Abstract
Background/Aim: Patients with metastatic renal cell carcinoma (RCC) with cardiac metastasis have had poor outcomes in the era of molecular targeted therapy. There are few reported outcomes for patients with cardiac metastasis of RCC treated with immune checkpoint inhibitors (ICIs). Case Report: A 32-year-old female presented with metastatic RCC (unclassified type) with contralateral renal and cardiac metastases, as well as renal hilar lymph node metastases (cT4N2M1). An 18F-fluorodeoxyglucose (FDG) positron-emission tomography (PET) computed tomographic (CT) scan was useful in diagnosing cardiac metastasis. Nivolumab plus ipilimumab achieved prominent shrinkage of almost all tumors except for one cardiac tumor. FDG-PET/CT scan also revealed the marked attenuation of FDG uptake in each tumor. In addition, a needle biopsy of the remaining primary renal tumor was pathologically observed to have no viable cancer cells. Conclusion: This successful case suggests that ICIs might provide a better outcome even for patients with cardiac metastasis of RCC, and that FDG-PET/CT scan might be useful for therapeutic assessment, as well as diagnosis.
Keywords: Renal cell carcinoma, cardiac metastasis, nivolumab plus ipilimumab, FDG-PET/CT scan
Secondary or metastatic cardiac tumors are observed at a relatively higher incidence than primary tumors of the heart. Three-quarters of them are benign and almost all are myxoma (1). The most common primary malignancies giving rise to cardiac metastases are lung cancer (36 to 39% of cardiac metastases), breast cancer (10% to 12%), and hematological malignancies (10% to 21%) (2). Autopsies found cardiac metastases in 7.3% of cases who died of advanced renal cell carcinoma (RCC) (3). The progression of RCC to the heart from the inferior vena cava (IVC) occurs in 5% to 10% of all patients with RCC. However, cardiac metastases originating from RCC without IVC involvement are extremely rare (<1%) (4).
Patients with metastatic RCC (mRCC) have been treated with molecular targeted therapy (MTT) in the first-line (5). In the era of MTT, the median overall survival of patients with cardiac metastases of RCC without IVC involvement was 9.2 months, demonstrating very poor outcomes (4). Because of the wider use of therapeutic strategies with immune checkpoint inhibitors (ICIs), such as anti-antibodies to programmed death-1 (PD1) or cytotoxic T-lymphocyte antigen-4 (CTLA4), the clinical outcomes for patients with mRCC have improved (6,7). We herein report the first case of a patient with mRCC concomitant with cardiac metastasis who showed a safe and positive response to nivolumab plus ipilimumab.
Case Report
A 32-year-old Japanese female (SIMC-Uro #11565: a unique, non-sequential patient control number for the Department of Uro-Oncology, Saitama Medical University International Medical Center) complained of left-upper abdominal pain from December 2018. At other hospitals, some careful examinations [e.g. upper gastrointestinal endoscopy, ultrasonography, and computed tomography (CT)] showed a left renal tumor without IVC involvement, with invasion of the spleen, pancreatic tail, and psoas muscle (78×71 mm, Figure 1A); multiple swelling of the left renal hilar lymph nodes; a right renal tumor (31×21 mm, Figure 1B); and a cardiac tumor in the left atrium (54×25 mm, Figure 1C). She was referred to our Institution for multidisciplinary treatment of a bilateral renal tumor with a cardiac tumor in July 2019.
