Shaw, Ngu, & Campbell, 2020).
To avoid such scenarios, the U.S. Centers for Disease Control and Prevention (CDC) along with state and local governmental entities have urged the public to adopt preventive behaviors. At this time, the known major transmission mode for coronavirus is through the exchange of respiratory fluid, often through aerosols via coughs and sneezes but also on common surfaces (van Doremalen, Bushmaker, & Morris, 2020). Its spread can be slowed by preventive practices such as social distancing (i.e., deliberately increasing the physical space between individuals and avoiding social gatherings) and handwashing (Fauci, Lane, & Redfield, 2020; Patel, 2020). Indeed, the Imperial College COVID-19 Response Team projects that such practices, in concert with mitigation policies such as quarantining positive cases, could reduce deaths by half (Ferguson et al., 2020, p. 20).
Yet, despite increasing awareness about these recommendations, polling data suggests a reluctance to perform preventive behaviors. For instance, in a March 2020 poll, while 70% of U.S. adults reported concern about coronavirus spreading to their community, less than half have taken preventive measures (aR/ewsHour/Marist, 2020a). This discrepancy between concern about coronavirus and uptake of the recommended preventive behaviors is of great public health significance. Such data points to the need to identify factors that inhibit coronavirus-relevant preventive behaviors to generate behavioral and social public health interventions that can help optimally contain the spread of coronavirus.
To be sure, there are many likely influences at play; one factor that could potentially contribute to this discrepancy between being concerned about coronavirus and inhibition of the recommended preventive behaviors is associating coronavirus with death. Why, given that coronavirus is not automatically deadly, would people associate it with death? First, health scenarios often elicit death-related cognitions, which in turn can influence health-relevant decisions (Arndt & Goldenberg, 2017). Second, the vast amount of coronavirus information and misinformation circulated on social media, cable news, and other sources may make people feel overloaded and, as a result, fatalistic. Consistent with this line of reasoning, prior research has shown that cancer information overload – that is, feeling overwhelmed by the amount of cancer information in the environment – is related to fatalistic perceptions (Jensen et al., 2014). Finally, given that coronavirus is often paired with death when portrayed in the media, it seems likely that people will internalize this association, particularly if they belong to groups portrayed as vulnerable.
In the present context, associating coronavirus with death – a coronavirus related mortality salience so to speak – could belie a fatalistic perception of coronavirus as a death sentence. Even a generalized connection between coronavirus and death may make health issues
seem uncontrollable (Straughan, Seow, 1998), thus inhibiting the performance of preventive behaviors. Fatalistic thinking (i.e., fatalism) has been widely found to undermine preventive behaviors in other diseases in which vaccines are currently not available (Niederdeppe & Levy, 2007). For instance, empirical evidence from an analysis of the Health Information National Trends Survey (HINTS), a national study on cancer-related attitudes and behaviors, found that the degree to which people agreed with the statement, “When I hear about cancer, I automatically think of death” predicted reported physician avoidance (Moser, Arndt, Jimenez, & Hesse, 2014). A subsequent study found that age and subjective health status were predictive of believing cancer to be a death sentence; specifically, younger (as compared to older) individuals and those with poorer (as compared to fairer) health were more likely to automatically associate cancer and death (Moser, Arndt, Jimenez, & Hesse, n.d.). Similarly, in the context of the HIV epidemic, fatalistic thinking has also been linked to increased HIV risk behaviors (i.e., condomless sex) (Yi, Sandfort, & Shidlo, 2010).
If associating coronavirus with death is found to predict reluctance to perform preventive behaviors, then it is vital to identify characteristics of individuals most likely to perceive this cognitive association. This identification will allow public health researchers and practitioners to develop targeted interventions aimed at increasing preventive behaviors. Given the specifics of coronavirus, it is unclear which factors would predict associating coronavirus with death. To fill in this gap, the purpose of this study is to: (1) identify factors that predict associating coronavirus with death; and (2) assess the relationship between associating coronavirus with death and preventive behavioral intentions such as social distancing and handwashing.
Methods
Study description, sample, and procedures
Two samples were recruited via Amazon's Mechanical Turk (Mturk) using CloudResearch. Mturk is an online platform widely used by researchers to recruit participants to complete online surveys. The first sample (N = 300), focusing on sociodemographic predictors of associating coronavirus with death, was collected on March 5, while the second sample (N = 290), focusing on the associations between coronavirus related mortality salience and preventive behavioral intentions, was collected on March 18. Detailed descriptions of all study materials and procedures can be found in the supplementary materials; the key difference in materials between samples was that the second sample included preventive behavioral intentions. Eligible participants completed a brief (10–15 min), one-time, cross-sectional web-based survey; the survey was accessible in English via electronic devices (e.g., laptop, smartphones, or tablet computers).
