Abstract
The COVID-19 pandemic has greatly impacted the daily clinical practice of cardiologists and cardiovascular surgeons. Preparedness of health workers and health services is crucial to tackle the enormous challenge posed by SARS-CoV-2 in wards, operating theatres, intensive care units, and interventionist laboratories. This Clinical Review provides an overview of COVID-19 and focuses on relevant aspects on prevention and management for specialists within the cardiovascular field.
Keywords: COVID-19, Coronavirus, Prevention, Treatment, Prognosis, Risk factors
Introduction and scope of the review
Case study 1: A 59-year-old male underwent cardiac surgery for complicated prosthetic valve endocarditis on 13 March. The following day, the referral hospital notified that the patient had been in contact for 24 h with a confirmed case of a COVID-19. A nasopharyngeal swab confirmed SARS-CoV-2 infection. The patient developed bilateral pneumonia with ARDS and died on March 20. The contact tracing revealed the patient had been in contact with 25 healthcare workers, one having become infected.
Takeaway: During the initial phases of the pandemic, while SARS-CoV-2 is actively circulating within the community and the healthcare system, systematic screening systematic screening for SARS-CoV-2 infection should be done in all transferred patients to avoid nosocomial transmission.
COVID-19 is an illness caused by a novel coronavirus initially called 2019-nCoV and currently named SARS-CoV-2. From December 2019 to date, COVID-19 has attained a global dimension, having been declared a pandemic by the World Health Organization (WHO) on 11 March 2020.1 The outbreak started in the Chinese city of Wuhan, Hubei Province, allegedly in the Central Market, and rapidly spread. On 30 January the WHO declared the COVID-19 outbreak a global health emergency.1 To date (May 5), >3.5 million SARS-CoV-2 infections and 250 000 deaths have been reported worldwide.2 The pandemic has obliged many countries to enforce strict control measures. They include home quarantines, lockdowns, or severe limitations of air and road transport, telework, and others, which have a deep impact on the global economy and people’s daily life and well-being. Moreover, COVID-19 has led to a large overload of health systems, especially at the hospital level, and has forced health authorities and healthcare professionals to rapidly adapt to a challenging and constantly changing situation. In some countries, hospitals have turned into virtually solely COVID-19 centres. A new disease far from being completely understood has totally challenged our institutions and put the function of cardiovascular services at stake.
In this Clinical Review, we aim to provide a comprehensive summary of the most relevant characteristics of SARS-COV-2 and COVID-19, as well as the specifics that cardiologists and cardiac surgeons must know in order to tackle prevention and treatment issues involving their patients exposed to SARS-CoV-2.
Current epidemiology
As of today, the pandemic has undergone three main phases in terms of geographical scope. From late December 2019 to mid-late February, the main focus was Asia, with China having the highest concentration of outbreaks, followed by South Korea. After applying severe containment measures, the dissemination has been controlled in these countries and the second phase, still ongoing, affected European countries from mid-February, Italy foremost followed by Spain. The third phase started in mid-March and is characterized by a pronounced increase in cases in the USA.2–5
Table 1 summarizes COVID-19 statistics in most affected European countries as of 4 May 2020.
Table 1.
Summary of the epidemiology of COVID-19 in the top 10 European countries
| Country | No. of cases | No. of deaths | No. of patients recovered | Estimated cumulative incidence (non-standardized rate per 100 000 inhabitants) | Reported mortality (%) | Estimated total population infected [mean (95% CI)]5 |
|---|---|---|---|---|---|---|
| Spain | 217 466 | 25 264 | 118 902 | 465.1 | 11.6 | 15% (3.7–41%) |
| Italy | 210 717 | 28 884 | 81 654 | 348.5 | 13.7 | 9.8% (3.2–26%) |
| UK | 187 842 | 28 446 | 902 | 276.7 | 15.1 | 2.7% (1.2–5.4%) |
| France | 168 925 | 24 864 | 50 885 | 258.8 | 14.7 | 3.0% (1.1–7.4%) |
| Germany | 165 745 | 6866 | 132 700 | 197.8 | 4.1 | 0.72% (0.28–1.8%) |
| Belgium | 50 267 | 7924 | 12 378 | 433.7 | 15.8 | 3.2% (1.3–7.6%) |
| Netherlands | 40 968 | 5082 | 322 | 239.1 | 12.4 | 3.7% (1.3–9.7%) |
| Switzerland | 29 981 | 1762 | 24 500 | 346.4 | 5.9 | – |
| Portugal | 25 524 | 1063 | 1712 | 250.3 | 4.2 | 1.1% (0.36–3.1%) |
| Ireland | 21 506 | 1303 | 13 386 | 435.5 | 6.0 | – |
| Total | 1 118 941 | 131 458 | 321 507 | – | 11.7 | – |
Incidence estimates are calculated based on current population data from each country (https://www.worldometers.info/world-population/population-by-country/) relying on data extracted from Johns Hopkins University Coronavirus Resource Center.2https://coronavirus.jhu.edu/map.html
Data in the last column (mathematical estimates) come from the Imperial College report5 issued on 30 March 2020. https://www.imperial.ac.uk/media/imperial-college/medicine/sph/ide/gida-fellowships/Imperial-College-COVID19-Europe-estimates-and-NPI-impact-30-03-2020.pdf
To calculate the approximate incidence in each country, the 2020 population by country was found on the Worldometer webpage: https://www.worldometers.info/world-population/population-by-country/
As regards baseline epidemiological characteristics, in China COVID-19 affected mostly people aged 30–79 years (87%), whereas cases over 80 years and below 19 years were relatively rare (3% and 2%, respectively).6 Mean age ranges from 47 to 56 years in the largest reports, men are more likely to present COVID-19 (∼65% of cases), ∼15% of cases occur in smokers, and 25–30% of patients present concomitant diseases, with up to 40% of these being cardiovascular diseases, of which remarkably hypertension makes up 15–30%.7–9 A recent meta-analysis found that hypertension, cardio-cerebrovascular disease, and diabetes in patients with COVID-19 were present in 17.1, 16.4, and 9.7%, respectively.10 Healthcare workers are a group at risk, with prevalence varying according to the setting, e.g. they represent 3.8% of infected individuals in China6 and 15.5% in Spain.11
The virus and pathogenesis
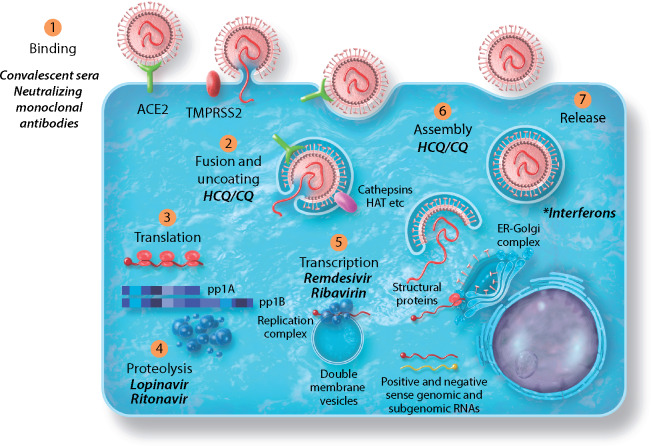
Coronaviruses are found in a variety of birds and mammals throughout the world and have a proclivity for emergence. In the past 20 years, three novel human coronaviruses have emerged, first SARS-CoV in 2002, Middle East respiratory syndrome (MERS)-CoV in 2012, and the causative agent of COVID-19, SARS-CoV-2, in 2019, and all three are believed to have originated in bats.12–14 SARS-CoV-2 is a beta-b coronavirus genetically related to but distinct from SARS-CoV.15 To gain entry into the host cell, the SARS-CoV-2 S glycoprotein binds the cellular receptor angiotensin-converting enzyme 2 (ACE2), which is also the receptor for the original SARS-CoV.13Figure 1 shows the life cycle of SARS-CoV-2.
Figure 1.
Life cycle of SARS-CoV-2 and potential medical countermeasures. The positive-sense RNA genome of SARS-CoV2 is encapsulated in a viral envelope studded with four viral structural proteins: spike (S), envelope (E), membrane (M), and nucleocapsid (N). SARS-CoV-2 gains entry into the host cell via binding of the S protein to the cellular receptor angiotensin-converting enzyme 2 (ACE2). Spike glycoprotein rearrangement that primes fusion of viral and host membranes is driven by host proteases (TMPRSS2, cathepsins, HAT, furin, etc.), after which the genome is deposited into the cytoplasm and translation of ORF1a/b ensues. The polyproteins generated from ORF1a/b are cleaved by viral proteases liberating 16 non-structural proteins that guide virus replication. The replication complex is formed on double membrane vesicles, creating both genome-length RNA as well as subgenomic RNAs that encode structure genes S, E, M, and N as well as accessory ORFs that probably play roles in modulating the host response. New virus particles are assembled on membranes derived from the ER–Golgi complex and then transported out of the cell via the secretory pathway. Medical countermeasures are shown in italics adjacent to the viral function they are thought to attack. Convalescent sera and neutralizing monoclonal antibodies should inhibit virus binding to ACE2 and entry. Chloroquine is thought to interrupt entry and/or egress. Protease inhibitors such as lopinavir/ritonavir are thought to prevent polyprotein proteolysis. Nucleoside analogues such as remdesivir and ribavirin are thought to prevent viral RNA synthesis. *Interferons induce the expression of antiviral and immunomodulatory genes that could affect multiple aspects of the virus replication cycle HCQ/CQ, hydroxychloroquine/chloroquine.
SARS-CoV (basic reproduction number-R0 1.8–2.5), MERS-CoV, and SARS-CoV-2 (R0 2.4–3.8) are primarily transmitted by the respiratory route on large droplet nuclei, close contact with infected people, or fomites. The main form of SARS-CoV-2 transmission is person to person through respiratory droplets in the air (reaching up to 2 m) and landing on surfaces, which can transmit the virus even after several days.16,17 SARS-CoV-2 is the most infectious of the three, with each case causing an estimated 2–4 new cases, whereas the R0 of influenza virus varies according to the season from 1.2 to 2.14 Pre-symptomatic and first symptomatic days correlate with a higher viral load, which has been proved to entail a higher risk of transmission.18
The virus targets cells lining the respiratory epithelium, causing a range of symptomology from asymptomatic infection to severe end-stage lung disease requiring mechanical ventilation as for ARDS.14 Disease severity is likely to be a combination of direct virus-induced pathology and the host inflammatory response to infection. In brief, two mechanisms have been proposed for lung injury leading to ARDS during coronavirus infections in humans. First, ACE2 not only acts as mediator of coronavirus entry into the cells, but also contributes to diffuse alveolar damage through imbalances in the renin–angiotensin system due to its down-regulation, activated by the S protein. Secondly, some coronavirus proteins are strong inducers of apoptosis of cell lines derived from different organs, primarily the lungs.19
Alveolar macrophages also play an important role, since their activation underlies the cytokine storm phenomenon: a massive release of macrophage migration inhibitory factor (MIF), tumour necrosis factor (TNF)-α, and interleukin (IL)-1, IL-2R, IL-6, IL-8, and IL-10, attracting neutrophils that will release leukotrienes, oxidants, and proteases, which will lead to the typical ARDS pathology with acute diffuse alveolar damage, pulmonary oedema, and formation of hyaline membranes.
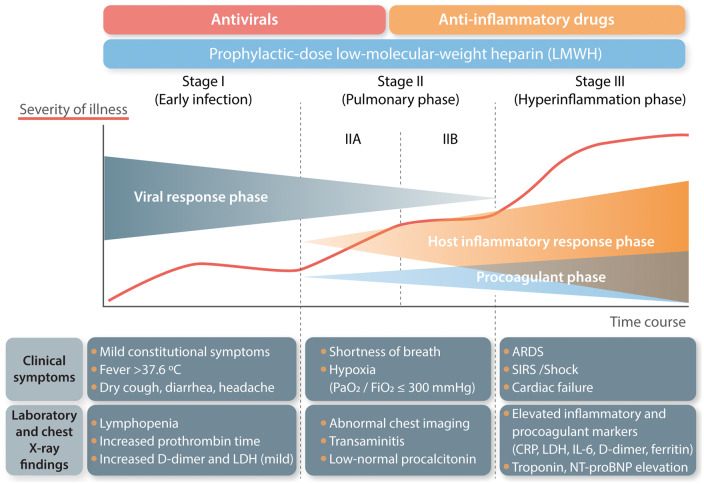
In summary, there are two phases in SARS-CoV-2 infection: during early infection (up to 7–10 days), viral syndrome predominates with a high viral load in the upper and lower respiratory tract; in a second phase, viral pneumonia can develop; and finally the viral infection can trigger the host inflammatory and procoagulant responses with SIRS, ARDS, shock, and cardiac failure (see Figure 2).
Figure 2.
Clinical stages of COVID-19 (adapted with permission from Siddiqu and Mehra125). During the first days from disease onset, patients typically present a first phase with symptoms resembling an upper respiratory tract viral infection, mostly characterized by fever and coughing. Over days 8–12 there is a transition to an inflammatory phase during which pulmonary symptoms such as shortness of breath might appear. In those patients progressing to the hyperinflammatory phase with relevant lung involvement, the risk of ARDS is notable. In addition, during this late phase, patients are at higher risk of suffering thrombotic and embolic events due to a procoagulant state. ARDS, acute respiratory distress syndrome; CRP, C-reactive protein; IL-1, interleukin 1; IL-6, interleukin 6; LDH, lactate dehydrogenase; NT-pro-BNP, natriuretic pro-brain natriuretic peptide; SIRS, systemic inflammatory response syndrome.
