Abstract
Coronaviruses (CoVs), a family of enveloped positive-sense RNA viruses, are characterized by club-like spikes that project from their surface, unusually large RNA genome, and unique replication capability. CoVs are known to cause various potentially lethal human respiratory infectious diseases, such as severe acute respiratory syndrome (SARS), Middle East respiratory syndrome (MERS), and the very recent coronavirus disease 2019 (COVID-19) outbreak. Unfortunately, neither drug nor vaccine has yet been approved to date to prevent and treat these diseases caused by CoVs. Therefore, effective prevention and treatment medications against human coronavirus are in urgent need. In the past decades, many natural compounds have been reported to possess multiple biological activities, including antiviral properties. In this article, we provided a comprehensive review on the natural compounds that interfere with the life cycles of SARS and MERS, and discussed their potential use for the treatment of COVID-19.
Key words: Natural compounds, Coronavirus, RNA-Virus, MERS-CoV, SARS-CoV, SARS-CoV-2, COVID-19
Abbreviations: ACE2, angiotensin-converting enzyme 2; BALF, bronchoalveolar lavage fluid; CoVs, coronaviruses; COVID-19, coronavirus disease 2019; DAT, desaminotyrosine; ER, endoplasmic reticulum; ERGIC, endoplasmic reticulum–Golgi intermediate compartment; HCoVs, human coronaviruses; HLH, hemophagocytic lymphohistiocytosis; HR, heptad repeats; HSV, herpes simplex virus; IL, interleukin; LHQWC, Lian-Hua-Qing-Wen Capsule; MERS, Middle East respiratory syndrome; MERS-CoV, Middle East respiratory syndrome coronavirus; MAPK, mitogen-activated protein kinase; N protein, nucleocapsid protein; NF-κB, nuclear factor-κB; NCIP, novel coronavirus-infected pneumonia; PLpro, papain-like protease; PI3K, phosphoinositide 3-kinases; RTC, replication transcription complex; S protein, spike protein; RdRp, RNA-dependent RNA polymerase; SARS, severe acute respiratory syndrome; SARS-CoV, severe acute respiratory syndrome coronavirus; SARS-CoV-2, severe acute respiratory syndrome coronavirus 2; STAT, signal transducer and activator of transcription; TCM, traditional Chinese medicine; WHO, World Health Organization; 3CLpro, chymotrypsin-like protease
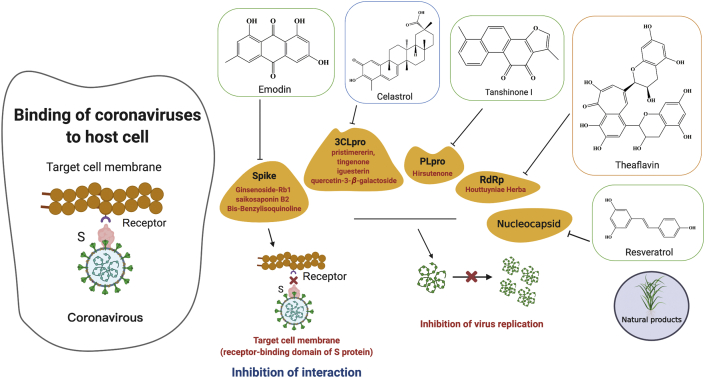
Graphical abstract
Chinese herbal medicines and natural compounds possess promising antiviral effects against Human coronaviruses (HCoVs) and provide a rich resource for novel antiviral drug development. This review provides an update on natural compounds against HCoVs and summarizes the active natural compounds and their possible action mechanisms.
1. Introduction
Coronaviruses (CoVs) comprise a large family of RNA viruses that infect a wide variety of mammalian and avian hosts, and cause a broad spectrum of diseases1. CoVs have a single-stranded, positive-sense RNA genome and comprise four genera of α-, β-, γ- and δ-coronaviruses2,3. CoVs are prone to mutation and recombination during replication, and this propensity has contributed to the diversity of coronavirus. Human coronaviruses (HCoVs) are known respiratory pathogens associated with a wide range of respiratory outcomes4. The advent of severe acute respiratory syndrome coronavirus (SARS-CoV) and Middle East respiratory syndrome coronavirus (MERS-CoV) in the past two decades have thrust HCoVs into the spotlight in the research community due to their high pathogenicity in humans5. More recently, the sudden emergence of a new coronavirus discovered at the end of 2019 has caused a major outbreak of human fatal pneumonia with a widespread global impact, and this infectious disease caused by the new coronavirus has been named coronavirus disease 2019 (COVID-19) by the World Health Organization (WHO)6,7. We have now known that the causative agent of this outbreak is a novel coronavirus phylogenetically in the SARS-CoV clade, hence referred to as severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). The SARS-CoV-2 is more widespread than the SARS-CoV8,9.
The common respiratory symptoms of a person infected with coronavirus include fever, cough, shortness of breath, and dyspnea. In more severe cases, infection can cause pneumonia, severe acute respiratory syndrome, kidney failure and even death10,11. By 20 May 2020, this potentially fatal virus has caused more than 4.98 million confirmed infected cases and resulted in over 327,000 deaths globally. COVID-19 has spread to more than 200 countries around the world, and its outbreak has seen no signs of abating. Unfortunately, despite extensive efforts have been devoted to the development of anti-coronavirus agents, effective therapeutics for coronavirus infection have remained elusive so far12. A lack of effective immunization and antiviral drugs poses a daunting challenge to current global efforts to contain the COVID-19 outbreak13,14. Thus, there clearly exists an unmet medical need for effective antivirals to manage the current COVID-19 pandemic.
Herbal medicines and medicinal plant-based natural compounds provide a rich resource for novel antiviral drug development. Some natural medicines have been shown to possess antiviral activities against various virus strains including coronavirus, herpes simplex virus15, 16, 17, 18, 19, 20, influenza virus21,22, human immunodeficiency virus23, 24, 25, hepatitis B and C viruses26, 27, 28, SARS and MERS29,30. To date, dozens of Chinese herbs and hundreds of natural compounds have been reported to possess antiviral activities. The past few decades have also witnessed tremendous efforts in revealing the antiviral action mechanisms of these natural agents on the influence of the viral life cycle, such as viral entry, replication, assembly, and release, as well as virus-host-specific interactions. The purpose of this review is to provide an update on natural products that have promising antiviral effects against coronaviruses and discuss their molecular targets and mechanisms.
2. Life cycle and pathogenesis of coronavirus
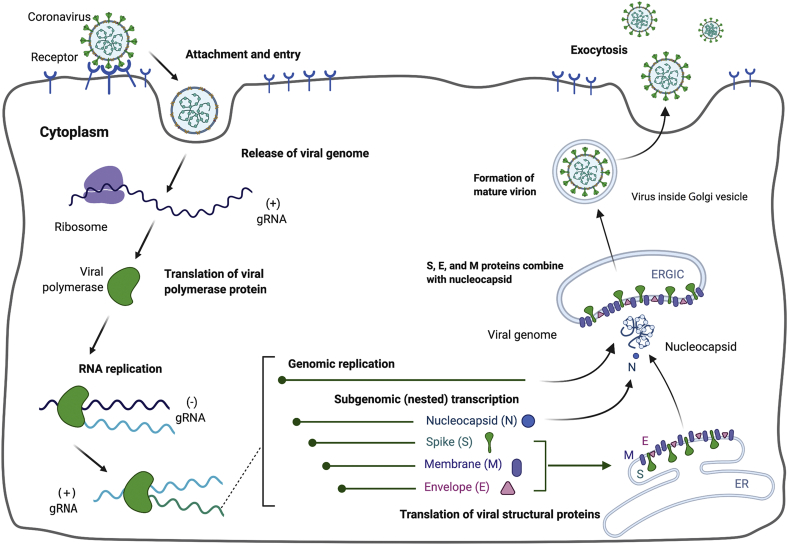
To understand the life cycle and pathogenesis of coronavirus is of importance for the development of anti-CoV agents. Coronavirus infection is initiated by the binding of virions to cellular receptors (Fig. 1). This sets off a series of events culminating in the deposition of the nucleocapsid into the cytoplasm, where the viral genome becomes available for translation.
Figure 1.
The life cycle of coronavirus. Coronavirus infections are initiated by the binding of virions to cellular receptors. After binding, virus accesses to host cell and is released to the cytosol of host cell. Viral RNA is translated by viral polymerase. Following replication and subgenomic RNA synthesis, the viral structural proteins, spike (S), envelope (E), and membrane (M) are translated and inserted into the endoplasmic reticulum (ER). These proteins move along the secretory pathway into the membranes of endoplasmic reticulum–Golgi intermediate compartment (ERGIC) and combine with nucleocapsid (N) protein. Virus goes inside the Golgi vesicle to form the mature virion. Finally, the virion-containing vesicle fuses with the membrane of the host cell to release the virus.
The route of the SARS-CoV entry into humans is through the respiratory tract mainly by droplet transmission. The surface envelops spike protein (S protein) of SARS-CoV-2 plays an important role in establishing infection and determining the cell and tissue tropism31. The initial attachment of the virion to the host cell is initiated by interactions between the S protein and its receptor32. Entry of the virus requires receptor binding, followed by conformational change of the S protein, and then cathepsin L-mediated proteolysis within the endosome. The angiotensin-converting enzyme 2 (ACE2), found in the lower respiratory tract of humans, is known as cell host receptor for SARS-CoV, and is expressed in a wide variety of body tissues and regulates both cross-species and human-to-human transmission33. Through analyzing the bronchoalveolar lavage fluid (BALF) from a COVID-19 patient, Zhou et al.34 and Walls et al.35 have confirmed that SARS-CoV-2 uses the same cellular entry receptor, ACE2, as does the SARS-CoV. The virion S glycoprotein on the surface of the coronavirus can attach to the ACE2 receptor on the surface of human cells34.
