Abstract
Background/Aim: Self-expandable metal stent (SEMS) as a bridge to surgery (BTS) for obstructive colorectal cancer (CRC) raises concerns regarding the short-term as well as oncological outcome. The present study aimed to investigate the safety of SEMS placement and risk factors of worse short-term and oncological outcomes as BTS. Patients and Methods: Twenty-four patients with obstructive CRC who underwent SEMS placement as BTS were included. Success rate of SEMS placement and 2-year relapse-free survival (RFS) rates in stage II/III BTS patients were assessed. Results: Technical and clinical success rates for SEMS placement were 100% and 87.5%, respectively. In Multivariate analyses, longer tumour length, longer interval to surgery, and angular positioning were risk factors related with the complication of stent placement. Two-year RFS rates were significantly higher in the no-complication than in the complication group (100% vs. 75%, log-rank test, p<0.01). Conclusion: A long tumour length, long interval between SEMS insertion and surgery, and angular positioning of the SEMS were identified as risk factors for SEMS-related complications. Moreover, SEMS insertion and/or surgery complications wereassociated with worse oncological outcome in CRC patients.
Keywords: Self-expandable metal stent, SEMS, bridge to surgery, obstructive colorectal cancer, colonic decompression
Colorectal cancer (CRC) often presents as large bowel obstruction. Traditionally, the treatment of malignant large bowel obstruction is surgery. However, emergency colorectal surgery is associated with high mortality and morbidity rates. The 30-day postoperative mortality rate for emergency surgery is reportedly 14.9%, compared with 5.8% for elective surgery (1). Colonic self-expandable metal stent (SEMS) was introduced as an alternative to surgery for malignant large bowel obstruction in 1991, with the presumed benefits of lower morbidity and mortality rates, shorter hospital stay, and reduced need for stoma creation (2,3). At first, SEMS was used for patients with non-resectable or metastatic rectal cancer (4). In 1994, Tejero et al. (5) published their experience of SEMS placement as a bridge to surgery (BTS) in patients with colonic obstruction.
Although some studies have shown that SEMS placement as a BTS might be a better alternative to traditional surgical decompression (2,3), others have reported conflicting data (6-10). There were concerns regarding the short-term adverse events associated with colonic stenting, as well as long-term survival in patients whose disease is potentially curable, because of the possible risk of both local progression of the cancer and metastatic spread (11,12).
The objective of this study was to investigate: i) the safety of SEMS placement for obstructive CRC and ii) risk factors of worse short-term and oncological outcomes of SEMS placement as a BTS.
Patients and Methods
Patient selection. Patients who were admitted to Soka Municipal Hospital with acute obstructive CRC and underwent SEMS placement between September 2014 and September 2017 for both palliation and as a BTS were included in this retrospective comparative study. Diagnosis of acute obstructive CRC was based on the clinical features of bowed obstruction using the ColoRectal Obstruction Scoring System (CROSS), and confirmed by histological examination. The CROSS is described in detail elsewhere (20,21). Briefly, the patient’s oral intake level was assessed as follows: CROSS 0, requiring continuous decompression; CROSS 1, no oral intake; CROSS 2, liquid or enteral nutrient intake; CROSS 3, soft solids, low-residue, and full diet with symptoms of stricture; or CROSS 4, soft solids, low-residue, and full diet without symptoms of stricture.
Patient baseline characteristics. Data on patient baseline characteristics (age, gender, CROSS score), tumour characteristics, diameter and length of the SEMS, surgical technique, and condition after operation, were retrieved from their medical records. Tumour location was classified as right-sided colon (ascending colon and right side of transverse colon), left-sided colon (left side of the transverse colon, descending colon and sigmoid colon), and rectum. The major axis of the tumour was measured using the final pathological report.
SEMS placement. SEMS placement was avoided where obstructive cancer presented below the perineal reflection (Rb) and caecum. From September 2014 to September 2017, 75 patients were admitted to Soka Municipal Hospital because of the malignant colonic obstruction. Thirty-four patients were excluded from this study because they underwent emergency surgery (n=14) or were inserted trans-anal obstructive CRC tubes (n=20). Among the 41 patients, 17 had unresectable stage IV disease and underwent SEMS placement for palliative aim. Finally, 24 patients, 17 of stage II/III and 7 of stage IV with resectable distant metastasis were included in this study and underwent SEMS placement as BTS.
