Abstract
Vitiligo is the most common hypopigmentation disease affecting both the skin and mucous membranes. The pathogenesis of this disorder is complex and involves the influence of genetic and environmental factors, oxidative stress, and autoimmune responses. Recent studies have indicated that skin lesions observed in vitiligo tend to recur in the same places where they were found before treatment. This phenomenon is explained by the presence of recently discovered tissue-resident memory T cells (TRM), whose primary function is to provide antiviral and antibacterial protection in non-lymphoid tissues. TRM cells show the presence of CD49a, CD69, and CD103 markers on their surface, although not all of them express these particles. Due to their ability to produce and secrete perforin, IFN-γ, and granzyme B, TRM cells demonstrate a cytotoxic effect on melanocytes, thus inducing depigmented lesions in the course of the vitiligo. It has been proved that the occurrence of TRM cells largely depends on IL-15, which promotes the TRM function ex vivo. The findings above, as well as their reference to the pathogenesis of autoimmune skin diseases will have a considerable influence on the development of new therapeutic strategies in the near future. This article presents an up-to-date review of information regarding the role of TRM cells in the development and progression of vitiligo.
Keywords: vitiligo, tissue-resident memory T cells, IL-15, autoimmune diseases
1. Introduction
Vitiligo is a disease characterized by white patches of different shapes and sizes, which appear on the skin, overlying hair, and mucous membranes. Depigmentation is a result of the destruction of melanin-producing cells, called melanocytes, which embryologically origin from neutral crest and are located in the hair bulbs and basal layer of epidermis [1]. Interestingly, the word “vitiligo”, is derived from the Latin “vitium”, meaning “blemishing fault” [2]. The lesions often appear on elbows, knees, wrists, or the back of hands, i.e., in places most exposed to sunlight. They also show up around natural body orifices, such as the mouth, nose, eyes, and genitourinary organs [3,4]. Although vitiligo was described thousands of years ago (some records come from ancient Egypt and India), there is still a negative social stigma connected with this disease [5]. Consequently, pigmentary disfigurement might be a considerable cosmetic problem, seriously affecting the quality of patients’ lives by decreasing their sense of self-esteem and causing negative feelings, such as depression or anxiety [6]. Importantly, vitiligo is fully reversible when appropriate treatment is applied. Nevertheless, current therapies help to achieve only short-term benefits [5]. In the past, various methods were used, which were supposed to stop the disease. The repigmentation procedure was based on cow dung, cobra snake bones, or toxic substances, like arsenic [5]. Today, there are many options available, including topical corticosteroids and calcineurin inhibitors, PUVA light therapy, narrow-band UVB (nbUVB) phototherapy, or even surgery. It depends on the patient’s age, overall health, and preferences. However, the most successful treatment effects are based both on immunosuppression and simultaneous regeneration of melanocytes [5,7].
Apart from the skin, melanocytes also occur in the uveal layer of the eye, vaginal epithelium, and endolymphatic sac of the inner ear [1,8]. In spite of the fact that the disease does not usually influence melanocytes residing in these tissues, some studies indicate the connection between loss of hearing and vitiligo, regardless of the duration of the disease [1]. Besides the peripheral auditory system, melanocytes are also present in the central auditory system [1,9]. Even though the functions of otic melanocytes are not fully recognized, it seems that they play a protective role in the hearing process [10]. Hospital-based studies conducted by Mahdi et al. demonstrated that sensory neural hearing loss was present in approximately 40% of patients with diagnosed vitiligo [1]. This result suggests that the melanocytotoxic effect is not only a cutaneous problem. Because of this, some researchers recommend that vitiligo diagnosis should also include pure tone audiometry and ABR measurement, irrespective of any hearing problem. In addition, patients should avoid ototoxic drugs or any other noise exposure, particularly during disease activation [11]. MITF (microphthalmia-associated transcription factor) is a protein encoded by Mitf gene in humans, which induces melanin synthesis by regulating the expression of melanogenic enzymes, including tyrosinase-related protein-1 (TRP-1) and 2 (TRP-2). Mutations in this gene are detected in the diseases with pigmentation and deafness background, therefore it can be supposed that this factor, apart from the influence on the melanocytes, is also required in the hearing process [12,13].
The vitiligo prevalence ranges from 0.1% to 2% in most populations around the world, with no significant differences between the sexes [3]. The occurrence varies between geographic regions [14], but globally, vitiligo remains the most common hypopigmentation disorder [15]. The latest research, focusing on the ethiopathogenesis of this disease, shows that apart from genetic and environmental factors, the development of vitiligo is strongly related to autoimmune processes [16]. This theory is supported by a recent discovery of a new population of memory T cells, called TRM, which, by initiating the inflammatory process, are able to cause recurrent vitiligo lesions in the same places where an effective therapy has been applied before. There are still several concepts regarding the primary role of TRM cells in immune response. In some studies, skin TRM cells characterized by promoting local inflammation do not recruit other effector T cells from blood circulation. In another concept, the major function of TRM cells is the production and secretion of cytokines which are responsible for T cells recruitment [5]. The study conducted by Frisoli et al. demonstrated that selective depletion of recirculating memory T cells or inhibition of their migration contributed to rapid repigmentation, in spite of the fact that the number of TRM cells did not change [5]. This observation led to the conclusion that TRM cells are not fully responsible for relapsing skin lesions in vitiligo without additional recruiting of T cells [5]. This seems to be important information due to the fact that ~40% of patients suffer from a disease episode within the first year after finishing treatment [17]. By secreting compounds like granzyme B, perforin, or IFN-γ, TRM cells exert a cytotoxic effect on melanocytes, leading to their apoptosis. Importantly, CD8+ TRM cells which are present in healthy human skin do not demonstrate high expression of these effector molecules [5]. Apart from the skin, this long-living subset of T cells is also found in many other peripheral tissues including brain, liver, kidneys, spleen and heart. In the mucosa, TRM cells have been detected in the gut, female reproductive tract and lungs. They are also present in secondary lymphoid organs, which represent the first line of defense against infection factors [18,19].
2. Vitiligo Classification
In 2011, during the International Pigment Cell Conference (IPCC), two main forms of vitiligo were distinguished: segmental (SV) and non-segmental (NSV). It is noteworthy that the term “vitiligo” refers to all non-segmental forms, including the following subtypes: acrofacial, mucosal (more than one mucosal site), universal, generalized, mixed and other rare variants (Table 1) [20].
Table 1.
Vitiligo classification (adapted from Ezzedine et al. [20] based on Bordeaux VGICC * classification and consensus nomenclature).
| Type | Subtypes |
|---|---|
| Non-segmented vitiligo/vitiligo | Acrofacial Generalized Universal Mucosal (more than one site) Mixed (coexistence of SV and NSV) Rare forms |
| Segmented vitiligo | Unisegmental Bisegmental Plurisegmental |
| Undetermined/unclassified vitiligo | Mucosal (one site) Focal |
* Vitiligo Global Issues Consensus Conference.
Generally, NSV refers to depigmented skin lesions that demonstrate a tendency to symmetrical localization, while SV refers to uni-, bi-, or plurisegmental white patches with earlier age of onset than NSV [20]. Acrofacial vitiligo is mainly located on the face and/or distal parts of the body, especially fingers. We can distinguish a subcategory of the acrofacial type, the lip-tip variety, which refers to the cutaneous lips and the distal tips of the fingers. Sometimes, acrofacial vitiligo demonstrates an ability to progress to a generalized or universal form of disease [20,21]. Generalized vitiligo usually refers to a symmetrical, bilateral depigmented skin area, which occurs over the entire body [21]. Usually, mucosal vitiligo is present on oral and/or genital mucosae. An isolated form is classified as undetermined vitiligo, while mucosal vitiligo, in the context of generalized vitiligo, is classified as NSV [20,21]. The term “universal vitiligo” is used to describe skin lesions that cover approximately 80–90% of body surface. This form of hypopigmentation disorder is a common consequence of generalized vitiligo progression with melanocyte destruction, not only from the skin but also the body hair and, rarely, oral/genital mucosae [20,21]. Focal vitiligo is characterized by small isolated white patches, without typical segmental distribution. This subtype can be diagnosed if after 1–2 years there is no progression to NSV [20]. Mixed vitiligo displays clinical features of SV and NSV [22]. This subtype was first noticed in a pediatric patient with NSV, treated with the UVB narrow band therapy, which revealed a segmental depigmented skin area on the child’s body. The difference in response to the treatment suggested a coexistence of SV and NSV [23]. The rare forms of vitiligo include vitiligo punctate (if depigmented macules do not occur with classical vitiligo skin lesions, than the term ‘leukoderma punctata’ is used), hypochromic vitiligo (also referred to as ‘vitiligo minor’) and follicular vitiligo [20,21]. SV is usually characterized by notable progression with hair follicle melanocytes destruction called poliosis [20]. In contrast to SV, NSV generally does not affect hair bulbs, but due to vitiligo progression, a decrease or absence of melanin may take place [20]. Because of clinical differences between SV and NSV, in the past, it was supposed that these two forms of skin disorder are connected with distinct pathogenetic processes. Nevertheless, further studies have pointed to the contribution of inflammatory and immunity-related mechanisms for both SV and NSV [21,24]. Distinguishing these two major types of vitiligo is very important from the prognostic point of view [21]. In spite of the fact that the final presumptive area of the segment involved is one of the most important issues for a patient with SV, there is still no international agreement on this question due to the scarcity of data [20]. The Vitiligo European Task Force (VETF) is a grading system that scores the extent, stage, and progression of disease based on skin and hair pigmentation connected with melanocyte reservoir. It seems to be a suitable prognostic option for NSV, so it should be tested in clinical trials [20,25].