Following receptor binding, the virus must next gain access to the host cell cytosol, and this is generally accomplished by acid-dependent proteolytic cleavage of S protein by a cathepsin or another protease, followed by fusion of the viral and cellular membranes. S glycoprotein includes two subunits, S1 and S232. S1 determines the virus-host range and cellular tropism with the key function domain (RBD), while S2 mediates virus-cell membrane fusion by two tandem domains, heptad repeats 1 (HR1) and HR236. The next step in the coronavirus lifecycle is the translation of the replicase gene from the virion genomic RNA. After membrane fusion, the viral genome RNA is released into the cytoplasm, and the uncoated RNA translates two polyproteins, pp1a and pp1ab32, which encode non-structural proteins, and form a replication–transcription complex (RTC) in the double-membrane vesicle37. Viral RNA synthesis follows the translation and assembly of the viral replicase complexes. RTC replicates and synthesizes a nested set of subgenomic RNAs, which encode accessory proteins and structural proteins. The latter is translated into structural proteins and accessory proteins. The membrane-bound structural proteins, membrane (M), S, and envelope (E) are inserted into the endoplasmic reticulum (ER), from there they transit to the endoplasmic reticulum–Golgi intermediate compartment (ERGIC). Nucleocapsids are formed from the encapsidation of progeny genomes by N protein, and these coalesce with the membrane-bound components, forming virions by budding into the ERGIC11,38. Lastly, the virion-containing vesicles fuse with the plasma membrane to release the virus.
3. Antiviral properties of natural products against coronavirus
Extensive studies have been conducted over the past years to identify anti-CoV agents from natural products and Chinese herbal medicine39. In this section, we discuss the medicinal plant-based natural compounds and traditional Chinese medicine (TCM) formulae with antiviral action against coronaviruses and their potential for use in clinical practice.
3.1. Natural products against CoVs
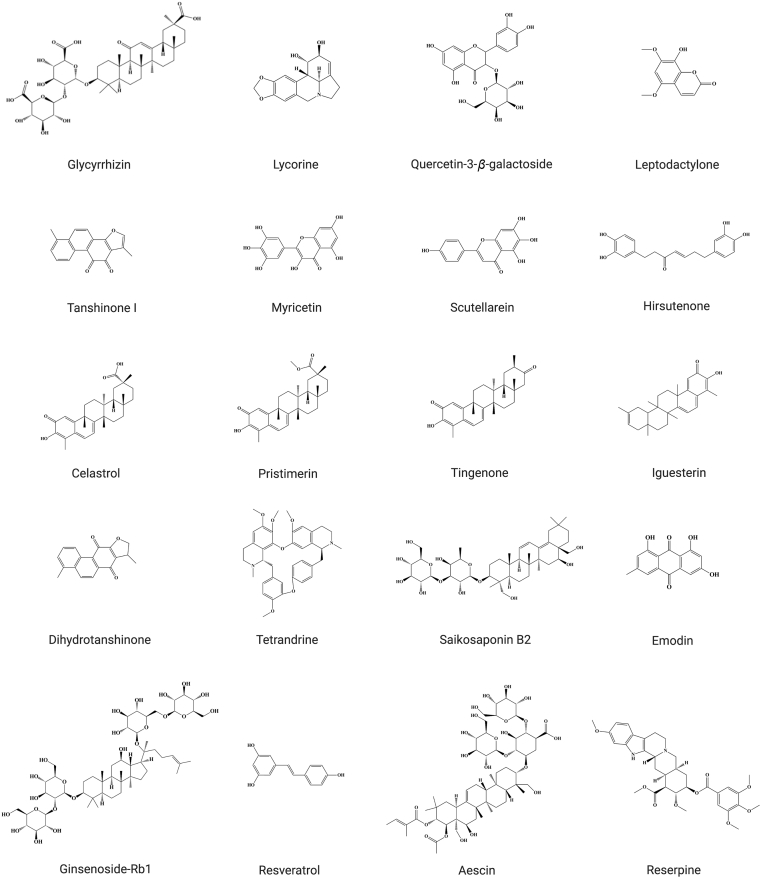
Various natural products have shown potent antiviral effects against SARS-CoV40, 41, 42, 43, MERS-CoV44, HCoV-229 E45 and HCoV-OC4346. Aescin isolated from Aesculus hippocastanum and reserpine isolated from various Rauwolfia species40, were both shown to have significant anti-SARS activities with the concentration for 50% of maximal effect (EC50) values of 3.4 and 6.0 μmol/L, respectively41. Ginsenoside-Rb1, one of the pharmacologically active components of Panax ginseng47, was reported to possess activity against SARS-CoV at the concentration of 100 μmol/L41. Boenninghausenia sessilicarpa (Rutaceae), a slender and perennial plant, has long been known as a coumarin-rich Chinese herbal medicine distributed in the temperate hilly regions at an altitude of 1500–2500 m in southwestern China. It is traditionally used for the treatment of fever, festers and tonsillitis. Leptodactylone, extracted from B. sessilicarpa, was found to have a strong protective effect against virus-infected cells and anti-SARS-CoV activity with the inhibition rate of 60% at 100 mg/mL42. It has also been shown that lycorine extracted from Lycoris radiata was identified to have anti-SARS-CoV activity with EC50 value of 15.7 ± 1.2 nmol/L43. Latest study of repurposing of clinically approved drugs for treatment of COVID-19 showed that cepharanthine, a bisbenzylisoquinoline alkaloid from tubers of Stephania japonica (Qianjinteng), exhibited a potent inhibition of a 2019-nCoV-related pangolin coronavirus GX_P2V infection, with EC50 value of 0.98 μmol/L using a 2019-novel coronavirus-related coronavirus model48. Dihydrotanshinone is a major lipophilic compound isolated from Salviae Miltiorrhizae Radix et Rhizoma, which is commonly used in TCM. A recent study showed that dihydrotanshinone exerted inhibitory effects against viral entry in the MERS-CoV with the IC50 value of 1 μg/mL44. Saikosaponin B2, isolated from Bupleuri Radix, exerted potent antiviral activity against HCoV-22E9, with the IC50 value of 1.7 ± 0.1 μmol/L45. The antiviral action mechanism of saikosaponin B2 may be mediated, at least in part, by inhibiting viral attachment to cells, blocking viral penetration into cells, and interfering with the early stage of viral replication, such as virus absorption and penetration. Tetrandrine, isolated from Stephaniae Tetrandrae Radix, has been found to dramatically suppress the replication of HCoV-OC43, with the IC50 value of 0.33 ± 0.03 μmol/L46. All these natural compounds possess antiviral effects against the coronavirus, and their action mechanisms were summarized in Table 129,30,41, 42, 43, 44, 45, 46,48, 49, 50, 51, 52, 53, 54, 55, 56, 57, while their chemical structures shown in Fig. 2. This article also reported the IC50 values of the natural products against the HCoVs including SARS and MERS. As shown in Table 1, the IC50 values of these compounds mostly ranged from micro to milligrams per milliliter, or from nano to micromoles per liter. These natural compounds have been reported to act on various viral targets such as spike (S) glycoprotein, coronavirus main proteinase-chymotrypsin-like protease (3CLpro), the papain-like protease (PLpro), RNA-dependent RNA polymerase (RdRp), and nucleocapsid (N) proteins. These pharmacological targets are further discussed in the section below.
Table 1.
Summary of the anti-CoVs effects of natural compounds and their possible action mechanisms.
| Plant | Compound | Virus acting on | IC50 value | Reported antiviral mechanism | Ref. |
|---|---|---|---|---|---|
| Licorice root | Glycyrrhizin | SARS-CoV | 300 mg/L | Upregulates nitrous oxide synthase and nitrous oxide production | 29,49 |
| Polygonum cuspidatum | Resveratrol | MERS-CoV | – | – | 30 |
| Panax ginseng | Ginsenoside-Rb1 | SARS-CoV | 100 μmol/L | Inhibits glycoprotein activity | 41 |
| Rauvolfia serpentina | Reserpine | SARS-CoV | 6.0 μmol/L | – | 41 |
| Aesculus hippocastanum | Aescin | SARS-CoV | 3.4 μmol/L | – | 41 |
| Boenninghausenia sessilicarpa | Leptodactylone | SARS-CoV | 100 μg/mL | – | 42 |
| Lycoris radiata | Lycorine | SARS-CoV | 15.7 ± 1.2 nmol/L | – | 43 |
| Salvia miltiorrhiza | Dihydrotanshinone | MERS-CoV | 1 μg/mL | – | 44 |
| Bupleurum chinense | Saikosaponin B2 | HCoV-229E | 1.7 ± 0.1 μmol/L | Interferes with events of early viral entry | 43,45 |
| Stephania tetrandra | Tetrandrine | HCoV-OC43 | 0.33 ± 0.03 μmol/L | Inhibits p38 MAPK pathway | 46 |
| Stephania japonica | Cepharanthine | SARS-CoV-2 | 0.98 μmol/L | ACE inhibitor | 48 |
| Rheum palmatum | Emodin | SARS-CoV | 200 μmol/L | Blocks the binding of S protein to ACE2 | 50 |
| Triterygium regelii | Celastrol | SARS-CoV | 10.3 μmol/L | Inhibits SARS-CoV 3CLpro | 51 |
| Triterygium regelii | Pristimererin | SARS-CoV | 5.5 μmol/L | Inhibits SARS-CoV 3CLpro | 51 |
| Triterygium regelii | Tingenone | SARS-CoV | 9.9 μmol/L | Inhibits SARS-CoV 3CLpro | 51 |
| Triterygium regelii | Iguesterin | SARS-CoV | 2.6 μmol/L | Inhibits SARS-CoV 3CLpro | 51 |
| Ginkgo biloba | Quercetin-3-β-galactoside | SARS-CoV | 42.79 ± 4.97 μmol/L | Competitively inhibits SARS-CoV 3CLpro | 52 |
| Salvia miltiorrhiz | Tanshinones I–VII | SARS–CoV | 0.7–30 μmol/L | Inhibits PLpro activity | 53 |
| Alnus japonica | Hirsutenone | SARS-CoV | 4.1 μmol/L | Inhibits PLpro activity | 53,54 |
| Black tea | Theaflavin | SARS-CoV-2 | – | Inhibits RdRp activity | 55 |
| Myrica rubra | Myricetin | SARS-CoV | 2.71 ± 0.19 μmol/L | Inhibits ATPase activity | 56 |
| Scutellaria baicalensis | Scutellarein | SARS-CoV | 0.86 ± 0.48 μmol/L | Inhibits ATPase activity | 56 |
| Angelica keiskei | Chalcones I–IX | SARS–CoV | 11.4–129.8 μmol/L | Competitively inhibits SARS-CoV 3CLpro | 57 |
–IC50 value or the mechanism of antiviral activity of these active compounds is not clear.