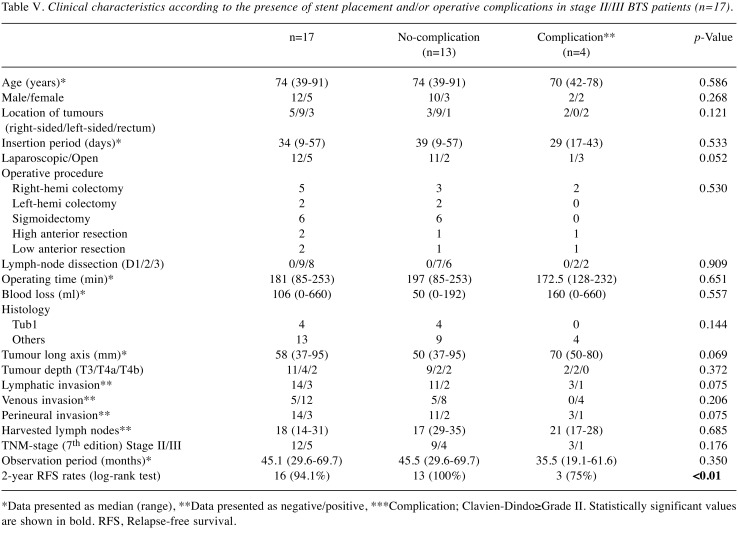
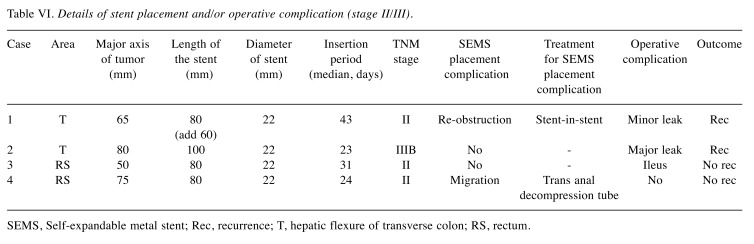
All SEMS procedures were performed to relieve obstructions by the gastroenterologists. The procedures were performed under fluoroscopic guidance with colonoscopic assistance (Figure 1), and uncovered stents (Niti-S, TaeWoong Medical Co., Ltd, Republic of Korea) with a diameter of 18 or 22 mm and lengths of 60 mm, 80 mm, 100 mm or 120 mm were chosen according to the status of the obstruction. Technical success was defined as a successful SEMS placement on the first attempt with correct deployment confirmed radiologically. Clinical success was defined as the relief of obstructive symptoms or signs within 48 h of stent deployment (defaecation and loss of air-fluid level or decrease in the colon gas).
Figure 1. Self-expandable metal stent (SEMS) procedures performed under fluoroscopic guidance with colonoscopic assistance. Uncovered stents were placed to relieve obstructions (A). The length and diameter of SEMS were chosen according to the status of the obstruction (diameters of 18 or 22 mm, lengths of 60 mm, 80 mm, 100 mm or 120 mm) (B). The red arrow shows the area of obstruction.
Surgery and follow-up. Elective surgery was performed few days to weeks after SEMS placement in BTS cases. Patients who underwent surgery were followed up for 5 years, initially at 3-month intervals for 3 years and then at 6-month intervals for the next 2 years. Follow-up examination included clinical history, physical examination, and carcinoembryonic antigen (CEA) and CA19-9 levels. Computed tomography was performed at 6-month intervals over the entire follow-up period and colonoscopy was performed every 2 years after the surgery. Follow-up of patients who underwent SEMS for palliative reasons was ended if the patients were transferred to other hospitals for further palliative care. Adjuvant chemotherapy was administered to patients with final stage III for which R0 resection was performed, and the function of major organs was maintained according to the guidelines (22). Relapse-free survival (RFS) was measured from the time of surgery until recurrence/death.
Endpoints of the study. The endpoints of the study were: i) technical and clinical success rate of SEMS placement, ii) risk factors of complications related to SEMS placement and surgery, and iii) 2-year RFS rate of stage II/III BTS cases. Risk factors of complications related to SEMS placement, i.e., perforation, migration and re-obstruction, were defined based on negative events that occurred between stent placement and elective surgery. Operative complications, including in-hospital morbidities or mortality were defined as those that occurred within 30 days of surgery and were graded according to the Clavien-Dindo Classification (CDC) (23). Anastomotic leakage was defined as fistula from anastomosis of the intestinal tract to the bowel that was either radiologically verified or diagnosed during re-laparotomy.