3. The Pathogenesis of Vitiligo
Vitiligo is probably the result of an interaction between genetic, environmental, and biochemical factors supporting autoimmune processes, in which melanocytes are destroyed on the body areas affected by the disease. Considering the high incidence (11–31%) of developing this skin disorder in the family, as well as the early age when the first symptoms are observed (usually in patients aged 10–30; over half of the cases are patients below 20), it has been suggested that genetic predispositions contribute to the development of vitiligo [4,26,27,28]. In addition, a study conducted by Alkhateeb et al. demonstrated that the outbreak age of the disease is lower in family cases [3]. This concept is supported by the fact that, compared to general population, vitiligo occurs more frequently (18 times) among siblings [3]. Genome analysis of multigeneration families with generalized depigmentation lesions and other associated diseases indicated that vitiligo is an autosomal dominant pattern with incomplete penetrance [29]. Other studies, based on familial aggregation, suggested that polygenic, multifactorial inheritance explains partial heritability [15]. It is interesting that the concordance for vitiligo in monozygotic twins was 23%, demonstrating a 60-fold increased risk in comparison with general population [3,15]. Additionally, these results suggest that apart from genetic factors, other components are also important for the development of this depigmenting skin disorder [3,15]. Further observations confirmed that the major genetic risk of vitiligo is strongly connected with polymorphism in HLA-A, HLA-DRB1/DQA1, and CPVL [5]. In fact, HLA genes are responsible for antigen presentation, while CPVL is postulated to play a role in antigen processing [30,31].
By means of the Genome Wide Association Study (GWAS), it was proved that vitiligo patients, as well as their relatives, are more exposed to other autoimmune diseases. Several genes have been identified which seem to be associated with both generalized vitiligo and other autoimmune/autoinflammatory diseases [15,30]. Usually, these patients show higher values of antibodies to thyroid peroxidase and thyroglobulin compared to the general population. Moreover, we can observe a greater incidence of rheumatoid arthritis, psoriasis, type 1 diabetes mellitus, pernicious anemia, systemic lupus erythematosus or Addison’s disease [5,28,29]. The GWA study indicated nearly 50 loci associated with genes controlling the innate (NLRP1, IFIH1, casp7, c1qtnf6, trif) and acquired (FOXP3, BACH2, CD80, CCR6, PTPN22, IL2R, αG2MB, HLA class I and II) immunity system [15,32,33,34]. This finding may, to a certain extent, explain recruitment of cells such as NK (natural killer), as well as increased production and secretion of proinflammatory proteins and cytokines including IL-1β, IL-6, IL-8 and heat shock proteins (HSP), especially HSP70i, participating in vitiligo progression [32,34,35]. Recently, it has been found that NLRP1, which is a gene located on chromosome 17p, is responsible for the regulation of the innate immune system, stimulation of IL-1β secretion and apoptotic process by coding an apoptosis protein from Ced-family. In addition, NLRP1 is a susceptibility gene for generalized vitiligo and other autoimmune vitiligo-associated diseases [33,36].
The depigmentation process is connected with both the decreasing number of melanocytes and their slower proliferation in comparison with healthy skin [37]. Despite the fact that the mechanisms of vitiligo pathogenesis are described in many studies, it is unclear which factor is crucial for activating melanocytes destruction. Some hypotheses suggest dysregulation in redox balance, which is strongly connected with lower expression of catalase, an enzyme which has a major role in protection from oxidative damage caused by reactive oxygen species (ROS) [5,38]. Cellular stress can directly influence melanocytes, stimulating them to release DAMPs (damage-associated molecular patterns). As a consequence, a noninfectious inflammatory reaction with recruitment of dendric cells (DCs), NK cells and CD8+ T cells to vitiligo lesions is initiated [39]. Chemical compounds such as 4-TBP (4-tertiary butyl phenol) or MBEH (monobenzyl ether of hydroquinone) are known to partake in ROS induction and activation of the unfolded protein response (UPR). The transcription factor x-box-binding protein 1 (XBP1) is a key UPR component demonstrating an increase due to an exposure to chemical triggers. It is partly responsible for regulating the production and secretion of proinflammatory cytokines IL-6 and IL-8 by melanocytes. Both of these interleukins are believed to influence the attraction of T-cells to depigmented skin lesions [40]. Furthermore, IL-6 has an impact on the expression of Intercellular Adhesion Molecule 1 (ICAM-1) on melanocytes, which might induce cytotoxic response by stimulating leukocyte-melanocyte attachment [41]. Interestingly, some studies point to the connection between the higher level of IL-6 in the tissue and/or serum and the presence of autoimmune disorders accompanying vitiligo [42,43]. Additionally, as a result of the oxidative stress, keratinocytes show growing expression of chemokine CXCL16, which has an influence on the migration of lymphocytes T CD8+ CXCR6+. The infiltration of these cells leads to decreasing the number of melanocytes within the area of skin lesions in patients with vitiligo [44].
CD4+ helper T cells are mainly responsible for activation of other immune cells by producing cytokines in response to antigen stimulation. Some studies suggest that in lymphocytes Th CD4+, Th1 and Th17 are the major subset in vitiligo development [45]. Patients with melanocytes destruction display a heightened level of cells Th17 [46]. It has been proved that this subset of helper T cells is involved in expression of IL-17A, IL-17F, as well as IL-22 [47,48]. In turn, IL-22 affects keratinocytes by stimulating them to secretion of IL-1β, also known as a mononuclear cell factor, inducing in this way an inflammatory response. In addition, IL-β, next to IL-1 and tumor necrosis factor (TNF-α), is a significant cytokine which demonstrates an influence on Th17 cell development [48]. Moreover, Th17 cells demonstrate ability to secrete IL-6 and also stimulate keratinocytes to express this interleukin [49]. Finally, a higher expression of IL-17 was noticed in the lesional edge, which seems to explain a possible role of lymphocyte Th17 in the pathogenesis of vitiligo [49]. Some studies indicated a positive correlation between the increased number of Th17 cells and the level of IL-21 and TGF-β1 and the area of the body occupated by depigmented skin patches [50]. It was also showed that the transcription factor for aryl hydrocarbon receptor (AhR) and retinoid-related orphan receptor (RORC), which are involved in the production of IL-22 by cells Th17 and Th22, increased considerably [46,51,52]. The research conducted by Zhen et al. demonstrated enhanced Th1 and Th17 response in the circulatory system of vitiligo patients [45]. In addition, Das et al. confirmed an increased concentration of IL-2, which is a cytokine produced by cells Th1 [53].
Regulatory T cells (Tregs) represent a subset of peripheral CD4+T cells responsible for, among others, inhibiting the development of autoimmune diseases. At the same time, they do not influence generalized immunodeficiency. Accumulating studies demonstrate that dysfunctions and/or deficiency of Tregs cells have an impact on occurrence of autoimmune diseases [54]. The analysis of the examination results, obtained by means of flow cytometry, showed a slightly decreased number of these cells in progressive vitiligo patients in comparison with stable patients [55]. This confirms reports on the possible recruitment of the circulating Tregs from the peripheral blood to inflamed skin areas. Other research reported a significant decrease in the amount of Tregs cells in marginal skin lesions in both active and stable forms of disease [56]. Despite this, regulatory T cells in vitiligo patients do not have a sufficient inhibitory effect on proliferation and the cytolytic activity of lymphocytes T CD8+. It shows a functional defect of peripheral regulatory T cells in vitiligo patients. These observations suggest that the impairment of Treg cell functions combined with the hyperactivity of lymphocytes T CD8+ may be significant for the development of the depigmented skin disorder in question [54,55].
