Abstract
Objective
Adolescents at risk for suicide are highly heterogeneous in terms of psychiatric and social risk factors, yet there has been little systematic research on risk profiles, which would facilitate recognition and the matching of patients to services. Our primary study aims were to identify latent class profiles of adolescents with elevated suicide risk, and to examine the association of these profiles with mental health service use (MHSU).
Method
Participants were 1,609 adolescents from the Emergency Department Screen for Teens at Risk for Suicide (ED-STARS) cohort. Participants completed baseline surveys assessing demographics, MHSU, and suicide risk. Telephone follow-up interviews were conducted at 3-months to assess suicide attempts. Participants met pre-established baseline criteria for suicide risk.
Results
Using latent class analysis, we derived five profiles of elevated suicide risk with differing patterns of eight risk factors: history of multiple suicide attempts, past-month suicidal ideation, depression, alcohol and drug misuse, impulsive-aggression, and sexual and physical abuse. In comparison to adolescents who did not meet baseline criteria for suicide risk, each profile was associated with increased risk of a suicide attempt within 3 months. MHSU was lowest for adolescents fitting profiles with previous (but no recent) suicidal thoughts and behavior and for adolescents from racial and ethnic minority groups.
Conclusion
Adolescents at elevated risk for suicide present to EDs with differing profiles of suicide risk. MHSU varies across these profiles and by race/ethnicity, indicating that targeted risk recognition and treatment linkage efforts may be necessary to reach some adolescents at risk.
Keywords: adolescence, suicide risk, mental health service use, latent class profiles
Introduction
In 2017, suicide was the second leading cause of death among US adolescents, ages 12 to 17 years.1 Further, approximately 17.2 percent of high school students reported having seriously considered making a suicide attempt in the past year, including 22.1% of female and 11.9% of male students.2 The rate of suicide among adolescents has increased substantially since 2000,3 with increases from 1.9 to 4.0 (per 100,000) for adolescent girls and 6.6 to 9.6 for adolescent boys,1 and a concomitant increase in visits to emergency departments (EDs) for adolescent suicidal behavior.4 These increases have occurred despite national prioritization of suicide prevention.
Youth suicide risk factors encompass emotional, behavioral, and psychosocial concerns.5,6 A history of a previous suicide attempt or other self-harmful behavior predicts future attempts, and the risk for attempts increases with the frequency of previous self-harmful behavior.7–9 Depression is a risk factor for suicide attempts,10 repeat suicide attempts,11 and suicide.12 Alcohol abuse, drug use, and patterns of aggressive behavior are other primary risk factors.7,8 The risk of suicide attempts increases as substance use increases, and when substance use is associated with multiple risky behaviors.13 Moreover, the likelihood of repeated suicide attempts increases with the severity of aggressive/violent behavior and substance abuse.14 Childhood maltreatment, specifically sexual abuse, physical abuse, emotional abuse, and emotional neglect, has also been associated with suicide attempts in multiple studies.15
Many youth at elevated risk for suicide, including those who die by suicide, receive no mental health (MH) services.6 When MH services are obtained, this is often after the onset of suicidal behavior.9 Under-treatment is particularly prominent among racial and ethnic minority youth.16 Knowledge of the differing presentations or profiles of youth at high risk for suicide may help us to recognize youth for whom proactive screening is necessary for identification and subsequent intervention. Latent class analyses (LCA) enables us to more systematically identify distinct profiles of risk, taking into consideration well-established risk factors for adolescent suicide. LCA is an approach that uses patterns of characteristics to identify mutually exclusive subgroups that are not directly observable (“latent”). Previous studies have used LCA to examine profiles of youth suicide risk in primary care17 and school-based samples,18 and point to the importance of experiences such as sexual abuse.18 Psychological autopsy studies of youth who died by suicide, which entail interviews with significant others and review of social, legal, and medical records, also provide evidence for the existence of differing profiles.19,20 In these studies, substance or alcohol abuse was more common among male participants19,20 and older adolescents,20 depression was more common among the female participants,19 conduct disorder was more common among male participants,20 and expressed suicidal intent was less common among younger adolescents who died by suicide.20
Previous studies have not, however, used a comprehensive inventory of behavior, mental health, substance use, adaptive functioning and social risk factors (e.g., childhood sexual abuse) to develop distinct suicide risk profiles among youth seen in pediatric EDs. The objectives of this study are: (1) to identify distinct profiles of youth at elevated risk for suicide, and (2) to examine the association of these profiles with history of mental health service use (MHSU).