Statistical analysis. All statistical analyses were performed using SPSS version 22 (IBM SPSS, Chicago, IL, USA). For categorical data, the significance of between-group differences was estimated using a chi-squared test. For continuous variables, descriptive statistics (median and range) were calculated, and the significance of between-group differences was estimated using the Mann-Whitney U-test and Kruskal-Wallis test, as appropriate. Multivariate logistic regression analysis was used to examine the factors associated with complications of stent placement. Two-year RFS rate was compared using the log-rank test. All p-values<0.05 were considered statistically significant.
Ethical statement. All procedures and experimental protocol performed in studies involving human participants were approved by the ethical standards of the institutional review board of Soka Municipal Hospital. All methods were performed in accordance with the relevant guidelines and regulations including the 1964 Helsinki declaration and the “Ethical Guidelines for Medical and Health Research Involving Human Subjects” in Japan. Informed consent was obtained from all individual participants included in the study.
Results
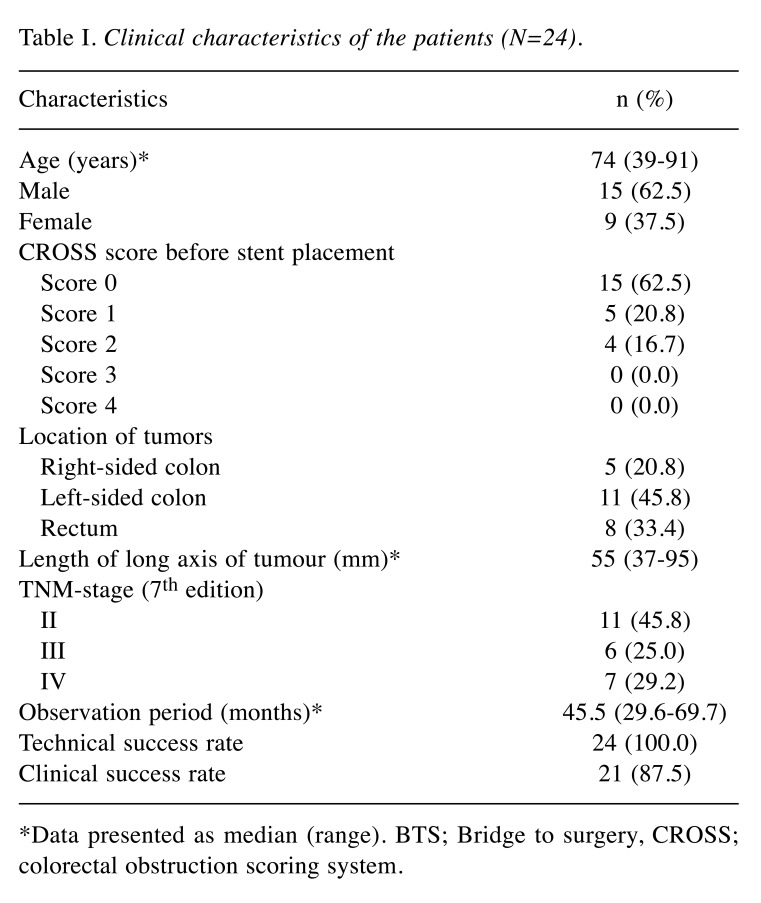
Patient characteristics. Patient background is summarized in Table I. A total of 24 patients were included in this study; 62.5% (15/24) of patients were classified as CROSS score 0. Most of the tumours were localised to the left side of the colon and rectum (19/24; 79.2%). Technical and clinical success rates were 100% and 87.5%, respectively. Patients were divided in 2 groups (complication vs. no-complication); comparisons were made between complication and no-complication group.
Table I. Clinical characteristics of the patients (N=24).