4. Tissue Resident Memory Cells (TRM)
Tissue-resident memory T cells are a heterogeneous group that was first described about 10 years ago, due to the discovery of T cells which do not demonstrate the capacity to recirculate [57]. This long-living subset include CD8+ and CD4+ cells, which are phenotypically, functionally, and transcriptionally different from circulating effector memory T cells [18]. It has been proved that the skin of a healthy adult person consists of over 20 billion TRM cells [58,59]. Traditionally, T cells are divided into two major subsets: naïve and memory T cells—this is connected with pathogen exposure. As a result of being stimulated by presented antigen, naïve T cells are transformed into several subsets, including central memory T cells (TCM), effector memory T cells (TEM) and the recently discovered tissue-resident memory T cells (TRM). TCM cells move within lymphoid tissue, while TEM cells circulate between peripheral tissues. TRM, in turn, are cells that do not have the ability to recirculate between the vascular system and the tissues in which they reside [59,60]. It is expected that the resident subpopulation of memory T cells can develop in the skin from cells that previously expressed KLRG1 protein [61]. Their primary role is to provide antiviral and antibacterial protection in non-lymphoid tissues [18,62,63,64].
The CD8+ TRM cells formation process is triggered by IL-7, TGF-β and IL-15 [62,65], wherein IL-15 has proven additional influence on their maintenance [66]. Their main feature is a capacity to survive and stay activated in the lesional skin for at least half a year after infection [67]. Due to the fact that cell residence requires specific environmental conditions, including limited access to oxygen and glucose, TRM cells had to develop a different transcriptional profile, compared to their precursors [5]. Adaptations of this long-living T cells subset among others include the following transcription factors: Hobit, Blimp1, and Runx3. It has been demonstrated that Blimp1 is responsible for regulating cytotoxic capacity by stimulating granzyme B expression, while Hobit is indispensable in the long-term maintenance of this enzyme [68]. IL-15 and the transcription factor T-bet stimulate expression of Hobit factor, whereas Blimp1 is induced by Runx3 [69,70]. Although the role of Runx3 in CD8+ T cells is not fully determined, it is suggested that this factor has an impact on the presence of CD69 and CD103 surface markers, so it is essential for TRM cell maintenance [71].
TRM cell population is characterized by specific markers of residency, such as CD49a, CD69 and CD103 (Table 2), though not all TRM cells express these particles [57,72]. Furthermore, the expression of adhesion molecules by CD4+ tissue-resident lymphocytes seems to be debatable. Some studies indicate the possibility of expression CD103 and CD69 by resided in the skin CD4+ effector T cells after antigen exposure [73,74]. Recent data presented by Wilk et al. demonstrated that infection triggered by B. pertussis induces CD69+CD4+ TRM cells with ability to express CD103 marker during and after infection [73]. Currently, the best described are CD8+ T cells with CD69 and CD103 surface markers [62]. CD103 (α-subunit of the αEβ7 integrin receptor) is involved in binding E-cadherin synthesized on epithelial cells and in this way promotes TRM cell retention. In turn, work published by Mackay et al. indicated that CD69 is needed for TRM cell development in nonlymphoid tissues, including skin [75]. Expression of this molecule seems to be stimulated by various factors such as antigens and type I interferon exposure [75]. In addition, CD69 has been found to suppress the function of sphingosine 1-phosphate receptor 1 (S1PR1), which appears to be crucial for TRM cell retention in tissues [75]. CD49a, also known as a very late antigen 1 (VLA-1), is an α-subunit of the α1β1 integrin receptor responsible for the induction of granzyme B, perforin, and IFN-γ expression due to the stimulation of IL-15. Therefore, it determines the high cytotoxic capacities of TRM cells [63]. Importantly, the expression of these molecules can vary between cells, depending on what tissue they are in [61]. TRM cell localization is probably related to the presence of β growth factor (TGF-β), which plays the main role in the expression of CD103 marker and in most cases is essential for tissue-resident lymphocytes development [61,62,63].
Table 2.
Surface markers of TRM cells and their main functions.
| Function | |||
|---|---|---|---|
| CD4+/ CD8+ | Co-receptors of the T cell receptor (TCR) [59] | ||
| Surface marker | CD 49a+ | Secretion of granzyme B, perforin, IFN-γ and achieving high cytotoxic properties following IL-15 stimulation [63] | |
| CD 69+ | Blockade of the sphingosine 1-phosphate receptor 1 (S1PR1) [75] | ||
| CD 103+ | Participation in binding TRM cells to E-cadherin to promote retention within epithelial tissues [72] | ||
TRM cells are formed as a result of stimulating naïve T cells by antigen-dependent signals. The long-living population of T cells in each tissue is able to recognize specific pathogens [76]. Recent studies have shown that TRM cells, after renewed contact with the antigen, begin to divide, thus leading to the formation of new subsets that may be present in the tissues for several months to several years after the stimulus factor disappears. For example, infection-induced CD8+ TRM are found in the nasal cavity epithelium up to 3 months after the onset of a respiratory tract infection [77], while in skin attacked by HSV for up to a year [78]. On the other hand, it has been proved that mice kept in pathogen-free and clean barrier facilities had few skin TRM cells [79]. It is generally agreed that TRM cells have the ability to slowly migrate in their environment. Therefore, antigen-specific cells, demonstrating uninterrupted movement in the epidermis, increase the protection of the tissue in which they reside [80]. Due to this property, TRM cells are able to identify a cell with expression of the proper antigen within a few hours [81,82]. In this way, it is possible to distinguish HSV-specific TRM cells present in the skin, rotavirus-stimulated TRM cells in the gut, or specifically for influenza virus tissue-resident lymphocytes localized near the airways and bronchovascular bundles in the lungs [73,83,84]. Furthermore, TRM CD4+ have a protective effect on the mucosa of the small intestine, and female genitals. They demonstrate an ability to influence on the course of skin infections involving Leishmania or Candida albicans by immune response based on IL-17 production [60,73,85].
On the other hand, their ability to multiply rapidly due to the antigenic stimulation shows the harmful effects of the influence of TRM cells on the body’s functioning. Furthermore, tissue resident memory T cells can increase their number during an ongoing inflammatory process, even without the presence of pathogens [59]. Considering the facts above, in recent years, studies have found that autoreactive TRM cells may play a role in the pathogenesis of many autoimmune disorders, such as psoriasis, rheumatoid arthritis, allergic contact dermatitis, or autoimmune hepatitis [3,85,86,87,88,89]. Some experiments conducted on mouse models demonstrating the graft-vs.-host disease (GVHD) indicated the presence of TRM cells in the digestive tract [90]. Recent research has been focused on broadening our understanding of the role of TRM cells in the pathogenesis of vitiligo.
5. TRM Cells and Vitiligo
A histological analysis of vitiligo patients’ skin biopsy revealed that the margin zones of depigmented lesions were strongly dominated by CD4+ and CD8+ T cells [91]. The hypothesis that CD8+ are critical for melanocyte depletion was formulated after discovering that these cytotoxic T cells isolated from vitiligo patches were able to induce depigmentation in an autologous healthy skin explants ex vivo [92], while the potential role of CD4+ cells is still not fully determined [93]. The mechanism by which perilesional CD8+ T cells cause melanocytes apoptosis is a consequence of their production of proinflammatory cytokines, especially IFN-γ [92]. Therefore, it was suggested that there was a correlation between CD8+ T cells response and the development of vitiligo [92]. In addition, patients with stronger CD8+ activity required a longer treatment before the first results were visible. This observation implies a connection between the reactivity of melanocyte antigen-specific T cells in the skin and the appearance of depigmented areas [92]. Interestingly, many of the CD8+ T cells presented within vitiligo patches possessed a TRM cell phenotype.
The role TRM cells play in the pathogenesis of vitiligo is proven by the fact that skin lesions often appear in the same places they occurred before treatment. A similar phenomenon is observed in psoriasis [85]. It was suspected that TRM CD8+ may take active part in blocking repigmentation, by inhibiting melanin-producing cells in the epithelium. Additionally, they probably affect the regeneration of melanocytes by blocking local regulatory T cells (Tregs), which play a vital role for hair follicles stem cells in this process [94]. Latest findings confirm the existence of autoreactive CD8+ cells with CD103+CD69+CD49a+ TRM phenotype in the skin of vitiligo patients [4,28,40,84]. Furthermore, melanocyte-specific CD8+ TRM cells were highly present in lesional skin as compared to blood regardless of whether the actual disease status was active or stable [86].