Figure 2.
Chemical structures of the natural compounds with antiviral activities.
3.2. Chinese herbal formulae against CoVs
TCM has been used for the treatment of epidemic diseases for a long history and accumulated rich experience. Thus, the antiviral activities are not limited to natural compounds, and also extended to TCM formulae. For example, Lian-Hua-Qing-Wen Capsule (LHQWC, Clearing Pestilential Disease with Forsythiae Fructus-Lonicerae Capsule), a commonly used Chinese medicine preparation, is widely used in clinical practice to treat viral influenza, and plays a very important role in the fight against SARS-CoV58, 59, 60 in particular. LHQWC has been reported to exert inhibitory effects on the SARS-CoVs in cultured Vero-E6 cells, with the EC50 value of 0.11 mg/mL61. LHQWC ameliorated the clinical symptoms such as fever, cough, fatigue and shortness of breath in 63 patients with COVID-1962. A recent study by Academician Nanshan Zhong revealed that LHQWC significantly inhibited the SARS-CoV-2 replication with the IC50 value of 411.2 μg/mL, affected virus morphology, and exerted anti-inflammatory activity in vitro63. They also conducted a prospective multicenter open-label randomized controlled trial on the effectiveness of LHQWC in 284 confirmed cases of COVID-19 (142 each in treatment and control group). The results showed that COVID-19 patients treated with LHQWC for 14 days resulted in a significantly higher recovery rate (91.5% vs. 82.4%, P = 0.022), a markedly shorter median time to symptom recovery (7 vs. 10 days, P < 0.001), as well as a dramatically shorter time to recovery of fever (2 vs. 3 days), fatigue (3 vs. 6 days) and coughing (7 vs. 10 days) (P < 0.001 for all) than the control group (baseline treatment). The results of this trial amply attested the safety and efficacy of LHQWC in patients with COVID-1964. In a retrospective clinical analysis, it was revealed that LHQWC could significantly ameliorate the major symptoms associated with the novel coronavirus-infected pneumonia (NCIP) patients by shortening the duration of fever and cough, and improving the recovery rate65. Moreover, the functional indications of LHQWC have been added to the originally approved indications for COVID-19 treatment. LHQWC can be used to treat clinical symptoms such as fever, cough, and fatigue for the light and common types of COVID-19 patients66.
As revealed by network pharmacology approach, Ren-Shen-Bai-Du-San (Ginseng to Defeat Toxicity Powder) may inhibit the cytokine storm formation in COVID-19 patients through regulating chemokines, increasing blood oxygen saturation, inhibiting signal transducer and activator of transcription (STAT), mitogen-activated protein kinase (MAPK), nuclear factor-κB (NF-κB), phosphoinositide 3-kinases (PIK3K) and interleukin-6 (IL-6) signaling pathways67. Another TCM formula, Qing-Fei-Jie-Du Decoction (Decoction for Clearing the Lung and Detoxification) was used for the prevention and treatment of SARS68 and also recommended for COVID-19 treatment according to the 7th edition of the Guidelines of Diagnosis and Treatment for COVID-1969 issued by the National Health Commission of China. Based on this latest edition of the Guidelines, several TCM formulae were recommended for the prevention and treatment of patients with COVID-19, including Jin-Hua-Qing-Gan Granule70,71 (Lonicerae Flos for Clearing Influenza Granule), Huo-Xiang-Zheng-Qi Water (Agastaches Herba Qi-Correcting Water), Shu-Feng-Jie-Du Capsule72, 73, 74 (Wind-Expelling and Detoxification Capsule), Xue-Bi-Jing Injection75 (Blood Definitely Be Cleansed Injection Fluid) and other herbal formulae (as shown in Table 258, 59, 60,62,67, 68, 69, 70, 71, 72, 73, 74, 75, 76, 77, 78, 79, 80, 81). Among the components of these formulae, Rhei Radix et Rhizoma, Scutellariae Radix, Glycyrrhizae Radix et Rhizoma, Bupleuri Radix, Lonicerae Japonicae Flos, Isatidis Radix and Houttuyniae Herba have been found to exert antimicrobial activities.
Table 2.
Chinese herbal formulae used for the treatment of SARS-CoV and COVID-19.
| Type of virus | TCM formulae | Constituent | Ref. |
|---|---|---|---|
| SARS-CoV COVID-19 | Lian-Hua-Qing-Wen Capsule | Forsythiae Fructus, Lonicerae Japonicae Flos, Ephedrae Herba, Armeniacae Semen Amarum, Isatidis Radix, Dryopteridis Crassirhizomatis Rhizoma, Houttuyniae Herba, Pogostemonis Herba, Rhei Radix et Rhizoma, Rhodiolae Crenulatae Radix et Rhizoma, Glycyrrhizae Radix et Rhizoma and Gypsum Fibrosum | 58, 59, 60,62 |
| COVID-19 | Ren-Shen-Bai-Du-San | Bupleuri Radix, Peucedani Radix, Notopterygii Rhizoma et Radix, Platycodonis Radix, Glycyrrhizae Radix et Rhizoma, Ginseng Radix et Rhizoma, Poria, Chuanxiong Rhizoma, Aurantii Fructus, Angelicae Pubescentis Radix | 67 |
| SARS-CoV | Qing-Fei-Jie-Du Decoction | Astragali Radix, Bupleuri Radix, Ephedrae Herba, Armeniacae Semen Amarum, Gypsum Fibrosum, Coicis Semen, Trichosanthis Pericarpium, Platycodonis Radix, Menthae Haplocalycis Herba, Scutellariae Radix, Glycyrrhizae Radix et Rhizoma, Lonicerae Japonicae Flos, and Artemisiae Annuae Herba | 68 |
| SARS-CoV COVID-19 | Jin-Hua-Qing-Gan Granule | Lonicerae Japonicae Flos, Gypsum Fibrosum, Ephedrae Herba, Armeniacae Semen Amarum, Scutellariae Radix, Forsythiae Fructus, Fritillariae Thunbergii Bulbus, Anemarrhenae Rhizoma, Arctii Fructus, Artemisiae Annuae Herba, Menthae Haplocalycis Herba, Glycyrrhizae Radix et Rhizoma | 69, 70, 71 |
| SARS-CoV COVID-19 | Shu-Feng-Jie-Du Capsule | Patriniae Herba, Isatidis Radix, Bupleuri Radix, Glycyrrhizae Radix et Rhizoma, Polygoni Cuspidati Rhizoma et Radix, Forsythiae Fructus, Phragmitis Rhizoma, Verbenae Herba | 72, 73, 74 |
| COVID-19 | Xue-Bi-Jing Injection | Carthami Flos, Paeoniae Radix Rubra, Chuanxiong Rhizoma, Salviae Miltiorrhizae Radix et Rhizoma, Angelicae Sinensis Radix | 75 |
| SARS-CoV | Ma-Xing-Shi-Gan Decoction | Ephedrae Herba, Armeniaca Semen Amarum, Gypsum Fibrosum, Glycyrrhizae Radix et Rhizoma | 76,77 |
| SARS-CoV | Shuang-Huang-Lian Granule | Lonicerae Japonicae Flos, Scutellariae Radix, Forsythiae Fructus | 78,79 |
| SARS-CoV | Yin-Qiao Powder | Forsythiae Fructus, Lonicerae Japonicae Flos, Platycodonis Radix, Menthae Haplocalycis Herba, Lophatheri Herba, Glycyrrhizae Radix et Rhizoma, Schizonepetae Spica, Sojae Semen Praeparatum, Arctii Fructus, Phragmitis Rhizoma | 80,81 |
4. The targets of natural products against CoVs
Natural products alone and TCM herbal formulae have antiviral activities against coronaviruses through acting on different molecular targets. We summarized the molecular targets of natural products against coronavirus, and these targets include S glycoprotein, coronavirus main 3CLpro, PLpro, RdRp, N proteins and other kinase such as viral helicase.
4.1. Targeting on S glycoprotein
The coronavirus spike (S) glycoprotein is the main antigen presented at the viral surface and is the target of neutralizing antibodies during infection, and a focus of vaccine design. S is a class I viral fusion protein synthesized as a single polypeptide chain precursor of approximately 1300 amino acids. For many coronaviruses, S is processed by host proteases to generate two subunits, designated S1 and S2, which remain non-covalently bound in the pre-fusion conformation82. The size of the abundantly N-glycosylated S protein varies greatly between CoV species ranging from approximately 1100 to 1600 residues in length, with an estimated molecular mass of up to 220 kDa. Trimers of the S protein form the 18−23-nm long, club-shaped spikes that decorate the membrane surface of the CoV particle. Besides being the primary determinant in CoV host tropism and pathogenesis, the S protein is also the main target for neutralizing antibodies elicited by the immune system of the infected host83. The CoV S protein is responsible for host cell attachment and mediates host cell membrane and viral membrane fusion during infection, the two key steps in the viral life cycle and major targets for antiviral drugs and vaccines35,84. Various antiviral natural compounds act on antiviral S glycoprotein. For instance, emodin, the major component of Rhei Radix et Rhizoma, has been demonstrated to possess antiviral effects against SARS-CoV via targeting S protein and blocking the binding of S protein to ACE2 in a dose-dependent manner50,85. Extracts of Eucalyptus globulus and Lonicera Japonica Flos, as well as ginsenoside-Rb1 have been reported to possess antiviral activity against SARS-CoV due to their ability to disrupt the envelope glycoprotein processing41,43. Saikosaponins isolated from Bupleuri Radix exerted antiviral activity against HCoV-22E9. More specifically, saikosaponin B2 possessed potent anti-CoV activity via affecting the viral penetration process including viral attachment and penetration through disturbing viral glycoproteins45. Bis-benzylisoquinoline alkaloids-tetrandrine from Stephaniae Tetrandrae Radix dramatically suppressed the replication of HCoV-OC4346 via targeting S protein.
