Abstract
Building on prior work using Tom Dishion’s Family Check-Up, the current article examined intervention effects on dysregulated irritability in early childhood. Dysregulated irritability, defined as reactive and intense response to frustration, and prolonged angry mood, is an ideal marker of neurodevelopmental vulnerability to later psychopathology because it is a transdiagnostic indicator of decrements in self-regulation that are measurable in the first years of life and have lifelong implications for health and disease. This study is perhaps the first randomized trial to examine the direct effects of an evidence- and family-based intervention, the Family Check-Up (FCU), on irritability in early childhood and the effects of reductions in irritability on later risk of child internalizing and externalizing symptomatology. Data from the geographically and sociodemographically diverse multisite Early Steps randomized prevention trial were used. Path modeling revealed intervention effects on irritability at age 4, which predicted lower externalizing and internalizing symptoms at age 10.5. Results indicate that family-based programs initiated in early childhood can reduce early childhood irritability and later risk for psychopathology. This holds promise for earlier identification and prevention approaches that target transdiagnostic pathways. Implications for future basic and prevention research are discussed.
Keywords: Family Check-Up, irritability, parent training, transdiagnostic, early childhood, mental health prevention
The seeds of vulnerability and resilience to mental health problems are planted in early life (Cicchetti & Walker, 2003; Pine & Fox, 2015; Wakschlag et al., in press). Indeed, for the common emotional and behavioral problems of childhood, broadly captured within the internalizing/externalizing (INT/EXT) spectrum, the vast majority of all children who will manifest severe and chronic problems show some self-regulatory difficulties before the age of 5 (e.g., Trentacosta & Shaw, 2009). Over the past decades, there has been substantial effort to alter early life INT/EXT trajectories in early childhood (toddlers/preschoolers) via prevention efforts drawing from and/or embedded in naturalistic settings for broadest impact on population health (Perrin, Leslie, & Boat, 2016). At the same time, a burgeoning science base suggests that some neurodevelopmental markers of mental health risk are evident even earlier, beginning in the first year of life. These efforts to identify infants and toddlers at risk for later psychopathology have been aided by the application of developmental measurement science (Biedzio & Wakschlag, 2019; Bosl, Tager-Flusberg, & Nelson, 2018; Hay et al., 2014; Luby et al., 2019; Rogers et al., 2017). As neurodevelopmental and mechanistic understandings of developmental psychopathology have deepened, it has also become increasingly clear that transdiagnostic approaches are a powerful tool for highest impact identification and prevention at the earliest phases of the clinical sequence, particularly with an eye towards population health (Kessel, Meyer, et al., 2016; McGorry & Nelson, 2016; Nolen-Hoeksema & Watkins, 2011; Sonuga-Barke, Cortese, Fairchild, & Stringaris, 2015; Wakschlag et al., 2012; Wakschlag et al., 2015; Wakschlag et al., 2018; Walkup, Mathews, & Green, 2017; Wiggins, Mitchell, Stringaris, & Leibenluft, 2014). In this paper, we begin to weave these diverse streams of work together within a developmental framework by examining transdiagnostic impact of a well-validated early childhood prevention program, the Family Check-Up (FCU; Breitenstein, Fogg, Ocampo, Acosta, & Gross, 2016; Dishion et al., 2014; Dishion et al., 2008; Morgan, Rapee, & Bayer, 2016; Perrin, Sheldrick, McMenamy, Henson, & Carter, 2014).
INT/EXT syndromes are amongst the most common cause for concern for parents of young children and their caregivers (Sheldrick, Neger, & Perrin, 2012). For mental health screening measures to be useful in real-world systems of care, they must be brief and target modifiable and ideally, transdiagnostic risk—that efficiently captures the likelihood of developing INT/EXT problems via a single risk dimension. We previously have suggested that irritability is an ideal candidate risk marker because it is a transdiagnostic indicator of decrements in self-regulation that have lifelong implications for health and disease (Moffitt et al., 2011; Wakschlag et al., in press). Traditionally, irritability has been considered most centrally as a component of externalizing problem behavior syndromes that include aggression, noncompliance, impulsivity and irritability as “hot temper or tantrums.” Thus, the more reactive component of irritability has been an essential feature of EXT. A chronically-irritable mood state has been considered as a component of depressive syndromes which are a core feature of INT. Thus, the present transdiagnostic conceptualization of irritability, which is our central focus here, integrates these various components into a single dimension of behavioral and mood features of angry/irritable affectivity. In young children, clinically-salient irritability is dysregulated and includes a tendency to respond to frustration with intense and prolonged tantrums as well as to have a chronic angry/cranky mood state (Wakschlag et al., 2018). Dysregulated irritability is one of the best transdiagnostic indicators of INT/EXT psychopathology—a pattern that extends through adulthood (Charach, Bélanger, McLennan, & Nixon, 2017; Stringaris & Goodman, 2009a; Vidal-Ribas, Brotman, Valdivieso, Leibenluft, & Stringaris, 2016; Wakschlag et al., in press). In fact, irritability is represented in more than a dozen psychiatric disorders in the 5th Edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-5; American Psychiatric Association, 2013).
Broadly writ, problems in self-regulation (a complex construct which includes affective, cognitive, and behavioral elements) are substrates of both INT/EXT. In DSM-5, irritability is one of the three core dimensions of oppositional defiant disorder (ODD), is a core feature of the new disruptive mood dysregulation disorder (DMDD), and is present in pediatric depression as well as a central presenting problem and treatment target of a host of other pediatric mental health and neurodevelopmental problems that do not include it as a defining feature (e.g. ADHD, autism, language problems) (e.g., Faraone et al., 2018; Hawks, Marrus, Glowinski, & Constantino, 2018; Roberts et al., 2018). DMDD, DSM-5’s transdiagnostic irritability syndrome requires both reactive irritability (i.e., tantrums/outbursts) and irritable mood, with increasing evidence of its validity in early childhood (Copeland, Angold, Costello, & Egger, 2013; Dougherty et al., 2014; Kessel, Dougherty, et al., 2016; Wiggins et al., 2018). Irritability is an easily measurable component of self-regulatory problems that is a major driver of psychopathology risk; it lends itself to brief measurement via survey-based screening tools (Murray, Rosanbalm, Christopoulous, & Hamouidi, 2014; Wakschlag et al., in press). Irritability holds particular promise for early identification and prediction of broad INT/EXT risk because it is measurable beginning in infancy (Wakschlag et al., in press), is the chief indicator of dysregulation and mental health risk in pediatric infant screenings (Sheldrick, Merchant, & Perrin, 2011), and multiple large cohort studies have demonstrated its lifespan transdiagnostic import (Burke, 2012; Burke et al., 2014; Burke, Hipwell, & Loeber, 2010; Stringaris & Goodman, 2009a, 2009b).
Recent research using the irritability (“Temper Loss”) scale of the Multidimensional Assessment Profile for Disruptive Behavior (MAP-DB), a developmentally-based, dimensional parent-survey, has demonstrated irritability features that differentiate typical:atypical expression within early childhood and their transdiagnostic utility (Wakschlag et al., 2012; Wakschlag et al., 2018). This work has shown that probabilistic risk for INT/EXT (including disruptive behavior, ADHD, depression and anxiety) occurs at levels of irritability typically defined as within the normal range on traditional checklist ratings (Wakschlag et al., 2015). Using this MAPS sample, evidence from ROC analyses has demonstrated that just two MAP-DB irritability items (i.e., “is easily frustrated” and “has destructive tantrums) have good sensitivity/specificity (>70%) for concurrent and subsequent INT/EXT. In particular, preschoolers scoring high on irritability were likely to score high at two subsequent assessment points over a 16-month period, 23% of children were persistently high across time, and high scores were associated with later irritability-related syndromes: 58% meeting criteria for ODD, DMDD, and/or a depressive disorder. Conversely, of those preschool-age children with elevated irritability scores at baseline, 97% had a clinical disorder at school-age. This type of developmentally-based, dimensional approach is also proving fruitful for mechanistic studies, perhaps because narrow-band constructs can be more closely tied to underlying processes. For example, we have demonstrated prefrontal disruptions in frustration-related activation among preschoolers (age 3–5 years), including increased conflict monitoring (larger N2 amplitude) and atypicality thresholds on the MAP-DB that map to neural thresholds of atypicality in lateral prefrontal cortex (LPFC) responding (Deveney et al., 2019; Grabell et al., 2017; Li, Grabell, Wakschlag, Huppert, & Perlman, 2017).
Can Interventions Improve Irritability?
Although irritability is increasingly prominent in transdiagnostic phenomenological studies, it has received far less attention in prevention science (Biedzio & Wakschlag, 2019). Limited transdiagnostic phenomenological research occurs in part because of the absence of a diagnostic profile in DSM-5 to describe chronic irritability before DMDD was added. In a secondary data analysis study by Derella, Johnston, Loeber, and Burke (2017) of a randomized controlled effectiveness trial of the Stop Now and Plan (SNAP) Program for school-aged boys (a multicomponent intervention program focused on problem-solving and emotion regulation, and parenting practices; Chorpita et al., 2011), impact on irritability symptoms was tested. Path analysis showed significant indirect effects on irritability symptoms via improvements in child emotion regulation skills (e.g., flexibility and emotion modulated). In another trial of a parenting-based home visiting intervention for American Indian mothers with young children (age 0 at study entry), compared to controls, Barlow et al. (2013; 2015; 2009) found intervention effects on dysregulation—which included many items indicative of irritability—by age 36 months, alongside reducing both INT/EXT problems.