To be eligible for this study, participants had to (1) be at least 18 years old and (2) based in the United States. A number of web-based best practice measures were taken to ensure data quality. First, to eliminate potential bots from completing the survey, we included a captcha in the consent form. Second, following recommendations (Barends & de Vries, 2019), we included an attention check intended to screen out inattentive participants. This consisted of an item that instructed participants to select a specific response; participants who selected a different response (n = 12) were excluded from analyses. It must be noted that many populations in the U.S. would not be represented in the samples. For example, those who do not speak English and those without internet and computer access would not be reached by the present recruitment strategy. Such a strategy – recruiting participants from Mturk – affords an initial opportunity to examine the proposed psychological processes as the coronavirus pandemic unfolds.
All enrolled participants provided electronic written informed consent. All study procedures were approved by the Institutional Review Board at the University of Missouri.
Measures
Sociodemographic factors
Participants were asked to indicate their age, race, income, gender, political conservatism (1 [very liberal] to 7 [very conservative]), subjective health status (1 [very bad] to 5 [very good]), perceived ability to receive medical treatments (1 [definitely not] to 5 [definitely yes]), and perceived ability to take sick leave (1 [definitely not] to 5 [definitely yes]).
Coronavirus knowledge, worry, and intentions
Three questions assessed coronavirus knowledge, worry, and intentions scored on a scale of 1 (not at all) to 7 (a lot). Assessing knowledge about coronavirus, we asked, “How much have you heard about coronavirus (also known as COVID-19)?“. Measuring coronavirus worry, we asked, “How much are you worried about coronavirus (also known as COVID-19)?“. Finally, participants indicated their intentions to get tested for coronavirus if showing symptoms; “I plan to get tested for coronavirus if I have symptoms such as a fever and shortness of breath”.
Work-related self-esteem
To measure the tendency to derive self-esteem from work, we adapted seven items from the Contingencies of Self-Worth scale (Crocker, Luhtanen, Cooper, & Bouvrette, 2003). Items, scored on a one (strongly disagree) to seven (strongly agree) scale, included “When I do well at my job, I feel good about myself” and “I could not respect myself if I did poorly at my job”. Two items were removed to improve scale reliability (α = 0.69).
Associating coronavirus with death
An adapted item (Moser et al., 2014), which asked, “How much do you agree or disagree with the following statement? When I hear about coronavirus, I automatically think of death”, was included to assess perceiving associations between coronavirus and death. Participants responded to this question on a scale of 1 (strongly disagree) to 7 (strongly agree).
Preventive behavioral intentions
At the time of data collection (March 2020), the CDC recommended a number of preventive behaviors intended to slow the spread of coronavirus. These included, among others, avoiding close interpersonal contact (i.e., social distancing) and thorough handwashing. To assess intentions to perform these recommended preventive behaviors, we included eight items measured on a 1 (strongly disagree) to 7 (strongly agree) scale. Six items focused on social distancing (α = 0.75; e.g., “I intend to practice social distancing in the upcoming weeks”) and two focused on handwashing (α = 0.67; e.g., “I intend to wash my hands frequently in order to reduce my chances of catching coronavirus”).
Analysis
Descriptive statistics are summarized by study sample and tested for differences between the two samples. To determine internal reliability, we conducted sensitively analysis of our scaled variables. Then, a series of linear and multivariate regressions were employed. For the first sample, all sociodemographic factors, coronavirus knowledge, coronavirus attitudes, coronavirus worry, and work-related self-esteem were simultaneously used to predict associating coronavirus with death. Significant predictors were then included as control variables in a multivariate regression, which simultaneously predicted social distancing and handwashing from associating coronavirus with death. All statistical analyses were conducted in SPSS version 26.