4.2. Targeting on 3CLpro and PLpro
3CLpro and PLpro are two proteases that process the polypeptide translation product from the genomic RNA into the structural and nonstructural protein components, which are vital for the replication and packaging of a new generation of viruses. 3CLpro is an essential part of the polyprotein and is usually present as a monomer. However, upon substrate binding, dimer formation has been observed. Each monomer has two domains (I and II) along with a C-terminal domain. 3CLpro is an important drug target, as its protease activity is crucial for viral survival and replication86. PLpro enzyme has two distinct functions in viral pathogenesis. The first one is to process the viral polyprotein into individual proteins that are essential for viral replication. The second is to remove ubiquitin and ISG15 proteins from host cell proteins, which likely helps coronaviruses shun the host's innate immune response87. Both 3CLpro and PLpro are essential to the virus for replication and controlling the host cell, and are viable targets for antiviral agents88,89. The important functions of 3CLpro and PLpro in the life cycle of virus render them the key viable targets for the development of anti-SARS therapeutics. Numerous promising candidates have been reported to kill the virus via targeting 3CLpro and PLpro. For example, chalcones, flavanones and coumarins from Angelicae Sinensis Radix showed dose-dependent inhibitory effects against SARS-CoV by inhibiting the activity of 3CLpro. In addition, natural compounds such as hesperetin and sinigrin isolated from Isatidis Radix90, celastrol, pristimererin, tingenone and iguesterin isolated from Triterygium regelii51 and quercetin derivatives quercetin-3-β-galactoside52 have antiviral activities against SARS-CoV through targeting on SARS-CoV 3CLpro. Moreover, tanshinone I isolated from Salviae Miltiorrhizae Radxi et Rhizoma53 and hirsutenone isolated from Alnus japonica54 exhibited dose-dependent inhibitory effects against SARS-CoV through targeting PLpro, with the IC50 values of 0.7 and 4.1 μmol/L, respectively.
4.3. Targeting on RdRp
RdRp, also called RNA replicases, is an important protease that catalyzes the replication of RNA from RNA template and is an essential protein encoded in the genomes of all RNA-containing viruses with no DNA stage. An RdRp is involved in a pathway outside the “central dogma” of early molecular biology. RdRps, present in a wide variety of RNA viruses, are involved in genome replication, mRNA synthesis, and RNA recombination. They are essential for the survival of viruses91. RdRp has served as an excellent antiviral target against coronaviruses, and many promising naturally-occurring chemical principles exhibit their antiviral properties via targeting RdRp. For instance, theaflavin markedly suppressed SARS-CoV-2 replication through inhibiting RdRp55. Houttuyniae Herba also exhibited significant inhibitory effects against SARS-CoV via suppressing the activities of SARS-CoV 3CLpro and RdRp92.
4.4. Targeting on N proteins
The N protein is the only structural protein that is associated with RTCs. It binds to the gRNA, and is essential for the incorporation of the virus genetic material into CoV particles. Moreover, it is the major component of ribonucleoprotein complex sitting in the virion cores, and thus also plays an essential architectural role in the virus particle structural organization through a network of interactions with the gRNA, M protein and other N molecules. For CoVs, N protein primarily encapsidates the viral genome but also plays an important role in viral replication, virus particle assembly and release93,94. Due to its pivotal role in the incorporation of the virus genetic material into CoV particles, it has been recognized as an important target for various antiviral compounds. Resveratrol, a well-known natural compound widely presented in different plants, including Vitis vinifera, Polygonum cuspidatum and Vaccinium macrocarpon, has been demonstrated to decrease the production of nitric oxide in tissue to reduce inflammation95,96. It also acts as an antioxidant to remove free radicals to suppress tumor growth97 and treat age-related diseases98,99. Moreover, resveratrol has been shown to have antiviral activity on MERS-CoV via targeting N protein and prolong cellular survival after viral infection30.
4.5. Other targets
Besides targeting S protein, 3CLpro, PLpro, RdRp, and N proteins, natural products can also target on other proteins to exert their anti-CoV activities. Glycyrrhizin, an active ingredient of Glycyrrhizae Radix et Rhizoma, has been observed to exert anti-SARS-CoV activity through targeting protein kinase C, which upregulates the nitrous synthase and production29,49. Viral helicase is essential for subsequent viral replication and proliferation, and is considered as a potential target for antiviral therapy100. Natural compounds such as myricetin and scutellarein, potently inhibited the SARS-CoV helicase protein by affecting the ATPase activity56.
5. The potential of natural compounds for clinical treatment of COVID-19
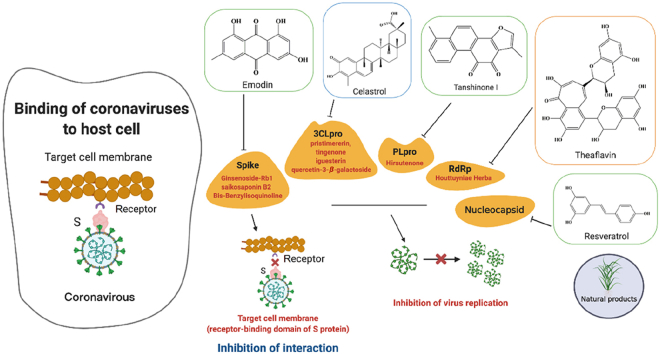
As shown in Fig. 3, CoV relies on its spike proteins to bind to the host cell surface receptor for entry. For SARS-CoV-2, it is now known that this receptor is ACE2101. After the virus entries into the host cell, its positive genomic RNA attaches directly to the host ribosome for the translation of two large, coterminal polyproteins that are processed by proteolysis into components for packaging new virions. Two proteases that participate in this proteolysis process are 3CLpro and PLpro. In order to replicate the RNA genome, the CoV encodes a replicase that is a RdRp. These four proteins are essential for the pathogenicity of virus. Therapeutics currently targeting spike, RdRp, 3CLpro, and PLpro are possible treatments for SARS-CoV-2102. Moreover, the initial analyses of genomic sequences from COVID-19 patients indicate that the catalytic sites of the four COVID-19 enzymes that could represent antiviral targets are highly conserved and share a high level of sequence similarity with the corresponding SARS and MERS enzymes. SARS-CoV-2 shares 82% similarity of sequence identity with SARS-CoV and more than 90% similarity of sequence identity in several essential enzymes103. Therefore, it is rational to consider repurposing existing MERS and SARS inhibitors for COVID-19 treatment102. As listed in Table 1, natural compounds such as theaflavin and cepharanthine suppressed SARS-CoV-2 by suppressing RdRp and ACE activities; hirsutenone and tanshinones I–VII showed antiviral action against SARS-CoV via inhibiting the PLpro activity, while celastrol, pristimererin, tingenone, iguesterin, chalcones I–IX and quercetin-3-β-galactoside were able to inhibit SARS-CoV by suppressing the 3CLpro activity. Owing to the close resemblance between SARS-CoV and SARS-CoV-2, all these natural compounds and their original plants with the antiviral activities against SARS-CoV and MERS-CoV may have potential protective effects against COVID-19.
Figure 3.
The possible action mechanisms of natural compounds against CoVs. Emodin, ginsenoside-Rb1, saikosaponin B2 and bis-benzylisoquinoline alkaloids-tetrandrine target the S protein to exert anti-SARS-CoV activity. Celastrol, pristimererin, tingenone and iguesterin act against SARS-CoV via inhibiting the 3CLpro activity. Tanshinone I and hirsutenone act against SARS-CoV via suppressing the PLpro activity. Theaflavin targets on the RdRp activity, while resveratrol acts on the N proteins against SARS-CoV and MERS-CoV, respectively.
6. Discussion and perspectives
CoVs are associated with a number of infectious disease outbreaks in humans in recent years, including SARS in 2002–2003 and MERS in 2012. Four other CoVs including human coronaviruses HKU1, OC43, NL63 and 229E are also associated with respiratory diseases104. The epidemic outbreak caused by SARS-CoV in 2002–2003 involved 8422 patients and affected 29 countries worldwide. The MERS-CoV outbreak in 2012 mainly affected the Middle Eastern countries. The sequence of SARS-CoV-2, which is responsible for COVID-19 outbreak, is different from the six other coronavirus subtypes, and can be classified as beta-coronavirus. The number of COVID-19 cases is growing rapidly and has affected more than 200 countries globally by early April 2020. It has become obvious that SARS-CoV-2 is more infectious than both SARS-CoV and MERS-CoV. It is now known that the SARS-CoV-2 can be transmitted by asymptomatic or presymptomatic COVID-19 patients105. Fever, cough and fatigue are the early signs and symptoms of COVID-19. Significant decrease in the lymphocyte counts and new pulmonary infiltrates on chest radiography were usually found in the COVID-19 patients. Moreover, 97% of COVID-19 cases confirmed by RT-PCR test eventually developed pneumonia as evidenced by CT scan106. However, the symptoms associated with COVID-19 did not improve after treatment with antibiotics for three days34.
Due to a lack of vaccine and efficacious antiviral agents, COVID-19 continues to cause havoc in many parts of the world. Only a small set of evidence-based non-pharmaceutical interventions are available for COVID-19107. There is clearly an unmet medical need for effective treatment of COVID-19. Increasing evidence suggested that a subgroup of severe COVID-19 patients might be caused by a cytokine storm syndrome108. Pulmonary involvement (including ARDS) occurs in approximately 50% of COVID-19 patients with hemophagocytic lymphohistiocytosis (HLH)109. A cytokine profile resembling secondary HLH is associated with the patients with severe COVID-19, characterized by an increase in TNF-α, IL-2, IL-7, interferon-γ inducible protein 10, granulocyte-colony stimulating factor, macrophage inflammatory protein 1-α and monocyte chemoattractant protein 1. A recent retrospective and multi-center study on 150 confirmed COVID-19 cases revealed the association between fatality and significantly elevated ferritin (mean 1297.6 ng/mL in non-survivors vs. 614.0 ng/mL in survivors, P < 0.001) and IL-6 (P < 0.0001), suggesting that the mortality of the patients with COVID-19 might be related to virus-induced hyperinflammation108.