Pro-inflammatory and pro-coagulant states as triggers of cardiovascular events
ACE2 receptors are also located in the heart, kidney, brain, and gut, and therefore COVID-19 might cause a plethora of extrapulmonary manifestations, including cardiovascular ones.20 In the case of heart injury, preliminary data indicate that pericytes with high expression of ACE2 might act as the target cardiac cell of SARS-CoV-2 and, once damaged, capillary endothelial cell dysfunction arises, inducing microvascular dysfunction.21,22 In addition to the immune pathway, leading to increased endothelial dysfunction, itself leading to ischaemic or arrhythmic events as a consequence of a pro-inflammatory cascade, SARS-CoV-2 induces coagulation disorders that might also decompensate pre-existing cardiovascular diseases.23 In brief, systemic hyperinflammatory response, coagulation disorders involving pro-thrombotic states, microvascular injury, stress cardiomyopathy, myocardial injury secondary to oxygen supply–demand mismatch, and acute coronary syndromes triggered by plaque instability are major pathways for cardiovascular events in COVID-19 patients.21–30 Moreover, social distancing and social isolation as preventive measures also seem to increase cardiovascular risk.22
Clinical manifestations
The most common symptoms of COVID-19 are fever and dry cough, together with shortness of breath (Table 2). More recently, anosmia, hyposmia, and dysgeusia have also been described as largely characteristic during the initial phase of COVID-19.31 Meanwhile, digestive symptoms can also be found. Common blood test parameters include lymphocytopenia, increased IL-6, C-reactive protein (CRP), lactate dehydrogenase (LDH), D-dimer, ferritin, transaminases, high-sensitivity troponin, and N-terminal pro-brain natriuretic peptide (NT-pro-BNP). Meanwhile, procalcitonin levels are usually very low, which helps to differentiate COVID-19 from acute bacterial infection. It should be noted that these parameters evolve dynamically throughout the course of the disease: for instance, white blood cell count often progresses from normal total counts with lymphocytopenia to leukopenia in severe cases. Moreover, the neutrophil–lymphocyte ratio appears to be associated with illness severity.32
Table 2.
Summary of clinical and imaging manifestations of COVID-19
| Study | Country | Sample size | Signs and symptoms, median incubation period (MIC) | Radiological findings | Complications |
|---|---|---|---|---|---|
| Wu and McGoogan6 | China | 72 314 (62% confirmed) |
|
– |
|
| Guan et al.7 | China | 1099 |
|
|
|
| Zhang et al.56 | China | 645 | Patients with pneumonia presented higher rates of fever, cough, expectoration, and headache, lower lymphocytes, albumin, serum sodium levels, and higher total bilirubin, creatine kinase, lactate dehydrogenase, and C-reactive protein levels, and lower oxygenation index |
|
|
| Zhou et al.13 | China | 191 | MIC 11 days (8–14)Fever 94%, cough 79%, sputum 23%, fatigue 23%, myalgia 15%, diarrhoea 5%, nausea, and vomiting 4%.Elevated LDH 67%, lymphocytopenia 40%, elevated ferritin 80%, elevated D-dimer 42%, elevated ALT 31%. |
|
|
| Wu et al.35 | China | 201 (all with pneumonia) | Fever 93.5%, cough 81.1%, dyspnoea 39.8%, and fatigue or myalgia 32.3% | Bilateral infiltrates 95%, unilateral infiltrates 5% |
|
| Wang et al.14 | China | 138 |
|
Bilateral patchy shadows or ground-glass opacity in all patients |
|
| Chen et al.8 | China | 99 (all with pneumonia) | Fever 83%, cough (82%, shortness of breath 31%, muscle ache 11%, confusion 9%, headache 8%, sore throat 5%, rhinorrhoea 4%, chest pain 2%, diarrhoea 2%, nausea and vomiting 1%. | Bilateral pneumonia 75%, unilateral pneumonia 25%, multiple mottling and ground-glass opacity 14%, pneumothorax 1%. |
|
| Spiteri et al.94 | WHO European region | 38 |
|
Pneumonia 11.8% |
|
| Korea Centers for Disease Control and Prevention95 | Korea | 28 |
|
Pneumonia 64.3% | LOS: 12.7 days (8–19) |
| Arentz et al.96 | USA | 21 (all in ICU) | Shortness of breath 76.2%, fever 52.4%, cough 47.6% | Bilateral reticular nodular opacities 52.4%, ground-glass opacities 47.6%, pleural effusion 28.6%, focal consolidation 19%, pulmonary oedema 9.5%, venous congestion 4.8%, atelectasis 4.8%, normal 4.8%. |
|
ARDS, acute respiratory distress syndrome; ECMO, extracorporeal membrane oxygenation; ICU, intensive care unit; IMV, invasive mechanical ventilation; LDH, lactate dehydrogenase; LOS, length of stay.
Radiological manifestations range from normal chest X-ray or CT scan in ∼10% of cases to lung fibrosis.33 More commonly, COVID-19 presents as pneumonia (bilateral in around half of the cases) with reticular nodular or ground-glass opacities.
Approximately 5–10% of patients require admission to the intensive care unit (ICU) and mechanical ventilation.34 Among patients with pneumonia, ICU admission is required in 23–26% of cases and ARDS develops in 16–42% of them.8,9,14,35 Shock has been described in up to 20% of cases,9 but most series range between 1% and 8%.
Figure 2 shows the different stages within COVID-19 natural history and their correlation with pathophysiology. Onset of pulmonary symptoms occurs at the transition from a viral phase characterized by high viral load and relatively low inflammation to a host inflammatory response phase characterized by increasing inflammation and coagulation disorders. Typically, complications appear around days 10–12 after initial symptoms, often related to the triggering of an inflammatory cascade leading to the ‘cytokine storm’.36
Cardiovascular manifestations
Table 3 shows a summary of the cardiovascular manifestations and complications related to COVID-19, as well as the guidance launched by scientific societies for their prevention and management. Although empirical data are lacking and the prevalence of cardiovascular events during and after COVID-19 has still not been described yet, it appears that cardiovascular events, especially myocarditis, are relatively common.37–44
Table 3.
Cardiovascular manifestations in COVID-19
| Study | Type of study | Country | Main findings |
|---|---|---|---|
| Original studies and case reports | |||
| Shi et al.54 | Prospective cohort | China | 82/416 (19.7%) patients presented cardiac injury. |
| Deng et al.37 | Retrospective study of 112 patients with COVID-19 | China | 14 (12.5%) presented abnormalities similar to myocarditis, but without typical signs on echocardiography and electrocardiogram. |
| Gao et al.38 | Retrospective, observational registry of 102 patients with severe COVID-19, only 54 of whom entered the analysis (NCT04292964) | China | Patients with high NT-pro-BNP values (>88.64 pg/mL) had a significantly increased risk of death during follow-up |
| Bangalore et al.39 | Cases series of 18 patients | USA | 18 patients with COVID-19 presenting with ST-segment elevation, 10 of whom had non-coronary myocardial injury |
| Sala et al.40 | Case report | Italy | Acute myocarditis presenting as a reverse Tako-Tsubo syndrome |
| Dong et al.41 | Series of four cases | China | Four patients with prior cardiovascular (CV) disease developed end-stage heart failure during COVID-19 (2 of them died). |
| Zeng et al.42 | Case report | China | Fulminant myocarditis |
| Kim et al.43 | Case report | China | Myocarditis in a 21-year-old patient |
| Zhang et al.44 | Series of three cases | China | Coagulopathy and antiphospholipid antibodies |
| Reviews and perspectives | |||
| Xiong et al.24 | Narrative review | China, UK | Coronaviruses, including SARS and MERS, have short- and long-term implications for the CV system. Patients presenting with CV manifestations seem to more frequently require ICU admission. |
| Madjid et al.25 | Narrative review | USA | Acute cardiac injury determined by elevated high-sensitivity troponin levels is commonly observed in severe cases and is strongly associated with mortality |
| Driggin et al.26 | Narrative review | USA | Patients with CV comorbidities more frequently require ICU admission. COVID-19 can lead to exacerbation of previous CV disease or to specific complications such as myocardial injury, myocarditis, and acute coronary syndromes, cardiogenic shock, or arrhythmia. |
| Liu et al.27 | Narrative review | USA | The CV system is commonly involved in early phases of COVID-19. Microangiopathy and thrombosis seem to be the main mechanisms of cardiac injury. Levels of hsTrP and NPs are prognostic. |
| Kochi et al.28 | Narrative review | Italy and Switzerland | Close monitoring of potential arrhythmogenic effects of both COVID-19 itself and antiviral medication is advisable, especially in patients with previous CV disease. |
| Libby29 | Short review and perspective | USA | There are likely to be multiple pathophysiological pathways involved in cardiac injury during COVID-19, which call for precaution in deciding therapeutic approaches until more robust evidence is available |
| Guidance | |||
| Edelson et al.97 | Guidelines | USA | Interim guidance for basic and advanced life support |
| Han et al.89 | Experts consensus | China | Clinical management of patients with severe emergent CV diseases |
| Welt et al.90 | Consensus statement | USA | Catheterization laboratory considerations |
| Romaguera et al.88 | Consensus statement | Spain | Considerations on the invasive management of ischaemic and structural heart disease during the COVID-19 coronavirus outbreak |
| Hunt et al.98 | Living guidance (updated weekly) | UK | Prevention of thrombosis and management of coagulopathy and disseminated intravascular coagulation of patients infected with COVID-19 |
| Zhai et al.99 | Consensus statement | China | Prevention and treatment of venous thromboembolism associated to COVID-19 |
| Zhai et al.88 | Consensus statement | China | Prevention and treatment of venous thrombo-embolism |
| Wood et al.93 | Summary of guidance from professional societies (North American Society Leadership) | USA | Safe reintroduction of cardiovascular services |
| European Society of Cardiology | Special section on website | Europe | https://www.escardio.org/Education/COVID-19-and-Cardiology |
| American Heart Association | Special section on website | USA | https://www.heart.org/en/coronavirus |
| American College of Cardiology | COVID-19 hub on website | USA | https://www.acc.org/latest-in-cardiology/features/accs-coronavirus-disease-2019-covid-19-hub |
Meanwhile, the COVID-19 pandemic seems to be associated with a decrease in consultations pertaining to cardiovascular events in non-COVID-19 patients. Studies from the USA, Italy, and Spain showed approximate reductions of 40% in ST-segment elevation myocardial infarction (STEMI) activations in cardiac catheterization laboratories and significant reductions in hospitalization rates due to acute coronary syndromes.45–47 The Italian report also described a concomitant increase in mortality rates compared with the previous year, which was not fully explained by COVID-19-related mortality, therefore raising the question of whether some patients might have died of acute coronary syndromes without seeking medical attention. Regarding cardiac arrest, data from Lombardy in Italy showed an increase of out-of-hospital cardiac arrest incidence strongly associated with the cumulative incidence of COVID-19.48 A study from Wuhan in China showed that survival of patients with COVID-19 suffering in-hospital cardiac arrest was extremely low at 30 days (2.9%).49
Finally, it should be borne in mind that acute pulmonary injury can potentially resemble pulmonary oedema, and thus differential diagnosis in patients with a prior history of heart failure is key, given the associated therapeutic implications [e.g. bilevel positive airway pressure (BiPAP) is to be avoided in COVID-19 patients]. The same is applicable to COVID-19 patients presenting with chest pain and elevated levels of troponin and to differentiating it from myocarditis.
Diagnosis
Laboratory diagnosis is a priority for clinical management and outbreak control of COVID-19. Respiratory samples have the greatest yield, but other specimens such as blood and stools can also be used; however, evidence on their efficacy is lacking.50,51 Real-time reverse-transcription polymerase chain reaction is the current gold standard.50 Detection of total antibodies, IgM and IgG, against SARS-CoV-2 in blood samples, may be non-sensitive during the first 7–14 days of disease.52 Performing combined testing strategies with PCR and antibodies increases sensitivity to 90%.51
Clinicians should consider testing for other respiratory pathogens using routine laboratory procedures if individual case management requires because both viral and bacterial co-infections can occur.53 Yet, in the context of epidemics, patients with a clinical presentation and radiological pattern that is compatible are assumed to have COVID-19, despite a negative (or unavailable) molecular or viral antigen detection test. However, clinical diagnosis should also take account of the clinical manifestations described in most series being constrained by a major population selection bias, with severe patients being more likely to be included in the studies.
Prognosis focused on cardiovascular risk factors
Older age is the most widely recognized epidemiological risk factor of mortality (Table 4). Mortality below 50 years is uncommon, but thereafter it doubles in each decade of life, going from 2% in the 50s to 16% or more in the 80s. Among comorbidities, hypertension and diabetes are also found among patients presenting poor outcomes, yet it should be noted that these both could be correlated to advanced age. Li et al. found that the percentage of patients with hypertension, cerebrovascular diseases, and diabetes was two-fold, three-fold, and two-fold higher, repspectively in patients admitted to the ICU than in patients not presenting severe or critical COVID-19, and that acute cardiac injury was also ∼13-fold higher in the former group of patients.10 Shi et al. also found a 10-fold higher mortality among patients presenting with cardiac injury in a cohort of 416 patients with COVID-19, and predictors of cardiac injury included epidemiological (older age, comorbidities), analytical (leukocytosis, CRP, procalcitonin, creatine kinase, myohaemoglobin, high-sensitivity troponin I, NT-pro-BNP, aspartate aminotansferase (AST), and creatinine], and higher radiological (multiple mottling and ground-glass opacities).54 Other studies have found that high levels of D-dimer, NT-pro-BNP, and high-sensitivity troponin I are strongly associated with acute cardiac injury and poor prognosis.38 More recently, Argulian and colleagues found that right ventricular dilation in the echocardiography is associated with an increased risk of in-hospital death in a large series of patients hospitalized with COVID-19.55
Table 4.