Results
Sample characteristics
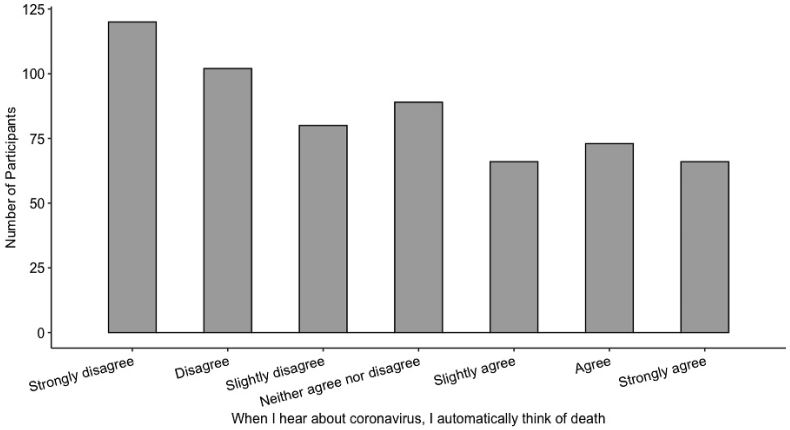
Sample characteristics, and variable means and standard deviations are displayed in Table 1a, Table 1ba and 1b. The majority of the sample felt they were exposed to a lot of coronavirus information and had coronavirus-related worries. People generally indicated high social distancing (5.7/7), handwashing (6.1/7), and screening intentions (5.6/7). Across both samples, 45% were cisgender women, 66% were White, with an age range of 18–74 (Mage = 37.12, SDage = 12.03). As the number of deaths from coronavirus in the U.S. increased from 11 to 108 between the two dates of data collection (March 5th and 18th), it was possible that the association between coronavirus and death would increase over time, thus affecting our outcomes of interest. A one-way ANOVA revealed no difference in the association between coronavirus with death on March 5th (M = 3.48, SD = 2.07) and on March 18th (M = 3.66, SD = 1.93) (F(1, 582) = 1.17, p = .28, η2 = 0.002). The distribution of associating coronavirus with death is displayed in (Fig. 1)
Table 1a.
Descriptive statistics.
| Variables | M | SD |
|---|---|---|
| Exposure to coronavirus information† | 6.23 | 1.07 |
| Perceiving coronavirus with death† | 3.61 | 2.02 |
| Coronavirus-related worry† | 4.88 | 1.79 |
| Social distancing intentions† | 5.77 | .97 |
| Handwashing intentions† | 6.10 | 1.01 |
| Political conservatism† | 3.89 | 1.93 |
| Subjective health status‡ | 4.12 | .71 |
| Work-related self-esteem† | 5.21 | .99 |
| Intentions to get tested if showing symptoms† | 5.66 | 1.49 |
| Perceived ability to receive medical treatments‡ | 3.73 | 1.22 |
| Perceived ability to take sick leave‡ | 3.97 | 1.22 |
Scored on a 1–7 scale; ‡Scored on a 1–5 scale. N = 590.
Table 1b.
Study demographics.
| Total Sample |
Sample 1 |
Sample 2 |
|
|---|---|---|---|
| n (%) | n (%) | n (%) | |
| Age | |||
| Mean ± SD | 37.12 ± 12.03 | 36.11 ± 11.46 | 37.93 ± 12.39 |
| Min-max | 18–74 | 18–74 | 18–73 |
| Race/ethnicity | |||
| White∗ | 413 (69.8) | 221 (72.7) | 198 (62.9) |
| Black | 119 (20.1) | 59 (19.4) | 66 (21) |
| Asian∗ | 46 (7.8) | 15 (4.9) | 31 (9.8) |
| American Indian or Alaska Native | 5 (0.8) | 2 (.7) | 3 (1.0) |
| Native Hawaiian or Pacific Islander | 4 (0.7) | 2 (.7) | 2 (.6) |
| Another race/ethnicity | 14 (2.4) | 6 (2.0) | 8 (2.5) |
| Income | |||
| Less than $10,000 | 25 (4.2) | 7 (2.3) | 18 (5.7) |
| $10,000 to $29,999 | 95 (16.1) | 50 (16.5) | 47 (14.9) |
| $30,000 to $49,999 | 151 (25.5) | 79 (26.0) | 78 (24.7) |
| $50,000 to $69,999 | 131 (22.1) | 67 (22.1) | 65 (20.6) |
| $70,000 to $99,999 | 108 (18.2) | 58 (19.1) | 53 (16.8) |
| $100,000 and more | 81 (13.7) | 42 (13.8) | 39 (12.4) |
| Gender∗ | |||
| Cisgender women | 270 (45.7) | 122 (40.1) | 150 (47.6) |
| Cisgender men | 319 (54.1) | 180 (59.2) | 148 (47.0) |
| Transgender or gender nonconforming | 1 (.002) | 1 (.3) | 2 (.6) |
Indicates a significant difference (p < .05) between samples. N = 590.