Although irritability is now recognized as a transdiagnostic construct, the large majority of prevention programs that have encompassed irritable behaviors fall within the externalizing syndromes. There is a long and robust literature on the efficacy of parenting-based approaches, such as FCU, Parent Management Training, and Triple P, all of which have been primarily focused on the prevention of externalizing problems (Piquero et al., 2016; van Aar, Leijten, de Castro, & Overbeek, 2017; Van Ryzin, Roseth, Fosco, Lee, & Chen, 2016) and treatment of clinical syndromes such as ODD (Burkey et al., 2018; Comer, Chow, Chan, Cooper, & Wilson, 2013; Sawyer, Borduin, & Dopp, 2015). More recently, modalities have been expanded to focus on emotion development as a preventive intervention for preschool depression (Luby, Barch, Whalen, Tillman, & Freedland, 2018), and for anxiety (Barlow et al., 2015). Because broadband INT/EXT and DSM syndromes are not mechanistically oriented and represent heterogeneous sets of behaviors, irritability per se has not been directly examined as an intervention target or mechanism in these evidence-based parenting programs. However, some studies have shown impact on component features of disruptive behavior and self-regulation, suggesting that parsing is possible. For example, FCU has demonstrated intervention effects on externalizing behaviors (e.g., Dishion et al., 2008; Shelleby, Shaw, Dishion, Wilson, & Gardner, 2018; Smith et al., 2014) and inhibitory control in early childhood (Lunkenheimer et al., 2008), self-regulation from early childhood into school age (Chang, Shaw, Dishion, Gardner, & Wilson, 2014; Shelleby et al., 2012), and ODD symptoms in school-age children and adolescence (e.g., Dishion et al., 2014; Shaw et al., in press; Shaw et al., 2016; Shelleby et al., 2018; Smith et al., 2014). Additionally, FCU has demonstrated direct and indirect effects on internalizing problems in school-age children after intervening in early childhood (Lemery-Chalfant, Clifford, Dishion, Shaw, & Wilson, 2018; Reuben, Shaw, Brennan, Dishion, & Wilson, 2015). While the impact of FCU on both INT/EXT pathways has been demonstrated, in light of the salience of irritability as a broad indicator of neurodevelopmental vulnerability to mental health problems and its salience for targeted prevention at even earlier ages (i.e., beginning in infancy), it is useful to examine whether there are distinct effects of prevention programs on irritability per se, and whether it adds incremental utility for prediction of later psychopathology on INT/EXT above and beyond baseline INT/EXT.
Aims and Hypotheses
The first aim of this study was to derive a “dysregulated irritability” score from standard parent-checklist measures of early childhood emotional and behavioral functioning. The dimensional Temper Loss scale from the MAP-DB, which has been extensively validated to characterize irritability within developmental context (Biedzio & Wakschlag, 2019; Wakschlag et al., 2012) was used to crosswalk items that would be included in the new dysregulated irritability score. Wakschlag and colleagues (Kaat et al., 2019) showed that modern psychometric methods can be used to link the commonly used Child Behavior Checklist (CBCL; Achenbach & Rescorla, 2001) to the developmentally-specified MAP-DB scores. We began with the CBCL and included items from the Eyberg Child Behavior Inventory (Robinson, Eyberg, & Ross, 1980). Next, we sought to evaluate effects of the FCU on dysregulated irritability in early childhood, accounting for non-irritable broadband externalizing and internalizing symptoms to ensure unique variance contributed by dysregulated irritability. Last, we analyzed long-term transdiagnostic correlates of improving dysregulated irritability in early childhood with the FCU, net effects of baseline INT/EXT. To do so, dysregulated irritability was treated as an intervening variable on caregiver-reported symptoms of oppositional defiant disorder, depression, and anxiety assessed when the child was 10.5 years of age. Based on prior research, we hypothesized participation in the FCU would lead to improvements in dysregulated irritability that would in turn predict fewer symptoms of internalizing and externalizing disorders in middle childhood.
This study builds on Tom Dishion’s interest in early preventive interventions targeting the substrates of coercive dynamics and psychopathology later in life (Dishion & Patterson, 2016). Tom recognized that these dynamics began very early in life and sought to disrupt the cascade toward deleterious outcomes by intervening with caregivers when they were normative but had the potential to persist without intervention. Tom’s insight led to FCU being applied to families of toddler-aged children with sociodemographic and behavioral risk. Dysregulated irritability is one such risk factor that could aid in identifying those children and families in need of FCU due to the risk of establishing coercive dynamics via the intense emotional expression of a child’s irritable behaviors that trigger a caregiver’s suboptimal response.
Method
Participants
This study involves the 731 families (49% female children) in the Early Steps study, a randomized trial of the FCU in early childhood. Caregivers with children between ages 2 years 0 months and 2 years 11 months were recruited from the Women, Infants, and Children Nutrition Program (WIC) in three geographically and culturally diverse U.S. regions near Charlottesville, Virginia (188 dyads), Eugene, Oregon (271), and Pittsburgh, Pennsylvania (272). Those who indicated socioeconomic, family, or child risk factors on screening measures were invited to participate in the study (367 were randomly assigned to the intervention condition and 364 families to WIC services as usual). The caregivers who participated in the assessment were predominantly biological mothers at study entry (96%). The sample is culturally diverse with European American (50.1%), African American (27.9%), and Latino/Hispanic (13.4%) families.
Procedures
Assessment and intervention schedule
Caregivers and children who agreed to participate in the study were scheduled for a 2.5-hour home visit to complete the assessment at age 2. At the end of the age 2 assessment, families were randomized to either the FCU condition or to WIC services as usual. Families in both arms of the trial were then assessed each year using caregiver completed questionnaires from ages 2–5 years and ages 7.5–10.5 years. Beginning at age 7.5, the child’s primary teacher was contacted to complete a questionnaire via mail. Families and teachers received a monetary incentive.
Family Check-Up
The FCU is an ecological approach to family intervention and treatment designed to improve children’s adjustment by motivating positive behavior support and other family management practices. The FCU is a brief, three-session intervention that is individually tailored to the needs of the family. Typically, the three meetings include an initial contact session, a home-based multi-informant ecological assessment, and a feedback session (Dishion & Stormshak, 2007). Feedback emphasizes parenting and family strengths, yet draws attention to possible areas of change. Each year of the study, families in the FCU condition were offered feedback, which occurred after the in-home assessment for research purposes. Engagement in the FCU, defined as receipt of feedback, from ages 2 to 4 were as follows: age 2, 76%; age 3, 69%; age 4, 70%. In total, 86% of the families in the FCU condition received at least one feedback by age 4 and 44% of families received feedback in all 3 years. Previous research found that intervention effects increase as a function of the number of feedback sessions received from ages 2 to 4 (Dishion et al., 2014). Overall, engagement varied highly over the course of the trial with a total of eight opportunities for feedback for those families in the FCU condition (see Smith, Berkel, Hails, et al., 2018). Following feedback each year for engaged families, parent training sessions focused on positive behavior support, monitoring and limit setting, and family relationship building were offered in an individualized manner. Among those families participating in at least one FCU feedback session during the trial (N = 343), the majority (82.8%) received an annual average of less than three hours of follow-up intervention services, while 10.2% averaged greater than five hours per year of follow-up intervention services (Smith, Berkel, Hails, et al., 2018).
Measures
Irritability in early childhood
Two measures were used to derive an irritability scale that aligns with the MAP-DB. First, the Child Behavior Checklist (CBCL) parent version (Achenbach & Rescorla, 2001) was administered during the age 2, 3, and 4 home visits. Respondents were asked to rate the applicability of several statements regarding child behaviors by using a 3-point Likert scale in which 0 = not true, 1 = somewhat, sometimes true, and 2 = very true, often true. Second, items were drawn from the Eyberg Child Behavior Inventory, a widely used 36-item measure of early childhood problem behavior (Robinson et al., 1980). Because the Intensity factor of the Eyberg is similar in content and structure to the CBCL, we used items on the Intensity scale, on which caregivers report the eextent to which the behavior is a problem for the parent using a 7-point scale. In total, 13 items comprise the scale; 7 from the CBCL (e.g., cries a lot, temper tantrums-hot temper) and 6 from the Eyberg (e.g., has temper tantrums, yells or screams) (see Table 1). Internal consistency was good??
Table 1.
Standardized Factor Loadings for CFA Models
| Configural Model | Metric Model | Scalar Model | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Measure: Item | Age 2 | Age 3 | Age 4 | Age 2 | Age 3 | Age 4 | Age 2 | Age 3 | Age 4 |
| CBCL: Cries a lot | .611 | .671 | .665 | .620 | .670 | .666 | .617 | .672 | .665 |
| CBCL: Nervous high strung or tense | .306 | .488 | .444 | .370 | .466 | .430 | .380 | .457 | .426 |
| CBCL: Screams a lot | .568 | .691 | .738 | .592 | .692 | .738 | .581 | .693 | .738 |
| CBCL: Stubborn, sullen, or irritable | .418 | .554 | .584 | .471 | .554 | .579 | .459 | .562 | .578 |
| CBCL: Sulks a lot | .408 | .432 | .574 | .439 | .462 | .558 | .436 | .488 | .555 |
| CBCL: Temper tantrums-hot temper | .597 | .758 | .800 | .662 | .755 | .795 | .649 | .757 | .795 |
| CBCL: Whining | .549 | .666 | .748 | .553 | .674 | .751 | .564 | .670 | .742 |
| Eyberg: Gets angry when doesn’t get own way | .646 | .779 | .760 | .641 | .775 | .760 | .673 | .773 | .771 |
| Eyberg: Has temper tantrums | .749 | .803 | .806 | .746 | .810 | .802 | .734 | .821 | .815 |
| Eyberg: Whines | .572 | .736 | .770 | .523 | .735 | .772 | .494 | .731 | .763 |
| Eyberg: Cries easily | .511 | .694 | .629 | .426 | .687 | .640 | .422 | .672 | .634 |
| Eyberg: Yells or screams | .593 | .785 | .780 | .584 | .784 | .783 | .585 | .782 | .779 |
| Eyberg: Destroys toys & other objects | .307 | .454 | .414 | .249 | .452 | .422 | .325 | .450 | .421 |
Note: All factor loadings significant (p < .01).