Historically, TCM has developed medical theories and accumulated rich and valuable experiences in the prevention and treatment of lung diseases, especially pneumonia110. Natural products such as Chinese herbs possess various bioactivities and have been extensively used to treat diseases of virus origin such as common cold, influenza and SARS. Many studies have reported the anti-inflammatory activities of natural compounds, and inflammation has been considered as the basic pathogenesis underlying various medical conditions, including flu and COVID-19. Emodin, a flavonoid isolated from the Rhei Radix et Rhizoma, is able to block the SARS-CoV via interfering the interaction of S protein and ACE250. It also exhibited anti-inflammatory111,112, anti-proliferative and anti-carcinogenic properties113. Emodin dose-dependently ameliorated the asthmatic airway inflammation by inhibiting the activated macrophages polarization and STAT6 phosphorylation111. Scutellarein, another plant-derived flavonoid, exerted anti-inflammatory via suppressing the expression of cyclooxygenase-2 and inducible nitric oxide synthase through inhibition of NF-κB pathway114. Flavonoids of Lonicerae Japonicae Flos, glycyrrhizin, and resveratrol have also been reported to possess anti-inflammatory effects115, 116, 117. A high-profile research published in the Science reported that desaminotyrosine (DAT), a microbial metabolite, was able to protect the host from influenza through suppression of the type I interferon signaling and augmentation of lung immunopathology118. DAT could be produced by human enteric bacteria from flavonoids and amino acid metabolism. Moreover, DAT is also a degradation product of flavonoids that is rich in certain foods and some Chinese medicines. Flavonoids have been reported to exert good anti-inflammation effects102,103,105. Overwhelming inflammation and cytokine-related lung injury might induce rapid and progressive pneumonia in critically ill patients with influenza119. Therefore, the protective effect of DAT against influenza may be related to the anti-inflammatory effect of flavonoids.
Because of a lack of specific antiviral therapeutics and vaccines for COVID-19, both conventional medicine and TCM are usually used for the treatment of COVID-19 patients in China. Western medicine used to treat COVID-19 patients usually include the broad-spectrum antibiotics, antivirals, corticosteroids, or their combination. These conventional medicine could quickly manage the major symptoms of the patients, but may cause severe side effects, while TCM treatment modality has the advantage of low toxicity. It is well known that TCM could modulate immune cells and cytokine production associated with immune responses120. Proper immune regulation helps maintain the homeostasis of the immune system, protect the body from sources of infection or other harmful substances. A systematic review and meta-analysis revealed that integrated Chinese and Western medicine had better effects and fewer adverse drug reactions on COVID-19 patients as compared with western medicine alone121. Moreover, it has been reported that TCM treatment could attenuate side effects associated with conventional therapeutics for SARS-CoV patients122. Therefore, more investigations are warranted to establish the efficacy and safety of the integrated Chinese and Western medicine for human CoVs.
Since TCM has the characteristics of multi-component, multi-target and multi-pathway for treatment of diseases, it possesses great potential for the treatment of COVID-19. As shown in this review, many natural products or TCM formulae have demonstrated promising antiviral activities against CoVs through multiple target-approaches, and can be further developed into bioactive derivatives and therapeutic leads. However, although natural products have shown good potential for the treatment of COVID-19, it is still a long way for them to be eventually used in clinic. One of the main limitations of developing natural products into pharmaceuticals is their solubility and bioavailability123. The high costs and complexity of clinical trials add another barrier to the development of new antivirals from natural products124. Pharmaceutical companies are facing with multiple regulatory bottlenecks such as increased stringency of trial design, and enhanced safety requirements for drug licensing. Despite many difficulties in developing natural compounds into antiviral drugs, increasing efforts have been seen in many parts of the world for the development of antivirals from natural products in both preclinical and clinical studies. Searching new antiviral agents from natural products remains a challenging yet exciting task.
Our present review provides an important update on a number of natural products that have shown promise as anti-CoV agents and potential for COVID-19 treatment. However, since many studies about the antiviral effects of the natural compounds and Chinese medicine in this domain are only preliminary, in-depth in vivo studies on appropriate animal models are needed to unravel the underlying cellular and molecular mechanisms. Pharmacokinetic studies on the promising natural compounds are few and far between, and should be conducted to obtain pharmacokinetic profile, including absorption, distribution, metabolism and excretion parameters. Moreover, clinical trials (phase I to III) are required to test their anti-CoV efficacy and safety on human subjects. More importantly, investigations should be carried out to explore the potential interactions between TCM or natural products and available antivirals on anti-CoV effects. Optimization of some of the aforementioned lead compounds with known or new mechanisms of action may lead to eventual development of new therapeutics for COVID-19.
Author contributions
Zhixiu Lin and Hongxi Xu conceived and designed the review. Yanfang Xian and Juan Zhang retrieved the literature and drafted the manuscript. Zhaoxiang Bian and Hua Zhou participated in the design of study and assessed the quality of study. Zhenbiao Zhang drew the chemical structures of nature compounds. Zhixiu Lin and Hongxi Xu revised the review. All authors have consented for publication.
Conflicts of interest
The authors declare that they have no competing interests.
Footnotes
Peer review under responsibility of Chinese Pharmaceutical Association and Institute of Materia Medica, Chinese Academy of Medical Sciences.
Contributor Information
Zhixiu Lin, Email: linzx@cuhk.edu.hk.
Hongxi Xu, Email: xuhongxi88@gmail.com.
References
- 1.Lim Y.X., Ng Y.L., Tam J.P., Liu D.X. Human coronaviruses: a review of virus-host interactions. Diseases. 2016;4:26. doi: 10.3390/diseases4030026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Zumla A., Chan J.F., Azhar E.I., Hui D.S., Yuen K.Y. Coronaviruses-drug discovery and therapeutic options. Nat Rev Drug Discov. 2016;15:327–347. doi: 10.1038/nrd.2015.37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Li F. Structure, function, and evolution of coronavirus Spike proteins. Annu Rev Virol. 2016;3:237–261. doi: 10.1146/annurev-virology-110615-042301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Schoeman D., Fielding B.C. Coronavirus envelope protein: current knowledge. Virol J. 2019;16:69. doi: 10.1186/s12985-019-1182-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Song Z.Q., Xu Y.F., Bao L.L., Zhang L., Yu P., Qu Y.J. From SARS to MERS, thrusting coronaviruses into the spotlight. Viruses Basel. 2019;11:59. doi: 10.3390/v11010059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wu C., Liu Y., Yang Y., Zhang P., Zhong W., Wang Y. Analysis of therapeutic targets for SARS-CoV-2 and discovery of potential drugs by computational methods. Acta Pharm Sin B. 2020;10:766–788. doi: 10.1016/j.apsb.2020.02.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wang H., Wang Z., Dong Y., Chang R., Xu C., Yu X. Phase-adjusted estimation of the number of coronavirus disease 2019 cases in Wuhan, China. Cell Discov. 2020;6:10. doi: 10.1038/s41421-020-0148-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Coronaviridae study group of the international committee on taxonomy of V The species severe acute respiratory syndrome-related coronavirus: classifying 2019-nCoV and naming it SARS-CoV-2. Nat Microbiol. 2020;5:536–544. doi: 10.1038/s41564-020-0695-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Liu Y., Gayle A.A., Wilder-Smith A., Rocklov J. The reproductive number of COVID-19 is higher compared to SARS coronavirus. J Trav Med. 2020;27 doi: 10.1093/jtm/taaa021. taaa021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Huang C., Wang Y., Li X., Ren L., Zhao J., Hu Y. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395:497–506. doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Guo Y.R., Cao Q.D., Hong Z.S., Tan Y.Y., Chen S.D., Jin H.J. The origin, transmission and clinical therapies on coronavirus disease 2019 (COVID-19) outbreak—an update on the status. Mil Med Res. 2020;7:11. doi: 10.1186/s40779-020-00240-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kim Y., Liu H., Galasiti Kankanamalage A.C., Weerasekara S., Hua D.H., Groutas W.C. Reversal of the progression of fatal coronavirus infection in cats by a broad-spectrum coronavirus protease inhibitor. PLoS Pathog. 2016;12 doi: 10.1371/journal.ppat.1005531. e1005531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Gordon C.J., Tchesnokov E.P., Feng J.Y., Porter D.P., Gotte M. The antiviral compound remdesivir potently inhibits RNA-dependent RNA polymerase from middle east respiratory syndrome coronavirus. J Biol Chem. 2020;295:4773–4779. doi: 10.1074/jbc.AC120.013056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lin L.T., Hsu W.C., Lin C.C. Antiviral natural products and herbal medicines. J Tradit Complement Med. 2014;4:24–35. doi: 10.4103/2225-4110.124335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kurokawa M., Ochiai H., Nagasaka K., Neki M., Xu H.X., Kadota S. Antiviral traditional medicines against herpes-simplex virus (Hsv-1), poliovirus, and measles-virus in-vitro and their therapeutic efficacies for Hsv-1 infection in mice. Antivir Res. 1993;22:175–188. doi: 10.1016/0166-3542(93)90094-y. [DOI] [PubMed] [Google Scholar]