Fig. 1.
Distribution of associating coronavirus with death across studies 1 and 2
Outcomes
Associated factors of associating coronavirus with death
Overall, age, race, coronavirus-related worry, perceived ability to take sick leave, and work-related self-esteem were each predictive of associating coronavirus with death (Table 2). There was a positive correlation between coronavirus-related worry and associating coronavirus with death (b = 0.43, 95% CI = [0.32, 0.55], p < .001). There was a negative relationship between age and associating coronavirus with death (b = .02, 95% CI = [-0.03, −0.001], p = .04). That is, older adults were less likely to hold this perception than were younger adults. Race (coded as Black = 1, non-Black = 0) positively predicted associating coronavirus with death (b = 1.36, 95% CI = [0.64, 2.08], p < .001). Having the ability to take sick leave negatively predicted associating coronavirus with death (b = −0.27, 95% CI = [-0.46, −0.08], p = .01). Finally, there was a positive association between work-related self-esteem and associating coronavirus with death (b = 0.37, 95% CI = [0.15, 0.60], p < .001).
Table 2.
Regression predicting perceiving coronavirus with death.
| b | 95% CI | SE | p | |
|---|---|---|---|---|
| Race: Black | 1.36 | .64–2.08 | .37 | < .001 |
| Coronavirus-related worry | .43 | .32–.55 | .06 | < .001 |
| Work-related self-esteem | .37 | .15–.60 | .11 | .001 |
| Perceived ability to take sick leave | -.27 | -.46–-.08 | .10 | .01 |
| Age | -.02 | -.03–-.001 | .01 | .04 |
| Race: White | .59 | -.03 – 1.22 | .32 | .06 |
| Gender | -.26 | -.66 – .15 | .20 | .21 |
| Subjective health status | -.25 | -.54 – .04 | .15 | .09 |
| Exposure to coronavirus information | -.16 | -.36 – .04 | .10 | .12 |
| Income | .05 | -.02 – .12 | .04 | .19 |
| Perceived ability to get medical treatment | .03 | -.17 – .23 | .10 | .77 |
| Political conservatism | .02 | -.09 – .13 | .06 | .74 |
Note: Regression coefficients are unstandardized. Race: White is coded as White = 1, non-White = 0; Race: Black is coded as Black = 1, non-Black = 0. Significant factors (p < .05) are bolded. N = 290.
Further examining the racial discrepancy, a one-way ANOVA showed that Black participants (M = 4.92, SD = 2.24) associated coronavirus with death more than did White participants (M = 3.07, SD = 1.83), (F(1, 292) = 47.21, p < .001, η2 = 0.14). This difference remained significant when controlling for work-related self-esteem, subjective health status, perceived ability to take sick leave, perceived ability to receive necessary medical treatments, political conservatism, and income.
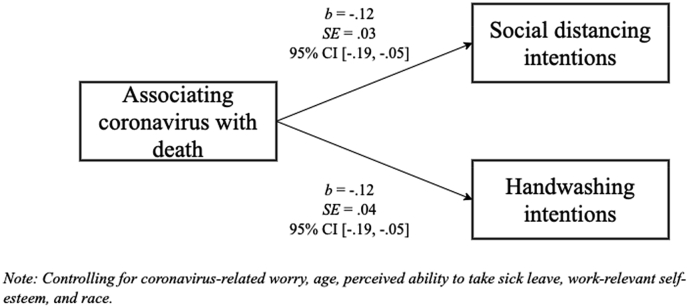
Associating coronavirus with death and preventive behavioral intentions
A multivariate regression was used to assess the relationship between associating coronavirus with death and preventive behavioral intentions. The model predicted the two dependent variables – social distancing and handwashing intentions – from associating coronavirus with death, while controlling for coronavirus-related worry, age, race (coded as Black and non-Black), perceived ability to take sick leave, and work-related self-esteem (the direct association between these sociodemographics and preventive behavioral intentions are displayed in Tables 3 and 4). Results revealed that associating coronavirus with death negatively predicted social distancing (b = −0.12, SE = 0.03, 95% CI = [-0.19, −0.05], p < .001) and handwashing intentions (b = −0.12, SE = 0.04, 95% CI = [-0.19, −0.05], p < .001) (Fig. 2). That is, the more people associated coronavirus with death, the less likely they were to report intentions to perform recommended preventive behaviors.