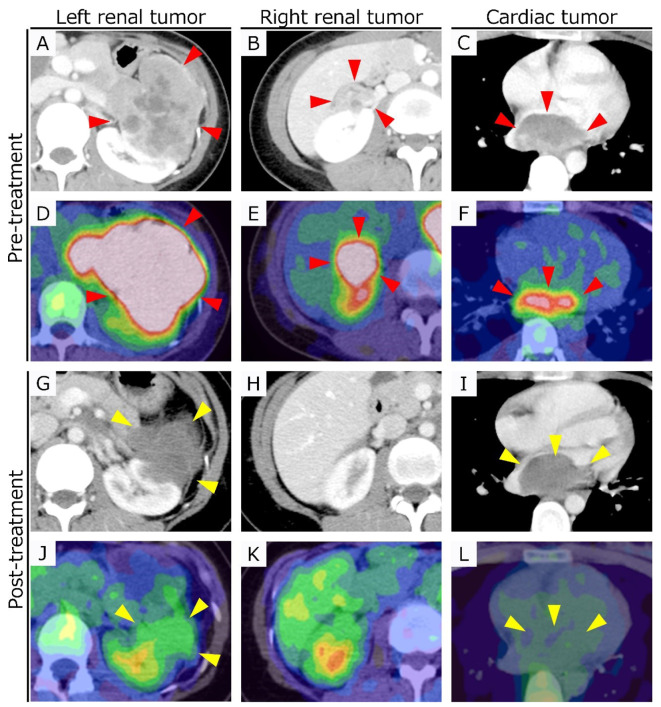
Figure 1. Contrast-enhanced computed tomographic images (A-C, and G-I) and 18F-fluorodeoxyglucose positron-emission tomography/computed tomographic images (D-F, and J-L) before and after nivolumab plus ipilimumab treatment. Red and yellow arrowheads indicate disease lesions.
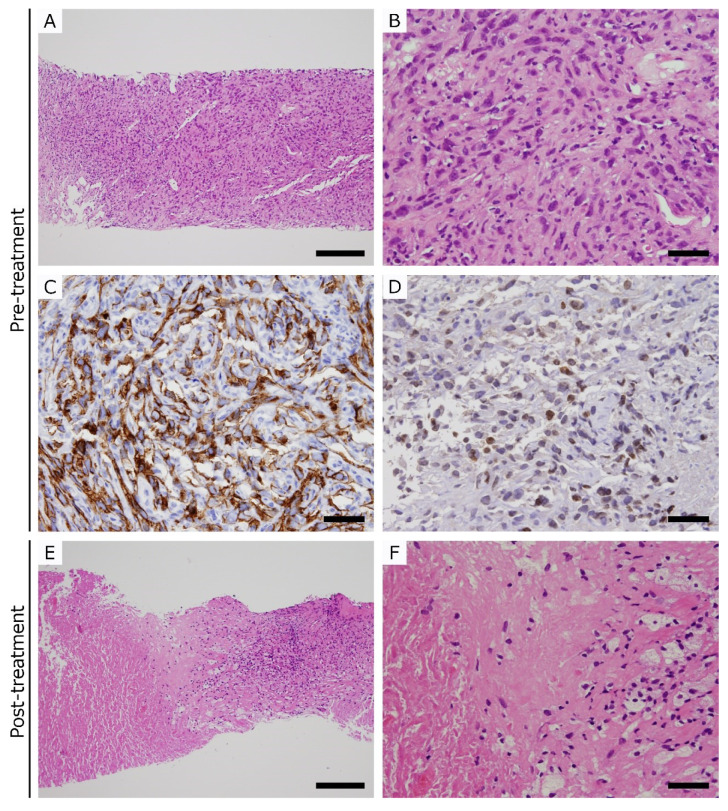
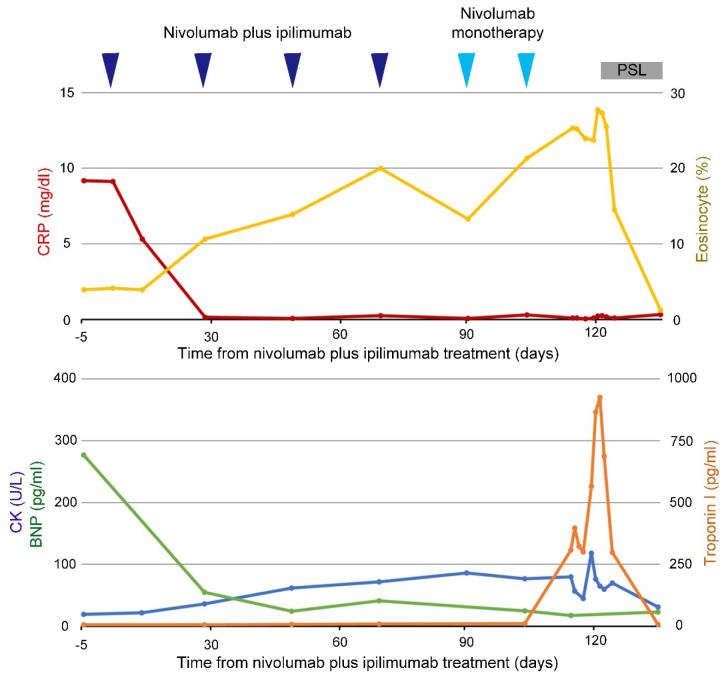
At the initial visit, the patient still had left-sided abdominal and back pain but had relatively good performance status (Karnofsky Performance Status, 90%). Physical examinations showed her to be 163 cm tall, weighing 48 kg, and with a palpable tumor in the left upper abdomen but no other abnormal findings. She had no notable medical history except for smoking (15 to 31 years old). The main laboratory examinations revealed low hemoglobin (11.0 g/dl; normal range=11.6-14.8 g/dl), high neutrophil level (81.4%; normal range=42.4-75.0%), high platelet count (388×103/μl; normal range=158-348×103/μl), normal corrected serum calcium concentration (9.8 mg/dl; normal range=8.0-10.2 mg/dl), high C-reactive protein (7.97 mg/dl; normal range=0.00-0.25 mg/dl), and high brain natriuretic peptide (BNP; 277.2 pg/ml; normal range=0.0-18.4 pg/ml). Pathological diagnosis of needle-biopsied specimens from the left renal tumor was unclassified RCC with sarcomatoid features (Fuhrman grade 4; Figure 2A to D). Concurrently, we performed imaging examinations to