- 16.Calland N., Dubuisson J., Rouille Y., Seron K. Hepatitis C virus and natural compounds: a new antiviral approach?. Viruses. 2012;4:2197–2217. doi: 10.3390/v4102197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Du J., He Z.D., Jiang R.W., Ye W.C., Xu H.X., But P.P.H. Antiviral flavonoids from the root bark of Morus alba L. Phytochemistry. 2003;62:1235–1238. doi: 10.1016/s0031-9422(02)00753-7. [DOI] [PubMed] [Google Scholar]
- 18.Xu H.X., Lee S.H., Lee S.F., White R.L., Blay J. Isolation and characterization of an anti-HSV polysaccharide from Prunella vulgaris. Antivir Res. 1999;44:43–54. doi: 10.1016/s0166-3542(99)00053-4. [DOI] [PubMed] [Google Scholar]
- 19.Xu H.X., Kadota S., Wang H., Kurokawa M., Shiraki K., Matsumoto T. A new hydrolyzable tannin from geum-japonicum and its antiviral activity. Heterocycles. 1994;38:167–175. [Google Scholar]
- 20.Xu H.X., Kadota S., Kurokawa M., Shiraki K., Matsumoto T., Namba T. Isolation and structure of woodorien, a new glucoside having antiviral activity, from woodwardia orientalis. Chem Pharm Bull. 1993;41:1803–1806. doi: 10.1248/cpb.41.1803. [DOI] [PubMed] [Google Scholar]
- 21.Kannan S., Kolandaivel P. Antiviral potential of natural compounds against influenza virus hemagglutinin. Comput Biol Chem. 2017;71:207–218. doi: 10.1016/j.compbiolchem.2017.11.001. [DOI] [PubMed] [Google Scholar]
- 22.Luganini A., Terlizzi M.E., Catucci G., Gilardi G., Maffei M.E., Gribaudo G. The cranberry extract oximacro® exerts in vitro virucidal activity against influenza virus by interfering with hemagglutinin. Front Microbiol. 2018;9:1826. doi: 10.3389/fmicb.2018.01826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Xu H.X., Zeng F.Q., Wan M., Sim K.Y. Anti-HIV triterpene acids from Geum japonicum. J Nat Prod. 1996;59:643–645. doi: 10.1021/np960165e. [DOI] [PubMed] [Google Scholar]
- 24.Xu H.X., Ming D.S., Dong H., But P.P. A new anti-HIV triterpene from Geum japonicum. Chem Pharm Bull. 2000;48:1367–1369. doi: 10.1248/cpb.48.1367. [DOI] [PubMed] [Google Scholar]
- 25.Xu H.X., Wan M., Loh B.N., Kon O.L., Chow P.W., Sim K.Y. Screening of traditional medicines for their inhibitory activity against HIV-1 protease. Phytother Res. 1996;10:207–210. [Google Scholar]
- 26.Sahuc M.E., Sahli R., Riviere C., Pene V., Lavie M., Vandeputte A. Dehydrojuncusol, a natural phenanthrene compound extracted from Juncus maritimus, is a new inhibitor of hepatitis C virus RNA replication. J Virol. 2019;93:e02009–e02018. doi: 10.1128/JVI.02009-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Zhang Y.B., Luo D., Yang L., Cheng W., He L.J., Kuang G.K. Matrine-type alkaloids from the roots of sophora flavescens and their antiviral activities against the hepatitis B virus. J Nat Prod. 2018;81:2259–2265. doi: 10.1021/acs.jnatprod.8b00576. [DOI] [PubMed] [Google Scholar]
- 28.Li B., Li L., Peng Z.G., Liu D., Si L.L., Wang J. Harzianoic acids A and B, new natural scaffolds with inhibitory effects against hepatitis C virus. Bioorg Med Chem. 2019;27:560–567. doi: 10.1016/j.bmc.2018.12.038. [DOI] [PubMed] [Google Scholar]
- 29.Cinatl J., Morgenstern B., Bauer G., Chandra P., Rabenau H., Doerr H.W. Glycyrrhizin, an active component of liquorice roots, and replication of SARS-associated coronavirus. Lancet. 2003;361:2045–2046. doi: 10.1016/S0140-6736(03)13615-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Lin S.C., Ho C.T., Chuo W.H., Li S., Wang T.T., Lin C.C. Effective inhibition of MERS-CoV infection by resveratrol. BMC Infect Dis. 2017;17:144. doi: 10.1186/s12879-017-2253-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Hui D.S., Memish Z.A., Zumla A. Severe acute respiratory syndrome vs. the middle east respiratory syndrome. Curr Opin Pulm Med. 2014;20:233–241. doi: 10.1097/MCP.0000000000000046. [DOI] [PubMed] [Google Scholar]
- 32.Fehr A.R., Perlman S. Coronaviruses: an overview of their replication and pathogenesis. Methods Mol Biol. 2015;1282:1–23. doi: 10.1007/978-1-4939-2438-7_1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Wan Y., Shang J., Graham R., Baric R.S., Li F. Receptor recognition by the novel coronavirus from wuhan: an analysis based on decade-long structural studies of SARS coronavirus. J Virol. 2020;94 doi: 10.1128/JVI.00127-20. e00127-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Zhou P., Yang X.L., Wang X.G., Hu B., Zhang L., Zhang W. A pneumonia outbreak associated with a new coronavirus of probable bat origin. Nature. 2020;579:270–273. doi: 10.1038/s41586-020-2012-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Walls A.C., Park Y.J., Tortorici M.A., Wall A., McGuire A.T., Veesler D. Structure, function, and antigenicity of the SARS-CoV-2 Spike glycoprotein. Cell. 2020;181:281–292. doi: 10.1016/j.cell.2020.02.058. e6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Yu F., Du L., Ojcius D.M., Pan C., Jiang S. Measures for diagnosing and treating infections by a novel coronavirus responsible for a pneumonia outbreak originating in Wuhan, China. Microb Infect. 2020;22:74–79. doi: 10.1016/j.micinf.2020.01.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Sawicki S.G., Sawicki D.L. Coronavirus transcription: a perspective. Curr Top Microbiol Immunol. 2005;287:31–55. doi: 10.1007/3-540-26765-4_2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Masters P.S. The molecular biology of coronaviruses. Adv Virus Res. 2006;66:193–292. doi: 10.1016/S0065-3527(06)66005-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Li-Weber M. Targeting apoptosis pathways in cancer by Chinese medicine. Canc Lett. 2013;332:304–312. doi: 10.1016/j.canlet.2010.07.015. [DOI] [PubMed] [Google Scholar]
- 40.Chen F.E., Huang J. Reserpine: a challenge for total synthesis of natural products. Chem Rev. 2005;105:4671–4706. doi: 10.1021/cr050521a. [DOI] [PubMed] [Google Scholar]
- 41.Wu C.Y., Jan J.T., Ma S.H., Kuo C.J., Juan H.F., Cheng Y.S. Small molecules targeting severe acute respiratory syndrome human coronavirus. Proc Natl Acad Sci U S A. 2004;101:10012–10017. doi: 10.1073/pnas.0403596101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Yang Q.Y., Tian X.Y., Fang W.S. Bioactive coumarins from Boenninghausenia sessilicarpa. J Asian Nat Prod Res. 2007;9:59–65. doi: 10.1080/10286020500382397. [DOI] [PubMed] [Google Scholar]
- 43.Li S.Y., Chen C., Zhang H.Q., Guo H.Y., Wang H., Wang L. Identification of natural compounds with antiviral activities against SARS-associated coronavirus. Antivir Res. 2005;67:18–23. doi: 10.1016/j.antiviral.2005.02.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Kim J.Y., Kim Y.I., Park S.J., Kim I.K., Choi Y.K., Kim S.H. Safe, high-throughput screening of natural compounds of MERS-CoV entry inhibitors using a pseudovirus expressing MERS-CoV spike protein. Int J Antimicrob Agents. 2018;52:730–732. doi: 10.1016/j.ijantimicag.2018.05.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Cheng P.W., Ng L.T., Chiang L.C., Lin C.C. Antiviral effects of saikosaponins on human coronavirus 229E in vitro. Clin Exp Pharmacol Physiol. 2006;33:612–616. doi: 10.1111/j.1440-1681.2006.04415.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Kim D.E., Min J.S., Jang M.S., Lee J.Y., Shin Y.S., Song J.H. Natural bis-benzylisoquinoline alkaloids-tetrandrine, fangchinoline, and cepharanthine, inhibit human coronavirus OC43 infection of MRC-5 human lung cells. Biomolecules. 2019;9:696. doi: 10.3390/biom9110696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Jeong C.S., Hyun J.E., Kim Y.S. Ginsenoside Rb1: the anti-ulcer constituent from the head of Panax ginseng. Arch Pharm Res (Seoul) 2003;26:906–911. doi: 10.1007/BF02980198. [DOI] [PubMed] [Google Scholar]
- 48.Fan H.H., Wang L.Q., Liu W.L., An X.P., Liu Z.D., He X.Q. Repurposing of clinically approved drugs for treatment of coronavirus disease 2019 in a 2019-novel coronavirus-related coronavirus model. Chin Med J (Engl) 2020;133:1051–1056. doi: 10.1097/CM9.0000000000000797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Hoever G., Baltina L., Michaelis M., Kondratenko R., Baltina L., Tolstikov G.A. Antiviral activity of glycyrrhizic acid derivatives against SARS-coronavirus. J Med Chem. 2005;48:1256–1259. doi: 10.1021/jm0493008. [DOI] [PubMed] [Google Scholar]
- 50.Ho T.Y., Wu S.L., Chen J.C., Li C.C., Hsiang C.Y. Emodin blocks the SARS coronavirus spike protein and angiotensin-converting enzyme 2 interaction. Antivir Res. 2007;74:92–101. doi: 10.1016/j.antiviral.2006.04.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Ryu Y.B., Park S.J., Kim Y.M., Lee J.Y., Seo W.D., Chang J.S. SARS-CoV 3CLpro inhibitory effects of quinone-methide triterpenes from Tripterygium regelii. Bioorg Med Chem Lett. 2010;20:1873–1876. doi: 10.1016/j.bmcl.2010.01.152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Chen L., Li J., Luo C., Liu H., Xu W., Chen G. Binding interaction of quercetin-3-beta-galactoside and its synthetic derivatives with SARS-CoV 3CL(pro): structure−activity relationship studies reveal salient pharmacophore features. Bioorg Med Chem. 2006;14:8295–8306. doi: 10.1016/j.bmc.2006.09.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Park J.Y., Kim J.H., Kim Y.M., Jeong H.J., Kim D.W., Park K.H. Tanshinones as selective and slow-binding inhibitors for SARS-CoV cysteine proteases. Bioorg Med Chem. 2012;20:5928–5935. doi: 10.1016/j.bmc.2012.07.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Park J.Y., Jeong H.J., Kim J.H., Kim Y.M., Park S.J., Kim D. Diarylheptanoids from Alnus japonica inhibit papain-like protease of severe acute respiratory syndrome coronavirus. Biol Pharm Bull. 2012;35:2036–2042. doi: 10.1248/bpb.b12-00623. [DOI] [PubMed] [Google Scholar]