Summary of studies assessing prognostic factors of mortality and complications in COVID-19
| Study | Sample size | Endpoint/s | Risk factors | Protective factors |
|---|---|---|---|---|
| Zhou et al.13 | 191 | In-hospital death | Older age, higher SOFA score, and high D-dimer greater on admission | – |
| Wang et al.14 | 138 | ICU admission | Older age, comorbidities, dyspnoea | – |
| Yang et al.100 | 52, all admitted to ICU | In-hospital death | Older age, ARDS, mechanical ventilation | – |
| Zhang et al.56 | 645 | Severe/critical COVID-19 categories | Myalgia, dyspnoea, nausea and vomiting, lymphocytopenia, higher creatinine and number of lobes radiologically involved at admission | – |
| Shi et al.54 | 416 | Cardiac injury (associated with higher in-hospital death) | Older age, more comorbidities, higher leucocyte counts, higher levels of C-reactive protein, procalcitonin, CK-MB, myohaemoglobin, high-sensitivity troponin I, NT-pro-BNP, AST, and creatinine, and higher proportion of multiple mottling and ground-glass opacity | – |
| Wu et al.35 | 201 | ARDS and progression to death in patients with ARDS | ARDS: older age, high fever, comorbidities, neutrophilia, lymphocytopenia (as well as lower CD3 and CD4 T-cell counts), elevated end-organ-related indices (e.g. AST, urea, LDH), elevated inflammation-related indices (high-sensitivity C-reactive protein and serum ferritin), and elevated coagulation function-related indicators (prothrombin time and D-dimer).Death in ARDS: older age, lower proportion of high fever, hypertension, neutrophilia, elevated bilirubin, urea, LDH, D-dimer, cystatin C, and IL-6. | Death in ARDS: high fever, treatment with methylprednisolone and antivirals. |
| Huang et al.101 | 41 | ICU admission | Dyspnoea, neutrophilia, lymphocytopenia, enlarged prothrombin time, elevated D-dimer, transaminases, bilirubin, troponin I, IL-2, IL-7, IL-10, GSCF, IP10, MCP1, MIP1A, and TNFα, and lower albumin | High fever |
| Liu et al.102 | 78 | Clinical deterioration, and likeliness of high-level respiratory support | Older age, history of smoking, high fever, respiratory failure, low albumin, high C-reactive protein | – |
| Sun et al.103 | 600 | Progression to critical condition | Older age, lymphocytopenia, oxygen supplementation and multiple/extensive pulmonary radiographic infiltrations | – |
| Mo et al.104 | 155 | Refractory pneumonia* | Male sex, anorexia, and high fever at admission, receiving oxygen, expectorants, corticosteroids, lopinavir/ritonavir, immune enhancer (thymalfasin, immunoglobulins) | – |
| Wang et al.105 | 68 | SpO2 <90% (related to death) | Older age, comorbidities, elevated IL-6, IL-10, LDH, and C-reactive protein | – |
Defined as those cases not fulfilling all the following: (i) obvious alleviation of respiratory symptoms (e.g. cough, chest distress. and shortness of breath) after treatment; (ii) maintenance of normal body temperature for ≥3 days without the use of corticosteroids or antipyretics; (iii) improvement in radiological abnormalities on chest CT or X-ray after treatment; and (iv) a hospital stay of ≤10 days.
High fever and dyspnoea on admission, and developing respiratory insufficiency have been commonly linked to poorer outcomes, as have high levels of D-dimer, LDH, IL-6, and transaminases, and low total lymphocyte count and CD3 and CD4 T-cell counts. Bilateral lung involvement as opposed to unilateral involvement does not seem to be associated with poorer mortality in most studies, yet Zhang et al. found that multilobar involvement was significantly associated with the severe/critical COVID-19 subtype.56
COVID-19 treatment and cardiovascular drugs
Currently there are no approved therapies specific to human coronavirus, and multiple medical countermeasures including direct acting antivirals (DAAs), host-targeted antivirals, and immunomodulators are being prescribed off-label for treating COVID-19 based on past observational studies for other coronaviruses as an attempt to diminish disease severity.57 In addition, multiple therapies are currently being evaluated in randomized control trials to conclusively determine efficacy,58,59 with >300 registered trials ongoing related to COVID-19.60
Table 5 shows a summary of the drugs utilized and proposed for treating COVID-19 to date.
Table 5.
Overview of drugs used for COVID-19 treatment
| Drug name | Drug family/mechanism of action | Recommended doses and length of therapy in adults | Potential secondary effects | Main potential interactions with cardiovascular drugs | References |
|---|---|---|---|---|---|
| Chloroquine/hydroxychloroquine* | Antimalarial; unknown mechanism | Loading dose 400 mg p.o. b.i.d. first day followed by 200 mg b.i.d. (5–14 days) | Ocular disturbances, reversible after early discontinuation; anorexia, weight loss, nausea, diarrhoea; elevation of liver enzymes; hypoglycaemia; hearing loss. QTc prolongation. | Amiodarone, flecainide, and other anti-arrhytmics; direct inhibitors of factor Xa; potential mild interaction with some beta-blockers (propranolol, nebivolol, metoprolol, timolol) and verapamil. | 106 –111 A recent statement by the International Society of Antimicrobial Chemotherapy111 expressed concern regarding the inclusion criteria of the study of Gautret et al.110 |
| Azithromycin (combined with hydroxychloroquine) | Macrolyde; unknown mechanism | Loading dose 500 mg p.o. the first day followed by 250 mg p.o. 4 days (5 days) | Diarrhoea, loose stools, nausea, abdominal pain, vomiting; QTc prolongation. | Digoxin, coumarins | 110 |
| Lopinavir/ritonavir | HIV protease inhibitors | 400/100 mg p.o. b.i.d. Individualized duration (maximum 14 days) | Frequent: diarrhoea, nausea, vomiting, altered lipid profile; uncommon: pancreatitis, QTc prolongation | Potent P450 inhibitor. Anti-arrhythmics, antiplatelet, anticoagulants, and other (some statins, eplerenone, aliskiren, ivabradine, sildenafil, calcium channel blockers, beta-blockers, digoxin, doxazosin, dinitrate isosorbide, etc.) | 64 , 112 , 113 |
| Remdesivir | Non-nucleoside analogue. Interferes with viral RNA polymerization. | Loading dose 200 mg i.v. the first day and 100 mg/day from day 2 to 10 | Hypotension during infusion; gastrointestinal (nausea, vomiting, diarrhoea, constipation, abdominal pain) | Carbamazepine, phenobarbital, rifampin and other P450 inducers can decrease remdesivir levels. Caution in concomitant use with vasopressors and inotropes due to the added haemodynamic effects. | 113–116 Recent FDA approval65 based on interim analyses of the NIH-sponsored ACTT trial66 and the SIMPLE trial (Gilead)67 |
| Tocilizumab† | IL-6 inhibitor | ≥80 kg body weight: two doses of 600 mg i.v. separated 12 h of from each other<80 kg body weight: 600 mg i.v. followed by 400 mg i.v. 12 h laterExceptionally, a third dose could be administered 16–24 h later | Upper respiratory tract infections, rhinopharyngitis, headache, hypertension, and elevation of transaminases | Potential mild interactions with amiodarone, quinidine, some anticoagulants, and antiplatelets | 71 , 72 , 117 |
| Sarilumab | IL-6 inhibitor | Single dose of 200–400 mg i.v. | Neutropenia, elevated transaminases, point of injection erythema, upper respiratory tract and urinary infections | Similar to tocilizumab | 118 |
| β-Interferon 1B | Immune modulator | 250 mg s.c. every 48 h for 14 days | Fever, headache, myastenia, rash, nausea, diarrhoea, lymphocytopenia, weakness, flu-like syndrome | Theophylline and oral anticoagulants | 113 , 117 , 118 NCT02845843 (in combination with lopinavir/ritonavir) |
| α-Interferon 2B | Immune modulator | 5 million units, inhaled, b.i.d. for 5–7 days | Similar to β-IFN | Theophylline and oral anticoagulants | 117 , 118 ChiCTR2000029308 |
| Ribavirin (in combination with IFN-α or lopinavir/ritonavir) | Synthetic nucleoside antiviral | 500 mg i.v. b.i.d. or t.i.d.; up to 10 days | Gastrointestinal, mood disorders, skin rash, severe anaemia | Digoxin, dicumarinics | 117 , 118 |
| Other drugs and interventions under evaluation (not enough evidence for their recommendation) | |||||
| Colchicine | Anti-inflammatory activity | 0.5 mg b.i.d. | Nausea, diarrhoea, myalgia, tachycardia | Statins, diltiazem, aspirin | 118 NCT04322682, NCT04326790, NCT04322565 |
| Convalescent patient serum | IgG binding antibodies against SARS-CoV-2 from donors recovered from COVID-19 | Administered in five patients 10–22 days after admission | 119 , 120 Used in patients with ARDS | ||
| Angiotensin receptor blockers (e.g. losartan) | Up-regulation of ACE2 receptor | 81 NCT04312009 and NCT04311177 | |||
| Dipyridamole | Suppresses SARS-CoV-2 replication in vitro | 121 | |||
| Amiodarone | Alters endosomes and inhibits SARS coronavirus infection at a post-endosomal level. | 122 , 123 | |||
| Statins | Up-regulation of ACE2 receptor | 81 Potentially useful to decrease ARDS severity | |||
| Siluximab | IL-6 inhibitor | 118 SISCO study (Italy) | |||
| Eculizumab | Complement inhibitor | 118 Potentially useful to avoid ARDS by disrupting inflammatory cascade through C5 inhibition | |||
| Danoprevir/ritonavir | Hepatitis C virus protease inhibitor | 117 Three patients cured in Ninth Hospital of Nanchang, China (unpublished data) | |||
| Favipiravir | Viral polymerase inhibitor | 124 Used for treating flu and Ebola. Data available for COVID-19 from a small open label trial | |||
| Darunavir/cobicistat | HIV protease inhibitor + pharmacokinetic booster | 118 Trial ongoing in China (NCT04252274) | |||
| Arbidol (umifenovir) | Viral membrane fusion inhibitor | 118 Several trials ongoing in China | |||
| APN01 | Human recombinant ACE2 analogue | 118 Potential role on avoiding and treating ARDS | |||
| Leronlimab | Monoclonal antibody; inhibits HIV CCR5 receptors and reduces cytokine storm | 118 | |||
| Camrelizumab and timosine | Blocking antibodies | 118 ChiCTR2000029806 and NCT04268537 | |||
| Regeneron (REGN3048 and REGN 3051) | Combination of two monoclonal antibodies against the surface spike protein of SARS-CoV2 | 118 | |||
Proposed as a prophylactic agent for contacts. †Indicated in patients presenting one or more of the following criteria: (i) interstitial pneumonia with severe respiratory failure; (ii) rapid respiratory worsening that requires mechanical ventilation (either invasive or non-invasive); (iii) non-respiratory organ failure (septic shock or SOFA score >3); and (iv) severe systemic inflammatory systemic response: IL-6 >40 pg/mL and/or D-dimer >1500 mg/dL.
The drugs currently under exploration are thought to target various aspects of the virus life cycle (Figure 1). The objectives of treatment are three-fold (Figure 2): first, to administer an early antiviral treatment that will be more effective on the first 7–14 days of infection, which is when the viral load is highest in the upper and lower respiratory tract; secondly, to address the cytokine storm in order to prevent onset of ARDS and avoid the need for mechanical ventilation, which has a mortality of ∼50%; and, thirdly, to reduce the likelihood of major thrombo-embolic events.
Case study 2: A 43-year-old male with a history of non-compaction cardiomyopathy bearing an implantable cardioverter defibrillator for primary prevention of sudden cardiac death underwent cardiac transplantation on 3 March. During the post-operative period, the patient shared nursing staff with a patient who several days later tested positive for SARS-CoV-2. On 16 March, he tested positive for SARS-CoV-2, developing a moderate COVID-19 pneumonia. The contact tracing revealed 10 exposures but no secondary cases. Corticosteroids were maintained at 0.5 mg/kg and tacrolimus was stopped during the 10-day lopinavir/ritonavir therapy. Tacrolimus serum levels evolved from 20 to 15 ng/mL during the 10-day period off the drug (the patient also received hydroxychloroquine and azithromycin without significant QT prolongation). He evolved well in a general ward and was discharged.
Takeaway: Nosocomial SARS-CoV-2 infection is possible and some antiviral SARS-CoV-2 therapies have significant pharmacokinetic and pharmacodynamic (QT prolongation) interactions.