confirm whether the cardiac tumor in the left atrium was benign or malignant. A transthoracic echocardiogram showed that the cardiac tumor in the left atrium was fixed. Contrast-enhanced CT imaging showed the cardiac tumor was slightly enhanced in a similar pattern to the left renal tumor. Cardiac magnetic resonance imaging revealed the tumor to be low intensity on T1-weighted images and heterogeneously high intensity on T2-weighted images; the tumor broadly adhered to the posterior wall of the left atrium and moved synchronously with the left atrium (not shown). An 18F-fluorodeoxyglucose (FDG) positron-emission tomography CT (PET/CT) scan demonstrated that the mean maximum standardized uptake values (SUVmax) were 5.4 in the cardiac tumor, 16.5 in the left renal tumor, and 11.9 in the right renal tumor (Figure 1D to F), suggesting that each tumor with increased FDG uptake was malignant. Based on the above findings, we diagnosed mRCC (unclassified type) with contralateral renal and cardiac metastases, and renal hilar lymph nodes metastases (cT4N2M1). This places this entity into a poor risk group according to the International Metastatic RCC Database Consortium prognostic model (8).
Figure 2. Pathological images of left renal tumor biopsies before (A-D) and after (E and F) treatment. A, B, E, and F: Hematoxylin and eosin staining; C: CD10 immunostaining; D: Paired box 8 immunostaining. Scale bars, A and E: 200 μm; B-D and F: 50 μm.