Table 3.
Direct associations between sociodemographics and social distancing intentions.
| b | 95% CI | SE | p | |
|---|---|---|---|---|
| Race: Black | -.25 | -.54 – .05 | .15 | .10 |
| Coronavirus-related worry | .12 | .05–.19 | .04 | .001 |
| Work-related self-esteem | .11 | -.01 – .23 | .06 | .07 |
| Perceived ability to take sick leave | .24 | .13–.35 | .05 | <.001 |
| Age | .02 | .01–.03 | .01 | .001 |
Note: Regression coefficients are unstandardized. Race: Black is coded as Black = 1, non-Black = 0. Significant factors (p < .05) are bolded. N = 290.
Table 4.
Direct associations between sociodemographics and handwashing intentions.
| b | 95% CI | SE | p | |
|---|---|---|---|---|
| Race: Black | -.10 | -.40 – .20 | .15 | .50 |
| Coronavirus-related worry | .16 | .09–.23 | .04 | <.001 |
| Work-related self-esteem | .18 | .06–.30 | .06 | .004 |
| Perceived ability to take sick leave | .16 | .05–.27 | .06 | .004 |
| Age | .02 | .01–.03 | .01 | .002 |
Note: Regression coefficients are unstandardized. Race: Black is coded as Black = 1, non-Black = 0. Significant factors (p < .05) are bolded. N = 290.
Fig. 2.
Multivariate regression results prediting preventive behavioral intentions from associating coronavirus with death.
Discussion
The present findings identify one factor underlying reluctance to perform preventive behaviors recommended for slowing the spread of coronavirus: associating coronavirus with death. Further, we show that associating coronavirus with death is predicted by a host of sociodemographic factors, including coronavirus-related worry, age, race, perceived ability to take sick leave, and work-related self-esteem. These findings are broadly consistent with the health fatalism literature and can inform coronavirus-related health communication strategies, specifically identifying segments of the population – Black, young, and those without sick leave – that would benefit most from interventions aimed at promoting preventive behaviors.
Given that the particular vulnerability of older adults to coronavirus morbidity and mortality has received considerable media attention, it was expected that associating coronavirus with death would be positively associated with age. However, an opposite pattern emerged; younger adults were more likely than older adults to associate coronavirus with death. This relationship did not change when controlling for political conservatism. This is interesting to note given the initial partisan media coverage of coronavirus, with many conservative outlets downplaying the seriousness of the pandemic. Although the direction of this age effect is surprising, this finding is consistent with other research showing a negative relationship between age and perceiving cancer as a death sentence (Moser, Arndt, Jimenez, & Hesse, n.d.). There are a number of possible explanations for why there was such an association between age and perceiving coronavirus as a death sentence, which future research may explore. First, it is possible that older adults are more able than are younger adults to handle threatening health information without holding fatalistic beliefs. Second, younger people may tend to be more fatalistic in regard to health given the potential years of life lost. Moreover, this finding suggests that public health messaging regarding preventive behaviors may not be reaching or resonating with younger audiences (Parvanta, Nelson , Parvanta , & Harner , 2010). In fact, early messaging about coronavirus suggested that younger people were less likely to experience severe illness and death due to the virus. Given that younger adults (age 20 to 54) currently make up nearly 40% of coronavirus hospitalizations in U.S. (CDCMMWR, 2020), there is a need for careful segmentation of public health messaging for this age group; one that denotes their severity and vulnerability for acquiring and transmitting coronavirus.
Black individuals in this sample were also particularly likely to associate coronavirus with death. While confidence in this finding should be tempered by the relatively small Black sample (n = 119), it is broadly consistent with prior research showing that fatalism is particularly experienced among Black (as compared to White) people (Powe, 1994), which can be understood as a reaction to historical and contemporary injustice (Powe & Johnson, 1995). Black people's experience with medical racism in the US has been widely documented and has had significant impacts on fatalistic beliefs (Hoberman, 2012). However, the relationship between fatalism and preventive behaviors is varied. For example, studies have shown that Black people who perceive racism (Ford et al., 2019) or hold HIV conspiracy beliefs (Bohnert & Latkin, 2009) are more likely to engage in HIV screening.