Broadband internalizing and externalizing in early childhood
Given that all of the items from the CBCL that were included on the irritability scale are included in either the broadband internalizing or externalizing scale, we created new scores for the broadband internalizing and externalizing scales for further analysis. The newly computed broadband scores included 33 items in the internalizing scale and 21 items in the externalizing scale. Internal consistencies were good at α = .81 and α = .84, respectively.
Oppositional and defiant behavior in later childhood
Caregiver reported child symptomatology was captured using the Disruptive Behavior Disorders Rating Scale (DBD; Pelham, Gnagy, Greenslade, & Milich, 1992). During the age 10.5 home assessments, primary and alternate caregivers completed the DBD, a 45-item measure keyed to DSM-IV child symptoms of ODD and other externalizing disorders. All items were rated on a 4-point scale (0 = not at all, 3 = very much), and items rated as very much were scored as a symptom being present. The total number of ODD symptoms endorsed, derived from 8 items (e.g., “often argues with adults”, “is often spiteful or vindictive”), was used. Internal consistencies of the primary caregiver (N = 561; α = .84 and alternate caregiver reports were acceptable (N = 402; α = .86).
The CBCL Teacher Report Form (TRF; Achenbach & Rescorla, 2001) was used to assess behavior problems in the classroom. As has been reported in prior studies with this sample, a measure of child oppositional and aggressive (Opp/Agg) behaviors was created from items of CBCL, which was to the primary teacher of study participants at the age 9.5 and age 10.5 assessments. Response options are the same as those listed above for the early childhood version of the CBCL. Eight items that map onto DSM-IV (American Psychiatric Association, 2000) criteria for oppositional defiant disorder and conduct disorder, including their aggressive hallmarks, were selected, and a composite variable was computed by averaging the values for these items. Internal consistency of the Opp/Agg scale was acceptable at both ages (9.5: α = .90, 10.5: α = .87). Because of the high level of missing data for the teacher reports (53% available at age 9.5; 49% available at age 10.5), either report was used as the outcome when only 1 year was available. A mean of the two scores was used when data were available at both time points (66% available for 9.5/10.5).
Depression and anxiety symptoms in later childhood
Symptoms of depression and anxiety were assessed using the National Institute of Mental Health Diagnostic Interview Schedule for Children—IV (Shaffer, Fisher, & Lucas, 1998; Shaffer, Fisher, Lucas, Dulcan, & Schwab-Stone, 2000), a structured psychiatric interview for children age 6 years and older. Caregiver responses are “Yes” or “No” for most questions, and follow-up questions are determined by previous answers in the module. The interrater reliability (r = .93) and test–retest reliability (r = .64) of the past-year diagnoses have been well established and are moderately related to (k = .52) to diagnoses generated from symptom ratings made after a clinical interview. The generalized anxiety disorder and major depression modules were used for analysis of disorder-specific symptom counts.
Covariates
Primary caregivers’ depressive symptomatology was assessed at child age 2 using the 20-item Center for Epidemiological Studies on Depression Scale (Radloff, 1977). Ratings are provided on a scale ranging from 0 (less than a day) to 3 (5–7 days) and are summed. Internal consistency was acceptable (α = .74). Child gender and child race/ethnicity were also included as both covariates and moderators. Two versions of the child race/ethnicity variable were used: 1) African American (N = 202) compared to all others (n = 529, 72%) and 2) three-group model comparing, African American, White (n = 341), and Latino/Hispanic (n = 98).
Data Analysis
To address our hypotheses, an iterative model-building process was conducted using confirmatory factor analysis (CFA) and path modeling in a structural equation modeling framework. Thirteen items were selected from the Eyberg and CBCL (see Table 1) and a multigroup CFA models were fitted across ages 2, 3, and 4 with each age treated as a separate group. The loading of one item (CBCL: “cries a lot”) on a factor was fixed to one and factor variance was freely estimated. Configural, metric, and scalar models with varying degrees of factor invariance were fitted. In the least restrictive configural model, item loadings, item thresholds, and factor variances were freely estimated across ages; factor means were fixed to zero and item scaling factors were fixed to one. In the metric model, thresholds for item CBCL: “cries a lot”, were constrained equal across age groups while other items across age groups were freely estimated. Factor loadings for all items were constrained equal across age groups. In the age 2 model, factor means were fixed to zero and item scaling factors were fixed to one, whereas in the two other age groups, factor means and item scaling factors were freely estimated. In the scalar model, loadings and thresholds were constrained equal across the age groups and factor variances were freely estimated. In the age 2 group, factor means were fixed to zero and item scaling factors fixed to one, while in the other age groups factor means and item scaling factors were freely estimated. Finally, factors scores were obtained for inclusion in path analysis.
To test hypotheses regarding intervention effects, we began with an unconditional model testing direct effects on irritability at ages 3 and 4 using an intention-to-treat approach. Next, we added caregiver-reported broadband externalizing and internalizing scores, with items included in the irritability construct removed, and baseline (age 2) covariates that are conceptually and theoretically linked to irritability: child gender, racial/ethnic status of the child, caregiver depressive symptoms. This analysis serves to determine whether the effects of the intervention on irritability are robust. We then added the later psychiatric outcomes that were hypothesized to be correlates of irritability and tested for indirect effects. That is, the extent to which intervention effects on irritability in early childhood were predictive of long-term improvements in behavioral and emotional syndromes. These included behaviors consistent with ODD, reported by primary caregiver, alternate caregiver, and teacher, and symptoms of generalized anxiety and major depression (reported by primary caregiver) assessed at age 10.5. Finally, tests of moderation were performed using a multiple-group analysis approach. Child gender and racial/ethnicity status, the living location of the family, and age 2 and age 4 child irritability scores were tested.
CFA and path modeling were conducted in Mplus 8.1 (Muthén & Muthén, 2018). CFA was run using the weighted least squares (WLSMV) estimator with delta parameterization while path models used maximum likelihood estimation with robust standard errors (MLR) to account for missingness in the data (see Table 1 for valid Ns of each variable). MLR has been shown to provide more valid estimates of standard errors in regression analysis when dependent variables are nonnormally distributed (Little & Rubin, 2002). Fit of each model was examined using the chi-square statistic, comparative fit index (CFI; Bentler, 1990), root mean square error of approximation (RMSEA; Steiger, 1990), and standardized root mean square residual (SRMR; Hu & Bentler, 1999). Small chi-squares correspond to better fit to the data. CFI values greater than 0.95 indicate good fit to the data (Bentler, 1992). RMSEA values less than 0.05 indicate good model fit, and values up to 0.08 represent reasonable errors of approximation (Browne & Cudeck, 1992). SRMR values less than .08 are generally considered good fit (Hu & Bentler, 1999). Model fit of the multigroup models were compared using the chi-square difference testing procedure.
Results
Concerning the 13-item irritability scale, the factor loadings for the configural, metric, and scalar models of the CFA are provided in Table 1. Factor loadings were significant and ranged from .31 to .75 for age 2, .43 to .82 for age 3, and .41 to .82 for age 4. Model fit was acceptable for all models. Multigroup analysis indicated invariance across ages for all three models. The configural model factor score was selected for analysis as it is the least restrictive model.
Table 2 contains the intercorrelations and descriptive statistics of the variables included in the path analysis. Of note, the irritability score was significantly (p < .001) and modestly intercorrelated amongst the three measurements (r = .15–.30) and with the living location of the child (r = .12–.17) and ethnic minority status at ages 2 (r = –.16) and 4 (r = –.09) but not at age 3 (r = –.06). Irritability was not significantly correlated with child gender at any age (r = .03–.07) and showed strong temporal correlations with major depressive and generalized anxiety symptoms and with ODD ratings by caregivers and teachers. Teacher ratings of ODD were correlated with the living location of the family, such that children in Pittsburgh were rated higher than those in Eugene or Charlottesville, child gender, such that boys were rated higher than girls, and child racial/ethnic minority status, such that African American children were rated higher than other children. Primary caregiver depressive symptoms were significantly correlated with all other variables in the model with the exception of treatment group assignment and teacher-reported ODD behaviors.
Table 2.