*Data presented as median (range). BTS; Bridge to surgery, CROSS; colorectal obstruction scoring system
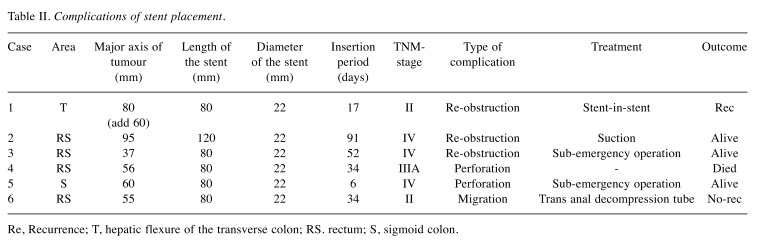
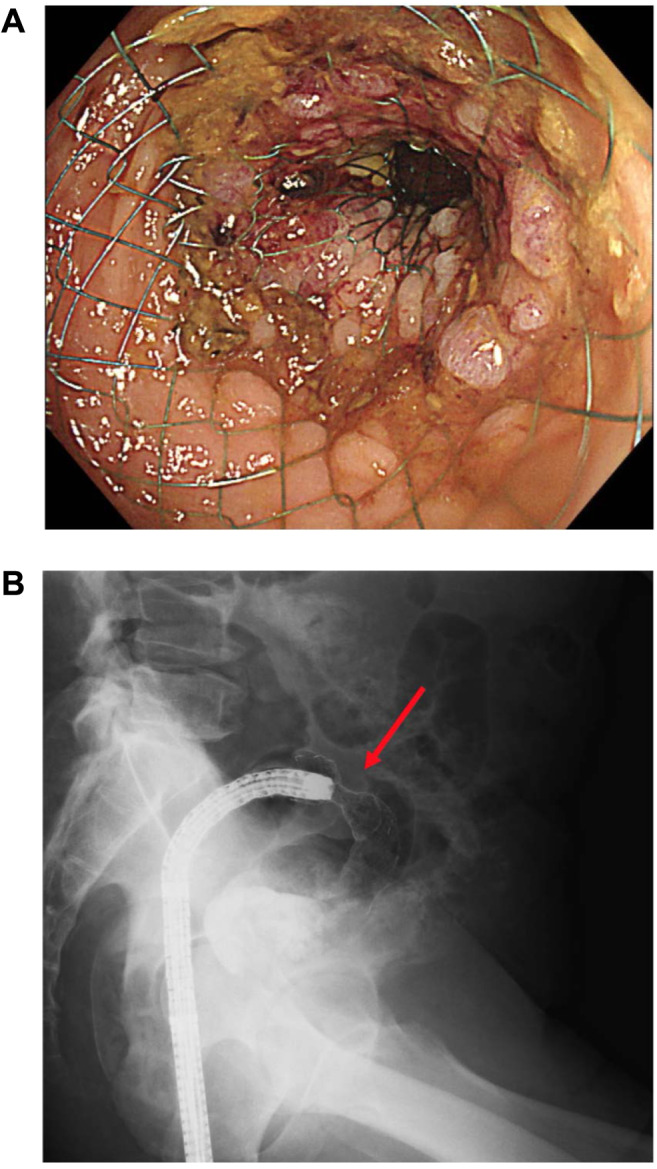
Complications of stent placement. Complications of stent placement occurred in 6 (25.0%) of 24 BTS cases (Table II). For these 6 cases, the median major axis of the tumours was 58 mm (range=37-95) and the median interval between SEMS insertion and surgery was 34 days (range=6-91). Details of the complications after SEMS placement are the following: 3 out of 6 patients had re-obstruction, 2 developed perforation, and 1 experienced stent migration. One patient died following perforation. Among the 6 patients, 4 underwent SEMS placement at the rectum, and 1 at the transverse colon at the hepatic flexure; another 1 at the sigmoid colon, who developed perforation due to the acute angle of the SEMS (Figure 2).
Table II. Complications of stent placement.
Complications of stent placement
Figure 2. Self-expandable metal stent (SEMS) placement with angular positioning at sigmoid colon. This patient developed perforation and resulted in sub-emergency operation. The red arrow shows the area of obstruction with angular position.

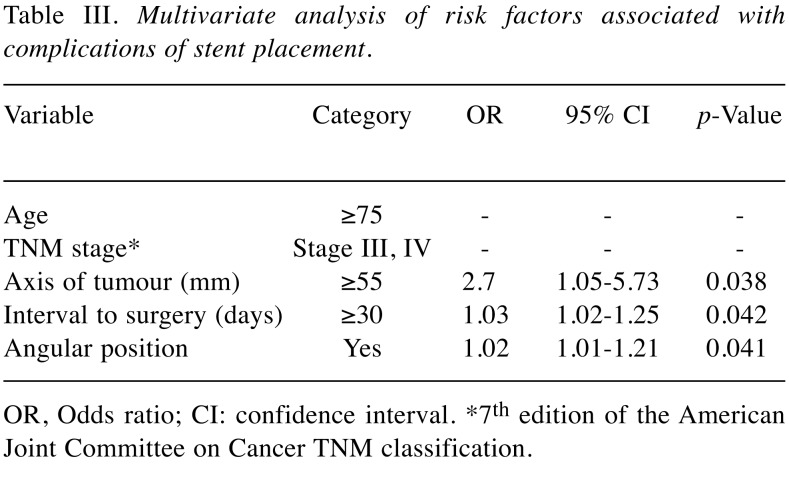
Risk factors for complications of stent placement. In multivariate analyses, longer tumour axis [odds ratio (OR)=2.70; 95% confidence interval (CI)=1.05-5.73, p=0.038)], longer interval to surgery (OR=1.03; 95% CI=1.02-1.25, p=0.042), and angular positioning (OR=1.02; 95% CI=1.01-1.21, p=0.041) as factors related with the complication of stent placement (Table III).