Hydroxychloroquine alone or combined with azithromycin, lopinavir/ritonavir, and remdesivir has been the most used off-label antiviral drugs. Hydroxychloroquine and chloroquine alone or combined with azithromycin may increase in hospital mortality and the risk of ventricular arrhythmia due to QT prolongation,61,62 and their use is currently not recommended outside of clinical trials.63 Lopinavir/ritonavir may also increase the QTc interval, has significant drug–drug interactions (as shown in case study 2) and side effects, and a randomized clinical trial did not show efficacy.64 Performance of an ECG is mandatory and periodic ECG monitoring should be considered in patients taking these drugs. Remdesivir was recently approved (1 May) by the US FDA for an emergency use authorization for the treatment of suspected or laboratory-confirmed COVID-19 in adults and children hospitalized with severe disease.65–67 The Liverpool web page periodically updates drug interactions with COVID-19 medications (www.covid19-druginteractions.org).68
Routine use of systemic corticosteroids is not recommended for preventing or treating ARDS in COVID-19 patients unless they are indicated for other reasons.69,70 Preliminary studies with IL-6 inhibitors (e.g. tocilizumab, see Table 5) have shown efficacy in patients with severe or critical COVID-19.71,72 The use of corticosteroids or other anti-inflammatories is recommended in the context of clinical trials. Due to the procoagulant state caused by SARS-CoV-2, subcutaneous low molecular weight heparin prophylaxis is recommended for all hospitalized patients if there is no contraindication.73 Weight-adjusted intermediate doses of heparin are recommended in patients with risk factors for venous thrombo-embolism, and patients with thrombo-embolic disease must be fully anticoagulated.73
Given the initial evidence pointing to a higher mortality in patients with hypertension,9,35 there has been a discussion, mainly generated through the media, regarding the necessity of avoiding the use of ACE inhibitors and angiotensin receptor blockers (ARBs) to increase the risk of infection and the severity of COVID-19. However, available evidence indicates that neither likelihood of contracting COVID-19 nor mortality is increased in patients receiving those drugs.74–77 On 13 March, the Council on Hypertension of the European Society of Cardiology launched a statement strongly recommending that physicians and patients should continue treatment with their usual antihypertensive therapy.78 More recently, a special Task Force within the European Society of Hypertension critically reviewed the available evidence and came to the conclusion that it does not support a deleterious effect of renin–angiotensin blockers in COVID-19, observing increased lower respiratory tract infections and lung injury.79 Moreover, Zhang et al. recently reported a significantly lower mortality rate among patients with hypertension receiving ACE inhibitors or ARBs during admission compared with other patients with hypertension hospitalized due to COVID-19.80 Based on the knowledge of SARS-CoV-2 pathogenicity traits, some authors advocate conducting studies to test the efficacy of both ARBs and statins to treat severe COVID-19, arguing that up-regulated ACE2 receptor activity is associated with a reduced severity of ARDS.81 There are currently two trials including patients without hypertension that are testing losartan (NCT04312009 and NCT04311177).60
Finally, there are some important points to be made for cardiovascular specialists regarding the management of critically ill patients in the context of COVID-19. First, due to general hospital overload and relative lack of ventilators, the avoidance of intubation in non-COVID-19 patients becomes even more relevant than usual. Secondly, differentiating patients with acute lung injury due to COVID-19 from patients with acute pulmonary oedema due to heart failure is crucial, since BiPAP should be avoided in the former. Thirdly, high-flow nasal cannula oxygen should be used in an effort to minimize alveolar injury prior to proceeding with intubation. Finally, where oro-tracheal intubation and mechanical ventilation are required, protective ventilation with relatively high pressures at the end of the expiratory period and low volumes is recommended.34,69
Prevention adapted to Cardiology and Cardiovascular Surgery
Once a first imported case of COVID-19 is confirmed and isolated, the potential for further exponential disease spread within the hospital and region is possible. Containment measures by tracking of contacts and quarantine are necessary to mitigate the risk of losing track of potentially infected individuals.82 Increasing prevention practices in the hospital needs to be supported to a scale that initially may seem draconian to employees and healthcare providers. The risk of internal disease spread puts not only patients at risk, but also co-workers and their families, and ultimately the whole of society.
Facemasks should be used by all infected patients to avoid transmission. Therefore, isolation of suspected or confirmed contagious individuals is mandatory in any instance within the hospital with the physical ability to avoid propagation of the virus. Healthcare personnel need to adopt appropriate protective measures and avoid cross-contamination to other patients or co-workers. In this regard, preventive measures may continue to escalate within the hospital, for example to conventional surgical masks for non-suspicious personnel and patients, cancellation of face-to-face meetings, and so on.82 Furthermore, surfaces (fomites) must be disinfected, and therefore frequent hand washing with soap and water is mandatory.
Full personal protection equipment (PPE) should be used following established protocols after appropriate training. PPE for healthcare professionals involved in the direct care of COVID-19 patients include the following elements: FFP3 respirators (filtering at least 99% of airborne particles)—FFP2 and N95 respirators (filtering 94% and 95% of particles, respectively) can be used if FFP3 are not available—fluid-resistant surgical masks (type IIR) provide barrier protection against droplets; goggles, full face shield, or visor, or polycarbonate safety spectacles for eye and face protection; gowns should be long sleeved and disposable; gloves; and fluid repellent.82,83
In addition to droplet and contact precautions, allocating COVID-19 (confirmed or suspected) patients in ICU cubicles with negative pressure to avoid propagation of the virus through aerosols that could reach outside the room and spread into clear areas should be pursued. In general terms, careful patient screening during urgent/emergent procedures is required, and adoption of full protection by means of meticulous donning and doffing of PPE needs to be considered along with staffing modifications. Also rescheduling of all non-urgent, elective procedures seems justified in order to avoid environmental and provider contamination. This underlines the need to develop individualized contingency plans, adapted to each cardiovascular team, and in a forward-looking way, i.e. with both the active epidemic phase and the progressive resumption of clinical and surgical activities in mind. These plans should be continuously updated. Managerial decisions and team coordination should rely on an increased use of virtual communication as opposed to face-to-face meetings. To prevent new infections involving either patients or staff, tailored triage systems largely based on telemedicine for programmed patients are of upmost importance, along with the set up of clean and dirty zones.84,85 The latter should have all the appropriate protection measures. Patients should be allocated to the latter areas where there is evidence for the reasonable suspicion of infection or contact with infected individuals. It is advisable to perform all urgent procedures in specially equipped areas on the assumption that patients are infected.
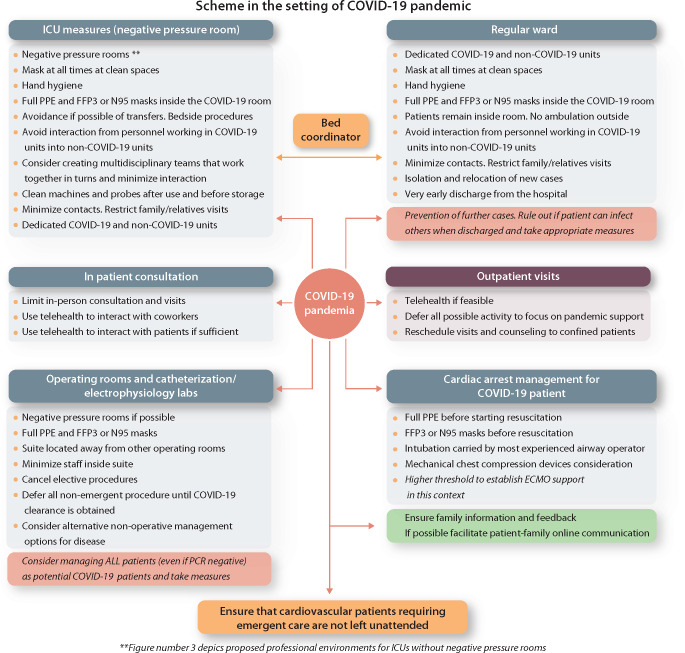
When a new case is detected within the hospital, contact tracing includes other patients, staff, and close contacts before admission in cases where there is suspicion of community acquisition rather than nosocomial. The preventive medicine service and infection control units carry out surveys to identify contacts and perform tests on them. High-risk contacts among healthcare personnel imply pre-emptive isolation. Figure 3 (Summarizing Illustration) shows a proposal of prevention measures in different hospital settings providing care to cardiovascular patients.
Figure 3.
Proposed scheme of prevention measures in different settings involving cardiovascular patients during the COVID-19 pandemic. ECMO, extracorporeal membrane oxygenation; PPE, personal protective equipment.
The operating room and the catheterization/electrophysiology labs
Case study 3: A 65-year-old male was admitted for a STEMI code on 11 March. An urgent angiography showed severe stenosis of the proximal left anterior descending artery, which was treated percutaneously with a drug-eluting stent in the haemodynamic laboratory. On 19 March, he developed a moderate COVID-19 pneumonia. Contact tracing revealed 20 contacts but no secondary cases in coronary and cardiology units. The patient was successfully treated and discharged to a convalescence centre 14 days later. However, the three staff members of the haemodynamic laboratory developed COVID-19.
Takeaway: When urgent screening for SARS-CoV-2 infection cannot be performed, appropriate PPE must be used. In addition, acute coronary syndrome could be indirectly related to COVID-19.
An operating room with a negative pressure setting located as far away as possible from other operating rooms, with separate access, is recommended for suspected or confirmed COVID-19 patients.86 Full PPE should be worn in compliance with current recommendations (including an N95 or FFP3 mask). If negative pressure environments are not available, the operating room doors should be kept closed to avoid airborne spreading of the virus. This applies to any interventional cardiovascular procedure. However, specific problems can be encountered in cardiac surgeries requiring surgical field magnification loupes that may compromise compliance with protective recommendations. In this scenario, other forms of myocardial revascularization may be preferable.
For catheterization suites, the conventional emergent transfer for diagnostic/therapeutic purposes has been questioned during the pandemic situation, and proposals to screen every single patient for COVID-19, regardless of delay in therapy, have been adopted by some practitioners.87,88 The consensus is that percutaneous coronary intervention (PCI) remains the first option except for cases of severe COVID-19. This strategy may apply to any non-emergent cardiac surgery. The need to individualize decisions gains relevance in this context.89,90 When in doubt, if the situation does not allow for confirmatory tests, the recommendation should be to proceed with full PPE and adopt all strategies as when dealing with a confirmed COVID-19 patient. Any other non-urgent/emergent procedure which merits full investigation and systematic screening prior to invasive procedures may ultimately be indicated to prevent some of the exposed clinical issues here.
Special considerations for management of cardiovascular emergencies in confirmed or suspected COVID-19 patients
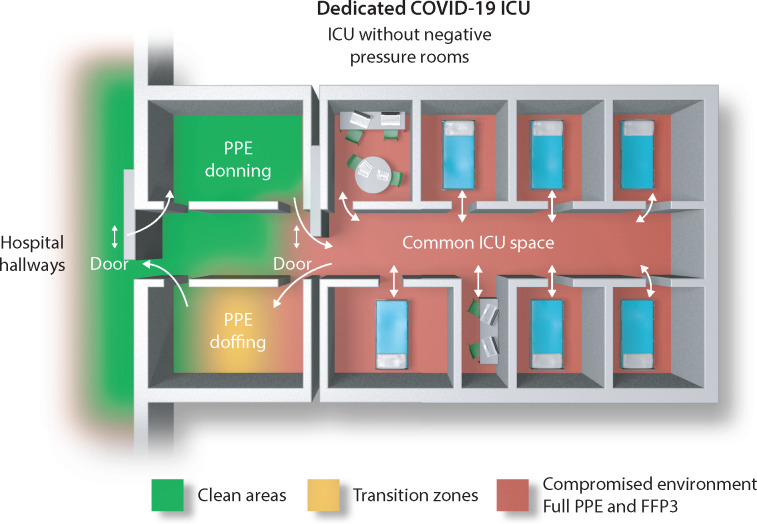
While it is crucial that prevention measures, especially in the ICU, do not compromise appropriate monitoring and timely therapeutic action, it is also of outstanding importance to avoid healthcare workers and other patients being infected due to the lack of appropriate actions taken during a cardiovascular emergency. Prevention and control of COVID-19 transmission should be adopted as the highest priority, including self-protection of medical staff.82 If possible, invasive procedures should be replaced by more conservative ones while aiming for the best possible patient outcomes. Also, minimizing transfers within the hospital is recommended, and therefore all tests and procedures should be performed at the bedside if feasible. Figure 4 shows a proposed organization of ICU areas to minimize spread of the virus among patients and staff.
Figure 4.
Proposed organization of an ICU during the COVID-19 pandemic (see text for explanation). FFP3, filtering facepiece protection 3; PPE, personal protective equipment.
During a cardiac arrest, PPE needs to be worn by all members of the resuscitation team. Prolonged facemask ventilation should be avoided to decrease the amount of aerosol generation. Consideration should be given to using automated chest compression devices to minimize contact. Intubation and chest compressions should be delayed until fully equipped personnel with PPE become ready to interact safely.89
Burdens of operability in a COVID-19 environment
The burdens of cardiac operability, procedural choice, and best resource allocation during a pandemic outbreak may remain debatable and are under investigation. A delay in emergent life-threatening conditions requiring cardiac surgery is not justified unless restrictive criteria (limitation to ICU acceptance) are applied to the entire healthcare system. Fortunately, the majority of patients with severe forms of heart disease may tolerate a delay of weeks to months under best medical treatment. Estimates of hospital occupancy and availability of resources need to be frequently revisited with the intention of reallocating these patients into the surgical schedule as soon as possible. For urgent conditions that cannot be delayed (most frequently unstable coronary disease), alternative modalities of treatment may be given priority despite different existing guideline recommendations. In the transplant arena and due to a perceived increased risk of complications in such patients, it may be justifiable to accept a ‘programme lock down’ period for elective heart transplantation.