Intercorrelations Between Study Variables
| Variable | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | 15 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Treatment group assignment | — | −.03 | −.07 | −.12** | .02 | .03 | .00 | .04 | −.05 | .01 | −.01 | .02 | −.00 | .00 | −.02 |
| 2. Irritability (age 2) | — | .59** | .47** | .61** | .40** | .25** | .16** | .10* | .13** | .08 | .17** | .12** | .02 | −.16** | |
| 3. Irritability (age 3) | — | .66** | .47** | .35** | .22** | .24** | .08 | .21** | .12** | .24** | .15** | −.01 | −.06 | ||
| 4. Irritability (age 4) | — | .38** | .29** | .37** | .53** | .43** | .22** | .22** | .19** | .17** | .05 | −.09* | |||
| 5. CBCL Externalizing (age 2) | — | .45** | .37 ** | .23** | .16** | .18** | .17** | .16** | .08* | −.08* | .03 | ||||
| 6. CBCL Internalizing (age 2) | — | .18** | .14** | .03 | .25** | .16** | .26** | .01 | .07 | −.04 | |||||
| 7. Primary caregiver reported ODD (age 10.5) | — | .56** | .28** | .33** | .41** | .18** | .14** | −.01 | .07 | ||||||
| 8. Alternate caregiver reported ODD (age 10.5) | — | .20** | .21** | .24** | .18** | .03 | −.15** | .13* | |||||||
| 9. Teacher reported ODD (age 9.5/10.5) | — | .05 | .09 | .09* | .12** | −.27** | −.19** | ||||||||
| 10. Generalized anxiety disorder symptoms (age 10.5) | — | .56** | .19** | −.01 | .06 | −.01 | |||||||||
| 11. Major depressive episode symptoms (age 10.5) | — | .18** | −.00 | .04 | .04 | ||||||||||
| 12. Primary caregiver depression (age 2) | – | .13** | −.04 | −.03 | |||||||||||
| 13. Location of family | – | .01 | −.21** | ||||||||||||
| 14. Child gender | – | −.21** | |||||||||||||
| 15. Ethnic minority | −.01 | ||||||||||||||
| Mean | .50 | .00 | .00 | .00 | 17.51 | 10.86 | .83 | .70 | .23 | 3.63 | 2.54 | 16.75 | 2.11 | 4.47 | .72 |
| Standard Deviation | .50 | .54 | .62 | .61 | 6.33 | 5.90 | .63 | .57 | .34 | 3.46 | 2.25 | 10.66 | .79 | 3.50 | .45 |
| N | 731 | 731 | 658 | 628 | 730 | 730 | 561 | 402 | 483 | 538 | 538 | 729 | 731 | 731 | 731 |
Note.
p < .01.
p < .001.
Intervention effects on irritability
The unconditional model testing effects of the intervention on irritability showed a small non-significant effect at age 3 (β = –.06, SE = .039, B = –.05, d = –.12) and a medium significant effect at age 4 (β = –.14***, SE = .043, B = –.12, d = –.28). These results indicate that assignment to the FCU was related to lower subsequent irritability, as reported by primary caregivers, and that effects grew over time. After adding covariates to the model, effects on irritability remained significant and effect sizes improved slightly at age 3 (β = .08*, SE = .037, B = –.06, d = –.16) and age 4 (β = –.16***, SE = .042, B = –.13, d = –.32). Of the covariates, caregiver depressive symptoms, child internalizing and externalizing, and location of the family were related to irritability. All covariates were retained for the next step of model building, which was to add later outcomes on ODD behaviors, and symptoms of anxiety and depression (age 10.5). Fit statistics were not reported as the above models were saturated.
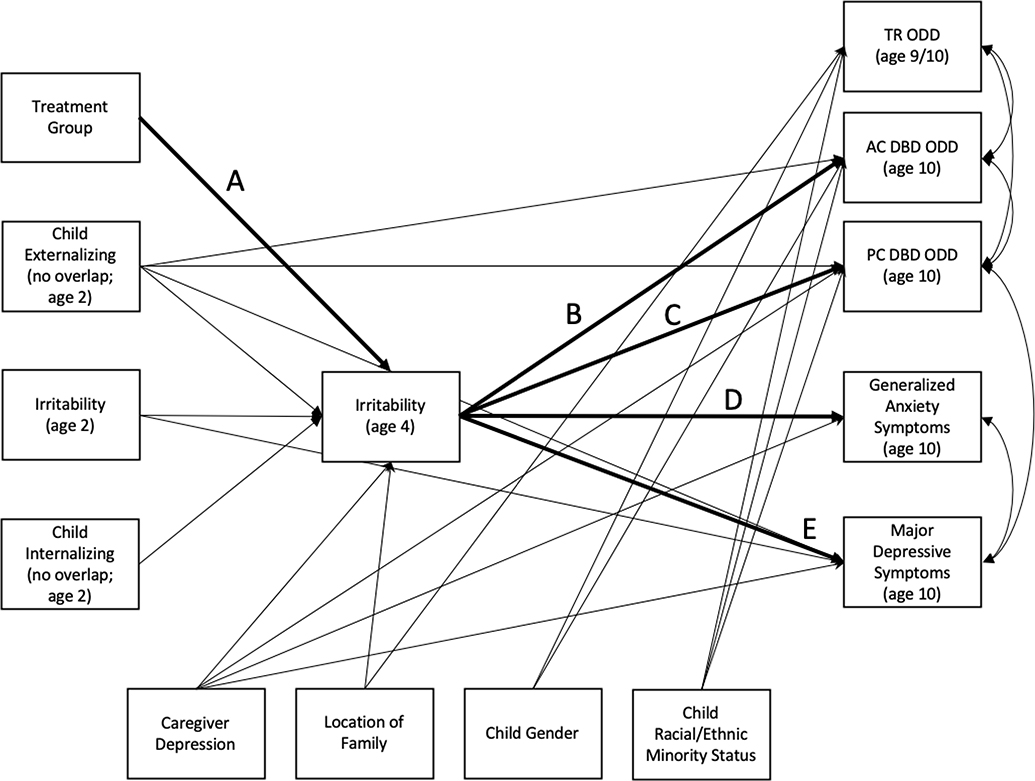
The coefficients for the paths in the final model related to the hypotheses of this study—presented in Figure 1 in darker weight lines—are provided in Table 2. All paths presented in Figure 1 were significant. The final model was saturated and thus provided good fit to the data. Comprehensive results are available by request from the first author. As suggested by bivariate correlations, caregiver depressive symptoms were significantly associated with all primary caregiver-reported endogenous variables in the model as shown. Significant associations were found between baseline levels of irritability and irritability at age 4 and depressive symptoms at age 10.5; child externalizing (age 2) and irritability at age 4, primary and alternate caregiver reported ODD at age 10.5, and depressive symptoms at age 10.5; and child internalizing (age 2) and irritability at age 4, above and beyond baseline INT/EXT.
Figure 1.
Path model.
Note. All paths shown are significant. Path labels correspond to tests of indirect effects presented in Table 3. All covariates at bottom of figure were assessed at study entry (child age 2).
All but one of the hypothesized intervention effects were significant: 1) intervention effects on irritability (age 4), controlling for age 2 levels and other externalizing and internalizing behaviors; 2) indirect intervention effects on ODD, both on primary and alternate caregiver reports, and on symptoms of generalized anxiety and major depression, through reductions in irritability at age 4. The only indirect effect not observed was on teacher reported ODD. Effect sizes of the significant indirect effects were small and ranged from d = .02–14. Relatedly, with irritability in the model at age 4, there were no direct intervention effects on the other endogenous variables. In the final model, mean differences were found for irritability (age 4) by location of the family. Analysis of variance indicated that living in an urban location was associated with higher irritability scores (M = .17, SD = .639) than living in suburban (M = –.09, SD = .547) or rural locations (M = –.08, SD = .623). Rural and suburban did not differ from one another. The final model accounted for 29% of the variance in irritability at age 4, 25% and 13% of primary and alternate caregiver-reported ODD symptoms at age 10.5, respectively; 15% of teacher-reported ODD behavers; 8% of major depression symptoms; and 6% of generalized anxiety symptoms (net effects of INT/EXT). All R-square estimates were significant at p ≤ .001 except for generalized anxiety (p = .016).
Last, tests of moderation based on child gender, ethnic minority status, living location of the family, and levels of age 2 and age 4 irritability did not reveal significant structural invariance. Each variable was removed as a covariate from the model one at a time to conduct a multiple group analysis for moderation. Two models were tested for moderation by child racial/ethnic status: African American compared to all others and a three-group model comparing, African American, White, and Latino/Hispanic. Concerning irritability, results indicated that intervention effects were not restricted to certain levels of baseline (age 2) irritability nor certain levels of irritability at age 4.
Discussion
The aims of this study further Tom Dishion’s interests in understanding the underpinnings of the transdiagnostic effects of FCU. We focus on the impact of FCU on dysregulated irritability. Early childhood irritability has been linked to long-term psychopathology across the INT/EXT spectrum (Vidal-Ribas et al., 2016; Wakschlag et al., 2018). This study is the first to test the effects of an early childhood parenting intervention, the FCU, on irritability and its downstream transdiagnostic correlates. After creating an irritability score using items from common caregiver-report measures, results of path analyses indicated that the FCU has a direct effect on reducing irritability compared to families receiving services as usual, and that these changes are related to lower externalizing (oppositional and aggressive) and internalizing (anxiety and depression) symptomatology eight years later. These effects were found while controlling for broadband INT/EXT problems at study entry and other relevant covariates, and were robust across child gender, race/ethnicity, and location of the family in this multisite trial. Additionally, ratings of problem behavior provided by other caregivers of the child also indicated that irritability effects are not merely a reflection of correlated parental perspective across domains. However, there appears to be a contextual difference between the home and school environments, as teacher-reported oppositional and defiant behaviors at school-age were not related to caregiver-reported irritability in the home during early childhood. This finding needs further examination as we did not have teacher reports of child irritability ratings in early childhood, and must test for method variance.
These findings support the contention that irritability in early childhood is a meaningful transdiagnostic risk indicator that can be used to identify children and families in need of selective interventions, namely parent training programs such as FCU. There is a tremendous need for transdiagnostic selective interventions to be delivered in non-specialty settings (Walkup et al., 2017). In this study, FCU was delivered as home visitation but it has been shown to be feasible for delivery in public schools, preschools (e.g., Head Start), in conjunction with other home visiting programs (e.g., Early Head Start), family support centers, and in pediatrics (Shaw, 2017; Smith, Berkel, Rudo-Stern, et al., 2018). Regarding integration into pediatrics, some implementations of the FCU have been coordinated with, but not delivered in the pediatric primary care system. Disorder specific intervention protocols are often complex and require intensive training in multiple protocols to address common presenting problems (Walkup et al., 2017). The promise of a parenting intervention that effectively alters the course of critical mechanisms of action for later INT/EXT psychopathology is key for achieving population impact as it increases scalability. As developmental methods and advances in developmental neuroscience increasingly indicate that INT/EXT risk at brain and behavioral levels can be identified as early as the neonatal period, and persistent irritability in the first year of life has been linked to lifespan psychopathology risk (Biedzio & Wakschlag, 2019; Bilgin et al., 2018; Graham et al., 2016; Hay et al., 2014; Lorber, Del Vecchio, & Slep, 2015; Rogers et al., 2017), prevention programs initiated even prior to the first year of life hold promise. Focusing on irritability is highly relevant towards advancing this goal because it is measurable from birth and does not rely on higher order capacities (e.g., language, effortful control) for it to emerge, although its typical and atypical expression varies as maturation occurs.