Table III. Multivariate analysis of risk factors associated with complications of stent placement.
OR, Odds ratio; CI: confidence interval. *7th edition of the American Joint Committee on Cancer TNM classification
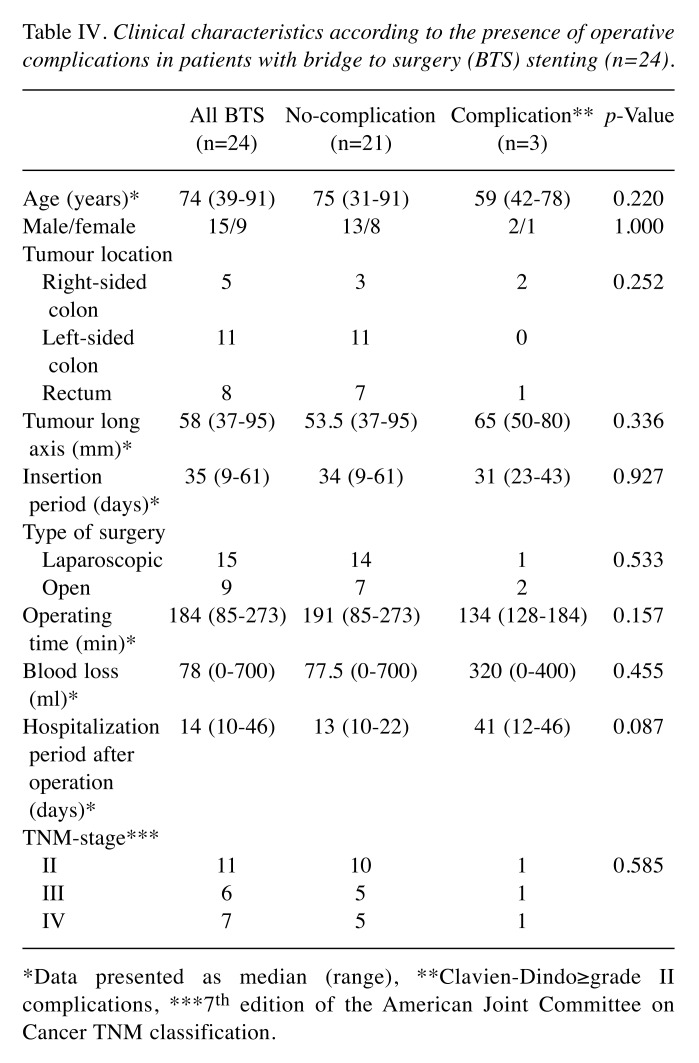
No significant differences in clinical characteristics were observed between patients with or without operative complications. Among BTS patients (n=24), 3 patients were found with complications of CDC grade II or higher; 2 of these patients showed anastomotic leakage. Analysis of patient characteristics and clinical features in the 24 BTS cases is shown in Table IV. When patients were divided into two groups according to the development of operative complications, no significant differences were found between the two groups in terms of preoperative factors including tumour location, tumour length and insertion period, as well as intraoperative factors, including operative time, blood loss and type of surgery. Pathological findings indicated no differences between the complication and no-complication groups in tumour depth, number of metastatic lymph nodes and lympho-vascular invasion.
Table IV. Clinical characteristics according to the presence of operative complications in patients with bridge to surgery (BTS) stenting (n=24).
*Data presented as median (range), **Clavien-Dindo≥grade II complications, ***7th edition of the American Joint Committee on Cancer TNM classification
Analyses of clinical factors related to stent placement and/or operative complications. The relationship between complications and clinical factors among stage II/III 17 BTS cases, including complications due to SEMS placement and/or operation (CDC Grade II or higher) is shown in Table V. Four out of 17 patients had complications. More details about the complications are presented in Table VI. Two patients developed anastomotic leakage, 1 developed ileus after operation, and the other 1 developed re-obstruction after SEMS placement. There were no significant differences in background, pre- and intra- operative factors, and pathological findings (Table V). There was also no significant difference in median observation periods between no-complication and complication group [45.5 months (range=29.6-69.7) vs. 35.5 months (range=19.1-61.6), respectively, p=0.350]. Two-year RFS rate was significantly higher in the no-complication group than in the complication group (100% vs. 75%, log-rank test, p<0.01).