Allocation of resources and service preservation in cardiovascular departments
Care for non-COVID-19 patients must continue despite the extreme pressures to which many European healthcare systems have been exposed. Cardiac surgery departments have a responsibility to their patients that may have been compromised, in a large number of practices, during the pandemic. This may have happened as a result of reallocation of hospital resources or due to maintaining unaltered practices in healthcare environments that were not safe, resulting in an incremental risk of surgery. Preservation of dedicated teams for highly specialized practices could make sense as long as the pandemic situation does not force the system to use all its assets. The proposed clustered or high-intensity staffing models could maintain operability throughout part of the crisis if containment measures towards the COVID-19 pandemic does not collapse the healthcare system.91 Such teams would be designed to cluster an attending physician, a cardiovascular resident or fellow, two to three nurses, and anesthesiologists. The teams would remain available and together until one member becomes infected (or under suspicion of infection). The workload would be distributed to a number of clustered teams to provide a full operative service. Maintaining certain physicians with a particular unique skill set (e.g. interventional cardiologists and cardiac surgeons) working away from the frontline services may be reasonable when the system can still compensate for their absence without imposing a downgrade of care to COVID-19 patients. In the event the system becomes overwhelmed due to a lack of manpower, such physicians should be prepared to commit the full spectrum of their skills and capabilities to mitigate the consequences of a pandemic.92
Reintroducing cardiovascular services after COVID-19
Once the peak of COVID-19 is overcome in a particular setting, the safe reintroduction of cardiovascular services requires close collaboration between public health officials and health systems. It is to be noted that different invasive procedures and diagnostic tests might be at different levels of re-escalation within a given region depending on local COVID-19 penetrance and infrastructure requirements. The process of reincorporating cardiovascular services is dynamic and the capacity to manage a potential second wave of COVID-19 should be maintained while there is still a risk of a second surge.93
Conclusions
The COVID-19 pandemic is largely and rapidly affecting daily clinical practice, and cardiologists and cardiovascular surgeons are not exempt. Being aware of and updated on how SARS-CoV-2 is transmitted, how it can be prevented, and who should be screened for infection is currently crucial for the exercise of professional duties. Also, all clinicians should be able to identify early clinical manifestations of COVID-19, including cardiovascular complications, and therapeutic options as well as potential interactions with cardiovascular drugs should be well known.
From a professional standpoint it seems wise to build a strong, straightforward, coordinated, and anticipated response during the initial phase of disease locally. Early implementation of exponential preventive measures by means of universal use of masks, minimization of personnel/patient and co-worker interaction, along with rescheduling non-urgent consultations and surgeries, may facilitate better institutional preparation for the peak caseload.
Alignment of regulatory bodies, healthcare institutions, clinical services, and individual professional initiatives in the right direction could allow avoidance of unnecessary mortality and complications related to severe forms of COVID-19 in the general population and early after cardiovascular procedures.
Author contributions
All the authors listed in the contributors’ affiliations meet the ICMJE Authorship Criteria; that is, they substantially contributed to conception and design, acquisition of data, drafting of the article, critical revision, and final approval of the manuscript.
Acknowledgements
We would like to thank all of our fellow health professionals that are giving the best of themselves to face the daunting situation generated by the ongoing COVID-19 pandemic, with a special recognition to those who lost their lives as a consequence of discharging their professional duties.
Funding
This work was supported by the Ministerio de Sanidad y Consumo of Spain (FIS NCT00871104. Instituto de Salud Carlos III). Institut d’Investigacions Biomèdiques Pi i Sunyer (IDIBAPS) provided to J.M.M. a personal 80:20 research grant during 2017–2021. A grant from the National Institute of Allergy and Infectious Diseases (NIAID, 5R01AI132178) supported T.P.S. in this endeavour.
Conflict of interest: J.M.M. has received consulting honoraria and/or research grants from Angelini, Bristol-Myers Squibb, Contrafect, Genentech, Gilead Sciences, Medtronic, MSD, Novartis, Pfizer, and ViiV. All other authors have no conflicts to declare.
Appendix. Members of the Hospital Clínic Endocarditis Study Group, Hospital Clínic-IDIBAPS, University of Barcelona School of Medicine, Barcelona, Spain
Jose M. Miró, Juan Ambrosioni, Juan M. Pericàs, Adrian Téllez, Marta Hernandez-Meneses, Delia Garcia-Pares, Asunción Moreno (Infectious Diseases Service); Cristina Garcia de la Maria, Anders Dahl, Javier Garcia-González, María-Alejandra Cañas-Pacheco (Experimental Endocarditis Laboratory); Manel Almela, Climent Casals, Francesc Marco, Jordi Vila (Microbiology Service); Eduard Quintana, Elena Sandoval, Carlos Falces, Ruth Andrea, Daniel Pereda, Manel Azqueta, Maria Angeles Castel, Ana Garcia, Marta Sitges, Marta Farrero, Barbara Vidal, Felix Pérez-Villa, José L. Pomar, Manuel Castella, José M. Tolosana, José Ortiz (Cardiovascular Institute); Guillermina Fita, Irene Rovira (Anesthesiology Department); Andrés Perissinotti, David Fuster (Nuclear Medicine Service); Jose Ramírez, (Pathology Department); Mercè Brunet (Toxicology Service); Dolors Soy (Pharmacy Service); Pedro Castro (Intensive Care Unit); and Jaume Llopis (Department of Statistics, Faculty of Biology, University of Barcelona).
Contributor Information
Hospital Clínic Cardiovascular Infections Study Group:
Jose M Miró, Juan Ambrosioni, Juan M Pericàs, Adrian Téllez, Marta Hernandez-Meneses, Delia Garcia-Pares, Asunción Moreno, Cristina Garcia de la Maria, Anders Dahl, Javier Garcia-González, María-Alejandra Cañas-Pacheco, Manel Almela, Climent Casals, Francesc Marco, Jordi Vila, Eduard Quintana, Elena Sandoval, Carlos Falces, Ruth Andrea, Daniel Pereda, Manel Azqueta, Maria Angeles Castel, Ana Garcia, Marta Sitges, Marta Farrero, Barbara Vidal, Felix Pérez-Villa, José L Pomar, Manuel Castella, José M Tolosana, José Ortiz, Guillermina Fita, Irene Rovira, Andrés Perissinotti, David Fuster, Jose Ramírez, Mercè Brunet, Dolors Soy, Pedro Castro, and Jaume Llopis
One-sentence summary: This review provides an overview and practical guidance for cardiologists and cardiovascular surgeons on the prevention, diagnosis, treatment, and prognosis of COVID-19.
References
- 1. Lauer SA, Grantz KH, Bi Q, Jones FK, Zheng Q, Meredith HR, Azman AS, Reich NG, Lessler J.. The incubation period of coronavirus disease 2019 (COVID-19) from publicly reported confirmed cases: estimation and application. Ann Intern Med 2020;172:577–582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Johns Hopkins University Coronavirus Resource Center. https://coronavirus.jhu.edu/map.html (4 May 2020).
- 3.Presidenza del Consiglio dei Ministri, Dipartimento della Protezione Civile, News (Italy) http://www.protezionecivile.gov.it/media-comunicazione/news
- 4.Catalonian Agency of Healthcare Quality and Evaluation (AQuAS). http://aquas.gencat.cat/.content/IntegradorServeis/mapa_covid/atlas.html
- 5. Flaxman S, Mishra S, Gandy A, Unwin H, Coupland H, Mellan T, Zhu H, Berah T, Eaton J, Perez Guzman P, Schmit N, Cilloni L, Ainslie K, Baguelin M, Blake I, Boonyasiri A, Boyd O, Cattarino L, Ciavarella C, Cooper L, Cucunuba Perez Z, Cuomo-Dannenburg G, Dighe A, Djaafara A, Dorigatti I, Van Elsland S, Fitzjohn R, Fu H, Gaythorpe K, Geidelberg L, Grassly N, Green W, Hallett T, Hamlet A, Hinsley W, Jeffrey B, Jorgensen D, Knock E, Laydon D, Nedjati Gilani G, Nouvellet P, Parag K, Siveroni I, Thompson H, Verity R, Vol E, Walters C, Wang H, Wang Y, Watson O, Winskill P, Xi X, Whittaker C, Walker P, Ghani A, Donnelly C, Riley S, Okell L, Vollmer M, Ferguson N, Bhatt S; Imperial College COVID-19 Response Team. Estimating the number of infections and the impact of nonpharmaceutical interventions on COVID-19 in 11 European countries. 30 March 2020. https://www.imperial.ac.uk/media/imperial-college/medicine/sph/ide/gida-fellowships/Imperial-College-COVID19-Europe-estimates-and-NPI-impact-30-03-2020.pdf
- 6. Wu Z, McGoogan JM.. Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China: summary of a report of 72314 cases from the Chinese Center for Disease Control and Prevention. JAMA 2020;doi: 10.1001/jama.2020.2648. [DOI] [PubMed] [Google Scholar]
- 7. Guan WJ, Ni ZY, Hu Y, Liang WH, Ou CQ, He JX, Liu L, Shan H, Lei CL, Hui DSC, Du B, Li LJ, Zeng G, Yuen KY, Chen RC, Tang CL, Wang T, Chen PY,, Xiang J,, Li SY, Wang JL, Liang ZJ, Peng YX, Wei L, Liu Y, Hu YH, Peng P, Wang JM, Liu JY, Chen Z, Li G, Zheng ZJ, Qiu SQ, Luo J,, Ye CJ, Zhu SY, Zhong NS; China Medical Treatment Expert Group for Covid-19. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med 2020;382:1708–1720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Chen N, Zhou M, Dong X, Qu J, Gong F, Han Y, Qiu Y, Wang J, Liu Y, Wei Y, Xia J, Yu T, Zhang X, Zhang L.. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. Lancet 2020;395:507–513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Zhou F, Yu T, Du R, Fan G, Liu Y, Liu Z, Xiang J, Wang Y, Song B, Gu X, Guan L, Wei Y, Li H, Wu X, Xu J, Tu S, Zhang Y, Chen H, Cao B.. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet 2020;395:1054–1062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Li B, Yang J, Zhao F, Zhi L, Wang X, Liu L, Bi Z, Zhao Y.. Prevalence and impact of cardiovascular metabolic diseases on COVID-19 in China. Clin Res Cardiol 2020;109:531–538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.National Epidemiology Center, Instituto de Salud Carlos III. [Seventeenth report on the situation of COVID-19 in Spain]. 27 March 2020.
- 12. de Wit E, van Doremalen N, Falzarano D, Munster VJ.. SARS and MERS: recent insights into emerging coronaviruses. Nat Rev Microbiol 2016;14:523–534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Zhou P, Yang XL, Wang XG, Hu B, Zhang L, Zhang W, Si HR, Zhu Y, Li B, Huang CL, Chen HD, Chen J, Luo Y, Guo H, Jiang RD, Liu MQ, Chen Y, Shen XR, Wang X, Zheng XS, Zhao K, Chen QJ, Deng F, Liu LL, Yan B, Zhan FX, Wang YY, Xiao GF, Shi ZL.. A pneumonia outbreak associated with a new coronavirus of probable bat origin. Nature 2020;579:270–273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Wang D, Hu B, Hu C, Zhu F, Liu X, Zhang J, Wang B, Xiang H, Cheng Z, Xiong Y, Zhao Y, Li Y, Wang X, Peng Z.. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus-infected pneumonia in Wuhan, China. JAMA 2020;doi: 10.1001/jama.2020.1585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Lu R, Zhao X, Li J, Niu P, Yang B, Wu H, Wang W, Song H, Huang B, Zhu N, Bi Y, Ma X, Zhan F, Wang L, Hu T, Zhou H, Hu Z, Zhou W, Zhao L, Chen J, Meng Y, Wang J, Lin Y, Yuan J, Xie Z, Ma J, Liu WJ, Wang D, Xu W, Holmes EC, Gao GF, Wu G, Chen W, Shi W, Tan W.. Genomic characterisation and epidemiology of 2019 novel coronavirus: implications for virus origins and receptor binding. Lancet 2020;395:565–574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. van Doremalen N, Bushmaker T, Morris DH, Holbrook MG, Gamble A, Williamson BN, Tamin A, Harcourt JL, Thornburg NJ, Gerber SI, Lloyd-Smith JO, de Wit E, Munster VJ.. Aerosol and surface stability of SARS-CoV-2 as compared with SARS-CoV-1. N Engl J Med 2020;382:1564–1567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Guo ZD, Wang ZY, Zhang SF, Li X, Li L, Li C, Cui Y, Fu RB, Dong YZ, Chi XY, Zhang MY, Liu K, Cao C, Liu B, Zhang K, Gao YW, Lu B, Chen W.. Aerosol and surface distribution of severe acute respiratory syndrome coronavirus 2 in hospital wards, Wuhan, China, 2020. Emerg Infect Dis 2020;26(7). doi: 10.3201/eid2607.200885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. He X, Lau EHY, Wu P, Deng X, Wang J, Hao X, Lau YC, Wong JY, Guan Y, Tan X, Mo X, Chen Y, Liao B, Chen W, Hu F, Zhang Q, Zhong M, Wu Y, Zhao L, Zhang F, Cowling BJ, Li F, Leung GM.. Temporal dynamics in viral shedding and transmissibility of COVID-19. Nat Med 2020;26:672–675. [DOI] [PubMed] [Google Scholar]