The mechanisms for this intervention effect were not tested as part of this initial inquiry into the mediating role of early childhood irritability on intervention effects between FCU and later INT/EXT psychopathology. However, the nature of the FCU and prior research with the FCU and related parenting programs provide some hypotheses to be tested in subsequent research. Intermediate mechanisms that may explain the link between irritability and later psychopathology likely include reduced rate of escalation of irritability and impairment, and improvements in self-regulation, including executive function supported by optimal functioning of prefrontal regions (e.g., more typical recruitment of neural resources during frustration; Grabell et al., 2017). Improved self-regulation, measured as reductions in children’s externalizing behaviors including irritability, is the key mechanism of life span health improvements resulting from early intervention (Heckman, Pinto, & Savelyev, 2013). Strengthening children’s capacity to adaptively manage emotions and behavior is the essential shared element of virtually all evidence-based preventions for common emotional and behavioral problems of early childhood (Dishion et al., 2014). Tom Dishion was keenly interested in understanding the common processes through which all parenting interventions work to improve child outcomes and family processes, primarily through the lens of the FCU and related behavioral parenting programs (Dishion, Forgatch, Chamberlain, & Pelham, 2016).
Parenting programs, especially parent training programs, target core caregiver skills that help children gain self-regulatory capacity. Smith and Dishion (2013) provide a summary of the evidence for the transdiagnostic effects of parent training interventions and argue that improving caregiver skills in three areas—positive behavior support, monitoring and limit setting, and family relationship building — lead to improved regulation for both the caregiver and the child, which in turn leads to downstream prevention of INT/EXT psychopathology and improved family functioning. Healthy family functioning serves as protective factor for the development or escalation of INT/EXT symptoms (Coatsworth, Duncan, Greenberg, & Nix, 2010). Future trials should consider a dismantling approach to determine the intervention elements and parenting targets that drive improvements in childhood irritability early in life. There is evidence indicating the broad salience of positive behavior support strategies being particularly important for toddler-age children (Dishion et al., 2008; Smith, St George, & Prado, 2017), but focusing exclusively on this parenting skill has not yet been tested. Subsequent research should also test the effectiveness of the intervention earlier in life (e.g., 12–18 months) because adverse parent-infant patterns are less entrenched and behavior is malleable during this period of high neuroplasticity (Campbell et al., 2014). Neuroscientific research suggests that earlier (Wakschlag et al., 2018)—before age 2—would lead to greater long-term prevention effects. Rigorous testing of this hypothesis on both neural and behavioral outcomes are needed. However, several initial efforts to examine this question at the behavioral level have demonstrated inconsistent findings (e.g., Gardner et al., 2019; Heckman et al., 2013), perhaps because of the relative instability of child behavior in general and irritability in particular before the second half of the second year.
Intervention effects of the FCU have been shown on children’s self-regulation and related constructs, including inhibitory control (Chang et al., 2014; Lunkenheimer et al., 2008), behavioral control (Shelleby et al., 2012), and effortful control (Chang, Shaw, Shelleby, Dishion, & Wilson, 2017). The effects on children’s self-regulation have been attributed to improvements in caregiver-child interactions (Chang et al., 2017) and caregiver’s use of positive behavior support skills (Shelleby et al., 2012). Additional research is needed to elucidate the precise causal pathway from parent training interventions to irritability and subsequent INT/EXT symptoms. Improvements in parenting likely precede improvements in irritability, which would help to explain the growing effect on irritability between age 3 and 4 that we observed in this study. Self-regulatory capacity might then occur as a result of reducing irritability. Irritability is highly salient and aversive to parents, and can undermine their sense of parental competence. To the extent that prevention focuses on the development of a parental toolkit for managing irritability behavior, a prevention focus is likely to have strong reverberating impact on interactional cycles and bolster self-regulatory skill. There are strong conceptual overlaps between irritability and capacity to self-regulate, meaning that improvements in one are likely to be seen simultaneously in the other. The distinctiveness of the two constructs, and not simply measurement and method (caregiver report versus observation) differences, is another area of future research.
Conclusions
This study builds on an emerging body of research on the salience of early childhood irritability as a potent risk factor for psychopathology in later childhood. These findings open the door to irritability being used as a primary screening tool that can be feasibly administered in real-world service systems and connected to parenting programs such as FCU. As the behavioral markers of irritability, namely tantrums and/or dysregulated fussiness, are highly salient to parents and providers alike, these are likely to be a meaningful target that is highly motivating for engagement. Accordingly, greater attention now needs to be given to implementation in real-world systems of care for both FCU and screening for irritability as an entry mechanism. This study indicates that FCU produces significant effects on irritability during early childhood and has high engagement of families over long periods (Smith, Berkel, Hails, et al., 2018). This delivery strategy meshes well with the pediatric primary care environment among other service contexts. Efforts are currently underway to implement parenting interventions in, or in coordination with, primary care. These include FCU (Shaw, 2017; Smith, Berkel, Rudo-Stern, et al., 2018) and a host of other evidence-based programs (e.g., Breitenstein, Shane, Julion, & Gross, 2015; Molleda et al., 2017). Fulfilling Tom Dishion’s vision of embedding FCU in real-world systems is critical to realizing the full potential of this transdiagnostic intervention.
Table 3.
Primary Results of Final Path Analysis
| Model path | B | SE (B) | β | 95% CI |
|---|---|---|---|---|
| Irritability (age 2) → Irritability (age 4) | .37*** | .052 | .32 | .265 | .469 |
| Internalizing (age 2) → Irritability (age 4) | .01* | .004 | .09 | .001 | .017 |
| Externalizing (age 2) → Irritability (age 4) | .01** | .005 | .14 | .005 | .023 |
| Intervention group → Irritability (age 4) | −.16*** | .042 | −.13 | −.239 | −.076 |
| Irritability (age 4) → PC ODD (age 10.5) | .37*** | .046 | .36 | .276 | .456 |
| Irritability (age 4) → AC ODD (age 10.5) | .21** | .050 | .23 | .113 | .311 |
| Irritability (age 4) → TR Opp/Agg (age 9.5/10.5) | .02 | .031 | .01 | −.058 | .063 |
| Irritability (age 4) → Generalized Anxiety Disorder symptoms (age 10.5) | .27*** | .108 | .11 | .055 | .480 |
| Irritability (age 4) → Major Depressive Episode symptoms (age 10.5) | 1.03*** | .285 | .18 | .474 | 1.590 |
| Indirect Effects | ||||
| Intervention group → Irritability (age 4) → PC ODD (age 10.5) | −.06*** | .017 | −.05 | −.091 | −.025 |
| Intervention group → Irritability (age 4) → AC ODD (age 10.5) | −.03** | .012 | −.03 | −.056 | −.011 |
| Intervention group → Irritability (age 4) → TR Opp/Agg (age 9.5/10.5) | .00 | .005 | −.00 | −.010 | .009 |
| Intervention group → Irritability (age 4) → Generalized Anxiety Disorder symptoms (age 10.5) | −.04* | .020 | −.01 | −.081 | −.003 |
| Intervention group → Irritability (age 4) → Major Depressive Episode symptoms (age 10.5) | −.16** | .060 | −.02 | −.281 | −.045 |
Note.
p < .05.
p < .01.
p < .001.
Effect is considered significant if the 95% confidence interval does not contain zero. PC = primary caregiver report. AC = alternate caregiver report. TR = teacher report. Opp/Agg = Oppositional/Aggressive score derived from the Child Behavior Checklist. Only paths in Figure 1 related to the study hypotheses are provided. Indirect effects and notable significant regressions from covariates on endogenous variables are provided in text. Comprehensive results of the path model are available by request from the first author.
Acknowledgments
This research was supported by grant P30DA016110 from the National Institute on Drug Abuse grant to Thomas Dishion, Daniel Shaw, and Melvin Wilson. Justin D. Smith was supported by grant R01DA027828 from the National Institute on Drug Abuse, awarded to C. Hendricks Brown. Laurie Wakschlag and Sheila Krogh-Jespersen were also supported by U01MH082830 and R01MH107652 awarded to Wakschlag. The authors gratefully thank the Early Steps team in Eugene, Pittsburgh, and Charlottesville, and the families who have participated in the study.
Contributor Information
Justin D. Smith, Center for Prevention Implementation Methodology for Drug Abuse and HIV, Department of Psychiatry and Behavioral Sciences, Feinberg School of Medicine & Institute for Innovations in Developmental Sciences, Northwestern University
Lauren Wakschlag, Department of Medical Social Sciences, Feinberg School of Medicine & Institute for Innovations in Developmental Sciences, Northwestern University.
Sheila Krogh-Jespersen, Department of Medical Social Sciences, Feinberg School of Medicine & Institute for Innovations in Developmental Sciences, Northwestern University.