Nivolumab plus ipilimumab immunotherapy (Nivo/Ipi; nivolumab at 240 mg plus ipilimumab at 1 mg/kg intravenously every 3 weeks for four doses, followed by nivolumab at 240 mg every 2 weeks) (7) was initiated for the patient in August 2019. After starting Nivo/Ipi, she had nocturnal wheezing, and a laboratory examination simultaneously showed eosinophilia, suggesting immune-related respiratory adverse events. Meanwhile, serum BNP and C-reactive protein fell to normal levels after two doses of Nivo/Ipi. After three doses of Nivo/Ipi, CT imaging revealed that there were no abnormal findings in the airway including the lungs; surprisingly, the left renal tumor had significantly shrunk (53×42 mm) and contrast enhancement was attenuated (Figure 1G). The right renal tumor (Figure 1H) and renal hilar lymph nodes disappeared and the cardiac tumor showed attenuation of contrast enhancement, but no change in size (Figure 1I). While Nivo/Ipi was continued, inhaled budesonide plus a tulobuterol patch combination treatment was performed, improving the respiratory symptoms, but not eosinophilia. Following two doses of nivolumab monotherapy after completion of Nivo/Ipi combination treatment, the patient gradually developed nausea and gastric distress, and a laboratory examination showed elevation in troponin-I (308.1 pg/ml; normal range=0.00-26.20 pg/ml), but normal creatine kinase and BNP (Figure 3). To diagnose immune-related gastritis or myocarditis, upper gastrointestinal endoscopy and myocardial biopsy were performed but there were no abnormal findings. Clinical symptoms and laboratory abnormal findings (troponin-I and eosinophilia) gradually recovered after cessation of nivolumab monotherapy and initiation of low dose prednisolone (10 mg/day).
Figure 3. Clinical course and the changes in laboratory data. PSL: Prednisolone; CRP: C-reactive protein; CK: creatine kinase; BNP: brain natriuretic peptide.
An FDG-PET/CT scan revealed that the mean SUVmax was 2.2 for the cardiac tumor, 3.1 for the left renal tumor, and not available for the right renal tumor as it had disappeared (Figure 1J to L), suggesting that FDG uptake in each tumor had significantly decreased. In addition, a CT scan-guided biopsy of the left renal tumor was pathologically observed to show no viable cancer cells (Figure 2E and F). Therefore, we are considering restart of nivolumab monotherapy.
Discussion
We experienced an extremely rare case of a patient with mRCC concomitant with cardiac metastasis, with good management of immune-related toxicities and a good response to Nivo/Ipi.
The frequency of RCC with extension of the tumor into the atrium from IVC is well recognized (5 to 10%). A pooled retrospective analysis of patients with mRCC treated in four clinical trials before the era of ICIs reported that cardiac metastases originating from RCC without IVC involvement were extremely rare (0.6%, n=10 of 1,765) (4). In that study, among 10 patients treated with MTT (sunitinib in one; sorafenib in five; axitinib in two; temsirolimus in two), only one patient (sunitinib) achieved a partial response; however, they soon experienced disease progression and died 7.8 months after the initial treatment. Overall in the cohort, the median progression-free and overall survival were 6.9 and 9.2 months, respectively, demonstrating poor outcomes in patients with cardiac metastases of RCC. Recently, ICIs improved the prognosis of patients with mRCC following the CheckMate 025 and 214 trials (6,7) but few case reports have confirmed the safety and efficacy of ICIs in patients with cardiac metastasis of RCC. Ansari et al. reported a case of RCC with cardiac metastasis with a good response who tolerated nivolumab well as a second-line treatment (9). Our case surprisingly showed great efficacy of Nivo/Ipi as a first-line treatment for an patient with cardiac metastasis of RCC.