- 19. Hui DS, Chan PK.. Severe acute respiratory syndrome and coronavirus. Infect Dis Clin North Am 2010;24:619–638 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. South AM, Diz DI, Chappell MC.. COVID-19, ACE2, and the cardiovascular consequences. Am J Physiol Heart Circ Physiol 2020;318:H1084–H1090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Chen L, Li X, Chen M, Feng Y, Xiong C.. The ACE2 expression in human heart indicates new potential mechanism of heart injury among patients infected with SARS-CoV-2. Cardiovasc Res 2020;116:1097–1100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Guzik TJ, Mohiddin SA, Dimarco A, Patel V, Savvatis K, Marelli-Berg FM, Madhur MS, Tomaszewski M, Maffia P, D'Acquisto F, Nicklin SA, Marian AJ, Nosalski R,, Murray EC, Guzik B, Berry C, Touyz RM, Kreutz R, Wang DW, Bhella D, Sagliocco O, Crea F, Thomson EC, McInnes IB.. COVID-19 and the cardiovascular system: implications for risk assessment, diagnosis, and treatment options. Cardiovasc Res 2020;doi: 10.1093/cvr/cvaa106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Giannis D, Ziogas IA, Gianni P.. Coagulation disorders in coronavirus infected patients: COVID-19, SARS-CoV-1, MERS-CoV and lessons from the past. J Clin Virol 2020;127:104362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Xiong TY, Redwood S, Prendergast B, Chen M.. Coronaviruses and the cardiovascular system: acute and long-term implications. Eur Heart J 2020;41:1798–1800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Madjid M, Safavi-Naeini P, Solomon SD, Vardeny O.. Potential effects of coronaviruses on the cardiovascular system: a review. JAMA Cardiol 2020;doi: 10.1001/jamacardio.2020 [DOI] [PubMed] [Google Scholar]
- 26. Driggin E, Madhavan MV, Bikdeli B, Chuich T, Laracy J, Biondi-Zoccai G, Brown TS, Der Nigoghossian C, Zidar DA, Haythe J, Brodie D, Beckman JA, Kirtane AJ, Stone GW, Krumholz HM, Parikh SA.. Cardiovascular considerations for patients, health care workers, and health systems during the coronavirus disease 2019 (COVID-19) pandemic. J Am Coll Cardiol 2020;75:2352–2371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Liu PP, Blet A, Smyth D, Li H.. The science underlying COVID-19: implications for the cardiovascular system. Circulation 2020;doi: 10.1161/CIRCULATIONAHA.120.047549 [DOI] [PubMed] [Google Scholar]
- 28. Kochi AN, Tagliari AP, Forleo GB, Fassini GM, Tondo C.. Cardiac and arrhythmic complications in patients with COVID-19. J Cardiovasc Electrophysiol 2020;31:1003–1008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Libby P. The heart in COVID19: primary target or secondary bystander? JACC Basic Transl Sci 2020;doi: 10.1016/j.jacbts.2020.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Atri D, Siddiqi HK, Lang J, Nauffal V, Morrow DA, Bohula EA.. COVID-19 for the cardiologist: a current review of the virology, clinical epidemiology, cardiac and other clinical manifestations and potential therapeutic strategies. JACC Basic Transl Sci 2020;doi: 10.1016/j.jacbts.2020.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.American Academy of Otolaryngology-Head and Neck Surgery. Anosmia, hyposmia, and dysgeusia symptoms of coronavirus disease. March 22, 2020https://www.entnet.org/content/coronavirus-disease-2019-resources
- 32. Qin C, Zhou L, Hu Z, Zhang S, Yang S, Tao Y, Xie C, Ma K, Shang K, Wang W, Tian DS.. Dysregulation of immune response in patients with COVID-19 in Wuhan, China. Clin Infect Dis 2020;doi: 10.1093/cid/ciaa248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Ye Z, Zhang Y, Wang Y, Huang Z, Song B.. Chest CT manifestations of new coronavirus disease 2019 (COVID-19): a pictorial review. Eur Radiol 2020;doi: 10.1007/s00330–020–06801–0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Poston JT, Patel BK, Davis AM.. Management of critically ill adults with COVID-19. JAMA 2020;doi: 10.1001/jama.2020.4914. [DOI] [PubMed] [Google Scholar]
- 35. Wu C, Chen X, Cai Y, Xia J, Zhou X, Xu S, Huang H, Zhang L, Zhou X, Du C, Zhang Y, Song J, Wang S, Chao Y, Yang Z, Xu J, Zhou X, Chen D, Xiong W, Xu L, Zhou F, Jiang J, Bai C, Zheng J, Song Y.. Risk factors associated with acute respiratory distress syndrome and death in patients with coronavirus disease 2019 pneumonia in Wuhan, China. JAMA Intern Med 2020;doi: 10.1001/jamainternmed.2020.0994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Mehta P, McAuley DF, Brown M, Sanchez E, Tattersall RS, Manson JJ; HLH Across Speciality Collaboration, UK. COVID-19: consider cytokine storm syndromes and immunosuppression. Lancet 2020;95:1033–1034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Deng Q, Hu B, Zhang Y, Wang H, Zhou X, Hu W, Cheng Y, Yan J, Ping H, Zhou Q.. Suspected myocardial injury in patients with COVID-19: evidence from front-line clinical observation in Wuhan, China. Int J Cardiol 2020;doi: 10.1016/j.ijcard.2020.03.087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Gao L, Jiang D, Wen XS, Cheng XC, Sun M, He B, You LN, Lei P, Tan XW, Qin S, Cai GQ, Zhang DY.. Prognostic value of NT-proBNP in patients with severe COVID-19. Respir Res 2020;21:83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Bangalore S, Sharma A, Slotwiner A, Yatskar L, Harari R, Shah B, Ibrahim H, Friedman GH, Thompson C, Alviar CL, Chadow HL, Fishman GI, Reynolds HR, Keller N, Hochman JS.. ST-segment elevation in patients with Covid-19—a case series. N Engl J Med 2020;doi: 10.1056/NEJMc2009020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Sala S, Peretto G, Gramegna M, Palmisano A, Villatore A, Vignale D, De Cobelli F, Tresoldi M, Cappelletti AM, Basso C, Godino C, Esposito A.. Acute myocarditis presenting as a reverse Tako-Tsubo syndrome in a patient with SARS-CoV-2 respiratory infection. Eur Heart J 2020;41:1861–1862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Dong N, Cai J, Zhou Y, Liu J, Li F.. End-stage heart failure with COVID-19: strong evidence of myocardial injury by 2019-nCoV. JACC Heart Fail 2020;doi: 10.1016/j.jchf.2020.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Zeng JH, Liu YX, Yuan J, Wang FX, Wu WB, Li JX, Wang LF, Gao H, Wang Y, Dong CF, Li YJ,, Xie XJ, Feng C, Liu L.. First case of COVID-19 complicated with fulminant myocarditis: a case report and insights. Infection 2020;doi: 10.1007/s15010-020-01424-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Kim IC, Kim JY, Kim HA, Han S.. COVID-19-related myocarditis in a 21-year-old female patient. Eur Heart J 2020;41:1859. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Zhang Y, Xiao M, Zhang S, Xia P, Cao W, Jiang W, Chen H, Ding X, Zhao H, Zhang H, Wang C, Zhao J, Sun X, Tian R, Wu W, Wu D, Ma J, Chen Y, Zhang D, Xie J, Yan X, Zhou X, Liu Z, Wang J, Du B, Qin Y, Gao P, Qin X, Xu Y, Zhang W, Li T, Zhang F, Zhao Y, Li Y, Zhang S.. Coagulopathy and antiphospholipid antibodies in patients with Covid-19. N Engl J Med 2020;382:e38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Garcia S, Albaghdadi MS, Meraj PM,, Schmidt C, Garberich R, Jaffer FA, Dixon S, Rade JJ, Tannenbaum M, Chambers J, Huang PP, Henry TD.. Reduction in ST-segment elevation cardiac catheterization laboratory activations in the United States during COVID-19 pandemic. J Am Coll Cardiol 2020;doi: 10.1016/j.jacc.2020.04.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Rodríguez-Leor O, Cid-Álvarez B, Ojeda S, Martín-Moreiras J, Ramón Rumoroso j, López-Palop R, Serrador A, Cequier A, Romaguera R, Cruz I, Pérez de Prado A, Moreno R, on behalf of all the participants of the ACI-SEC Infarction Code Registry. Impact of the COVID-19 pandemic on interventional cardiology activity in Spain. REC Interv Cardiol 2020;2:82–89 [Google Scholar]
- 47. De Filippo O, D’Ascenzo F, Angelini F, Bocchino PP, Conrotto F, Saglietto A, Secco GG, Campo G, Gallone G, Verardi R, Gaido L, Iannaccone M, Galvani M, Ugo F, Barbero U, Infantino V, Olivotti L, Mennuni M, Gili S, Infusino F, Vercellino M, Zucchetti O, Casella G, Giammaria M, Boccuzzi G, Tolomeo P, Doronzo B, Senatore G, Grosso Marra W, Rognoni A, Trabattoni D, Franchin L, Borin A, Bruno F, Galluzzo A, Gambino A, Nicolino A, Truffa Giachet A, Sardella G, Fedele F, Monticone S, Montefusco A, Omedè P,, Pennone M, Patti G, Mancone M, De Ferrari GM.. Reduced rate of hospital admissions for ACS during Covid-19 outbreak in Northern Italy. N Engl J Med 2020;doi: 10.1056/NEJMc2009166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Baldi E, Sechi GM, Mare C, Canevari F, Brancaglione A, Primi R, Klersy C, Palo A, Contri E, Ronchi V, Beretta G, Reali F, Parogni P, Facchin F, Bua D, Rizzi U, Bussi D, Ruggeri S, Oltrona Visconti L, Savastano S; Lombardia CARe Researchers. Out-of-hospital cardiac arrest during the Covid-19 outbreak in Italy. N Engl J Med 2020;doi: 10.1056/NEJMc2010418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Shao F, Xu S, Ma X, et al. In-hospital cardiac arrest outcomes among patients with COVID-19 pneumonia in Wuhan, China. Resuscitation 2020;151:18–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.World Health Organization. Laboratory testing for 2019 novel coronavirus (2019-nCoV) in suspected human cases. 19 March 2020. https://www.who.int/publications-detail/laboratory-testing-for-2019-novel-coronavirus-in-suspected-human-cases-20200117
- 51. Wang W, Xu Y, Gao R, Lu R, Han K, Wu G, Tan W.. Detection of SARS-CoV-2 in different types of clinical specimens. JAMA 2020;323:1843–1844. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Zhao J, Yuan Q, Wang H, Liu W, Liao X, Su Y, Wang X, Yuan J, Li T, Li J, Qian S, Hong C, Wang F, Liu Y, Wang Z, He Q, Li Z, He B, Zhang T, Fu Y, Ge S, Liu L, Zhang J, Xia N, Zhang Z.. Antibody responses to SARS-CoV-2 in patients of novel coronavirus disease 2019. Clin Infect Dis 2020;doi: 10.1093/cid/ciaa344 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Ding Q, Lu P, Fan Y, Xia Y, Liu M.. The clinical characteristics of pneumonia patients co-infected with 2019 novel coronavirus and influenza virus in Wuhan, China. J Med Virol 2020;doi: 10.1002/jmv.25781 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Shi S, Qin M, Shen B, Cai Y, Liu T, Yang F, Gong W, Liu X, Liang J, Zhao Q, Huang H, Yang B, Huang C.. Association of cardiac injury with mortality in hospitalized patients with COVID-19 in Wuhan, China. JAMA Cardiol 2020;doi: 10.1001/jamacardio.2020.0950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Argulian E, Sud K, Vogel B, Bohra C, Garg VP, Talebi VP, Garg VP, Garg VP. Right Ventricular Dilation in Hospitalized Patients With COVID-19 Infection. JACC Cardiovasc Imaging 2020;doi: 10.1016/j.jcmg.2020.05.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Zhang X, Cai H, Hu J, Lian J, Gu J, Zhang S, Ye C, Lu Y, Jin C, Yu G, Jia H, Zhang Y, Sheng J, Li L, Yang Y.. Epidemiological, clinical characteristics of cases of SARS-CoV-2 infection with abnormal imaging findings. Int J Infect Dis 2020;94:81–87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Zumla A, Chan JF, Azhar EI, Hui DS, Yuen KY.. Coronaviruses—drug discovery and therapeutic options. Nat Rev Drug Discov 2016;15:327–347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Bhimraj A, Morgan RL, Shumaker AH, Lavergne V, Baden L, Chi-Chung Cheng V, Edwards KM, Gandhi R, Muller WJ, O’Horo JC, Shoham S, Murad MH, Mustafa RA, Sultan Falck-Ytter Y. Infectious Diseases Society of America Guidelines on the Treatment and Management of Patients with COVID-19. Infectious Disease Society of America, 11 April 2020. https://www.idsociety.org/practice-guideline/covid-19-guideline-treatment-and-management/ [DOI] [PMC free article] [PubMed]
- 59. Sanders JM, Monogue ML, Jodlowski TZ, Cutrell JB.. Pharmacologic treatments for coronavirus disease 2019 (COVID-19): a review. JAMA 2020;323:1824–1836. [DOI] [PubMed] [Google Scholar]
- 60.Clinicaltrials.gov. Studies found for ‘COVID-19’. https://clinicaltrials.gov/ct2/results?cond=covid-19&term=&cntry=&state=&city=&dist=
- 61. Mercuro NJ, Yen CF, Shim DJ, Maher TR, McCoy CM, Zimetbaum PJ, Gold HS.. Risk of QT interval prolongation associated with use of hydroxychloroquine with or without concomitant azithromycin among hospitalized patients testing positive for coronavirus disease2019 (COVID-19). JAMA Cardiol 2020;doi: 10.1001/jamacardio.2020.1834. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Bessière F, Roccia H, Delinière A, Charrière R, Chevalier P, Argaud L, Cour M.. Assessment of QT intervals in a case series of patients with coronavirus disease 2019 (COVID-19) infection treated with hydroxychloroquine alone or in combination with azithromycin in an intensive care unit. JAMA Cardiol 2020;doi: 10.1001/jamacardio.2020.1787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Pastick KA, Okafor EC, Wang F, Lofgren SM, Skipper CP, Nicol MR, Pullen MF, Rajasingham R, McDonald EG, Lee TC, Schwartz IS, Kelly LE, Lother SA, Mitjà O, Letang E, Abassi M, Boulware DR. Review: hydroxychloroquine and chloroquine for treatment of SARS-CoV-2 (COVID-19). Open Forum Infect Dis 2020;7:ofaa130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Cao B, Wang Y, Wen D, Liu W, Wang J, Fan G, Ruan L, Song B, Cai Y, Wei M, Li X, Xia J, Chen N, Xiang J, Yu T, Bai T, Xie X, Zhang L, Li C, Yuan Y, Chen H, Li H, Huang H, Tu S, Gong F, Liu Y, Wei Y, Dong C, Zhou F, Gu X, Xu J, Liu Z, Zhang Y, Li H, Shang L, Wang K, Li K, Zhou X, Dong X, Qu Z, Lu S, Hu X, Ruan S, Luo S, Wu J, Peng L, Cheng F, Pan L, Zou J, Jia C, Wang J, Liu X, Wang S, Wu X, Ge Q, He J, Zhan H, Qiu F, Guo L, Huang C, Jaki T, Hayden FG, Horby PW, Zhang D, Wang C.. A trial of lopinavir–ritonavir in adults hospitalized with severe Covid-19. N Engl J Med 2020;382:1787–1799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Walker M. FDA OKs Remdesivir Emergency Use for Severe COVID-19. Medpage Today. 1 May 2020. https://www.medpagetoday.com/infectiousdisease/covid19/86280
- 66.Beigel JH,Tomashek KM, Dodd LE, Mehta AK, Zingman BS, Kalil AC, Hohmann E, Chu HY, Luetkemeyer A, Kline S, Lopez de Castilla D, Finberg RW, Dierberg K, Tapson V, Hsieh L, Patterson TF, Paredes R, Sweeney DA, Short WR, Touloumi G, Lye DC, Ohmagari N, Oh MD, Ruiz-Palacios GM, Benfield T, Fätkenheuer G, Kortepeter MG, Atmar RL, Creech CB, Lundgren J, Babiker AG , Pett S, Neaton JD, Burgess TH, Bonnett T, Green M, Makowski M, Osinusi A, Nayak S, Lane HC, ACTT-1 Study Group Members. Remdesivir for the Treatment of Covid-19 - Preliminary Report. N Engl J Med 2020;doi: 10.1056/NEJMoa2007764.