- 55.Lung J., Lin Y.S., Yang Y.H., Chou Y.L., Shu L.H., Cheng Y.C. The potential chemical structure of anti-SARS-CoV-2 RNA-dependent RNA polymerase. J Med Virol. 2020;92:693–697. doi: 10.1002/jmv.25761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Yu M.S., Lee J., Lee J.M., Kim Y., Chin Y.W., Jee J.G. Identification of myricetin and scutellarein as novel chemical inhibitors of the SARS coronavirus helicase, nsP13. Bioorg Med Chem Lett. 2012;22:4049–4054. doi: 10.1016/j.bmcl.2012.04.081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Park J.Y., Ko J.A., Kim D.W., Kim Y.M., Kwon H.J., Jeong H.J. Chalcones isolated from Angelica keiskei inhibit cysteine proteases of SARS-CoV. J Enzym Inhib Med Chem. 2016;31:23–30. doi: 10.3109/14756366.2014.1003215. [DOI] [PubMed] [Google Scholar]
- 58.Ding Y., Zeng L., Li R., Chen Q., Zhou B., Chen Q. The Chinese prescription lianhuaqingwen capsule exerts anti-influenza activity through the inhibition of viral propagation and impacts immune function. BMC Compl Alternative Med. 2017;17:130. doi: 10.1186/s12906-017-1585-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Dong L., Xia J.W., Gong Y., Chen Z., Yang H.H., Zhang J. Effect of lianhuaqingwen capsules on airway inflammation in patients with acute exacerbation of chronic obstructive pulmonary disease. Evid Based Complement Alternat Med. 2014;2014:637969. doi: 10.1155/2014/637969. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Jia W., Wang C., Wang Y., Pan G., Jiang M., Li Z. Qualitative and quantitative analysis of the major constituents in Chinese medical preparation Lianhua-Qingwen capsule by UPLC-DAD–QTOF-MS. Sci World J. 2015;2015:731765. doi: 10.1155/2015/731765. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Zhu S.Y., Li X.Y., Wei Y.L., Yang P.Y., Qing E.D. Inhibitory effects of three precriptions of traditional Chinese medicine on SARS-associated coronavirus in vitro. Lett in biotecnol. 2003;14:390–392. [Google Scholar]
- 62.Lv R.B., Wang W.J., Li X. COVID-19 suspected cases treated with Lianhua Qingwen decoction: a clinical observation of 63 cases. J Chin Med. 2020;2:1–5. [Google Scholar]
- 63.Li R.F., Hou Y.L., Huang J.C., Pan W.Q., Ma Q.H., Shi Y.X. Lianhuaqingwen exerts anti-viral and anti-inflammatory activity against novel coronavirus (SARS-CoV-2) Pharmacol Res. 2020;156:104761. doi: 10.1016/j.phrs.2020.104761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Hu K., Guan W.J., Bi Y., Zhang W., Li L., Zhang B. Efficacy and safety of Lianhuaqingwen capsules, a repurposed Chinese herb, in patients with Coronavirus disease 2019: a multicenter, prospective, randomized controlled trial. Phytomedicine. 2020 doi: 10.1016/j.phymed.2020.153242. Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Yao K.T., Liu M.Y., Li X., Huang J.H., Cai H.B. Retrospective clinical analysis on treatment of novel coronavirus-infected pneumonia with traditional Chinese medicine Lianhua Qingwen. Chin J Exp Tradit Med Form. 2020:1–7. [Google Scholar]
- 66.2020. National medical products administration of the people's Republic of China.http://www.satcm.gov.cn/hudongjiaoliu/guanfangweixin/2020-04-15/14662.html Available from: [Google Scholar]
- 67.Li J.J., Zhang K., Wang S.S., Jing W.L., Bao J.M., Yang J.Y. The network pharmacology for treatment of COVID-19 with Renshenbaidusan based on cytokines. Chin Tradit Herb Drugs. 2020;51:1375–1385. [Google Scholar]
- 68.Chen F., Chan K.H., Jiang Y., Kao R.Y., Lu H.T., Fan K.W. In vitro susceptibility of 10 clinical isolates of SARS coronavirus to selected antiviral compounds. J Clin Virol. 2004;31:69–75. doi: 10.1016/j.jcv.2004.03.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.National Health Commission of the People's Republic of China . 7 ed. 2020. Notice on the issunance of guidelines of diagnosis and treatment for 2019-nCoV infected pneumonia (version 7)http://www.nhc.gov.cn/yzygj/s7653p/202003/46c9294a7dfe4cef80dc7f5912eb1989.shtml Available from: [Google Scholar]
- 70.Li G.Q., Zhao J., Tu Z.T., Li J.B., Liu Q.Q., Shi L.Q. Treating influenza patients of wind-heat affecting Fei syndrome by jinhua qinggan granule: a double-blinded randomized control trial. Chin J Integr Med. 2013;33:1631–1635. [PubMed] [Google Scholar]
- 71.Tao Z.G., Yang Y.X., Shi W.N., Xue M.M., Yang W.Q., Song Z.J. Complementary and alternative medicine is expected to make greater contribution in controlling the prevalence of influenza. Biosci Trends. 2013;7:253–256. [PubMed] [Google Scholar]
- 72.Tao Z., Gao J., Zhang G., Xue M., Yang W., Tong C. Shufeng Jiedu Capsule protect against acute lung injury by suppressing the MAPK/NF-kappaB pathway. Biosci Trends. 2014;8:45–51. doi: 10.5582/bst.8.45. [DOI] [PubMed] [Google Scholar]
- 73.Yuan Y., Liao Q., Xue M., Shi Y., Rong L., Song Z. Shufeng Jiedu capsules alleviate lipopolysaccharide-induced acute lung inflammatory injury via activation of GPR18 by verbenalin. Cell Physiol Biochem. 2018;50:629–639. doi: 10.1159/000494184. [DOI] [PubMed] [Google Scholar]
- 74.Song J., Zhang F., Tang S., Liu X., Gao Y., Lu P. A module analysis approach to investigate molecular mechanism of TCM formula: a trial on Shu-feng-jie-du formula. Evid Based Complement Alternat Med. 2013;2013:731370. doi: 10.1155/2013/731370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Wang P., Song Y., Liu Z., Wang H., Zheng W., Liu S. Xuebijing injection in the treatment of severe pneumonia: study protocol for a randomized controlled trial. Trials. 2016;17:142. doi: 10.1186/s13063-016-1282-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Fei Y.X., Zhao B., Yin Q.Y., Qiu Y.Y., Ren G.H., Wang B.W. Ma Xing Shi Gan decoction attenuates PM2.5 induced lung injury via inhibiting HMGB1/TLR4/NFkappaB signal pathway in rat. Front Pharmacol. 2019;10:1361. doi: 10.3389/fphar.2019.01361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Gao W., Li J.Y., Tang Y., Zhuang C.L., Li B., Wang S.G. Experiment study on Ma-Xing-Shi-Gan-Tang (MXSGT) and its decomposed recipes on anti-influenza virus A in vitro. Nature Preceding. 2008;3 doi: 10.1038/npre.2008.2260.1. [DOI] [Google Scholar]
- 78.Zhang H., Chen Q., Zhou W., Gao S., Lin H., Ye S. Chinese medicine injection shuanghuanglian for treatment of acute upper respiratory tract infection: a systematic review of randomized controlled trials. Evid Based Complement Alternat Med. 2013;2013:987326. doi: 10.1155/2013/987326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Tang Y., Wang Z., Huo C., Guo X., Yang G., Wang M. Antiviral effects of Shuanghuanglian injection powder against influenza A virus H5N1 in vitro and in vivo. Microb Pathog. 2018;121:318–324. doi: 10.1016/j.micpath.2018.06.004. [DOI] [PubMed] [Google Scholar]
- 80.Fu Y.J., Yan Y.Q., Qin H.Q., Wu S., Shi S.S., Zheng X. Effects of different principles of traditional Chinese medicine treatment on TLR7/NF-kappaB signaling pathway in influenza virus infected mice. Chin Med. 2018;13:42. doi: 10.1186/s13020-018-0199-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Liu L.S., Lei N., Lin Q., Wang W.L., Yan H.W., Duan X.H. The effects and mechanism of Yinqiao Powder on upper respiratory tract infection. Int J Biotechnol Wellness Ind. 2015;4:57–60. [Google Scholar]
- 82.Tortorici M.A., Walls A.C., Lang Y., Wang C., Li Z., Koerhuis D. Structural basis for human coronavirus attachment to sialic acid receptors. Nat Struct Mol Biol. 2019;26:481–489. doi: 10.1038/s41594-019-0233-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Hulswit R.J., de Haan C.A., Bosch B.J. Coronavirus spike protein and tropism changes. Adv Virus Res. 2016;96:29–57. doi: 10.1016/bs.aivir.2016.08.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Walls A.C., Tortorici M.A., Snijder J., Xiong X., Bosch B.J., Rey F.A. Tectonic conformational changes of a coronavirus spike glycoprotein promote membrane fusion. Proc Natl Acad Sci USA. 2017;114:11157–11162. doi: 10.1073/pnas.1708727114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Schwarz S., Wang K., Yu W.J., Sun B., Schwarz W. Emodin inhibits current through SARS-associated coronavirus 3a protein. Antivir Res. 2011;90:64–69. doi: 10.1016/j.antiviral.2011.02.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Durai P., Batool M., Shah M., Choi S. Middle East respiratory syndrome coronavirus: transmission, virology and therapeutic targeting to aid in outbreak control. Exp Mol Med. 2015;47:e181. doi: 10.1038/emm.2015.76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Ratia K., Kilianski A., Baez-Santos Y.M., Baker S.C., Mesecar A. Structural basis for the ubiquitin-linkage specificity and deISGylating activity of SARS-CoV papain-like protease. PLoS Pathog. 2014;10 doi: 10.1371/journal.ppat.1004113. e1004113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Sulea T., Lindner H.A., Purisima E.O., Menard R. Deubiquitination, a new function of the severe acute respiratory syndrome coronavirus papain-like protease?. J Virol. 2005;79:4550–4551. doi: 10.1128/JVI.79.7.4550-4551.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Baez-Santos Y.M., St John S.E., Mesecar A.D. The SARS-coronavirus papain-like protease: structure, function and inhibition by designed antiviral compounds. Antivir Res. 2015;115:21–38. doi: 10.1016/j.antiviral.2014.12.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Lin C.W., Tsai F.J., Tsai C.H., Lai C.C., Wan L., Ho T.Y. Anti-SARS coronavirus 3C-like protease effects of Isatis indigotica root and plant-derived phenolic compounds. Antivir Res. 2005;68:36–42. doi: 10.1016/j.antiviral.2005.07.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Ganeshpurkar A., Gutti G., Singh S.K. RNA-dependent RNA polymerases and their emerging roles in antiviral therapy. In: Gupta Satya., editor. Viral polymerases: structures, functions, and roles as antiviral drug targets. Academic Press; New York: 2019. pp. 1–42. [Google Scholar]