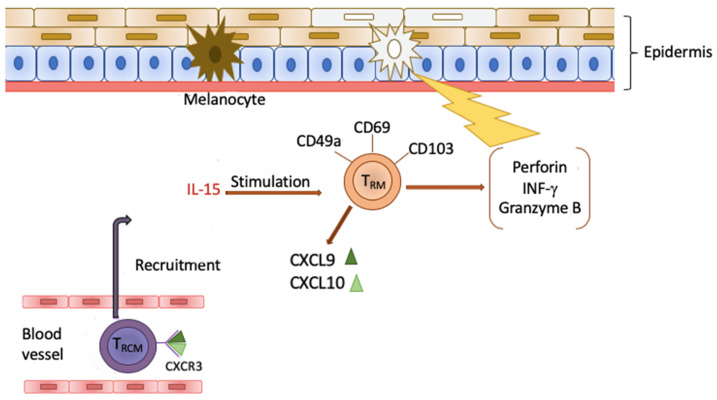
Research from 2013 [62] focused on receptor CXCR3 (chemokine receptor CXCL9 and CXCL10), which is important for the location of the effector T cells in the epithelium, as well as for the growth of TRM cells. Due to the affinity of CXCL9 and CXCL10, chemokines for receptor CXCR3 found on the surface of TRCM cells (recirculating TRM) are able to recruit them to the skin. Next, TRM and TRCM, through the synergistic effect and secretory properties of IFN-γ, trigger depigmentation of the affected skin patches on the body. It is interesting that the circulating CXCR3+ CD8+ TRCM cells in vitiligo patients show increased proliferation potential compared to the cells in healthy people [86]. Moreover, it was observed that the inhibition of TRCM recruitment to the skin had reversed the symptoms of the disease [95]. Considering the role of the chemokines and their receptor, the attempts to base the therapy on targeting the CXCL9/10-CXCR3 path may potentially prove very effective in vitiligo treatment. In addition, some studies revealed the presence of CXCR3 on the majority of CD8+ TRM, including the cells showing specificity for melanocyte receptors and antigens. Those cells had secretory properties IFN-γ and TNF-α [86]. Other discoveries indicated that IFN-γ and granzyme B are the key cytokines partaking in the course of vitiligo, because they stimulate the apoptosis of melanocytes [96]. These findings show the significant role of TRM cells in the pathogenesis of vitiligo (Figure 1), which explains the growing interest in them in the quest for new treatments.
Figure 1.
TRM cells demonstrate expression of CD49a, CD69 and CD103 particles. Due to the stimulation of IL-15, they secreting perforin, granzyme B and IFN-γ, indicating in this way a cytotoxic effect on melanocytes. Additionally, TRM produce chemokines CXCL9 and CXCL10, which, after binding with receptor CXCR3 on the surface of TRCM cells, influence their recruitment from the blood vessels to the skin. Next, through the synergistic effect, they cause the depigmentation of the skin in the course of disease.
6. Clinical Significance of TRM Cells
Some studies have demonstrated a correlation between TRM cells and IL-15. It was shown that the formation of TRM largely depends on IL-15, and IL-15 promotes the function of TRM cells ex vivo [66]. Moreover, continuous signaling of this cytokine is indispensable for skin TRM cells to survive. Thus, in the course of developing new therapeutic methods, subsequent researcher were focused on this interleukin. Three forms of IL-15 receptor can be distinguished: a monomer, heterodimer, and heterotrimer. The heterotrimeric IL-15 receptor consists of CD122, CD215, and CD132 subunits. This receptor is mainly expressed on NK cells, whereas the heterodimeric receptor is composed of CD122 and CD132 molecules. It is generally present on memory T cells population. What is more, both human and mouse TRM cells which exist in skin lesions present elements of the IL-15 receptor [66]. Furthermore, specific for melanocytes, TRM cells demonstrate expression of CD122. It was found that using CD122 antibody reversed the disease in mice with vitiligo [62,65,66,69]. A 2-week short-term treatment decreased IFN-γ expression, while an 8-week long-term blockade of the IL-15 receptor caused the reduction of autoreactive TRM cells [66]. This observation proves that targeting the IL-15 signal transmission may be an effective method of treatment, both in vitiligo and, perhaps, other diseases where TRM cells play a role in a pathogenesis.
Another trend shows that the life functions of TRM cells also depend on exogenous lipids uptake, as well as their oxidative metabolism. CD8+ TRM demonstrate overexpression of lipoprotein lipase (lpl), CD36 (a lipid scavenger receptor) and fatty acid-binding proteins (FABP4 and FABP5), which are molecules facilitating exogenous FFAs acquisition and metabolism [84]. Interestingly, such activity of these molecules is not present in naïve T cells or effector memory T cells [84]. It is proved that cells in vivo with a disability of uptaking exogenous FFAs died prematurely. Additionally, it was indicated that administering medication blocking lipid metabolism decreases TRM cells survivality. For example, etomoxir treatment inhibits the activity of CPT-1 (carnitine palmitoyltransferase-1), which is an enzyme on the mitochondrial membrane. As a result, fatty acid import into these organelles is reduced. Summarizing, CD8+ TRM cells which are unable to metabolize exogenous FFAs because of deficiency of FABP4 (Adipocyte—FABP), FABP5 (Epiderma—FABP), or blocking mitochondrial β-oxidation cannot remain in the skin. The lack of fatty acid-binding proteins affects long-term survival of CD8+ TRM cells in the skin but does not have any influence on cytotoxic T cells proliferation or recruitment [97]. These observations suggest that by interfering with lipid metabolism processes, it may be possible to manipulate the number of tissue-resident lymphocytes from peripheral tissues during treatment of chronic inflammatory conditions [84,97].
7. Anti-Tumor Role of TRM Cells
TRM cells demonstrate an ability to stimulate protective immune responses against pathogen reinfection. They represent a major line of defense by recruiting memory T cells and B cells to the site of ongoing inflammation [67,82,98]. The latest studies demonstrate another very promising function of TRM cells in antitumor immunity. Nevertheless, this phenomenon is not fully understood yet. Some studies with a mouse model shed some light on tumor-specific CD8+ TRM cells which might have an inhibitor effect on highly aggressive melanoma. Tissue-resident memory T cells, driven by a model of autoimmune vitiligo, were capable of slowing down the growth of melanoma, in a CD103-dependent manner [99]. In addition, multiple groups’ observations indicated that infiltration of CD8+ T cells with a TRM phenotype has an impact on patients’ increased survival in endometrial, breast and high-grade serous ovarian cancer (HGSC) [100,101,102]. Gálvez-Cancino et al. demonstrated that intradermal vaccination is able to stimulate generation of skin-TRM cells from their memory precursors. This vaccination-provoked long-living subset was responsible for significant suppression of B16F10 melanoma [99]. Similarly, OVA-expressing melanoma progression was delayed by injecting recombinant vaccine virus, expressing full-length ovalbumin (OVA) protein. As a result, CD8+ TRM and recirculating memory T cells (TCIRC) were generated. Intraperitoneal vaccination demonstrated that both TCIRC and TRM cells were able to protect against B16-OVA re-development [103].
8. Conclusions
Discovering the TRM cells and connecting their occurrence to the pathogenesis of autoimmune skin diseases allowed the researchers to understand the complicated relations between melanocytes and keratinocytes. Due to recent studies focusing on tissue-resident memory T cells, we will hopefully be able to apply new effective therapeutic strategies in vitiligo treatment in the near future. Identifying the TRM cells precursors and describing their mechanisms helped to broaden the knowledge about their influence on certain processes in the human body, which seems to be a very promising trend.
Though the specific contribution of TRM cells is not unreservedly recognized, emergency reports point to the growing significance of these cells in the development of cancer diseases. It seems that manipulation of tissue-resident lymphocytes might be a promising target for future anti-tumor therapies.