- 67. Goldman JD, Lye DCB, Hui DS, Marks KM, Bruno R, Montejano R, Spinner CD, Galli M, Ahn M-Y, Nahass RG, Chen Y-S, SenGupta D, Hyland RH, Osinusi AO, Cao H, Blair C, Wei X, Gaggar A, Brainard DM, Towner WJ, Muñoz J, Mullane KM, Marty FM, Tashima KT, Diaz G, Subramanian A; GS-US-540-5773 Investigators Remdesivir for 5 or 10 Days in Patients With Severe Covid-19. N Engl J Med 2020;doi: 10.1056/NEJMoa2015301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.University of Liverpool. COVID-19 drug interactions. https://www.covid19-druginteractions.org/
- 69.Surviving Sepsis Campaign. COVID-19 Guidelines. 20 March 2020. https://www.sccm.org/SurvivingSepsisCampaign/Guidelines/COVID-19
- 70.World Health Organization. Clinical management of severe acute respiratory infection when COVID-19 is suspected. 13 March 2020. https://www.who.int/publications-detail/clinical-management-of-severe-acute-respiratory-infection-when-novel-coronavirus-( ncov)-infection-is-suspected
- 71. Xu X, Han M, Li T, Sun W, Wang D, Fu B, Zhou Y, Zheng X, Yang Y, Li X, Zhang X, Pan A, Wei H.. Effective treatment of severe COVID-19 patients with tocilizumab. Proc Natl Acad Sci USA 2020;doi: 10.1073/pnas.2005615117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72. Sciascia S, Aprà F, Baffa A, Baldovino S, Boaro D, Boero R, Bonora S, Calcagno A, Cecchi I, Cinnirella G, Converso M, Cozzi M, Crosasso P, De Iaco F, Di Perri G, Eandi M, Fenoglio R, Giusti M, Imperiale D, Imperiale G, Livigni S, Manno E, Massara C, Milone V, Natale G, Navarra M, Oddone V, Osella S, Piccioni P, Radin M, Roccatello D, Rossi D.. Pilot prospective open, single-arm multicentre study on off-label use of tocilizumab in patients with severe COVID-19. Clin Exp Rheumatol 2020;in press. [PubMed] [Google Scholar]
- 73. Bikdeli B, Madhavan MV, Jimenez D, Chuich T, Dreyfus I, Driggin E, Nigoghossian C, Ageno W, Madjid M, Guo Y, Tang LV, Hu Y, Giri J, Cushman M, Quéré I, Dimakakos EP,, Gibson CM, Lippi G, Favaloro EJ, Fareed J, Caprini JA, Tafur AJ, Burton JR, Francese DP, Wang EY, Falanga A, McLintock C, Hunt BJ, Spyropoulos AC, Barnes GD, Eikelboom JW, Weinberg I, Schulman S, Carrier M, Piazza G, Beckman JA, Steg PG, Stone GW, Rosenkranz S, Goldhaber SZ, Parikh SA, Monreal M, Krumholz HM, Konstantinides SV, Weitz JI, Lip GYH.. COVID-19 and thrombotic or thromboembolic disease: implications for prevention, antithrombotic therapy, and follow-up. J Am Coll Cardiol 2020;doi: 10.1016/j.jacc.2020.04.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74. Danser AHJ, Epstein M, Batlle D.. Renin–angiotensin system blockers and the COVID-19 pandemic: at present there is no evidence to abandon renin–angiotensin system blockers. Hypertension 2020;75:1382–1385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75. Reynolds HR, Adhikari S, Pulgarin C, Troxel AB, Iturrate E, Johnson SB, Hausvater A, Newman JD, Berger JS,, Bangalore S, Katz SD, Fishman GI, Kunichoff D, Chen Y, Ogedegbe G, Hochman JS.. Renin–angiotensin–aldosterone system inhibitors and risk of Covid-19. N Engl J Med 2020; doi: 10.1056/NEJMoa2008975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76. Li J, Wang X, Chen J, Zhang H, Deng A.. Association of renin–angiotensin system inhibitors with severity or risk of death in patients with hypertension hospitalized for coronavirus disease 2019 (COVID-19) infection in Wuhan, China. JAMA Cardiol 2020;doi: 10.1001/jamacardio.2020.1624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77. Mancia G, Rea F, Ludergnani M, Apolone G, Corrao G.. Renin–angiotensin–aldosterone system blockers and the risk of Covid-19. N Engl J Med 2020;doi: 10.1056/NEJMoa2006923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Position Statement of the ESC Council on Hypertension on ACE-Inhibitors and Angiotensin Receptor Blockers. 13 March 2020. https://www.escardio.org/Councils/Council-on-Hypertension-( CHT)/News/position-statement-of-the-esc-council-on-hypertension-on-ace-inhibitors-and-ang
- 79. Kreutz R, Algharably EAE, Azizi M, Dobrowolski P, Guzik T, Januszewicz A, Persu A, Prejbisz A, Riemer TG, Wang JG, Burnier M.. Hypertension, the renin–angiotensin system, and the risk of lower respiratory tract infections and lung injury: implications for COVID-19. Cardiovasc Res 2020;doi: 10.1093/cvr/cvaa097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80. Zhang P, Zhu L, Cai J, Lei F, Qin JJ, Xie J, Liu YM, Zhao YC, Huang X, Lin L, Xia M, Chen MM, Cheng X, Zhang X, Guo D, Peng Y, Ji YX, Chen J, She ZG, Wang Y,, Xu Q, Tan R, Wang H, Lin J, Luo P, Fu S, Cai H, Ye P, Xiao B, Mao W, Liu L, Yan Y, Liu M, Chen M, Zhang XJ, Wang X, Touyz RM, Xia J, Zhang BH, Huang X, Yuan Y, Rohit L, Liu PP, Li H.. Association of inpatient use of angiotensin converting enzyme inhibitors and angiotensin II receptor blockers with mortality among patients with hypertension hospitalized with COVID-19. Circ Res 2020;doi: 10.1161/CIRCRESAHA.120.317134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81. Fedson DS, Opal SM, Rordam OM.. Hiding in plain sight: an approach to treating patients with severe COVID-19 infection. mBio 2020;11:e00398–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.World Health Organization. Infection prevention and control during health care when novel coronavirus (nCoV) infection is suspected. 19 March 2020. https://www.who.int/publications-detail/infection-prevention-and-control-during-health-care-when-novel-coronavirus-(ncov)-infection-is-suspected-20200125
- 83.Public Health England. COVID-19 personal protective equipment (PPE). 2 April 2020. https://www.gov.uk/government/publications/wuhan-novel-coronavirus-infection-prevention-and-control/covid-19-personal-protective-equipment-ppe
- 84. Rubin GA, Biviano A, Dizon J, Yarmohammadi H, Ehlert F, Saluja D, Rubin DA, Morrow JP, Waase M, Berman J, Kushnir A, Abrams MP, Garan H, Wan EY.. Performance of electrophysiology procedures at an academic medical center amidst the 2020 coronavirus (COVID-19) pandemic. J Cardiovasc Electrophysiol 2020;doi: 10.1111/jce.14493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85. Shah PB, Welt FGP, Mahmud E, Phillips A, Kleiman NS, Young MN, Sherwood M, Batchelor W, Wang DD,, Davidson L, Wyman J, Kadavath S, Szerlip M, Hermiller J, Fullerton D, Anwaruddin S; from the American College of Cardiology (ACC) and the Society for Cardiovascular Angiography and Interventions (SCAI). Triage considerations for patients referred for structural heart disease intervention during the coronavirus disease 2019 (COVID-19) pandemic: an ACC /SCAI Consensus Statement. Catheter Cardiovasc Interv 2020;doi: 10.1002/ccd.28910. [DOI] [PubMed] [Google Scholar]
- 86. Ti LK, Ang LS, Foong TW, Ng BSW.. What we do when a COVID-19 patient needs an operation: operating room preparation and guidance. Can J Anaesth 2020;67:756–758. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87. Szerlip M, Anwaruddin S,, Aronow HD, Cohen MG, Daniels MJ, Dehghani P, Drachman DE, Elmariah S, Feldman DN, Garcia S, Giri J, Kaul P, Kapur N, Kumbhani DJ,, Meraj PM, Morray B, Nayak KR, Parikh SA, Sakhuja R, Schussler JM, Seto A, Shah B, Swaminathan RV, Zidar DA, Naidu SS. Considerations for cardiac catheterization laboratory procedures during the COVID-19 pandemic. Perspectives from the Society for Cardiovascular Angiography and Interventions Emerging Leader Mentorship (SCAI ELM) Members and Graduates. Catheter Cardiovasc Interv 2020;doi: 10.1002/ccd.28887. [DOI] [PubMed] [Google Scholar]
- 88. Romaguera R, Cruz-González I, Ojeda S, Jiménez-Candil J, Calvo D, García Seara J, Cañadas-Godoy V, Calvo E, Brugaletta S, Sánchez Ledesma M, Moreno R. [Gestión de las salas de procedimientos invasivos cardiológicos durante el brote de coronavirus COVID-19. Documento de consenso de la Asociación de Cardiología Intervencionista y la Asociación del Ritmo Cardiaco de la Sociedad Española de Cardiología]. REC Interv Cardiol 2020;doi: 10.24875/RECIC.M20000114 [Google Scholar]
- 89. Han Y, Zeng H, Jiang H, Yang Y, Yuan Z, Cheng X, Jing Z, Liu B, Chen J, Nie S, Zhu J, Li F, Ma C.. CSC Expert Consensus on Principles of Clinical Management of Patients with Severe Emergent Cardiovascular Diseases during the COVID-19 Epidemic. Circulation 2020;doi: 10.1161/CIRCULATIONAHA.120.047011 [DOI] [PubMed] [Google Scholar]
- 90. Welt FGP, Shah PB, Aronow HD, Bortnick AE, Henry TD, Sherwood MW, Young MN, Davidson LJ, Kadavath S, Mahmud E, Kirtane AJ; American College of Cardiology’s Interventional Council and the Society for Cardiovascular Angiography and Interventions. Catheterization laboratory considerations during the coronavirus (COVID-19) pandemic: from ACC’s Interventional Council and SCAI. J Am Coll Cardiol 2020;75:2372–2375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91. Lim JY, Kang PJ, Kim JB, Jung SH, Choo SJ, Chung CH, Lee JW.. Influence of a high-intensity staffing model in a cardiac surgery intensive care unit on postoperative clinical outcomes. J Thorac Cardiovasc Surg 2020;159:1382–1389. [DOI] [PubMed] [Google Scholar]
- 92. Drake D, De Bonis M, Sade R. Cardiothoracic surgeons in pandemics: ethical considerations. CTSNet. https://www.ctsnet.org/article/cardiothoracic-surgeons-pandemics-ethical-considerations (24 March 2020). [DOI] [PMC free article] [PubMed]
- 93. Wood DA, Mahmud E, Thourani VH, Sathananthan J, Virani A, Poppas A, Harrington R, Dearani JA, Swaminathan M, Russo AM, Blankstein R, Dorbala S, Carr J, Virani S, Gin K, Packard A, Dilsizian V, Légaré JF, Leipsic J, Webb JG, Krahn AD.. Safe reintroduction of cardiovascular services during the COVID-19 pandemic: guidance from North American Society leadership. Ann Thorac Surg 2020;doi: 10.1016/j.athoracsur.2020.04.017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94. Spiteri G, Fielding J, Diercke M, Campese C, Enouf V, Gaymard A, Bella A, Sognamiglio P, Sierra Moros MJ, Riutort AN, Demina YV, Mahieu R, Broas M, Bengnér M, Buda S, Schilling J, Filleul L, Lepoutre A, Saura C, Mailles A, Levy-Bruhl D, Coignard B, Bernard-Stoecklin S, Behillil S, van der Werf S, Valette M, Lina B, Riccardo F, Nicastri E, Casas I, Larrauri A, Salom Castell M, Pozo F, Maksyutov RA, Martin C, Van Ranst M, Bossuyt N, Siira L, Sane J, Tegmark-Wisell K, Palmérus M, Broberg EK, Beauté J, Jorgensen P, Bundle N, Pereyaslov D, Adlhoch C, Pukkila J, Pebody R, Olsen S, Ciancio BC.. First cases of coronavirus disease 2019 (COVID-19) in the WHO European Region, 24 January to 21 February 2020. Euro Surveill 2020;25(9).doi: 10.2807/1560-7917.ES.2020.25.9.2000178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.COVID-19 National Emergency Response Center, Epidemiology and Case Management Team, Korea Centers for Disease Control and Prevention. Early epidemiological and clinical characteristics of 28 cases of coronavirus disease in South Korea. Osong Public Health Res Perspect 2020;11:8–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96. Arentz M, Yim E, Klaff L, Lokhandwala S, Riedo FX, Chong M, Lee M.. Characteristics and outcomes of 21 critically ill patients with COVID-19 in Washington State. JAMA 2020;doi: 10.1001/jama.2020.4326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97. Edelson DP,, Sasson C, Chan PS, Atkins DL, Aziz K, Becker LB, Berg RA, Bradley SM, Brooks SC, Cheng A, Escobedo M, Flores GE, Girotra S, Hsu A, Kamath-Rayne BD, Lee HC, Lehotzky RE, Mancini ME, Merchant RM, Nadkarni VM, Panchal AR, Peberdy MAR, Raymond TT, Walsh B, Wang DS, Zelop CM, Topjian A.. Interim Guidance for Basic and Advanced Life Support in Adults, Children, and Neonates With Suspected or Confirmed COVID-19: from the Emergency Cardiovascular Care Committee and Get With the Guidelines®-Resuscitation Adult and Pediatric Task Forces of the American Heart Association in Collaboration with the American Academy of Pediatrics, American Association for Respiratory Care, American College of Emergency Physicians, The Society of Critical Care Anesthesiologists, and American Society of Anesthesiologists: Supporting Organizations: American Association of Critical Care Nurses and National EMS Physicians. Circulation 2020;doi: 10.1161/CIRCULATIONAHA.120.047463 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98. Hunt B, Retter A, McClintock C. Practical guidance for the prevention of thrombosis and management of coagulopathy and disseminated intravascular coagulation of patients infected with COVID-19. International Society on Thrombosis and Hemostasis. https://academy.isth.org/isth/2020/covid-19/290533/beverley.hunt.andrew.retter.26.claire.mcclintock.practical.guidance.for.the.html?f=menu%3D8%2Abrowseby%3D8%2Asortby%3D2%2Alabel%3D19794