It is possible that those without sick leave were more likely to associate coronavirus with death because they may assume that continued work leaves them susceptible to coronavirus transmission and that a lack of sick leave will leave them unable to receive treatment. An inability to take sick leave may contribute to limited perceived personal control over prevention options (Náfrádi, Nakamoto, & Schulz, 2017). Addressing such perceptions should be done through both interventions and policy. For essential workers, individual-level interventions should attempt to disrupt the association between coronavirus and death, perhaps by emphasizing the efficacy of preventive behaviors. For non-essential workers, policies such as the newly passed guaranteed sick leave in New York (Unger, 2020) might prove more beneficial. As suggested by other studies (Hammig & Bouza, 2019), such measures may have positive downstream effects on the practicing of preventive behaviors.
Interestingly, the present finding that associating coronavirus with death negatively predicted preventive behavioral intentions is seemingly at odds with the Health Belief Model (HBM) (Janz, Becker, 1984). According to the HBM, the perceived severity of a potential health issue should be positively related to preventive behavioral intentions (Carpenter, 2010). Thus, in the current case, the HBM would predict that greater associations between coronavirus and death would predict greater social distancing and handwashing intentions. As this was not the case, and other research has similarly shown that associating cancer with death predicts physician avoidance (Moser et al., 2014), it seems likely that, while conceptually similar, severity and fatalism do not always predict behavioral intentions in the same way. Moreover, there is considerable research derived from protection motivation theory and other such perspectives that indicates the impact of perceived severity on health behavior change can be moderated by perceptions of (personal and response) efficacy (Kok et al., 2018, Prentice-Dunn and Rogers, 1986). Future work might seek to distinguish these fatalism and severity, perhaps by examining factors that lead to, and those which follow from, perceptions of efficacy, severity, and experiences of fatalism.
Understanding the centrality of associating coronavirus with death in relevant health behaviors can benefit health researchers and practitioners alike. Researchers should continue to investigate factors that influence whether people associate coronavirus with death, particularly as death tolls continue to mount; the pandemic is developing at a rapid rate, which is likely to influence the degree to which people associate coronavirus with death. Those in medicine and public health might utilize the degree to which people associate coronavirus with death as a tool to direct how best to communicate. As suggested by the present studies, those who strongly hold such a perception are least likely to perform necessary preventive behaviors, and thus the most likely to benefit from targeted interventions.
Limitations
While the present studies provide preliminary evidence regarding factors that contribute to coronavirus-related preventive behaviors, they are not without limitation. First, the convenience samples used were not nationally representative in terms of gender, age, and race, and relied on self-reports of attitudes and behavioral intentions. Further, as the sample only included English-speaking U.S. residents, it remains unclear whether the findings can be extrapolated outside of this context. Second, as a cross-sectional study, we cannot claim causality, nor can we rule out the possibility that fatalistic beliefs may be influenced by individuals’ willingness to engage in preventive behaviors. Third, as the samples consisted of American participants, it is unclear whether the results are applicable to other national contexts. Supplementary work should address these limitations by recruiting nationally representative samples, using experimental and ecological methods, and testing the relationship between associating coronavirus with death and preventive behaviors in non-U.S. countries. Further, future research may examine how specific sources of coronavirus-related information (e.g., social media) shape the degree to which people associate coronavirus with death and intentions to perform preventive behaviors.
Conclusion
As coronavirus continues to spread, research on factors that inhibit preventive behaviors is urgently needed. The present study offers novel empirical evidence that associating coronavirus with death predicts reluctance to perform recommended preventive behaviors such as social distancing and handwashing. Further, we show that coronavirus-related worry, age, race, perceived ability to take sick leave, and work-related self-esteem are predictive of associating coronavirus with death. These findings can help inform our understanding of and responses to the global coronavirus pandemic.
Ethics approval
All research in this manuscript was approved by the University of Missouri Institutional Review Board. We have no conflicts of interest. Personal research funds were used to support this study. Tyler Jimenez, Dr. Arjee Restar, Rebekah Israel Cross, and Deanna Barath are supported by the Robert Wood Johnson Foundation's Health Policy Research Scholars program. Dr. Restar is supported by the National Institute of Allergy and Infectious Diseases under grant T32AI102623.