Funding
This research received no external funding.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- 1.Mahdi P., Rouzbahani M., Amali A., Khiabanlu S.R., Kamali M. Audiological manifestation in vitiligo patient. Iran J. Otorhinolaryngol. 2012;24:35–40. [PMC free article] [PubMed] [Google Scholar]
- 2.Kopera D. Historical aspects and definition of vitiligo. Clin. Dermatol. 1997;15:841–843. doi: 10.1016/S0738-081X(97)00124-7. [DOI] [PubMed] [Google Scholar]
- 3.Alkhateeb A., Fain P.R., Thody A., Bennett D.C., Spritz R.A. Epidemiology of vitiligo and associated autoimmune diseases in Caucasian probands and their families. Pigment Cell Res. 2003;16:208–214. doi: 10.1034/j.1600-0749.2003.00032.x. [DOI] [PubMed] [Google Scholar]
- 4.Kutwin M., Sysa-Jędrzejowska A., Woźnicka A. Virtiligo and autoimmune diseases. Dermatol. 2016;103:400–404. doi: 10.5114/dr.2016.62892. [DOI] [Google Scholar]
- 5.Frisoli M.L., Essien K., Harris J.E. Vitiligo: Mechanisms of Pathogenesis and Treatment. Annu. Rev. Immunol. 2020;38:621–648. doi: 10.1146/annurev-immunol-100919-023531. [DOI] [PubMed] [Google Scholar]
- 6.Salzes C., Abadie S., Seneschal J., Whitton M., Meurant J.-M., Jouary T., Ballanger F., Boralevi F., Taïeb A., Taïeb C., et al. The Vitiligo Impact Patient scale (VIPs): Development and validation of a vitiligo burden assessment tool. J. Investig. Dermatol. 2016;136:52–58. doi: 10.1038/JID.2015.398. [DOI] [PubMed] [Google Scholar]
- 7.Prasad D. A new era of vitiligo research and treatment. J. Cutan. Aesthet. Surg. 2013;6:63–64. doi: 10.4103/0974-2077.112664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Fukazawa K., Sakagami M., Umemoto M., Senda T. Development of Melanosomes and Cytochemical Observation of Tyrosinase Activity in the Inner Ear. ORL J. Otorhinolaryngol. Relat. Spec. 1994;56:247–252. doi: 10.1159/000276667. [DOI] [PubMed] [Google Scholar]
- 9.Creel D., Garber S.R., King R.A., Witkop C.J. Auditory brainstem anomalies in human albinos. Science. 1980;209:1253–1255. doi: 10.1126/science.7403883. [DOI] [PubMed] [Google Scholar]
- 10.Murillo-Cuesta S., Contreras J., Zurita E., Cediel R., Cantero M., Varela-Nieto I., Montoliu L. Melanin precursors prevent premature age-related and noise-induced hearing loss in albino mice. Pigment Cell Melanoma Res. 2010;23:72–83. doi: 10.1111/j.1755-148X.2009.00646.x. [DOI] [PubMed] [Google Scholar]
- 11.De Jong M.A., Adelman C., Gross M. Hearing loss in vitiligo: Current concepts and review. Eur. Arch. Oto-Rhino-Laryngol. 2017;274:2367–2372. doi: 10.1007/s00405-017-4452-8. [DOI] [PubMed] [Google Scholar]
- 12.Opdecamp K., Nakayama A., Nguyen M.T., Hodgkinson C.A., Pavan W.J., Arnheiter H. Melanocyte development in vivo and in neural crest cell cultures: Crucial dependence on the Mitf basic-helix-loop-helix transcription factor. Development. 1997;124:2377–2386. doi: 10.1242/dev.124.12.2377. [DOI] [PubMed] [Google Scholar]
- 13.Sato-Jin K., Nishimura E.K., Akasaka E., Huber W., Nakano H., Miller A., Du J., Wu M., Hanada K., Sawamura D., et al. Epistatic connections between microphthalmia-associated transcription factor and endothelin signaling in Waardenburg syndrome and other pigmentary disorders. FASEB J. 2008;22:1155–1168. doi: 10.1096/fj.07-9080com. [DOI] [PubMed] [Google Scholar]
- 14.Zhang Y., Cai Y., Shi M., Jiang S., Cui S., Wu Y., Gao X.-Y., Chen H.-D. The Prevalence of Vitiligo: A Meta-Analysis. Plos One. 2016;11:e0163806. doi: 10.1371/journal.pone.0163806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Spritz R.A. The genetics of generalized vitiligo. Curr. Dir. Autoimmun. 2008;10:244–257. doi: 10.1159/000131501. [DOI] [PubMed] [Google Scholar]
- 16.Harris J.E. Cellular stress and innate inflammation in organ-specific autoimmunity: Lessons learned from virtiligo. Immunol Rev. 2016;269:11–25. doi: 10.1111/imr.12369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Cavalieé M., Ezzedine K., Fontas E., Montaudieé H., Castela E., Bohadoran P., Taïeb A., Lacour J.P., Passeron T. Maintenance therapy of adult vitiligo with 0.1% tacrolimus ointment: A randomized, double blind, placebo-controlled study. J. Investig. Derm. 2015;135:970–974. doi: 10.1038/jid.2014.527. [DOI] [PubMed] [Google Scholar]
- 18.Wu H., Liao W., Li Q., Long H., Yin H., Zhao M., Chan V., Lau C.S., Lu Q. Pathogenic role of tissue resident memory T cells in autoimmune diseases. Autoimmun. Rev. 2018;17:906–911. doi: 10.1016/j.autrev.2018.03.014. [DOI] [PubMed] [Google Scholar]
- 19.Topham D.J., Reilly E.C. Tissue-Resident Memory CD8+ T Cells: From Phenotype to Function. Front. Immunol. 2018;9:515. doi: 10.3389/fimmu.2018.00515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ezzedine K., Lim H.W., Suzuki T., Katayama I., Hamzavi I., Lan C.C., Goh B.K., Anbar T., Silva de Castro C., Lee A.Y., et al. Vitiligo Global Issue Consensus Conference Panelists. Revised classification/nomenclature of vitiligo and related issues: The Vitiligo Global Issues Consensus Conference. Pigment. Cell Melanoma Res. 2012;25:E1–E13. doi: 10.1111/j.1755-148X.2012.00997.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Bergqvist C., Ezzedine K. Vitiligo: A Review. Dermatology. 2020;10:1–22. doi: 10.1159/000506103. [DOI] [PubMed] [Google Scholar]
- 22.Ezzedine K., Gauthier Y., Léauté-Labrèze C., Marquez S., Bouchtnei S., Jouary T., Taïeb A. Segmental vitiligo associated with generalized vitiligo (mixed vitiligo): A retrospective case series of 19 patients. J. Am. Acad. Dermatol. 2011;65:965–971. doi: 10.1016/j.jaad.2010.08.031. [DOI] [PubMed] [Google Scholar]
- 23.Gauthier Y., Cario Andre M., Taïeb A. A critical appraisal of vitiligo etiologic theories. Is melanocyte loss a melanocytorrhagy? Pigment Cell Res. 2003;16:322–332. doi: 10.1034/j.1600-0749.2003.00070.x. [DOI] [PubMed] [Google Scholar]
- 24.Van Geel N.A., Mollet I.G., De Schepper S., Tjin E.P.M., Vermaelen K., Clark R.A., Kupper T.S., Luiten R.M., Lambert J. First histopathological and immunophenotypic analysis of early dynamic events in a patient with segmental vitiligo associated with halo nevi. Pigment Cell Melanoma Res. 2010;23:375–384. doi: 10.1111/j.1755-148X.2010.00703.x. [DOI] [PubMed] [Google Scholar]
- 25.Taïeb A., Picardo M. The definition and assessment of vitiligo: A consensus report of the Vitiligo European Task Force. Pigment Cell Res. 2007;20:27–35. doi: 10.1111/j.1600-0749.2006.00355.x. [DOI] [PubMed] [Google Scholar]
- 26.Nejad S.B., Qadim H.H., Nazeman L., Fadaii R., Goldust M. Frequency of autoimmune diseases in those suffering from vitiligo in comparison with normal population. Pak. J. Biol. Sci. 2013;16:570–574. doi: 10.3923/pjbs.2013.570.574. [DOI] [PubMed] [Google Scholar]
- 27.Ingordo V., Cazzaniga S., Raone B., Digiuseppe M.D., Musumeci M.L., Fai D., Pellegrino M., Pezzarossa E., Di Lemia V., Battarra V.C., et al. Circulating autoantibodies and autoimmune comorbidities in vitiligo patients: A multicenter Italian study. Dermatology. 2014;228:240–249. doi: 10.1159/000357807. [DOI] [PubMed] [Google Scholar]
- 28.Narita T., Oiso N., Fukai K., Kabashima K., Kawada A., Suzuki T. Generalized vitiligo and associated autoimmune diseases in Japanese patients and their families. Allergol. Int. 2011;60:505–508. doi: 10.2332/allergolint.11-OA-0303. [DOI] [PubMed] [Google Scholar]