Table V. Clinical characteristics according to the presence of stent placement and/or operative complications in stage II/III BTS patients (n=17).
*Data presented as median (range), **Data presented as negative/positive, ***Complication; Clavien-Dindo≥Grade II. Statistically significant values are shown in bold. RFS, Relapse-free survival
Table VI. Details of stent placement and/or operative complication (stage II/III).
SEMS, Self-expandable metal stent; Rec, recurrence; T, hepatic flexure of transverse colon; RS, rectum
Discussion
Our results showed the risk factors for SEMS placement and suggested that complications related to both SEMS placement and surgery may be risk factors for worse mid-term oncological outcomes. In terms of oncological outcomes, 2-year RFS rates in stage II/III BTS no-complication cases were significantly higher than in those who developed complications (100% vs. 75%, log-rank test, p<0.01).
The clinical success rates of SEMS placement differ from institution to institution according to the results of previous randomised controlled trials (RCTs). For favourable and unfavourable SEMS insertion, the rates range from 87.5-88.8%, and from 55.1-58.5%, respectively (13). Our data showed that the clinical success rate of SEMS placement in BTS patients was 87.5%, which is acceptable compared to previous reports (13,14). The major axis of the tumour (median=58 mm) and interval between SEMS insertion and surgery (median=34 days) (Table II) were longer than in previous reports, which described optimal time to operation as 10 days (6). In a previous study it was demonstrated that technical and clinical failures increase with stenotic length >40 mm (15). The perforation related to SEMS placement occurred at the bent portion of the sigmoid colon that required angular positioning (Figure 2), consistent with previously reported results (14). In consistence with previous reports (6,15,16), the result of multivariate analyses of this study suggested that long major axis of tumour, long interval between SEMS insertion and surgery, and angular positioning of the SEMS might be risk factors of complications related to stent placement.
Evaluation of the oncological outcomes in this study showed that the 2-year RFS rate was significantly higher in no-complication than complication cases of stage II/III BTS (Table IV). A recent report showed that although SEMS placement does not result in significantly worse oncological outcomes (17), disease recurrence is still a matter of concern (11,12,18). In this study, two cases with anastomotic leakage developed local recurrence. One of these 2 patients also experienced re-obstruction after SEMS placement before surgery, therefore we cannot conclude about the main reason for the local recurrence. However, obstruction and/or anastomotic leakage with cancer-bearing may affect the local recurrence.
This study has several limitations. First, this was a retrospective study with a small number of patients with obstructive CRC who were treated at a single institution. Second, we evaluated the 2-year RFS rate which is not long enough to clarify the mid-term oncological outcomes (19). Third, there was selection bias because 34 patients with obstructive CRC in the observation period underwent emergency surgery or inserted trans-anal decompression tube. Further research with a longer observation period using a prospective study design is needed.
A long major axis of the tumour, a long interval between SEMS insertion and surgery, and angular positioning of the SEMS may be risk factors of SEMS placement. Complications related to SEMS placement and/or surgery may be risk factors for worse mid-term oncological outcomes among patients who undergo SEMS placement as a BTS.
Conflicts of Interest
The Authors declare no competing interests.
Authors’ Contributions
Marie Hanaoka wrote the main manuscript text. Taichi Ogo, Yudai Kawamura, Tomiyuki Miura, Tomoki Aburatani, Hitoshi Sugimoto, Naoaki Hoshino, Tsunehito Yauchi, Yoshinobu Nishioka worked out the technical details. Tatsuyuki Kawano provided critical feedback. All authors discussed the result and commented on the manuscript.