Method
Participants and Procedures
Study data are from the Emergency Department Screening for Teens at Risk for Suicide (ED-STARS) Study One cohort of 6,536 adolescents (ages 12 to 17) recruited from 13 pediatric EDs between June, 2015 and July, 2016.21 These EDs were members of the Pediatric Emergency Care Applied Research Network (PECARN) and spanned diverse geographic regions of the US. Recruitment was conducted during randomly assigned screening shifts. Among the 16,060 patients identified as study eligible, 10,554 patients (66%) were approached for possible study participation and 6,536 were recruited (62.0% of approached patients). Exclusion criteria were: (1) ward of State, (2) previously enrolled, (3) non-English speaking, (4) medically unstable, and (5) severe cognitive impairment.
Written informed consent and assent were obtained from parents (legal guardians) and adolescents, respectively. Adolescents completed a self-report suicide risk survey, and parents completed a brief survey regarding their child’s behavioral problems, adaptive functioning, and MHSU. Adolescents received a $15 gift certificate for participation. Procedures were approved by each site’s Institutional Review Board.
To identify profiles of elevated suicide risk, this study used the baseline subsample of 1,609 adolescents from ED-STARS who met the study’s baseline criteria for “high risk” for suicide attempt, which was defined by the presence of one or more of the following: suicidal ideation with intent and/or plan,22 history of one or more suicide attempts,9 non-suicidal self-injury (NSSI) five or more times in past year,23 or homicidal ideation with current intent or plan.7 This subsample was 24.5% (395/1,609) male participants with a mean age of 15.2 years (SD = 1.5) and the following racial distribution: White 59.4% (882/1,484), Black 24.0% (356/1,484), Multi-racial 7.1% (106/1,484), Unknown 6.1% (90/1,484), American Indian/Alaska Native 1.6% (24/1,484), Asian 0.9% (13/1,484), Pacific Islander 0.9% (13/1,484). Their ethnic distribution was 22.7% (340/1,500) Latinx, 70.7% (1061/1,500) not Latinx, and 6.6% (99/1,500) Unknown. Levels of education for mothers/stepmothers and fathers/stepfathers, respectively, were as follows: high school graduate or less 31.8% (488/1,535) and 42.3% (647/1,528), some college/technical 28.5% (437/1,535) and 19.1% (292/1,528), college graduate 37.2% (571/1,535) and 27.3% (417/1,528), and Unknown 2.5% (39/1,535) and 11.3% (172/1,528). Forty-six percent (697/1,523) of families were receiving some form of public assistance (e.g., food stamps, Medicaid).
To validate our baseline “high risk” for suicide attempt criteria, we examined the likelihood of a suicide attempt outcome between adolescents completing follow-up who did (n = 1,054, 47%) and did not (n = 1,205, 53%) meet these “high risk” criteria at baseline. The demographic characteristics of these “high risk” and “low/moderate risk” groups are provided in Supplement 1.
Measures
The self-report survey included 92 primary and 27 follow-up questions. Measures represented in the final LCA model are described in this section. Supplement 2 provides additional psychometric information for these and other measures considered in LCA models.
History of Mental Health Service Utilization
We asked parents/guardians questions at baseline to assess youth: (1) history of psychiatric hospitalization; (2) medication for mental health concern; (3) outpatient psychotherapy/psychosocial intervention. Response options were Yes/No for lifetime and past month. The primary reason for the ED visit was coded as psychiatric or non-psychiatric.
Suicidal Ideation, History of Multiple Suicide Attempts
The severity of youth’s suicidal thoughts was assessed with the Suicide Severity Scale of the Columbia-Suicide Severity Rating Scale (C-SSRS), which includes five items related to suicidal thoughts (scores range from 0 to 5).24 Adolescents also completed an adapted version of the C-SSRS Behavior scale, which includes yes/no questions about suicidal behaviors at baseline, 3-month, and 6-month follow-up. A suicide attempt was defined as a positive response to one of the following: “In the past 3 months (or since the last assessment), have you made a suicide attempt?”, “In the past 3 months (or since the last assessment), have you tried to harm yourself because you were at least partly trying to end your life?”, or if the adolescent or parent indicated that the adolescent had visited an emergency department or been hospitalized with suicide attempt as the most immediate concern.
The Ask Suicide-Screening Questions (ASQ), a 4-item self-report screen, was also used to assess lifetime history of suicide attempt at baseline.25 A suicide attempt was defined as a “yes” to a history of suicide attempt question on the C-SSRS or the ASQ.