- 29.Alkhateeb A., Stetler G.L., Old W., Talbert J., Uhlhorn C., Taylor M., Fox A., Miller C., Dills D.G., Ridgway E.C., et al. Mapping of an autoimmunity susceptibility locus (AlS1) to chromoseome 1p31.3-p32.2. Hum. Mol. Genet. 2002;11:661–667. doi: 10.1093/hmg/11.6.661. [DOI] [PubMed] [Google Scholar]
- 30.Spritz R.A., Andersen G.H.L. Genetics of vitiligo. Dermatol. Clin. 2017;35:245–255. doi: 10.1016/j.det.2016.11.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Li Z., Ren J., Niu X., Xu Q., Wang X., Liu Y., Xiao S. Meta-analysis of the association between vitiligo and human leukocyte antigen-A. BioMed. Res. Int. 2016:1–13. doi: 10.1155/2016/5412806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Zar A.R., Malik A., Mahmood A., Naseer Q.A., Yumei L. Pathogenesis and the emerging therapy of virtiligo. Arch. Clin. Biomed. Res. 2019;3:361–373. doi: 10.26502/acbr.50170080. [DOI] [Google Scholar]
- 33.Levandowski C.B., Mailloux C.M., Ferrara T.M., Gowan K., Ben S., Jin Y., McFann K.K., Holland P.J., Fain P.R., Dinarello C.A., et al. NLRP1 haplotypes associated with vitiligo and autoimmunity increase interleukin-1beta processing via the NLRP1 inflammasome. Proc. Natl. Acad. Sci. USA. 2013;110:2952–2956. doi: 10.1073/pnas.1222808110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Shen C., Gao J., Sheng Y., Dou J., Zhou F., Zheng X., Ko R., Tang X., Zhu C., Yin X., et al. Genetic Susceptibility to Vitiligo: GWAS Approaches for Identifying Vitiligo Susceptibility Genes and Loci. Front. Genet. 2016;7:3. doi: 10.3389/fgene.2016.00003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Van den Boorn J.G., Jakobs C., Hagen C., Renn M., Luiten R.M., Melief C.J., Tuting T., Garbi N., Hartmann G., Homung V. Inflammasome-Dependent Induction of Adaptive NK Cell Memory. Immunity. 2016;44:1406–1421. doi: 10.1016/j.immuni.2016.05.008. [DOI] [PubMed] [Google Scholar]
- 36.Jin Y., Birlea S.A., Fain P.R., Spritz R.A. Genetic Variations in NALP1 Are Associated with Generalized Vitiligo in a Romanian Population. J. Investig. Dermatol. 2007;127:2558–2562. doi: 10.1038/sj.jid.5700953. [DOI] [PubMed] [Google Scholar]
- 37.Puri N., Mojamdar M., Ramaiah A. In Vitro Growth Characteristics of Melanocytes Obtained From Adult Normal and Vitiligo Subjects. J. Investig. Dermatol. 1987;88:434–438. doi: 10.1111/1523-1747.ep12469795. [DOI] [PubMed] [Google Scholar]
- 38.Schallreuter K.U., Moore J., Wood J.M., Beazley W.D., Gaze D.C., Tobin D.J., Marshall H.S., Panske A., Panzig E., Hibberts N.A. In Vivo and In Vitro Evidence for Hydrogen Peroxide (H2O2) Accumulation in the Epidermis of Patients with Vitiligo and its Successful Removal by a UVB-Activated Pseudocatalase. J. Investig. Dermatol. Symp. Proc. 1999;4:91–96. doi: 10.1038/sj.jidsp.5640189. [DOI] [PubMed] [Google Scholar]
- 39.Richmond J.M., Frisoli M.L., Harris J.E. Innate immune mechanisms in vitiligo: Danger from within. Curr. Opin. Immunol. 2013;25:676–682. doi: 10.1016/j.coi.2013.10.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Toosi S., Orlow S.J., Manga P. Vitiligo-inducing phenols activate the unfolded protein response in melanocytes resulting in upregulation of IL6 and IL8. J. Investig. Dermatol. 2012;132:2601–2609. doi: 10.1038/jid.2012.181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Kirnbauer R., Charvat B., Schauer E., Köck A., Urbanski A., Förster E., Neuner P., Assmann I., Luger T.A., Schwarz T. Modulation of intercellular adhesion molecule-1 expression on human melanocytes and melanoma cells: Evidence for a regulatory role of IL-6, IL-7, TNF beta, and UVB light. J. Investig. Dermatol. 1992;98:320–326. doi: 10.1111/1523-1747.ep12499793. [DOI] [PubMed] [Google Scholar]
- 42.Alexandraki K.I., Piperi C., Ziakas P.D., Apostolopoulos N.V., Makrilakis K., Syriou V., Diamanti-Kandarakis E., Kaltsas G., Kalofoutis A. Cytokine secretion in long-standing diabetes mellitus type 1 and 2: Associations with low-grade systemic inflammation. J. Clin. Immunol. 2008;28:314–321. doi: 10.1007/s10875-007-9164-1. [DOI] [PubMed] [Google Scholar]
- 43.Salvi M., Girasole G., Pedrazzoni M., Passeri M., Giuliani N., Minelli R., Braverman L.E., Roti E. Increased serum concentrations of interleukin-6 (IL-6) and soluble IL-6 receptor in patients with Graves’ disease. J. Clin. Endocrinol. Metab. 1996;81:2976–2979. doi: 10.1210/jcem.81.8.8768861. [DOI] [PubMed] [Google Scholar]
- 44.Li S., Zhu D., Yang Y., Jian Z., Guo S., Dai W., Shi Q., Ge R., Ma J., Liu L., et al. Oxidative stress drives CD8(+) T-cell skin trafficking in patients with vitiligo through CXCL16 upregulation by activating the unfolded protein response in keratinocytes. J. Allergy Clin. Immunol. 2017;140:177–189. doi: 10.1016/j.jaci.2016.10.013. [DOI] [PubMed] [Google Scholar]
- 45.Zhen Y., Yao L., Zhong S., Song Y., Cui Y., Li S. Enhanced Th1 and Th17 responses in peripheral blood in active non-segmental vitiligo. Arch. Dermatol. Res. 2016;308:703–710. doi: 10.1007/s00403-016-1690-3. [DOI] [PubMed] [Google Scholar]
- 46.Yssel H., Pene J. Interleukin-22-producing T cells: A specialized population involved in skin inflammation. Immunol. Cell. Biol. 2009;87:574–576. doi: 10.1038/icb.2009.68. [DOI] [Google Scholar]
- 47.Liang S.C., Tan X.-Y., Luxenberg D.P., Karim R., Dunussi-Joannopoulos K., Collins M., Fouser L.A. Interleukin (IL)-22 and IL-17 are coexpressed by Th17 cells and cooperatively enhance expression of antimicrobial peptides. J. Exp. Med. 2006;203:2271–2279. doi: 10.1084/jem.20061308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Wilson N.J., Boniface K., Chan J.R., McKenzie B.S., Blumenschein W.M., Mattson J.D. Development, cytokine profile and function of human interleukin 17–producing helper T cells. Nat. Immunol. 2007;8:950–957. doi: 10.1038/ni1497. [DOI] [PubMed] [Google Scholar]
- 49.Bassiouny D.A., Shaker O. Role of interleukin-17 in the pathogenesis of vitiligo. Clin. Exp. Dermatol. 2010;36:292–297. doi: 10.1111/j.1365-2230.2010.03972.x. [DOI] [PubMed] [Google Scholar]
- 50.Li Z., Shi Y.L., Li K., Hamzavi I., Gao T.W., Huggins R.H., Lim H.W., Mi Q.S. Increased circulating Th17 cells and elevated serumlevels of TGF-beta and IL-21 are correlated with humannon-segmental vi- tiligo development. Pigment Cell Melanoma Res. 2015;28:324–329. doi: 10.1111/pcmr.12355. [DOI] [PubMed] [Google Scholar]
- 51.Trifari S., Kaplan C.D., Tran E.H., Natasha K., Crellin N.K., Spits H. Identification of a human helper T cell population that has abundant production of interleukin 22 and is distinct from Th17, Th1 and Th2 cells. Nat. Immunol. 2009;10:864–871. doi: 10.1038/ni.1770. [DOI] [PubMed] [Google Scholar]
- 52.Behfarjam F., Jadali Z. Vitiligo patients show significant up-regulation of aryl hydrocarbon receptor transcription factor. An. Bras. Derm. 2018;93:302–303. doi: 10.1590/abd1806-4841.20187183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Das D., Akhtar S., Kurra S., Gupta S., Sharma A. Emerging role of immune cell network in autoimmune skin disorders: An update on pemphigus, vitiligo and psoriasis. Cytokine Growth Factor Rev. 2019;45:35–44. doi: 10.1016/j.cytogfr.2019.01.001. [DOI] [PubMed] [Google Scholar]