John T. Walkup, Department of Psychiatry and Behavioral Sciences, Division of Child & Adolescent Psychiatry, Feinberg School of Medicine, Institute for Innovations in Developmental Sciences, Northwestern University, & Ann & Robert H. Lurie Children’s Hospital
Melvin N. Wilson, Department of Psychology, University of Virginia
Thomas J. Dishion, REACH Institute, Department of Psychology, Arizona State University & Oregon Research Institute
Daniel S. Shaw, Department of Psychology, University of Pittsburgh
References
- Achenbach TM, & Rescorla LA (2001). Manual for the ASEBA school-age forms and profiles. Burlington, VT: University of Vermont, Research Center for Children, Youth, & Families. [Google Scholar]
- American Psychiatric Association. (2000). Diagnostic and statistical manual of mental disorders, text revision (4th ed.). Washington, DC: American Psychiatric Publishing. [Google Scholar]
- American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.). Arlington, VA: American Psychiatric Publishing. [Google Scholar]
- Barlow A, Mullany B, Neault N, Compton S, Carter A, Hastings R, …Walkup JT (2013). Effect of a paraprofessional home-visiting intervention on American Indian teen mothers’ and infants’ behavioral risks: A randomized controlled trial. American Journal of Psychiatry, 170(1), 83–93. doi: 10.1176/appi.ajp.2012.12010121 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barlow A, Mullany B, Neault N, Goklish N, Billy T, Hastings R, …Walkup JT (2015). Paraprofessional-delivered home-visiting intervention for American Indian teen mothers and children: 3-Year outcomes from a randomized controlled trial. American Journal of Psychiatry, 172(2), 154–162. doi: 10.1176/appi.ajp.2014.14030332 [DOI] [PubMed] [Google Scholar]
- Bentler PM (1990). Comparative fit indexes in structural models. Psychological Bulletin, 107(2), 238–246. doi: 10.1037/0033-2909.107.2.238 [DOI] [PubMed] [Google Scholar]
- Bentler PM (1992). On the fit of models to covariances and methodology to the Bulletin. Psychological Bulletin, 112(3), 400–404. doi: 10.1037/0033-2909.112.3.400 [DOI] [PubMed] [Google Scholar]
- Biedzio D, & Wakschlag LS (2019). Developmental emergence of disruptive behaviors beginning in infancy: Delineating normal:abnormal boundaries to enhance early identification In Zeenah C (Ed.), Handbook of infant mental health (4th ed., pp. 407–425). New York, NY: The Guilford Press. [Google Scholar]
- Bilgin A, Baumann N, Jaekel J, Breeman LD, Bartmann P, Bauml JG, … Wolke D (2018). Early crying, sleeping, and feeding problems and trajectories of attention problems from childhood to adulthood. Child Development. doi: 10.1111/cdev.13155 [DOI] [PubMed] [Google Scholar]
- Bosl WJ, Tager-Flusberg H, & Nelson CA (2018). EEG analytics for early detection of autism spectrum disorder: A data-driven approach. Scientific Reports, 8(1), 6828. doi: 10.1038/s41598-018-24318-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Breitenstein SM, Fogg L, Ocampo EV, Acosta DI, & Gross D (2016). Parent use and efficacy of a self-administered, tablet-based parent training intervention: A randomized controlled trial. Journal of Medical Internet Research, 4(2), e36. doi: 10.2196/mhealth.5202 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Breitenstein SM, Shane J, Julion W, & Gross D (2015). Developing the eCPP: Adapting an evidence-based parent training program for digital delivery in primary care settings. Worldviews on Evidence-Based Nursing, 12(1), 31–40. doi: 10.1111/wvn.12074 [DOI] [PubMed] [Google Scholar]
- Browne MW, & Cudeck R (1992). Alternative ways of assessing model fit. In Bollen KA & Long JS (Eds.), Testing structural equation models (pp. 136–162). Newbury Park, CA: Sage. [Google Scholar]
- Burke JD (2012). An affective dimension within oppositional defiant disorder symptoms among boys: Personality and psychopathology outcomes into early adulthood. Journal of Child Psychology and Psychiatry, 53(11), 1176–1183. doi: 10.1111/j.1469-7610.2012.02598.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burke JD, Boylan K, Rowe R, Duku E, Stepp SD, Hipwell AE, & Waldman ID (2014). Identifying the irritability dimension of ODD: Application of a modified bifactor model across five large community samples of children. Journal of Abnormal Psychology, 123(4), 841–851. doi: 10.1037/a0037898 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burke JD, Hipwell AE, & Loeber R (2010). Dimensions of oppositional defiant disorder as predictors of depression and conduct disorder in preadolescent girls. Journal of the American Academy of Child and Adolescent Psychiatry, 49(5), 484–492. doi: 10.1016/j.jaac.2010.01.016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burkey MD, Hosein M, Morton I, Purgato M, Adi A, Kurzrok M, … Tol, W. A. (2018). Psychosocial interventions for disruptive behaviour problems in children in low- and middle-income countries: A systematic review and meta-analysis. Journal of Child Psychology and Psychiatry, 59(9), 982–993. doi: 10.1111/jcpp.12894 [DOI] [PubMed] [Google Scholar]
- Campbell F, Conti G, Heckman JJ, Moon SH, Pinto R, Pungello E, & Pan Y (2014). Early childhood investments substantially boost adult health. Science, 343(6178), 1478–1485. doi: 10.1126/science.1248429 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chang H, Shaw DS, Dishion TJ, Gardner F, & Wilson MN (2014). Direct and indirect effects of the Family Check-Up on self-regulation from toddlerhood to early school-age. Journal of Abnormal Child Psychology, 42(7), 1117–1128. doi: 10.1007/s10802-014-9859-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chang H, Shaw DS, Shelleby EC, Dishion TJ, & Wilson MN (2017). The long-term effectiveness of the Family Check-Up on peer preference: Parent-child interaction and child effortful control as sequential mediators. Journal of Abnormal Child Psychology, 45(4), 705–717. doi: 10.1007/s10802-016-0198-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Charach A, Bélanger SA, McLennan JD, & Nixon MK (2017). Screening for disruptive behaviour problems in preschool children in primary health care settings. Paediatrics & Child Health, 22(8), 478–484. doi: 10.1093/pch/pxx128 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chorpita BF, Daleiden EL, Ebesutani C, Young J, Becker KD, Nakamura BJ, … Starace N (2011). Evidence-based treatments for children and adolescents: An updated review of indicators of efficacy and effectiveness. Clinical Psychology: Science and Practice, 18(2), 154–172. doi: 10.1111/j.1468-2850.2011.01247.x [DOI] [Google Scholar]
- Cicchetti D, & Walker EF (2003). Neurodevelopmental mechanisms in psychopathology. New York, NY: Cambridge University Press. [Google Scholar]
- Coatsworth JD, Duncan LG, Greenberg MT, & Nix RL (2010). Changing parent’s mindfulness, child management skills and relationship quality with their youth: Results from a randomized pilot intervention trial. Journal of Child and Family Studies, 19(2), 203–217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Comer JS, Chow C, Chan P, Cooper C, & Wilson LA (2013). Psychosocial treatment efficacy for disruptive behavior problems in very young children: A meta-analytic examination. Journal of the American Academy of Child and Adolescent Psychiatry, 52(1), 26–36. doi: 10.1016/j.jaac.2012.10.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Copeland WE, Angold A, Costello EJ, & Egger H (2013). Prevalence, comorbidity, and correlates of DSM-5 proposed disruptive mood dysregulation disorder. American Journal of Psychiatry, 170(2), 173–179. doi: 10.1176/appi.ajp.2012.12010132 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Derella OJ, Johnston OG, Loeber R, & Burke JD (2017). CBT-enhanced emotion regulation as a mechanism of improvement for childhood irritability. Journal of Clinical Child & Adolescent Psychology, 48, S146–S154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Deveney CM, Briggs-Gowan MJ, Pagliaccio D, Estabrook CR, Zobel E, Burns JL, … Wakschlag LS (2019). Temporally sensitive neural measures of inhibition in preschool children across a spectrum of irritability. Developmental Psychobiology, 61(2), 216–227. doi: 10.1002/dev.21792 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dishion TJ, Brennan LM, Shaw DS, McEachern AD, Wilson MN, & Jo B (2014). Prevention of problem behavior through annual Family Check-Ups in early childhood: Intervention effects from home to early elementary school. Journal of Abnormal Child Psychology, 42(3), 343–354. doi: 10.1007/s10802-013-9768-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dishion TJ, Forgatch M, Chamberlain P, & Pelham WE (2016). The Oregon model of behavior family therapy: From intervention design to promoting large-scale system change. Behavior Therapy, 47(6), 812–837. doi: 10.1016/j.beth.2016.02.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dishion TJ, & Patterson GR (2016). The development and ecology of antisocial behavior: Linking etiology, prevention, and treatment In Cicchetti D (Ed.), Developmental Psychopathology (pp. 1–32). New York, NY: John Wiley & Sons, Inc. [Google Scholar]
- Dishion TJ, Shaw D, Connell A, Gardner F, Weaver C, & Wilson M (2008). The Family Check-Up with high-risk indigent families: Preventing problem behavior by increasing parents’ positive behavior support in early childhood. Child Development, 79(5), 1395–1414. doi: 10.1111/j.1467-8624.2008.01195.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dishion TJ, & Stormshak EA (2007). Intervening in children’s lives: An ecological, family-centered approach to mental health care (Vol. 43). Washington, DC: American Psychological Association. [Google Scholar]