Depression, Alcohol Use, Drug Use
Depression was assessed by the Patient Health Questionnaire (PHQ-9).26 The Alcohol Use Disorders Identification Test- Consumption (AUDIT-C) was used to assess at-risk drinking and alcohol consumption in the past year,27 and the National Institute on Drug Abuse – Modified Alcohol, Smoking and Substance Involvement Screening Test version28 of the Drug Use Scale (DUS) assessed frequency of use during the past 3 months for multiple drug categories. In the LCA, we included dichotomous variables to indicate whether or not the youth scored 3 or higher on the AUDIT-C and whether or not the youth had used cannabis at least monthly during the past 3 months.
Aggression
The Impulsive-Aggression (IA) Quick Screen is a 1-item screen from the Impulsive Premeditated Aggression Scale (IPAS):29 “Over the past three months, have you had times when you became angry and enraged with others in a way that was out-of-control or inappropriate?” “Yes” responses are followed by a question about if they have done any of the following during these times: verbally attacked someone, thrown or destroyed objects, physically attacked someone. The score is the number of these items endorsed.
Childhood Sexual and Physical Abuse
Abuse was assessed with a brief two-item screener derived from the Childhood Trauma Questionnaire (CTQ-SF).30 which has been used previously with adolescents and has excellent sensitivity and specificity for identifying childhood abuse. It uses an adapted Yes/No response format: “People in my family have hit me so hard that it left me with bruises or marks.” and “Someone has tried to touch me in a sexual way or tried to make me touch them.”
Data Analyses
As a check on the baseline criteria for assignment in the “high risk” cell, which was a requirement for inclusion in LCA analyses for the present study, we calculated the association between baseline cell assignment (low/moderate risk versus high risk) and suicide attempt (yes/no) during the 6-month follow-up.
We used LCA to identify latent classes underlying the observed data based on both continuous measures (suicidal ideation, depression, aggression) and binary indicators (history of suicide attempts, alcohol and drug use, and history of sexual and physical abuse). The resulting classes are subgroups of adolescents who display similar patterns. Products of this analysis include estimates of the proportion having each categorical characteristic and the mean response for numeric measures within each latent class. We began by including six candidate variables: suicidal ideation, history of multiple suicide attempts, depression, aggression, alcohol use, and cannabis use, which we identified a priori as important for consideration based on the extant research literature.5 Next, other candidate variables (e.g., history of sexual abuse, parent/family connectedness, NSSI, peer victimization, among others) were added to the model and assessed for theoretical fit and contribution to the model (i.e., modification of classes). Selection of final LCA model was made prior to any other analyses.
LCAs were conducted in Mplus version 7.431 using the Mplus Automation package in R language and environment.32 We considered the possibility of up to six latent classes, limiting the total number to increase the likelihood that each class would characterize a meaningful percentage of adolescents. Full information maximum likelihood was used to handle missing data. Model fit was evaluated using Bayesian information criterion (BIC). Summaries and statistical tests were performed using SAS software version 9.4.33 We compared latent classes (using chi-square tests for categorical variables and Kruskal-Wallis tests for numeric variables) with respect to demographics, then compared classes with respect to MHSU using single- and multi-variable logistic regression and adjusting for age, sex, race, and ethnicity. For these analyses, adolescents were placed in the latent class with the highest posterior probability of membership.
Finally, we calculated univariable associations between the five latent class profiles for elevated suicide risk (and the low/moderate risk group) and suicide attempts during the 6-month follow-up period. Odds ratios and 95% confidence intervals are reported for these associations.
Results
Specific Study Sample
A total of 1,609 youth from the ED-STARS Study One sample of 6,536 youth (24.6%) met baseline criteria for a “high risk” designation and, therefore, inclusion in this profile analysis. Within this “high risk” subsample, 1,339 (84%) were randomized to follow-up and 1,054 (79%) were retained for 3-month and/or 6-month follow-up. The remaining 4,927 youth met baseline criteria for either “low” or “moderate” risk or did not complete the baseline assessment; 1,506 (31%) of these youth were randomized to follow-up, and 1,205 (80%) were retained for 3-month and/or 6-month follow-up. The retention rates for youth designated for “high risk” (79% retention rate) versus low/moderate risks cells (80% retention rate) at baseline did not differ (p=0.39). Overall, 79% of youth had at least one follow-up interview (2,259/2,845). This includes 1,787 subjects with 3-month and 6-month follow-up interviews, 288 adolescents with 3-month follow-up interviews only, and 184 adolescents with 6-month follow-up interviews only.