- 54.Lili Y., Yi W., Ji Y., Yue S., Weimin S., Ming L. Global activation of CD8+ cytotoxic T lymphocytes correlates with an impairment in regulatory T cells in patients with generalized vitiligo. PLoS ONE. 2012:7. doi: 10.1371/journal.pone.0037513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Ben Ahmed M., Zaraa I., Rekik R., Elbeldi-Ferchiou A., Kourda N., Belhadj Hmida N., Abdeladhim M., Karoui O., Ben Osman A., Mokni M., et al. Functional defects of peripheral regulatory T lymphocytes in patients with progressive vitiligo. Pigment Cell Melanoma Res. 2011;25:99–109. doi: 10.1111/j.1755-148X.2011.00920.x. [DOI] [PubMed] [Google Scholar]
- 56.Abdallah M., Lotfi R., Othman W., Galal R. Assessment of tissue FoxP3+, CD4+and CD8+T-cells in active and stable nonsegmental vitiligo. Int. J. Dermatol. 2014;53:940–946. doi: 10.1111/ijd.12160. [DOI] [PubMed] [Google Scholar]
- 57.Mami-Chouaib F., Tartour E. Tissue Resident Memory T cells. Front. Immunol. 2019 doi: 10.3389/fimmu.2019.01018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Clark R.A., Chong B., Mirchandani N., Brinster N.K., Yamanaka K., Dowgiert R.K., Kupper T.S. The vast majority of CLA+ t cells are resident in normal skin. J. Immunol. 2006;176:4431–4439. doi: 10.4049/jimmunol.176.7.4431. [DOI] [PubMed] [Google Scholar]
- 59.Khalil S., Bardawil T., Kurban M., Abbas O. Tissue-resident memory T cells in the skin. Inflamm. Res. 2020;69:245–254. doi: 10.1007/s00011-020-01320-6. [DOI] [PubMed] [Google Scholar]
- 60.Chen L., Shen Z. Tissue-resident memory T cells and their biological characteristics in the recurrence of inflammatory skin disorders. Cell. Mollecular Immunol. 2019;17:64–75. doi: 10.1038/s41423-019-0291-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Martin M.D., Badovinac V.P. Defining Memory CD8 T Cell. Front. Immunol. 2018;9:2692. doi: 10.3389/fimmu.2018.02692. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Mackay L.K., Rahimpour A., Ma J.Z., Collins N., Stock A.T., Hafon M.L., Vega-Ramos J., Lauzurica P., Mueller S.N., Stefanovic T., et al. The developmental pathway for CD103+ CD8+ tissue-resident memory T cells of skin. Nat. Immunol. 2013;14:1294–1391. doi: 10.1038/ni.2744. [DOI] [PubMed] [Google Scholar]
- 63.Cheuk S., Schlums H., Gallais Sérézal I., Martini E., Chiang S.C., Marquardt N., Gibbs A., Detlofsson E., Forkel M., Höög C., et al. CD49a expression defines tissue - resident CD8+ T cells poised for cytotoxic function in human skin. Immunity. 2017;46:287–300. doi: 10.1016/j.immuni.2017.01.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Casey K.A., Fraser K.A., Schenkel J.M., Moran A., Abt M.C., Beura L.K., Lucas P.J., Artis D., Wherry J., Hogquist K., et al. Antigen-independent differentiation and maintenance of effector-like resident memory T cells in tissues. J. Immunol. 2012;188:4866–4875. doi: 10.4049/jimmunol.1200402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Adachi T., Kobayashi T., Sugihara E., Yamada T., Ikuta K., Pittaluga S., Saya H., Amagai M., Nagao K. Hair follicle–derived IL-7 and IL-15 mediate skin-resident memory T cell homeostasis and lymphoma. Nat. Med. 2015;21:1272–1279. doi: 10.1038/nm.3962. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Richmond J.M., Strassner J.P., Zapata L., Jr., Garg M., Riding R.L., Refat M.A., Fan X., Azzolino V., Tovar-Garza A., Tsurushita N., et al. Antibody blockade of IL-15 signaling has the potential to durably reverse vitiligo. Sci. Transl. Med. 2018;10:eaam7710. doi: 10.1126/scitranslmed.aam7710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Jiang X., Clark R.A., Liu L., Wagers A.J., Fuhlbrigge R.C., Kupper T.S. Skin infection generates non-migratory memory CD8+ TRM cells providing global skin immunity. Nature. 2012;483:227–231. doi: 10.1038/nature10851. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Kragten N.A.M., Behr F.M., Vieira Braga F.A., Remmerswaal E.B.M., Wesselink T.H., Oja A.E., Hombrink P., Kallies A., Van Lier R.A.W., Stark R., et al. Blimp-1 induces and Hobit maintains the cytotoxic mediator granzyme B in CD8 T cells. Eur. J. Immunol. 2018;48:1644–1662. doi: 10.1002/eji.201847771. [DOI] [PubMed] [Google Scholar]
- 69.Mackay L.K., Minnich M., Kragten N.A., Liao Y., Nota B., Seillet C., Zaid A., Man K., Preston S., Freestone D., et al. Hobit and Blimp1 instruct a universal transcriptional program of tissue residency in lymphocytes. Science. 2016;352:459–463. doi: 10.1126/science.aad2035. [DOI] [PubMed] [Google Scholar]
- 70.Wang D., Diao H., Getzler A.J., Rogal W., Frederick M.A., Milner J., Yu B., Crotty S., Goldrath A.W., Pipkin M.E. The transcription factor Runx3 establishes chromatin accessibility of cis-regulatory landscapes that drive memory cytotoxic T lymphocyte formation. Immunity. 2018;48:659–674. doi: 10.1016/j.immuni.2018.03.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Milner J.J., Toma C., Yu B., Zhang K., Omilusik K., Phan A.T., Wang D., Getzler A.J., Nguyen T., Crotty S., et al. Runx3 programs CD8+ T cell residency in non-lymphoid tissues and tumours. Nature. 2017;552:253–257. doi: 10.1038/nature24993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Schenkel J.M., Masopust D. Tissue-resident memory T cells. Immunity. 2014;41:886–897. doi: 10.1016/j.immuni.2014.12.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Wilk M.M., Mills K.H.G. CD4 TRM Cells Following Infection and Immunization: Implications for More Effective Vaccine Design. Front. Immunol. 2018;9 doi: 10.3389/fimmu.2018.01860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Park C.O., Fu X., Jiang X., Pan Y., Teague J.E., Collins N., Tian T., O’Malley J.T., Emerson R.O., Kim J.H., et al. Staged development of long-lived T-cell receptor alphabeta TH17 resident memory T-cell population to Candida albicans after skin infection. J. Allergy Clin. Immunol. 2017;142:647–662. doi: 10.1016/j.jaci.2017.09.042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Mackay L.K., Braun A., Macleod B.L., Collins N., Tebartz C., Bedoui S., Carbone F.R., Gebhardt T. Cutting Edge: CD69 interference with sphingosine-1-phosphate receptor function regulates peripheral T cell retention. J. Immunol. 2015;194:2059–2063. doi: 10.4049/jimmunol.1402256. [DOI] [PubMed] [Google Scholar]
- 76.Milner J., Goldrath A.W. Transcriptional programming of tissue-resident memory CD8+ T cells. Curr. Opin. Immunol. 2018;51:162–169. doi: 10.1016/j.coi.2018.03.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Pizzolla A., Nguyen T.H.O., Smith J.M., Brooks A.G., Kedzieska K., Heath R.W., Reading P.C., Wakim L.M. Resident memory CD8(+) T cells in the upper respiratory tract prevent pulmonary influenza virus infection. Sci. Immunol. 2017;2:eaam6970. doi: 10.1126/sciimmunol.aam6970. [DOI] [PubMed] [Google Scholar]