- Dougherty LR, Smith VC, Bufferd SJ, Carlson GA, Stringaris A, Leibenluft E, & Klein DN (2014). DSM-5 disruptive mood dysregulation disorder: Correlates and predictors in young children. Psychological Medicine, 44(11), 2339–2350. doi: 10.1017/S0033291713003115 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Faraone SV, Rostain AL, Blader J, Busch B, Childress AC, Connor DF, & Newcorn JH (2018). Practitioner Review: Emotional dysregulation in attention-deficit/hyperactivity disorder - implications for clinical recognition and intervention. Journal of Child Psychology and Psychiatry, 60(2), 133–150. doi: 10.1111/jcpp.12899 [DOI] [PubMed] [Google Scholar]
- Gardner F, Leijten P, Melendez-Torres GJ, Landau S, Harris V, Mann J, … Scott S (2019). The earlier the better? Individual participant data and traditional meta-analysis of age effects of parenting interventions. Child Development, 90(1), 7–19. doi: 10.1111/cdev.13138 [DOI] [PubMed] [Google Scholar]
- Grabell AS, Li Y, Barker JW, Wakschlag LS, Huppert TJ, & Perlman SB (2017). Evidence of non-linear associations between frustration-related prefrontal cortex activation and the normal:abnormal spectrum of irritability in young children. Journal of Abnormal Child Psychology, 1–11. doi: 10.1007/s10802-017-0286-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Graham AM, Buss C, Rasmussen JM, Rudolph MD, Demeter DV, Gilmore JH, …Fair DA (2016). Implications of newborn amygdala connectivity for fear and cognitive development at 6-months-of-age. Developmental Cognitive Neuroscience, 18, 12–25. doi: 10.1016/j.dcn.2015.09.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hawks ZW, Marrus N, Glowinski AL, & Constantino JN (2018). Early origins of autism comorbidity: Neuropsychiatric traits correlated in childhood are independent in infancy. Journal of Abnormal Child Psychology, 47(2), 369–379. doi: 10.1007/s10802-018-0410-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hay D, Waters C, Perra O, Swift N, Kairis V, Phillips R, … Van Goozen S (2014). Precursors to aggression are evident by 6 months of age. Developmental Science, 17, 471–480. doi: 10.1111/desc.12133 [DOI] [PubMed] [Google Scholar]
- Heckman J, Pinto R, & Savelyev P (2013). Understanding the mechanisms through which an influential early childhood program boosted adult outcomes. American Economic Review, 103(6), 2052–2086. doi: 10.1257/aer.103.6.2052 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hu LT, & Bentler PM (1999). Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Structural Equation Modeling: A Multidisciplinary Journal, 6(1), 1–55. doi: 10.1080/10705519909540118 [DOI] [Google Scholar]
- Kaat AJ, Blackwell CK, Estabrook R, Burns JL, Petitclerc A, Briggs-Gowan MJ, … Wakschlag LS (2019). Linking the Child Behavior Checklist (CBCL) with the Multidimensional Assessment Profile of Disruptive Behavior (MAP-DB): Advancing a dimensional spectrum approach to disruptive behavior. Journal of Child and Family Studies, 28(2), 343–353. doi: 10.1007/s10826-018-1272-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessel EM, Dougherty LR, Kujawa A, Hajcak G, Carlson GA, & Klein DN (2016). Longitudinal associations between preschool disruptive mood dysregulation disorder symptoms and neural reactivity to monetary reward during preadolescence. Journal of Child and Adolescent Psychopharmacology, 26, 131–137. doi: 10.1089/cap.2015.0071 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessel EM, Meyer A, Hajcak G, Dougherty LR, Torpey-Newman DC, Carlson GA, & Klein DN (2016). Transdiagnostic factors and pathways to multifinality: The error-related negativity predicts whether preschool irritability is associated with internalizing versus externalizing symptoms at age 9. Development and Psychopathology, 28(4pt1), 913–926. doi: 10.1017/S0954579416000626 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lemery-Chalfant K, Clifford S, Dishion TJ, Shaw DS, & Wilson MN (2018). Genetic moderation of the effects of the Family Check-Up intervention on children’s internalizing symptoms: A longitudinal study with a racially/ethnically diverse sample. Development and Psychopathology, 30(5), 1729–1747. doi: 10.1017/S095457941800127x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li Y, Grabell AS, Wakschlag LS, Huppert TJ, & Perlman SB (2017). The neural substrates of cognitive flexibility are related to individual differences in preschool irritability: A fNIRS investigation. Developmental Cognitive Neuroscience, 25, 138–144. doi: 10.1016/j.dcn.2016.07.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Little RJA, & Rubin DB (2002). Statistical analysis with missing data (2nd ed.). New York, NY: Wiley. [Google Scholar]
- Lorber MF, Del Vecchio T, & Slep AMS (2015). The emergence and evolution of infant externalizing behavior. Development and Psychopathology, 27(3), 663–680. doi: 10.1017/S0954579414000923 [DOI] [PubMed] [Google Scholar]
- Luby JL, Barch DM, Whalen D, Tillman R, & Freedland KE (2018). A randomized controlled trial of parent-child psychotherapy targeting emotion development for early childhood depression. American Journal of Psychiatry, 175(11), 1102–1110. doi: 10.1176/appi.ajp.2018.18030321 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luby JL, Estabrook R, Rogers C, Krogh-Jespersen S, Norton E, Allen A, … Wakschlag LS (2019). Mapping infant neurodevelopmental precursors to mental disorder: Enhancing prediction of early childhood psychopathology via synthetic cohort & computational approaches. Submitted manuscript. [DOI] [PMC free article] [PubMed]
- Lunkenheimer ES, Dishion TJ, Shaw DS, Connell AM, Gardner F, Wilson MN, & Skuban EM (2008). Collateral benefits of the Family Check-Up on early childhood school readiness: Indirect effects of parents’ positive behavior support. Developmental Psychology, 44(6), 1737–1752. doi: 10.1037/a0013858 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McGorry P, & Nelson B (2016). Why we need a transdiagnostic staging approach to emerging psychopathology, early diagnosis, and treatment. JAMA Psychiatry, 73(3), 191–192. doi: 10.1001/jamapsychiatry.2015.2868 [DOI] [PubMed] [Google Scholar]
- Moffitt T, Arseneault L, Belsky D, Dickson N, Hancox R, Harrington H, … Caspi A (2011). A gradient of childhood self-control predicts health, wealth and public safety. Proceedings of the National Academy of Sciences, 108, 2693–2698. doi: 10.1073/pnas.1010076108 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Molleda L, Bahamon M, George SMS, Perrino T, Estrada Y, Herrera DC, … Prado G (2017). Clinic personnel, facilitator, and parent perspectives of eHealth Familias Unidas in primarycare. Journal of Pediatric Health Care, 31(3), 350–361. doi: 10.1016/j.pedhc.2016.11.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morgan AJ, Rapee RM, & Bayer JK (2016). Prevention and early intervention of anxiety problems in young children: A pilot evaluation of Cool Little Kids Online. Internet Interventions, 4, 105–112. doi: 10.1016/j.invent.2016.05.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murray D, Rosanbalm K, Christopoulous C, & Hamouidi A (2014). Self-regulation and toxic stress: Foundations for understanding self-regulation from an applied developmental perspective. Retrieved from Washington, DC: Office of Planning, Research and Evaluation, Administration of Children and Families, US Department of Health & Human Services [Google Scholar]
- Muthén BO, & Muthén LK (2018). Mplus, Version 8.1. Los Angeles, CA: Muthén & Muthén. [Google Scholar]
- Nolen-Hoeksema S, & Watkins E (2011). A heuristic for developing transdiagnostic models of psychopathology: Explaining multifinality and divergent trajectories. Perspectives on Psychological Sciences, 6, 589–609. doi: 10.1177/1745691611419672 [DOI] [PubMed] [Google Scholar]
- Pelham WE Jr., Gnagy EM, Greenslade KE, & Milich R (1992). Teacher ratings of DSM-III-R symptoms for the disruptive behavior disorders. Journal of the American Academy of Child and Adolescent Psychiatry, 31(2), 210–218. doi: 10.1097/00004583-199203000-00006 [DOI] [PubMed] [Google Scholar]
- Perrin EC, Leslie LK, & Boat T (2016). Parenting as primary prevention. JAMA Pediatrics, 170(7), 637–638. doi: 10.1001/jamapediatrics.2016.0225 [DOI] [PubMed] [Google Scholar]
- Perrin EC, Sheldrick R, McMenamy JM, Henson BS, & Carter AS (2014). Improving parenting skills for families of young children in pediatric settings: A randomized clinical trial. JAMA Pediatrics, 168(1), 16–24. doi: 10.1001/jamapediatrics.2013.2919 [DOI] [PubMed] [Google Scholar]
- Pine D, & Fox NA (2015). Childhood antecedents and risk for adult mental disorders. Annual Review of Psychology, 66, 459–485. doi: 10.1146/annurev-psych-010814-015038 [DOI] [PubMed] [Google Scholar]
- Piquero AR, Jennings WG, Diamond B, Farrington DP, Tremblay RE, Welsh BC, & Gonzalez JMR (2016). A meta-analysis update on the effects of early family/parent training programs on antisocial behavior and delinquency. Journal of Experimental Criminology, 12(2), 229–248. doi: 10.1007/s11292-016-9256-0 [DOI] [Google Scholar]
- Radloff LS (1977). The CES-D scale: A self-report depression scale for research in the general population. Applied Psychological Measurement, 1(3), 385–401. [Google Scholar]
- Reuben JD, Shaw DS, Brennan LM, Dishion TJ, & Wilson MN (2015). A family-based intervention for improving children’s emotional problems through effects on maternal depressive symptoms. Journal of Consulting and Clinical Psychology, 83(6), 1142–1148. doi: 10.1037/ccp0000049 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roberts MY, Curtis P, Estabrook R, Norton ES, Davis MM, Burns J, … Wakschlag LS (2018). Talking tots and the terrible twos: Early language and disruptive behavior in toddlers. Journal of Developmental and Behavioral Pediatrics, 39(9), 709–714. doi: 10.1097/DBP.0000000000000615 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robinson EA, Eyberg SM, & Ross AW (1980). Inventory of child behavior problems: The standardization of an inventory of child conduct problem behaviors. Journal of Clinical Child Psychology, Spring, 22–29. [Google Scholar]