Latent Classes of Suicide Risk
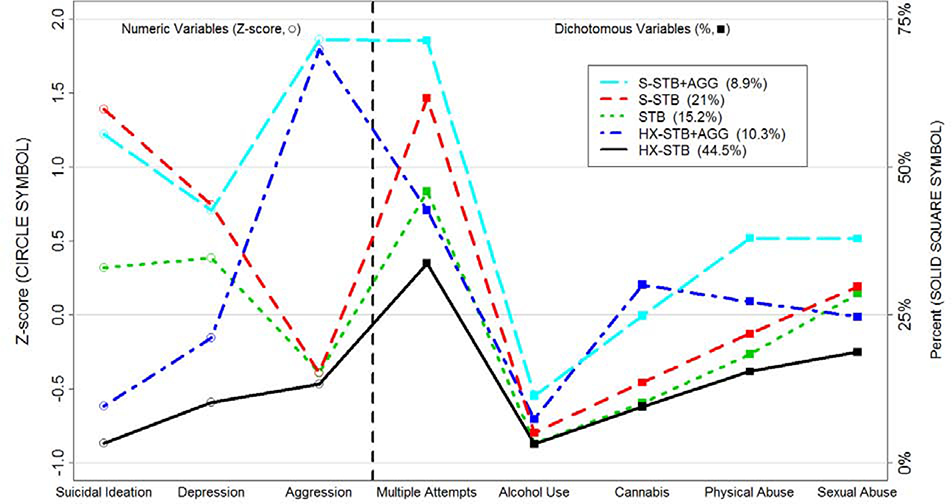
In the final LCA model, which we examined using the 1,609 youth who met “high suicide risk” criteria at baseline in ED-STARS Study One, we identified five latent class profiles using eight suicide risk factors (Figure 1). This model had the lowest BIC and highest entropy (0.97, indicating clear class distinctions) of the models considered.34 The defining characteristics and frequency of these 5 classes were: (1) Severe Suicidal Thoughts and Behavior plus Aggression (S-STB+AGG, 9%); (2) Severe Suicidal Thoughts and Behavior (S-STB, 21%); (3) Suicidal Thoughts and Behaviors (STB, 15%); (4) History of Suicidal Thoughts and Behavior plus Aggression (HX-STB+AGG, 10%); and (5) History of Suicidal Thoughts and Suicidal Behavior (HX-STB, 45%); see Table 1. The fit statistics for models with three, four, and five classes are in Table S1, available online. Figure 2 illustrates key defining characteristics of the latent classes: whether or not the youth reported current (versus past only) STB, the severity of STB, and the presence of aggressive behavior.
Figure 1.
Five Latent Class Profiles of Adolescent Suicide Risk.
Note: This figure illustrates five distinct profiles of suicide risk among adolescents presenting to pediatric emergency departments. These profiles were based on differing patterns of eight suicide risk factors: suicidal ideation, history of multiple suicide attempts, depression, impulsive-aggression, alcohol and drug use, and history of sexual and physical abuse.
Table 1.
Defining Characteristics of Five Latent Classes of Suicide Risk a
| Latent Class Assignment b |
|||||
|---|---|---|---|---|---|
| S-STB+AGG (n = 142) (9%) | S-STB (n = 342) (21%) | STB (n = 239) (15%) | HX-STB+AGG (n = 164) (10%) | HX-STB (n = 722) (45%) | |
| C-SSRS: Multiple attempts | 98 (71%) | 205 (62%) | 107 (45%) | 69 (42%) | 238 (34%) |
| AUDIT-C: Score ≥ 3 | 24 (17%) | 23 (7%) | 10 (4%) | 26 (16%) | 37 (5%) |
| DUS: Used cannabis ≥ monthly (past 3 months) | 35 (25%) | 46 (14%) | 24 (10%) | 49 (30%) | 69 (10%) |
| C-SSRS: Suicide Severity Score (past month) Mean (SD) | 4.3 (0.84) | 4.7 (0.47) | 2.5 (0.50) | 0.6 (0.84) | 0.1 (0.33) |
| IA-Quick Screen, Mean (SD) | 2.4 (0.49) | 0.3 (0.44) | 0.3 (0.44) | 2.4 (0.48) | 0.2 (0.39) |
| History Physical Abuse | 53 (38%) | 74 (22%) | 44 (19%) | 44 (27%) | 110 (15%) |
| History Sexual Abuse | 53 (38%) | 100 (30%) | 68 (29%) | 40 (25%) | 134 (19%) |
| PHQ9: Total Score Depression | 17.8 (7.07) | 18.1 (6.08) | 15.4 (6.33) | 11.3 (6.22) | 8.2 (5.79) |
| Severity: Mean (SD) | |||||
Note: S-STB+AGG= Severe Suicidal Thoughts/Behavior + Aggression; S-STB= Severe Suicidal Thoughts/Behavior; STB= Suicidal Thoughts/Behavior; HX-STB+AGG= History of Suicidal Thoughts/Behavior + Aggression; HX-STB= History of Suicidal Thoughts/Behavior; C-SSRS= Columbia-Suicide Severity Rating Scale; AUDIT-C=Alcohol Use Disorders Identification Test; DUS: Drug Use Scale; IA-Quick Screen: Impulsive Aggression Quick Screen; PHQ9=Patient Health Questionnaire-9.