References
- 1.Morris EJ, Taylor EF, Thomas JD, Quirke P, Finan PJ, Coleman MP, Rachet B, Forman D. Thirty-day postoperative mortality after colorectal cancer surgery in England. Gut. 2011;60:806–813. doi: 10.1136/gut.2010.232181. [DOI] [PubMed] [Google Scholar]
- 2.van den Berg MW, Sloothaak DA, Dijkgraaf MG, van der Zaag ES, Bemelman WA, Tanis PJ, Bosker RJ, Fockens P, ter Borg F, van Hooft JE. Bridge to surgery stent placement versus emergency surgery for acute malignant colonic obstruction. Br J Surg. 2014;101:867–873. doi: 10.1002/bjs.9521. [DOI] [PubMed] [Google Scholar]
- 3.Furuke H, Komatsu S, Ikeda J, Tanaka S, Kumano T, Imura K, Shimomura K, Taniguchi F, Ueshima Y, Takashina K, Lee CJ, Deguchi E, Ikeda E, Otsuji E, Shioaki Y. Self-expandable metallic stents contribute to reducing perioperative complications in colorectal cancer patients with acute obstruction. Anticancer Res. 2018;38(3):1749–1753. doi: 10.21873/anticanres.12411. [DOI] [PubMed] [Google Scholar]
- 4.Dohmoto M. New method: endoscopic implantation of rectal stent in palliative treatment of malignant stenosis. Endosc Dig. 1991;(3):1507–1512. [Google Scholar]
- 5.Tejero E, Mainar A, Femandez L, Tieso A, Cuezva JF, San Jose A. New procedure for relief of malignant obstruction of the left colon. Br J Surg. 1995;(82):34–35. doi: 10.1002/bjs.1800820113. [DOI] [PubMed] [Google Scholar]
- 6.van Hooft JE, van Halsema EE, Vanbiervliet G, Beets-Tan RGH, DeWitt JM, Donnellan F, Dumonceau JM, Glynne-Jones RGT, Hassan C, Jiménez-Perez J, Meisner S, Muthusamy VR, Parker MC, Regimbea JM, Sabbagh C, Sagar J, Tanis PJ, Vandervoort J, Webster GJ, Manes G, Barthet MA, Repici A. Self-expanded metal stents for obstructing colonic and extracolonic cancer: European Society of Gastrointestinal Endoscopy (ESGE) Clinical Guideline. Endoscopy. 2014;(46):990–1002. doi: 10.1055/s-0034-1390700. [DOI] [PubMed] [Google Scholar]
- 7.Fiori E, Crocetti D, Lamazza A, De Felice F, Tarallo M, Sterpetti AV, Mingoli A, Sapienza P, DE Toma G. Resection or stenting in the treatment of symptomatic advanced metastatic rectal cancer: A dilemma. Anticancer Res. 2019;39:6781–6786. doi: 10.21873/anticanres.13893. [DOI] [PubMed] [Google Scholar]
- 8.Zhang Y, Shi J, Shi B, Song CY, Xie WF, Chen YX. Self-expanding metallic stent as a bridge to surgery versus emergency surgery for obstructive colorectal cancer: a meta-analysis. Surg Endosc. 2012;(26):110–119. doi: 10.1007/s00464-011-1835-6. [DOI] [PubMed] [Google Scholar]
- 9.Pirlet IA, Slim K, Kwiatkowski F, Michot F, Millat BL. Emergency preoperative stenting versus surgery for acute left-sided malignant colonic obstruction: a multicenter randomized controlled trial. Surg Endosc. 2011;(25):1814–1821. doi: 10.1007/s00464-010-1471-6. [DOI] [PubMed] [Google Scholar]
- 10.Gorissen KJ, Tuynman JB, Fryer E, Wang L, Uberoi R, Jones OM, Cunningham C, Lindsey I. Local recurrence after stenting for obstructing left-sided colonic cancer. Br J Surg. 2013;(100):1805–1809. doi: 10.1002/bjs.9297. [DOI] [PubMed] [Google Scholar]
- 11.Knight AL, Trompetas V, Saunders MP, Anderson HJ. Does stenting of left-sided colorectal cancer as a “bridge to surgery” adversely affect oncological outcomes? A comparison with non-obstructing elective left-sided colonic resections. Int J Colorectal Dis. 2012;(27):1509–1514. doi: 10.1007/s00384-012-1513-8. [DOI] [PubMed] [Google Scholar]
- 12.Sabbagh C, Browet F, Diouf M, Cosse C, Brehant O, Bartoli E, Mauvais F, Chauffert B, Dupas JL, Nguyen-Khac E, Regimbeau JM. Is stenting as “a bridge to surgery” an oncologically safe strategy for the management of acute, left-sided, malignant, colonic obstruction? A comparative study with a propensity score analysis. Ann Surg. 2013;258(1):107–115. doi: 10.1097/SLA.0b013e31827e30ce. [DOI] [PubMed] [Google Scholar]