- Rogers CE, Sylvester CM, Mintz C, Kenley JK, Shimony JS, Barch DM, & Smyser CD (2017). Neonatal amygdala functional connectivity at rest in healthy and preterm infants and early internalizing symptoms. Journal of the American Academy of Child and Adolescent Psychiatry, 56(2), 157–166. doi: 10.1016/j.jaac.2016.11.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sawyer AM, Borduin CM, & Dopp AR (2015). Long-term effects of prevention and treatment on youth antisocial behavior: A meta-analysis. Clinical Psychology Review, 42, 130–144. doi: 10.1016/j.cpr.2015.06.009 [DOI] [PubMed] [Google Scholar]
- Shaffer D, Fisher P, & Lucas C (1998). Diagnostic interview schedule for children, version IV In. New York, NY: Columbia University, Division of Psychiatry. [Google Scholar]
- Shaffer D, Fisher P, Lucas C, Dulcan M, & Schwab-Stone M (2000). NIMH Diagnostic Interview Schedule for Children Version-IV (NIMH DISC-IV): Description, differences from previous versions, and reliability of some common diagnoses. Journal of the American Academy of Child and Adolescent Psychiatry, 39(1), 28–38. doi: 10.1097/00004583-200001000-00014 [DOI] [PubMed] [Google Scholar]
- Shaw DS (2017). The use of the Family Check-Up in pediatric care: The SafeKeeping Youth and Smart Beginnings projects. Paper presented at the Society for Prevention Research, Washington, DC. [Google Scholar]
- Shaw DS, Galán CA, Lemery-Chalfant K, Wilson MN, Elam KK, Gardner F, & Dishion TJ (in press). Early predictors of children’s early-starting conduct problems: Child, family, genetic, and intervention effects. Development and Psychopathology. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shaw DS, Sitnick SL, Brennan LM, Choe DE, Dishion TJ, Wilson MN, & Gardner F (2016). The long-term effectiveness of the Family Check-Up on school-age conduct problems: Moderation by neighborhood deprivation. Development and Psychopathology, 28(4), 1471–1486. doi: 10.1017/S0954579415001212 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sheldrick RC, Merchant S, & Perrin EC (2011). Identification of developmental-behavioral problems in primary care: A systematic review. Pediatrics, 128(2), 356–363. doi: 10.1542/peds.2010-3261 [DOI] [PubMed] [Google Scholar]
- Sheldrick RC, Neger EN, & Perrin EC (2012). Concerns about development, behavior & learning among parents seeking pediatric care. Journal of Developmental and Behavioral Pediatrics, 33(2), 156. doi: 10.1097/DBP.0b013e3182420f4a [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shelleby EC, Shaw DS, Cheong J, Chang H, Gardner F, Dishion TJ, & Wilson MN (2012). Behavioral control in at-risk toddlers: The influence of the Family Check-Up. Journal of Clinical Child and Adolescent Psychology, 41(3), 288–301. doi: 10.1080/15374416.2012.664814 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shelleby EC, Shaw DS, Dishion TJ, Wilson MN, & Gardner F (2018). Effects of the Family Check-Up on reducing growth in conduct problems from toddlerhood through school age: An analysis of moderated mediation. Journal of Consulting and Clinical Psychology, 86(10), 856–867. doi: 10.1037/ccp0000337 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith JD, Berkel C, Hails KA, Dishion TJ, Shaw DS, & Wilson MN (2018). Predictors of participation in the Family Check-Up program: A randomized trial of yearly services from age 2 to 10 years. Prevention Science, 19(5), 652–662. doi: 10.1007/s11121-016-0679-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith JD, Berkel C, Rudo-Stern J, Montano Z, St George SM, Prado G, … Dishion TJ (2018). The Family Check-Up 4 Health (FCU4Health): Applying implementation science frameworks to the process of adapting an evidence-based parenting program for prevention of pediatric obesity and excess weight gain in primary care. Frontiers in Public Health, 6, 293. doi: 10.3389/fpubh.2018.00293 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith JD, & Dishion TJ (2013). Mindful parenting in the development and maintenance of youth psychopathology In Ehrenreich-May J & Chu BC (Eds.), Transdiagnostic mechanisms and treatment for youth psychopathology (pp. 138–160). New York, NY: The Guilford Press. [Google Scholar]
- Smith JD, Dishion TJ, Shaw DS, Wilson MN, Winter CC, & Patterson GR (2014). Coercive family process and early-onset conduct problems from age 2 to school entry. Development and Psychopathology, 26(4), 917–932. doi: 10.1017/S0954579414000169 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith JD, St George SM, & Prado G (2017). Family-centered positive behavior support interventions in early childhood to prevent obesity. Child Development, 88(2), 427–435. doi: 10.1111/cdev.12738 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sonuga-Barke EJS, Cortese S, Fairchild G, & Stringaris A (2015). Annual Research Review: Transdiagnostic neuroscience of child and adolescent mental disorders–differentiating decision making in attention-deficit/hyperactivity disorder, conduct disorder, depression, and anxiety. Journal of Child Psychology and Psychiatry, 57(3), 321–349. doi: 10.1111/jcpp.12496 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steiger JH (1990). Structural model evaluation and modification: An interval estimation approach. Multivariate Behavioral Research, 25(2), 173–180. doi: 10.1207/s15327906mbr2502_4 [DOI] [PubMed] [Google Scholar]
- Stringaris A, & Goodman R (2009a). Longitudinal outcome of youth oppositionality: Irritable, headstrong, and hurtful behaviors have distinctive predictions. Journal of the American Academy of Child and Adolescent Psychiatry, 48, 404–412 [DOI] [PubMed] [Google Scholar]
- Stringaris A, & Goodman R (2009b). Three dimensions of oppositionality in youth. Journal of Child Psychology and Psychiatry, 50(3), 216–223. [DOI] [PubMed] [Google Scholar]
- Trentacosta CJ, & Shaw DS (2009). Emotional self-regulation, peer rejection, and antisocial behavior: Developmental associations from early childhood to early adolescence. Journal of Applied Developmental Psychology, 30(3), 356–365. doi: 10.1016/j.appdev.2008.12.016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Aar J, Leijten P, de Castro BO, & Overbeek G (2017). Sustained, fade-out or sleeper effects? A systematic review and meta-analysis of parenting interventions for disruptive child behavior. Clinical Psychology Review, 51, 153–163. doi: 10.1016/j.cpr.2016.11.006 [DOI] [PubMed] [Google Scholar]
- Van Ryzin MJ, Roseth CJ, Fosco GM, Lee YK, & Chen IC (2016). A component-centered meta-analysis of family-based prevention programs for adolescent substance use. Clinical Psychology Review, 45, 72–80. doi: 10.1016/j.cpr.2016.03.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vidal-Ribas P, Brotman MA, Valdivieso I, Leibenluft E, & Stringaris A (2016). The status of irritability in psychiatry: A conceptual and quantitative review. Journal of the American Academy of Child and Adolescent Psychiatry, 55(7), 556–570. doi: 10.1016/j.jaac.2016.04.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wakschlag LS, Choi S, Carter AS, Hullsiek H, Burns J, McCarthy K, … Briggs-Gowan MJ (2012). Defining the developmental parameters of temper loss in young children: Implications for developmental psychopathology. Journal of Child Psychiatry and Psychology, 53, 1099–1108. doi: 10.1111/j.1469-7610.2012.02595.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wakschlag LS, Estabrook R, Petitclerc A, Henry D, Burns J, Perlman SB, … Briggs-Gowan MJ (2015). Clinical implications of a dimensional approach: The normal:abnormal spectrum of early irritability. Journal of the American Academy of Child and Adolescent Psychiatry, 54(8), 626–634. doi: 10.1016/j.jaac.2015.05.016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wakschlag LS, Perlman S, Blair J, Leibenluft E, Briggs-Gowan MJ, & Pine DS (2018). The neurodevelopmental basis of early childhood disruptive behavior: Irritable and callous phenotypes as exemplars. American Journal of Psychiatry, 175(2), 114–130. doi: 10.1176/appi.ajp.2017.17010045 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wakschlag LS, Roberts M, Flynn R, Marino B, Norton E, & Davis M (in press). Future directions for advancing earlier identification and prevention of mental disorders: A “Mental Health, Earlier” framework. Journal of Clinical Child & Adolescent Psychology. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walkup JT, Barlow A, Mullany BC, Pan W, Goklish N, Hasting R, … Reid R (2009). Randomized controlled trial of a paraprofessional-delivered in-home intervention for young reservation-based American Indian mothers. Journal of the American Academy of Child and Adolescent Psychiatry, 48(6), 591–601. doi: 10.1097/CHI.0b013e3181a0ab86 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walkup JT, Mathews T, & Green C (2017). Transdiagnostic behavioral therapies in pediatric primary care: Looking ahead. JAMA Psychiatry, 74(6), 557–558. doi: 10.1001/jamapsychiatry.2017.0448 [DOI] [PubMed] [Google Scholar]
- Wiggins JL, Briggs-Gowan MJ, Estabrook R, Brotman MA, Pine DS, Leibenluft E, & Wakschlag LS (2018). Identifying clinically significant irritability in early childhood. Journal of the American Academy of Child and Adolescent Psychiatry, 57(3), 191–199. doi: 10.1016/j.jaac.2017.12.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wiggins JL, Mitchell C, Stringaris A, & Leibenluft E (2014). Developmental trajectories of irritability and bidirectional associations with maternal depression Journal of the American Academy of Child and Adolescent Psychiatry, 53(11), 1191–1205. doi: 10.1016/j.jaac.2014.08.005 [DOI] [PMC free article] [PubMed] [Google Scholar]