FDG-PET/CT scan are not always necessary in order to diagnose RCC. Rahbar et al. reported that FDG-PET/CT scan with a cutoff SUVmax of 3.5 was used to determine tumor malignancies with a sensitivity of 100%, and that this may be useful for differentiation of benign and malignant cardiac tumors (10). In the present case, during a short follow-up, the shrinkage of cardiac tumor was not observed but an FDG-PET/CT scan showed a significant decrease in FDG uptake (decline of SUVmax in the cardiac tumor from 5.4 to 2.2), suggesting the suppression of tumor viability. This means that an FDG-PET/CT scan may be noninvasively useful to evaluate the therapeutic outcome, as well as in detecting malignant cardiac tumors. Furthermore, as in our previous report, even if radiographic examinations show residual tumor after ICI treatment, the tumor may achieve a pathological complete response (11). In the era of ICIs, conventional RECIST criteria for evaluating the change in tumor size may not be enough alone to judge the therapeutic response in solid tumors. Further accumulated cases will be needed to confirm a more suitable assessment strategy for ICI treatment.
Although as far as we are aware there have been no reports about an increase in cardiac disorders for patients with mRCC and cardiac metastases treated with either MTT or ICI, a systematic review reported that the incidence of immune-related fatal cardiac disorders, including myocarditis, was higher in patients treated with a combination of antibodies to PD1/PD-L1 plus CTLA4 as compared with anti-PD1 alone [4/1,549 (0.26%); 4/9,136 (0.04%)] (12). Therefore, this case with an increased BNP level at diagnosis was carefully initiated on Nivo/Ipi. A sudden increase in troponin-I with non-specific digestive symptoms during the treatment was immediately suspicious of immune-related cardiac toxicity. Fortunately, cardiac examinations including myocardial biopsy showed no abnormal findings; however, the administration of low-dose prednisolone was started as a precaution, and both the troponin-I level and non-specific digestive symptoms quickly improved. In cases like this, the need for prednisolone treatment is controversial. Even so, the possibility of immune-related toxicity should be kept in mind both during and after ICI treatment.
In conclusion, this successful case suggests that Nivo/Ipi is able to provide a better outcome even for patients with cardiac metastasis of RCC, and that FDG-PET/CT scan can be helpful for therapeutic assessment as well as diagnosis.
Ethical Statement
The Authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Patient Consent for Publication
Opt-out consent was applied for this case report.
Conflicts of Interest
All Authors declare that they have no conflicts of interest in regard to this study.
Authors’ Contributions
SS, YU and TO planned the case study, and collected the data and the images of the case in addition to producing the draft of the article. GK, KK, KN and MO critically revised the article for important intellectual content. All Authors read and approved the final article to be published.
References
- 1.Reynen K, Kockeritz U, Strasser RH. Metastases to the heart. Ann Oncol. 2004;15(3):375–381. doi: 10.1093/annonc/mdh086. [DOI] [PubMed] [Google Scholar]
- 2.Goldberg AD, Blankstein R, Padera RF. Tumors metastatic to the heart. Circulation. 2013;128(16):1790–1794. doi: 10.1161/CIRCULATIONAHA.112.000790. [DOI] [PubMed] [Google Scholar]