- 99. Zhai Z, Li C, Chen Y, Gerotziafas G, Zhang Z, Wan J, Liu P, Elalamy I, Wang C; Prevention Treatment of VTE Associated with COVID-19 Infection Consensus Statement Group. Prevention and treatment of venous thromboembolism associated with coronavirus disease 2019 infection: a Consensus Statement before Guidelines. Thromb Haemost 2020;doi: 10.1055/s-0040-1710019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100. Yang X, Yu Y, Xu J, Shu H, Xia J, Liu H, Wu Y, Zhang L, Yu Z, Fang M, Yu T, Wang Y, Pan S, Zou X, Yuan S, Shang Y.. Clinical course and outcomes of critically ill patients with SARS-CoV-2 pneumonia in Wuhan, China: a single-centered, retrospective, observational study. Lancet Respir Med 2020;8:475–481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101. Huang C, Wang Y, Li X, Ren L, Zhao J, Hu Y, Zhang L, Fan G, Xu J, Gu X, Cheng Z, Yu T, Xia J, Wei Y, Wu W, Xie X, Yin W, Li H, Liu M, Xiao Y, Gao H, Guo L, Xie J, Wang G, Jiang R, Gao Z, Jin Q, Wang J, Cao B.. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet 2020;395:497–506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102. Liu W, Tao ZW, Lei W, Yuan ML, Liu K, Zhou L, Wei S, Deng Y, Liu J, Liu HG, Yang M, Hu Y.. Analysis of factors associated with disease outcomes in hospitalized patients with 2019 novel coronavirus disease. Chin Med J (Engl) 2020;133:1032–1038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103. Sun Q, Qiu H, Huang M, Yang Y.. Lower mortality of COVID-19 by early recognition and intervention: experience from Jiangsu Province. Ann Intensive Care 2020;10:33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104. Mo P, Xing Y, Xiao Y, Deng L, Zhao Q, Wang H, Xiong Y, Cheng Z, Gao S, Liang K, Luo M, Chen T, Song S, Ma Z, Chen X, Zheng R, Cao Q, Wang F, Zhang Y.. Clinical characteristics of refractory COVID-19 pneumonia in Wuhan, China. Clin Infect Dis 2020;doi: 10.1093/cid/ciaa270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105. Wang Z, Yang B, Li Q, Wen L, Zhang R.. Clinical features of 69 cases with coronavirus disease 2019 in Wuhan, China. Clin Infect Dis 2020;doi: 10.1093/cid/ciaa272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106. Yao X, Ye F, Zhang M, Cui C, Huang B, Niu P, Liu X, Zhao L, Dong E, Song C, Zhan S, Lu R, Li H, Tan W, Liu D.. In vitro antiviral activity and projection of optimized dosing design of hydroxychloroquine for the treatment of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). Clin Infect Dis 2020;doi: 10.1093/cid/ciaa237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107. Cortegiani A, Ingoglia G, Ippolito M, Giarratano A, Einav S.. A systematic review on the efficacy and safety of chloroquine for the treatment of COVID-19. J Crit Care 2020;doi: 10.1016/j.jcrc.2020.03.005. [DOI] [PMC free article] [PubMed]
- 108. Wang M, Cao R, Zhang L, Yang X, Liu J, Xu M, Shi Z, Hu Z, Zhong W, Xiao G.. Remdesivir and chloroquine effectively inhibit the recently emerged novel coronavirus (2019-nCoV) in vitro. Cell Res 2020;30:269–271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109. Gao J, Tian Z, Yang X.. Breakthrough: chloroquine phosphate has shown apparent efficacy in treatment of COVID-19 associated pneumonia in clinical studies. Biosci Trends 2020;14:72–73. [DOI] [PubMed] [Google Scholar]
- 110. Gautret P, Lagier JC, Parola P, Hoang VT, Meddeb L, Mailhe M, Doudier B, Courjon J, Giordanengo V, Vieira VE, Dupont HT, Honoré S, Colson P, Chabrière E, La Scola B, Rolain JM, Brouqui P, Raoult D.. Hydroxychloroquine and azithromycin as a treatment of COVID-19: results of an open-label non-randomized clinical trial. Int J Antimicrob Agents 2020; doi: 10.1016/j.ijantimicag.2020.105949. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.International Society of Antimicrobial Chemotherapy. Statement on IJAA paper. 3 April 2020. https://www.isac.world/news-and-publications/official-isac-statement
- 112. Arabi YM, Asiri AY, Assiri AM, Aziz Jokhdar HA, Alothman A, Balkhy HH, AlJohani S, Al Harbi S, Kojan S, Al Jeraisy M, Deeb AM, Memish ZA, Ghazal S, Al Faraj S, Al-Hameed F, AlSaedi A, Mandourah Y, Al Mekhlafi GA, Sherbeeni NM, Elzein FE, Almotairi A, Al Bshabshe A, Kharaba A, Jose J, Al Harthy A, Al Sulaiman M, Mady A, Fowler RA, Hayden FG, Al-Dawood A, Abdelzaher M, Bajhmom W, Hussein MA; and the Saudi Critical Care Trials group. Treatment of Middle East respiratory syndrome with a combination of lopinavir/ritonavir and interferon-β1b (MIRACLE trial): statistical analysis plan for a recursive two-stage group sequential randomized controlled trial. Trials 2020;21:8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113. Sheahan TP, Sims AC, Leist SR,, Schäfer A, Won J, Brown AJ, Montgomery SA, Hogg A, Babusis D, Clarke MO, Spahn JE, Bauer L, Sellers S, Porter D, Feng JY, Cihlar T, Jordan R, Denison MR, Baric RS.. Comparative therapeutic efficacy of remdesivir and combination lopinavir, ritonavir, and interferon beta against MERS-CoV. Nat Commun 2020;11:222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114. Sheahan TP, Sims AC, Graham RL, Menachery VD, Gralinski LE, Case JB, Leist SR, Pyrc K, Feng JY, Trantcheva I, Bannister R, Park Y, Babusis D, Clarke MO, Mackman RL, Spahn JE, Palmiotti CA,, Siegel D, Ray AS, Cihlar T, Jordan R, Denison MR, Baric RS.. Broad-spectrum antiviral GS-5734 inhibits both epidemic and zoonotic coronaviruses. Sci Transl Med 2017;9:eaal3653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115. Grein J, Ohmagari N, Shin D, Diaz G, Asperges E, Castagna A, Feldt T, Green G, Green ML, Lescure FX, Nicastri E, Oda R, Yo K, Quiros-Roldan E, Studemeister A, Redinski J, Ahmed S, Bernett J, Chelliah D, Chen D, Chihara S, Cohen SH, Cunningham J, D'Arminio Monforte A, Ismail S,, Kato H, Lapadula G, L'Her E, Maeno T, Majumder S, Massari M, Mora-Rillo M, Mutoh Y, Nguyen D, Verweij E, Zoufaly A,, Osinusi AO, DeZure A, Zhao Y, Zhong L, Chokkalingam A, Elboudwarej E, Telep L, Timbs L, Henne I, Sellers S, Cao H, Tan SK, Winterbourne L, Desai P, Mera R, Gaggar A, Myers RP, Brainard DM, Childs R, Flanigan T.. Compassionate use of remdesivir for patients with severe Covid-19. N Engl J Med 2020;doi: 10.1056/NEJMoa2007016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116. Wang Y, Zhang D, Du G, Du R, Zhao J, Jin Y, Fu S, Gao L, Cheng Z, Lu Q, Hu Y, Luo G, Wang K, Lu Y, Li H, Wang S, Ruan S, Yang C, Mei C, Wang Y, Ding D, Wu F, Tang X, Ye X, Ye Y, Liu B, Yang J, Yin W, Wang A, Fan G, Zhou F, Liu Z, Gu X, Xu J, Shang L, Zhang Y, Cao L, Guo T, Wan Y, Qin H, Jiang Y, Jaki T, Hayden FG, Horby PW, Cao B, Wang C.. Remdesivir in adults with severe COVID-19: a randomised, double-blind, placebo-controlled, multicentre trial. Lancet 2020;doi: 10.1016/S0140-6736(20)31022-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117. Dong L, Hu S, Gao J.. Discovering drugs to treat coronavirus disease 2019 (COVID-19). Drug Discov Ther 2020;14:58–60. [DOI] [PubMed] [Google Scholar]
- 118.Spanish Drug and Sanitary Products Agency, Ministry of Health. [Available treatments for the management of respiratory infections caused by SARS-CoV-2]. https://www.aemps.gob.es/laAEMPS/docs/medicamentos-disponibles-SARS-CoV-2-19-3-2020.pdf?x98732
- 119. Cheng Y, Wong R, Soo YO, Wong WS, Lee CK, Ng MH, Chan P, Wong KC, Leung CB, Cheng G.. Use of convalescent plasma therapy in SARS patients in Hong Kong. Eur J Clin Microbiol Infect Dis 2005;24:44–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120. Shen C, Wang Z, Zhao F, Yang Y, Li J, Yuan J, Wang F, Li D, Yang M, Xing L, Wei J, Xiao H, Yang Y, Qu J, Qing L, Chen L, Xu Z, Peng L, Li Y, Zheng H, Chen F, Huang K, Jiang Y, Liu D, Zhang Z, Liu Y, Liu L.. Treatment of 5 critically ill patients with COVID-19 with convalescent plasma. JAMA 2020;doi: 10.1001/jama.2020.4783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121. Liu X, Li Z, Liu S, Sun J, Chen Z, Jiang M, Zhang Q, Wei Y, Wang X, Huang YY, Shi Y, Xu Y, Xian H,, Bai F, Ou C, Xiong B, Lew AM, Cui J, Fang R, Huang H, Zhao J, Hong X, Zhang Y, Zhou F, Luo HB.. Potential therapeutic effects of dipyridamole in the severely ill patients with COVID-19. Acta Pharm Sin B 2020;doi: 10.1016/j.apsb.2020.04.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122. Stadler K, Ha HR, Ciminale V, Spirli C, Saletti G, Schiavon M, Bruttomesso D, Bigler L, Follath F, Pettenazzo A, Baritussio A.. Amiodarone alters late endosomes and inhibits SARS coronavirus infection at a post-endosomal level. Am J Respir Cell Mol Biol 2008;39:142–149. [DOI] [PubMed] [Google Scholar]
- 123. Aimo A, Baritussio A, Emdin M, Tascini C.. Amiodarone as a possible therapy for coronavirus infection. Eur J Prev Cardiol 2020;doi: 10.1177/2047487320919233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124. Cai Q, Yanga M, Liua D, Chen J, Shu D, Xia J, Liao X, Gu Y, Cai Q, Yang Y, Shen C, Li X, Peng L, Huang D, Zhang J, Zhang S, Wang F, Liu J, Chen L, Chen S, Wang Z, Zhang Z, Cao R, Zhong W, Liu Y, Liu L.. Experimental treatment with favipiravir for COVID-19: an open-label control study. Engineering 2020;doi: 10.1016/j.eng.2020.03.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125. Siddiqu HK, Mehra MR.. COVID-19 illness in native and immunosuppressed states: a clinical–therapeutic staging proposal. J Heart Lung Transplant 2020;39:405–407. [DOI] [PMC free article] [PubMed] [Google Scholar]