- 92.Lau K.M., Lee K.M., Koon C.M., Cheung C.S., Lau C.P., Ho H.M. Immunomodulatory and anti-SARS activities of Houttuynia cordata. J Ethnopharmacol. 2008;118:79–85. doi: 10.1016/j.jep.2008.03.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Cong Y., Kriegenburg F., de Haan C.A.M., Reggiori F. Coronavirus nucleocapsid proteins assemble constitutively in high molecular oligomers. Sci Rep. 2017;7:5740. doi: 10.1038/s41598-017-06062-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Aboagye J.O., Yew C.W., Ng O.W., Monteil V.M., Mirazimi A., Tan Y.J. Overexpression of the nucleocapsid protein of Middle East respiratory syndrome coronavirus up-regulates CXCL10. Biosci Rep. 2018;38 doi: 10.1042/BSR20181059. BSR20181059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Wang L.L., Shi D.L., Gu H.Y., Zheng M.Z., Hu J., Song X.H. Resveratrol attenuates inflammatory hyperalgesia by inhibiting glial activation in mice spinal cords. Mol Med Rep. 2016;13:4051–4057. doi: 10.3892/mmr.2016.5027. [DOI] [PubMed] [Google Scholar]
- 96.Kimbrough C.W., Lakshmanan J., Matheson P.J., Woeste M., Gentile A., Benns M.V. Resveratrol decreases nitric oxide production by hepatocytes during inflammation. Surgery. 2015;158:1095–1101. doi: 10.1016/j.surg.2015.07.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Zulueta A., Caretti A., Signorelli P., Ghidoni R. Resveratrol: a potential challenger against gastric cancer. World J Gastroenterol. 2015;21:10636–10643. doi: 10.3748/wjg.v21.i37.10636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Toth P., Tarantini S., Tucsek Z., Ashpole N.M., Sosnowska D., Gautam T. Resveratrol treatment rescues neurovascular coupling in aged mice: role of improved cerebromicrovascular endothelial function and downregulation of NADPH oxidase. Am J Physiol Heart Circ Physiol. 2014;306:H299–H308. doi: 10.1152/ajpheart.00744.2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Gliemann L., Nyberg M., Hellsten Y. Effects of exercise training and resveratrol on vascular health in aging. Free Radic Biol Med. 2016;98:165–176. doi: 10.1016/j.freeradbiomed.2016.03.037. [DOI] [PubMed] [Google Scholar]
- 100.Jang K.J., Jeong S., Kang D.Y., Sp N., Yang Y.M., Kim D.E. A high ATP concentration enhances the cooperative translocation of the SARS coronavirus helicase nsP13 in the unwinding of duplex RNA. Sci Rep. 2020;10:4481. doi: 10.1038/s41598-020-61432-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Dong N., Yang X., Ye L., Chen K., Chan E.W.-C., Yang M. Genomic and protein structure modelling analysis depicts the origin and pathogenicity of 2019-nCoV, a new coronavirus which caused a pneumonia outbreak in Wuhan, China. F1000Research. 2020;9 doi: 10.12688/f1000research.22357.2. Available from: [DOI] [Google Scholar]
- 102.Morse J.S., Lalonde T., Xu S., Liu W.R. Learning from the past: possible urgent prevention and treatment options for severe acute respiratory infections caused by 2019-nCoV. Chembiochem. 2020;21:730–738. doi: 10.1002/cbic.202000047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Li G., De Clercq E. Therapeutic options for the 2019 novel coronavirus (2019-nCoV) Nat Rev Drug Discov. 2020;19:149–150. doi: 10.1038/d41573-020-00016-0. [DOI] [PubMed] [Google Scholar]
- 104.Wu F., Zhao S., Yu B., Chen Y.M., Wang W., Song Z.G. A new coronavirus associated with human respiratory disease in China. Nature. 2020;579:265–269. doi: 10.1038/s41586-020-2008-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Zhang Y.Z., Holmes E.C. A genomic perspective on the origin and emergence of SARS-CoV-2. Cell. 2020;181:223–227. doi: 10.1016/j.cell.2020.03.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Hope M.D., Raptis C.A., Shah A., Hammer M.M., Henry T.S. A role for CT in COVID-19? What data really tell us so far. Lancet. 2020;395:1189–1190. doi: 10.1016/S0140-6736(20)30728-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Flahault A. COVID-19 cacophony: is there any orchestra conductor?. Lancet. 2020;395:1037. doi: 10.1016/S0140-6736(20)30491-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Mehta P., McAuley D.F., Brown M., Sanchez E., Tattersall R.S., Manson J.J. COVID-19: consider cytokine storm syndromes and immunosuppression. Lancet. 2020;395:1033–1034. doi: 10.1016/S0140-6736(20)30628-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Seguin A., Galicier L., Boutboul D., Lemiale V., Azoulay E. Pulmonary involvement in patients with hemophagocytic lymphohistiocytosis. Chest. 2016;149:1294–1301. doi: 10.1016/j.chest.2015.11.004. [DOI] [PubMed] [Google Scholar]
- 110.Wu T., Yang X., Zeng X., Poole P. Traditional Chinese medicine in the treatment of acute respiratory tract infections. Respir Med. 2008;102:1093–1098. doi: 10.1016/j.rmed.2008.03.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Song Y.D., Li X.Z., Wu Y.X., Shen Y., Liu F.F., Gao P.P. Emodin alleviates alternatively activated macrophage and asthmatic airway inflammation in a murine asthma model. Acta Pharmacol Sin. 2018;39:1317–1325. doi: 10.1038/aps.2017.147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Zhu T., Zhang W., Feng S.J., Yu H.P. Emodin suppresses LPS-induced inflammation in RAW264.7 cells through a PPAR gamma-dependent pathway. Int Immunopharm. 2016;34:16–24. doi: 10.1016/j.intimp.2016.02.014. [DOI] [PubMed] [Google Scholar]
- 113.Chen Y.C., Shen S.C., Lee W.R., Hsu F.L., Lin H.Y., Ko C.H. Emodin induces apoptosis in human promyeloleukemic HL-60 cells accompanied by activation of caspase 3 cascade but independent of reactive oxygen species production. Biochem Pharmacol. 2002;64:1713–1724. doi: 10.1016/s0006-2952(02)01386-2. [DOI] [PubMed] [Google Scholar]
- 114.Pandith H., Zhang X.B., Thongpraditchote S., Wongkrajang Y., Gritsanapan W., Baek S.J. Effect of Siam weed extract and its bioactive component scutellarein tetramethyl ether on anti-inflammatory activity through NF-kappa B pathway. J Ethnopharmacol. 2013;147:434–441. doi: 10.1016/j.jep.2013.03.033. [DOI] [PubMed] [Google Scholar]
- 115.Sun X., Zeng H., Wang Q., Yu Q., Wu J., Feng Y. Glycyrrhizin ameliorates inflammatory pain by inhibiting microglial activation-mediated inflammatory response via blockage of the HMGB1-TLR4-NF-κB pathway. Exp Cell Res. 2018;369:112–119. doi: 10.1016/j.yexcr.2018.05.012. [DOI] [PubMed] [Google Scholar]
- 116.Liu D., Yu X., Sun H., Zhang W., Liu G., Zhu L. Flos lonicerae flavonoids attenuate experimental ulcerative colitis in rats via suppression of NF-kappaB signaling pathway. Naunyn-Schmiedeberg’s Arch Pharmacol. 2020 doi: 10.1007/s00210-020-01814-4. https://link.springer.com/article/10.1007/s00210-020-01814-4 Available from: [DOI] [PubMed] [Google Scholar]
- 117.is Alharris E., Alghetaa H., Seth R., Chatterjee S., Singh N.P., Nagarkatti M. Resveratrol attenuates allergic asthma and associated inflammation in the lungs through regulation of miRNA-34a that targets FoxP3 in mice. Front Immunol. 2018;9:2992. doi: 10.3389/fimmu.2018.02992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Steed A.L., Christophi G.P., Kaiko G.E., Sun L.L., Goodwin V.M., Jain U. The microbial metabolite desaminotyrosine protects from influenza through type I interferon. Science. 2017;357:498–502. doi: 10.1126/science.aam5336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Shang L.H., Zhao J.P., Hu Y., Du R.H., Cao B. On the use of corticosteroids for 2019-nCoV pneumonia. Lancet. 2020;395:683–684. doi: 10.1016/S0140-6736(20)30361-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Huang C.F., Lin S.S., Liao P.H., Young S.C., Yang C.C. The immunopharmaceutical effects and mechanisms of herb medicine. Cell Mol Immunol. 2008;5:23–31. doi: 10.1038/cmi.2008.3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Liu M., Gao Y., Yuan Y., Yang K., Shi S., Zhang J. Efficacy and safety of integrated traditional Chinese and Western medicine for corona virus disease 2019 (COVID-19): a systematic review and meta-analysis. Pharmacol Res. 2020 doi: 10.1016/j.phrs.2020.104896. Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Zhang M.M., Liu X.M., He L. Effect of integrated traditional Chinese and Western medicine on SARS: a review of clinical evidence. World J Gastroenterol. 2004;10:3500–3505. doi: 10.3748/wjg.v10.i23.3500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Coimbra M., Isacchi B., van Bloois L., Torano J.S., Ket A., Wu X.J. Improving solubility and chemical stability of natural compounds for medicinal use by incorporation into liposomes. Int J Pharm (Amst) 2011;416:433–442. doi: 10.1016/j.ijpharm.2011.01.056. [DOI] [PubMed] [Google Scholar]
- 124.Gupta S.K., Nayak R.P. Dry antibiotic pipeline: regulatory bottlenecks and regulatory reforms. J Pharmacol Pharmacother. 2014;5:4–7. doi: 10.4103/0976-500X.124405. [DOI] [PMC free article] [PubMed] [Google Scholar]