CRediT authorship contribution statement
Tyler Jimenez: Conceptualization, Methodology, Formal analysis, Investigation, Writing - original draft, Visualization, Project administration. Arjee Restar: Writing - review & editing, Project administration. Peter J. Helm: Methodology, Formal analysis, Investigation, Writing - review & editing. Rebekah Israel Cross: Writing - review & editing. Deanna Barath: Writing - review & editing. Jamie Arndt: Methodology, Investigation, Resources, Writing - review & editing, Supervision.
Footnotes
Supplementary data related to this article can be found at https://doi.org/10.1016/j.ssmph.2020.100615.
Appendix A. Supplementary data
The following is the supplementary data related to this article:
References
- NPR/PBS NewsHour/marist poll results: Coronavirus | home of the marist poll. 2020. http://maristpoll.marist.edu/npr-pbs-newshour-marist-poll-results-coronavirus/ Published. [Google Scholar]
- Arndt J., Goldenberg J.L. Where health and death intersect: Insights from a terror management health model. Current Directions in Psychological Science. 2017;26(2):126–131. doi: 10.1177/0963721416689563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barends A.J., de Vries R.E. Noncompliant responding: Comparing exclusion criteria in MTurk personality research to improve data quality. Personality and Individual Differences. 2019;143:84–89. doi: 10.1016/j.paid.2019.02.015. [DOI] [Google Scholar]
- Bohnert A.S.B., Latkin C.A. HIV testing and conspiracy beliefs regarding the origins of HIV among african Americans. AIDS Patient Care and STDs. 2009;23(9):759–763. doi: 10.1089/apc.2009.0061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carpenter C.J. A meta-analysis of the effectiveness of health belief model variables in predicting behavior. Health Communication. 2010;25(8):661–669. doi: 10.1080/10410236.2010.521906. [DOI] [PubMed] [Google Scholar]
- CDCMMWR Severe outcomes among patients with coronavirus disease 2019 (COVID-19) — United States, february 12–march 16, 2020. MMWR Morb Mortal Wkly Rep. 2020;69 doi: 10.15585/mmwr.mm6912e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coronavirus Map: Tracking the global outbreak . The New York Times. Published; 2020. https://www.nytimes.com/interactive/2020/world/coronavirus-maps.html Accessed March 19, 2020. [Google Scholar]
- Crocker J., Luhtanen R.K., Cooper M.L., Bouvrette A. Contingencies of self-worth in College students: Theory and measurement. Journal of Personality and Social Psychology. 2003;85(5):894–908. doi: 10.1037/0022-3514.85.5.894. [DOI] [PubMed] [Google Scholar]
- Fauci A.S., Lane H.C., Redfield R.R. Covid-19 — navigating the uncharted. New England Journal of Medicine. 2020 doi: 10.1056/NEJMe2002387. 0(0):null. doi. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ferguson N.M., Laydon D., Nedjati-Gilani G. 2020. Impact of non-pharmaceutical interventions (NPIs) to reduce COVID- 19 mortality and healthcare demand. Published online. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ford C.L., Daniel M., Earp J.A.L., Kaufman J.S., Golin C.E., Miller W.C. Perceived everyday racism, residential segregation, and HIV testing among patients at a sexually transmitted disease clinic. American Journal of Public Health. 2019;99(1):137–143. doi: 10.2105/AJPH.2007.120865. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ghebreyesus T.A. World Health Organization; 2020. WHO director-general’s opening remarks at the media briefing on COVID-19 - 11 March 2020.https://www.who.int/dg/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19---11-march-2020 Accessed March 21, 2020. [Google Scholar]
- Hammig B., Bouza B. Paid sick leave benefits and adherence to recommended screening tests among male labor workers in the United States. Journal of Occupational and Environmental Medicine. 2019;61(2):102–106. doi: 10.1097/JOM.0000000000001481. [DOI] [PubMed] [Google Scholar]
- Hoberman J. University of California Press; 2012. Black and blue: The origins and consequences of medical racism. [Google Scholar]
- Janz N.K., Becker M.H. The health belief model: A decade later. Health Education Quarterly. 1984;11(1):1–47. doi: 10.1177/109019818401100101. d84. [DOI] [PubMed] [Google Scholar]