- 78.Zaid A., Mackay L.K., Rahimpour A., Braun A., Veldhoen M., Carbone F.R., Manton J.H., Heath W.R., Mueller S.N. Persistence of skin-resident memory T cells within an epidermal niche. Proc. Natl. Acad. Sci. USA. 2014;111:5307–5312. doi: 10.1073/pnas.1322292111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Clark R.A. Resident memory T cells in human health and disease. Sci. Transl. Med. 2015;7:269rv1. doi: 10.1126/scitranslmed.3010641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Ariotti S., Beltman J.B., Chodaczek G., Hoekstra M.E., Van Beek A.E., Gomez-Eerland R., Ritsma L., Van Rheenen J., Marée A.F., Zal T., et al. Tissue-resident memory CD8+ T cells continuously patrol skin epithelia to quickly recognize local antigen. Proc. Natl. Acad. Sci. USA. 2012;109:19739–19744. doi: 10.1073/pnas.1208927109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Gebhardt T., Wakim M., Eidsmo L., Reading P.C., Heath W.R., Carbone F.R. Memory T cells in nonlymphoid tissue that provide enhanced local immunity during infection with herpes simplex virus. Nat. Immunol. 2009;10:524–530. doi: 10.1038/ni.1718. [DOI] [PubMed] [Google Scholar]
- 82.Ariotti S., Hogenbirk M.A., Dijkgraaf F.E., Visser L.L., Hoekstra M.E., Song J.Y., Jacobs H., Haanen J.B., Schumacher T.N. T cell memory. Skin-resident memory CD8⁺ T cells trigger a state of tissue-wide pathogen alert. Science. 2014;346:101–105. doi: 10.1126/science.1254803. [DOI] [PubMed] [Google Scholar]
- 83.Khan A.A., Srivastava R., Chentoufi A.A., Kritzer E., Cgilukuri S., Garg S., Yu D.C., Vahed H., Huang H.L., Syed S.A., et al. Bolstering the numer and function of HSV-1-specific CD8(+) effector memory T cells and tissue-resident memory T cells in latently infected trigeminal ganglia reduces recurrent ocular herpes infection and disease. J. Immunol. 2017;199:186–203. doi: 10.4049/jimmunol.1700145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Pan Y., Kupper T.S. Metabolic reprogramming and longevity of tissue-resident memory T cells. Front. Immunol. 2018;9:1347. doi: 10.3389/fimmu.2018.01347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Owczarczyk-Saczonek A., Krajewska-Włodarczyk M., Kasprowicz-Furmańczyk M., Placek W. Immunological memory of psoriatic lesions. Int. J. Mol. Sci. 2020;21:625. doi: 10.3390/ijms21020625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Boniface K., Jacquemin C., Darrigade A.S., Dessarthe B., Martins C., Boukhedouni N., Vernisse C., Grasseau A., Thiolat D., Rambert J., et al. Vitiligo skin is imprinted with resident memory CD8 T cells expressing CXCR3. J. Investig. Dermatol. 2018;138:355–364. doi: 10.1016/j.jid.2017.08.038. [DOI] [PubMed] [Google Scholar]
- 87.Richmond J.M., Strassner J.P., Rashighi M., Garwal P.A., Garg M., Essien K.I., Pell L.S., Harris J.E. Resident Memory and Recirculating Memory T Cells Cooperate to Maintain Disease in a Mouse Model of Vitiligo. J. Investig. Dermatol. 2019;139:769–778. doi: 10.1016/j.jid.2018.10.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Honda T., Egawa G., Grabbe S., Kabashima K. Update of immune events in the Murine Contact Hypersensitivity Model: Toawrd the understanding of Allergic Contact Dermatitis. J. Investig. Dermatol. 2013;133:303–315. doi: 10.1038/jid.2012.284. [DOI] [PubMed] [Google Scholar]
- 89.Gaide O., Emerson R.O., Jiang X., Gulati N., Nizza S., Desmarais C., Robins H., Krueger J.G., Clark R.A., Kupper T.S. Common clonal origin of central and resident memory T cells following skin immunization. Nat. Med. 2015;21:647–653. doi: 10.1038/nm.3860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Sacirbegovic F., Zhu J., Liu J., Rosenberg S., Shlomchik M.J., Schlochik W.D. Identifying tissue-resident memory T cells in graft-versus-host disease. Blood. 2016;128:4544. doi: 10.1182/blood.V128.22.4544.4544. [DOI] [Google Scholar]
- 91.Badri A.M.T.A., Todd P.M., Garioch J.J., Gudgeon J.E., Stewart D.G., Goudie R.B. An immunohistological study of cutaneous lymphocytes in vitiligo. J. Pathol. 1993;170:149–155. doi: 10.1002/path.1711700209. [DOI] [PubMed] [Google Scholar]
- 92.Van den Boorn J.G., Konijnenberg D., Dellemijn T.A., Van der Veen J.P., Bos J.D., Melief C.J., Vyth-Dreese F.A., Luiten R.M. Autoimmune Destruction of Skin Melanocytes by Perilesional T Cells from Vitiligo Patients. J. Investig. Dermatol. 2009;129:2220–2232. doi: 10.1038/jid.2009.32. [DOI] [PubMed] [Google Scholar]
- 93.Essien K.I., Harris J.E. Animal models of vitiligo: Matching the model to the question. Dermatol. Sin. 2014;32:240–247. doi: 10.1016/j.dsi.2014.09.008. [DOI] [Google Scholar]
- 94.Boniface K., Seneschal J. Vitiligo as a skin memory disease: The need for early interventio with immunomodulating agents and a maintenance therapy to target resident memory T cells. Exp. Dermatol. 2019;28:656–661. doi: 10.1111/exd.13879. [DOI] [PubMed] [Google Scholar]
- 95.Rashighi M., Agarwal P., Richmond J.M., Harris T.H., Dresser K., Su M.W., Zhou Y., Deng A., Hunter C.A., Luster A.D., et al. CXCL10 is critical for the progression and maintenance of depigmentation in a mouse model of vitiligo. Sci. Transl. Med. 2014;6:223ra23. doi: 10.1126/scitranslmed.3007811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Harris J.E., Harris T.H., Weninger W., Wherry E.J., Hunter C.A., Turka L.A. A mouse model of vitiligo with focused epidermal depigmentation requires IFN-γ for autoreactive CD8+ T-cell accumulation in the skin. J. Investig. Dermatol. 2012;132:1869–1876. doi: 10.1038/jid.2011.463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Pan Y., Tian T., Park C.O., Lofftus S.Y., Mei S., Liu X., Luo C., O’Malley J.T., Gehad A., Teague J.E., et al. Survival of tissue-resident memory T cells requires exogenous lipid uptake and metabolism. Nature. 2017;543:252–256. doi: 10.1038/nature21379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Schenkel J.M., Fraser K.A., Vezys V., Masopust D. Sensing and alarm function of resident memory CD8(+) T cells. Nat. Immunol. 2013;14:509–513. doi: 10.1038/ni.2568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Gálvez-Cancino F., López E., Menares E., Díaz X., Flores C., Cáceres P., Hidalgo S., Chovar O., Alcántara-Hernández M., Borgna V., et al. Vaccination-induced skin-resident memory CD8+ T cells mediate strong protection against cutaneous melanoma. OncoImmunology. 2018;7:e1442163. doi: 10.1080/2162402X.2018.1442163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Corgnac S., Boutet M., Kfoury M., Naltet C., Mami-Chouaib F. The emerging role of CD8(+) tissue resident memory T (TRM) cells in antitumor immunity: A unique functional contribution of the CD103 integrin. Front. Immunol. 2018;9:1904. doi: 10.3389/fimmu.2018.01904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Webb J.R., Milne K., Watson P., DeLeeuw R.J., Nelson B.H. Tumor-Infiltrating Lymphocytes Expressing the Tissue Resident Memory Marker CD103 Are Associated with Increased Survival in High-Grade Serous Ovarian Cancer. Clin. Cancer Res. 2013;20:434–444. doi: 10.1158/1078-0432.CCR-13-1877. [DOI] [PubMed] [Google Scholar]
- 102.Wang Z.-Q., Milne K., Derocher H., Webb J.R., Nelson B.H., Watson P.H. CD103 and Intratumoral Immune Response in Breast Cancer. Clin. Cancer Res. 2016;22:6290–6297. doi: 10.1158/1078-0432.CCR-16-0732. [DOI] [PubMed] [Google Scholar]
- 103.Enamorado M., Iborra S., Priego E., Cueto F.J., Quintana J.A., Martínez-Cano S., Mejías-Pérez E., Esteban M., Melero I., Hidalgo A., et al. Enhanced anti-tumour immunity requires the interplay between resident and circulating memory CD8+ T cells. Nat. Commun. 2017;8:16073. doi: 10.1038/ncomms16073. [DOI] [PMC free article] [PubMed] [Google Scholar]