- 13.Hong SP, Kim TI. Colorectal stenting: An advanced approach to malignant colorectal obstruction. World J Gastroenterol. 2014;20(43):16020–16028. doi: 10.3748/wjg.v20.i43.16020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Huang X, Zhang S, Meng L. Preoperative colonic stents versus emergency surgery for acute left-sided malignant colonic obstruction: a meta-analysis. J Gastrointest Surg. 2015;18(3):584–589. doi: 10.1007/s11605-013-2344-9. [DOI] [PubMed] [Google Scholar]
- 15.Manes G, de Bellis M, Fuccio L, Repici A, Masci E, Ardizzone S, Mangiavillano B, Carlino A, Rossi GB, Occhipinti P, Cennamo V. Endoscopic palliation in patients with incurable malignant colorectal obstruction by means of self-expanding metal stent: analysis of results and predictors of outcomes in a large multicenter series. Arch Surg. 2011;146(10):1157–1162. doi: 10.1001/archsurg.2011.233. [DOI] [PubMed] [Google Scholar]
- 16.Lee JG, Yoo KH, Kwon CI, Ko KH, Hong SP. Angular positioning of stent increases bowel perforation after self-expandable metal stent placement for malignant colorectal obstruction. Clin Endosc. 2013;46(4):384–389. doi: 10.5946/ce.2013.46.4.384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Alcántara M, Serra-Aracil X, Falcó J, Mora L, Bombardó J, Navarro S. Prospective, controlled, randomized study of intraoperative colonic lavage versus stent placement in obstructive left-sided colonic cancer. World J Surg. 2011;35(8):1904–1910. doi: 10.1007/s00268-011-1139-y. [DOI] [PubMed] [Google Scholar]
- 18.Maruthachalam K, Lash GE, Shenton BK, Horgan AF. Tumour cell dissemination following endoscopic stent insertion. Br J Surg. 2007;94(9):1151–1154. doi: 10.1002/bjs.5790. [DOI] [PubMed] [Google Scholar]
- 19.Longo W E, Johnson FE. The preoperative assessment and postoperative surveillance of patients with colon and rectal cancer. Surg Clin North Am. 2002;82(5):1091–1108. doi: 10.1016/s0039-6109(02)00050-6. [DOI] [PubMed] [Google Scholar]
- 20.Matsuzawa T, Ishida H, Yoshida S, Isayama H, Kuwai T, Maetani I, Shimada M, Yamada T, Saito S, Tomita M, Koizumi K1, Hirata N, Sasaki T, Enomoto T, Saida Y. A Japanese prospective multicenter study of self-expandable metal stent placement for malignant colorectal obstruction: short-term safety and efficacy within 7 days of stent procedure in 513 cases. Gastrointest Endosc. 2015;82(4):697–707. doi: 10.1016/j.gie.2015.03.1978. [DOI] [PubMed] [Google Scholar]
- 21.Saito S, Yoshida S, Isayama H, Matsuzawa T, Kuwai T, Maetani I, Shimada M, Yamada T, Tomita M, Koizumi K, Hirata N, Kanazawa H, Enomoto T, Sekido H, Saida Y. A prospective multicenter study on self-expandable metallic stents as a bridge to surgery for malignant colorectal obstruction in Japan: efficacy and safety in 312 patients. Surg Endosc. 2016;30(9):3976–3986. doi: 10.1007/s00464-015-4709-5. [DOI] [PubMed] [Google Scholar]
- 22.Watanabe T, Muro K, Ajioka Y, Hashiguchi Y, Ito Y, Saito Y, Hamaguchi T, Ishida H, Ishiguro M, Ishihara S, Kanemitsu Y, Kawano H, Kinugasa Y, Kokudo N, Murofushi K, Nakajima T, Oka S, Sakai Y, Tsuji A, Uehara K, Ueno H, Yamazaki K, Yoshida M, Yoshino T, Boku N, Fujimori T, Itabashi M, Koinuma N, Morita T, Nishimura G, Sakata Y, Shimada Y, Takahashi K, Tanaka S, Tsuruta O, Yamaguchi T, Yamaguchi N, Tanaka T, Kotake K, Sugihara K. Japanese Society for Cancer of the Colon and Rectum (JSCCR) guidelines 2016 for the treatment of colorectal cancer. Int J Clin Oncol. 2018;23(1):1–34. doi: 10.1007/s10147-017-1101-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004;240(2):205–213. doi: 10.1097/01.sla.0000133083.54934.ae. [DOI] [PMC free article] [PubMed] [Google Scholar]