- Jensen J.D., Carcioppolo N., King A.J., Scherr C.L., Jones C.L., Niederdeppe J. The cancer information overload (CIO) scale: Establishing predictive and discriminant validity. Patient Education and Counseling. 2014;94(1):90–96. doi: 10.1016/j.pec.2013.09.016. [DOI] [PubMed] [Google Scholar]
- Kok G., Peters G.-J.Y., Kessels L.T.E., Hoor GA ten, Ruiter R.A.C. Ignoring theory and misinterpreting evidence: The false belief in fear appeals. Health Psychology Review. 2018;12(2):111–125. doi: 10.1080/17437199.2017.1415767. [DOI] [PubMed] [Google Scholar]
- Moser R.P., Arndt J., Han P.K., Waters E.A., Amsellem M., Hesse B.W. Perceptions of cancer as a death sentence: Prevalence and consequences. Journal of Health Psychology. 2014;19(12):1518–1524. doi: 10.1177/1359105313494924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moser, R. P., Arndt, J., Jimenez, T., & Hesse, B. W. (under review). Perceptions of cancer fatalism by geography: Tracking trends in public perceptions from 2008 to 2017. under review. Submitted for publication. [DOI] [PubMed]
- Náfrádi L., Nakamoto K., Schulz P.J. Is patient empowerment the key to promote adherence? A systematic review of the relationship between self-efficacy, health locus of control and medication adherence. PloS One. 2017;12(10) doi: 10.1371/journal.pone.0186458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Niederdeppe J., Levy A.G. Fatalistic beliefs about cancer prevention and three prevention behaviors. Cancer Epidemiol Biomarkers Prev. 2007;16(5):998–1003. doi: 10.1158/1055-9965.EPI-06-0608. [DOI] [PubMed] [Google Scholar]
- Parvanta C., Nelson D.E., Parvanta S.A., Harner R.N. Essentials of public health communication. Jones & bartlett publishers. 2010. https://books.google.com/books?hl=en&lr=&id=FPrIgJslUeQC&oi=fnd&pg=PP1&dq=Parvanta,+C.+F.+(2010).+Essentials+of+public+health+communication:+&ots=NwWHeVC0GI&sig=z6LQ3d6nGpCR3T_-Ts4Qb1fsZPE#v=onepage&q=Parvanta%2C%20C.%20F.%20(2010).%20Essentials%20of%20public%20health%20communication%3A&f=false Accessed March 22, 2020.
- Patel A. Initial public health response and interim clinical guidance for the 2019 novel coronavirus outbreak — United States, december 31, 2019–february 4, 2020. MMWR Morb Mortal Wkly Rep. 2020;69 doi: 10.15585/mmwr.mm6905e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Powe B.D. Perceptions of cancer fatalism among african Americans: The influence of education, income, and cancer knowledge. Journal of National Black Nurses' Association. 1994;7(2):41–48. [PubMed] [Google Scholar]
- Powe B.D., Johnson A. Fatalism as a barrier to cancer screening among African-Americans: Philosophical perspectives. Journal of Religion and Health. 1995;34(2):119–126. doi: 10.1007/BF02248767. [DOI] [PubMed] [Google Scholar]
- Prentice-Dunn S., Rogers R.W. Protection motivation theory and preventive health: Beyond the health belief model. Health Education Research. 1986;1(3):153–161. doi: 10.1093/her/1.3.153. [DOI] [Google Scholar]
- Straughan P.T., Seow A. Fatalism reconceptualized: A concept to predict health screening behavior. Journal of Gender, Culture and Health. 1998;3(2):85–100. doi: 10.1023/A:1023278230797. [DOI] [Google Scholar]
- Unger A. Cuomo signs bill to guarantee sick leave for New Yorkers during COVID-19 outbreak. WKBW Buffalo. 2020 https://www.wkbw.com/news/coronavirus/cuomo-signs-bill-to-guarantee-sick-leave-for-those-under-quarantine-in-ny Published. [Google Scholar]
- van Doremalen N., Bushmaker T., Morris D.H. Aerosol and surface stability of HCoV-19 (SARS-CoV-2) compared to SARS-CoV-1. New England Journal of Medicine. 2020;382(16):1564–1567. doi: 10.1056/NEJMc2004973. https://www.medrxiv.org/content/10.1101/2020.03.09.20033217v2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Waldman A., Shaw A., Ngu A., Campbell S. ProPublica. Published; 2020. Are hospitals near me ready for coronavirus? Here are nine different scenarios.https://projects.propublica.org/graphics/covid-hospitals Accessed March 19, 2020. [Google Scholar]
- Yi H., Sandfort T.G.M., Shidlo A. Effects of disengagement coping with HIV risk on unprotected sex among HIV-negative gay men in New York city. Health Psychology. 2010;29(2):205–214. doi: 10.1037/a0017786. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.