- 3.Bussani R, De-Giorgio F, Abbate A, Silvestri F. Cardiac metastases. J Clin Pathol. 2007;60(1):27–34. doi: 10.1136/jcp.2005.035105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Viteri Malone MA, Ares GR, De Velasco G, Brandao R, Lin X, Norton C, Simantov R, Moslehi J, Krajewski KM, Choueiri TK, McKay RR. The clinical presentation, survival outcomes, and management of patients with renal cell carcinoma and cardiac metastasis without inferior vena cava involvement: Results from a pooled clinical trial database and systematic review of reported cases. Clin Genitourin Cancer. 2018;16(2):e327–e333. doi: 10.1016/j.clgc.2017.11.005. [DOI] [PubMed] [Google Scholar]
- 5.Hsieh JJ, Purdue MP, Signoretti S, Swanton C, Albiges L, Schmidinger M, Heng DY, Larkin J, Ficarra V. Renal cell carcinoma. Nat Rev Disprimers. 2017;3:17009. doi: 10.1038/nrdp.2017.9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Motzer RJ, Escudier B, McDermott DF, George S, Hammers HJ, Srinivas S, Tykodi SS, Sosman JA, Procopio G, Plimack ER, Castellano D, Choueiri TK, Gurney H, Donskov F, Bono P, Wagstaff J, Gauler TC, Ueda T, Tomita Y, Schutz FA, Kollmannsberger C, Larkin J, Ravaud A, Simon JS, Xu LA, Waxman IM, Sharma P, CheckMate 025 Investigators Nivolumab versus everolimus in advanced renal-cell carcinoma. N Engl J Med. 2015;373(19):1803–1813. doi: 10.1056/NEJMoa1510665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Motzer RJ, Tannir NM, McDermott DF, Aren Frontera O, Melichar B, Choueiri TK, Plimack ER, Barthelemy P, Porta C, George S, Powles T, Donskov F, Neiman V, Kollmannsberger CK, Salman P, Gurney H, Hawkins R, Ravaud A, Grimm MO, Bracarda S, Barrios CH, Tomita Y, Castellano D, Rini BI, Chen AC, Mekan S, McHenry MB, Wind-Rotolo M, Doan J, Sharma P, Hammers HJ, Escudier B, CheckMate 214 Investigators Nivolumab plus ipilimumab versus sunitinib in advanced renal-cell carcinoma. N Engl J Med. 2018;378(14):1277–1290. doi: 10.1056/NEJMoa1712126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Heng DY, Xie W, Regan MM, Warren MA, Golshayan AR, Sahi C, Eigl BJ, Ruether JD, Cheng T, North S, Venner P, Knox JJ, Chi KN, Kollmannsberger C, McDermott DF, Oh WK, Atkins MB, Bukowski RM, Rini BI, Choueiri TK. Prognostic factors for overall survival in patients with metastatic renal cell carcinoma treated with vascular endothelial growth factor-targeted agents: results from a large, multicenter study. J Clin Oncol. 2009;27(34):5794–5799. doi: 10.1200/JCO.2008.21.4809. [DOI] [PubMed] [Google Scholar]
- 9.Ansari J, Alhelali S, Albinmousa Z, Farrag A, Ali AM, Abdelgelil M, Alhamad A, Alzahrani G, Ansari A, Glaholm J. Rare case of intracardiac renal cell carcinoma metastasis with response to nivolumab: Case report and literature review. Case Rep Oncol. 2018;11(3):861–870. doi: 10.1159/000495459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Rahbar K, Seifarth H, Schafers M, Stegger L, Hoffmeier A, Spieker T, Tiemann K, Maintz D, Scheld HH, Schober O, Weckesser M. Differentiation of malignant and benign cardiac tumors using 18F-FDG PET/CT. J Nucl Med. 2012;53(6):856–863. doi: 10.2967/jnumed.111.095364. [DOI] [PubMed] [Google Scholar]
- 11.Shirotake S, Kaneko G, Nagata K, Oyama M, Nishimoto K. Histological complete response with nivolumab for renal cell carcinoma with multiple metastases: A case report. Mol Clin Oncol. 2019;10(2):244–248. doi: 10.3892/mco.2018.1779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wang DY, Salem JE, Cohen JV, Chandra S, Menzer C, Ye F, Zhao S, Das S, Beckermann KE, Ha L, Rathmell WK, Ancell KK, Balko JM, Bowman C, Davis EJ, Chism DD, Horn L, Long GV, Carlino MS, Lebrun-Vignes B, Eroglu Z, Hassel JC, Menzies AM, Sosman JA, Sullivan RJ, Moslehi JJ, Johnson DB. Fatal toxic effects associated with immune checkpoint inhibitors: A systematic review and meta-analysis. JAMA Oncol. 2018;4(12):1721–1728. doi: 10.1001/jamaoncol.2018.3923. [DOI] [PMC free article] [PubMed] [Google Scholar]