All measures differed at p-value of <.001 for latent classes (chi-squared and Kruskal-Wallis tests).
N’s for calculating percentages varied from 138–141 for S-STB+AGG, 331–339 for S-STB, 237–241 for STB, 162–165 for HX-STB+AGG, and 702 to 720 for HX-STB.
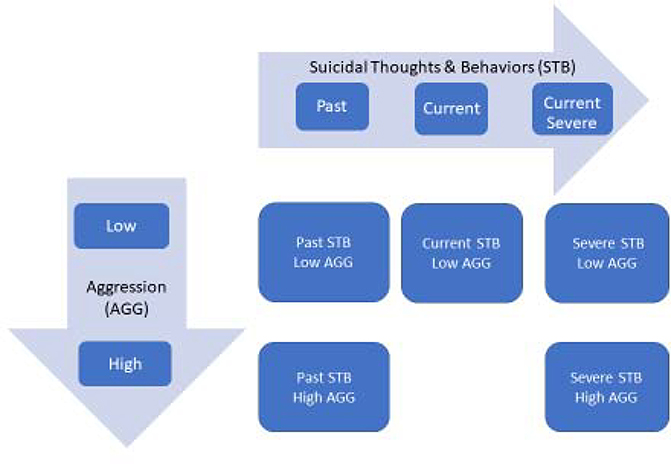
Figure 2.
Characterization of the Five Risk Profiles Obtained by Latent Class Analysis.
Note: The five profiles are defined by two main axes. First, with respect to suicidal ideation and behavior, there were those who reported no current suicidal ideation and behavior, but had a history of suicidal ideation and behavior, those with current suicidal ideation that was less severe (ie, without intent or plan) and those with suicidal ideation that was characterized by more severity (ie, with intent). Second, the groups were differentiated by the presence or absence of significant aggressive behavior. Figure 2 shows the names of the groups and where the groups fit within these two dimensions.
The majority of youth in the two classes labeled with “Severe” Suicidal Thoughts and Behavior reported multiple suicide attempts (71% and 62% of S-STB+AGG and S-STB classes, respectively). Similarly, the majority of youth in these classes reported suicidal ideation with a plan and/or suicidal intent. A majority of adolescents in the HX-STB, HX-STB+AGG classes, which were least likely to report current STB, reported a previous suicide attempt (64%). In addition, many of the adolescents in these two classes reported a history of multiple suicide attempts (34% of HX-STB and 42% of HX-STB+AGG profiles), and nearly all (82%) reported a lifetime history of suicidal thoughts. In fact, adolescents with the HX-STB+AGG profile were just as likely as adolescents with the STB profile to report a history of multiple suicide attempts. Moreover, among adolescents best described by the HX-STB+AGG profile, 30% had recently used cannabis, most reported aggressive outbursts and significant depressive symptoms, 25% reported a history of sexual abuse, and 24% reported homicidal ideation. Additional information about the five classes is provided in Table 2.
Table 2.
Suicidal Ideation, Homicidal Ideation, and Suicide Attempts for Youth in Each Latent Class
| Latent Class Assignment | |||||
|---|---|---|---|---|---|
| Baseline Question/Score | S-STB+AGG (n = 142) | S-STB (n = 342) | STB (n = 239) | HX-STB+AGG (n = 164) | HX-STB (n = 722) |
| Have you ever in your life made a suicide attempt? a | 118 (83%) | 276 (81%) | 172 (72%) | 109 (66%) | 459 (64%) |
| In the past month, have you made a suicide attempt? b | 77 (54%) | 208 (61%) | 64 (27%) | 18 (11%) | 47 (7%) |
| In the past month, have you had any thoughts about wanting to kill someone else? | 45 (32%) | 50 (15%) | 27 (11%) | 40 (24%) | 46 (6%) |
| Do you currently have any intent or plan to kill someone? | 7 (5%) | 11 (3%) | 3 (1%) | 8 (5%) | 8 (1%) |
| In the past 12 months, have you ever harmed or hurt your body on purpose? (5 or more times) | 62 (44%) | 133 (39%) | 73 (31%) | 38 (23%) | 91 (13%) |
| Lifetime Suicide Ideation Severity Score: Mean (SD) | 4.6 (0.70) | 4.8 (0.46) | 3.6 (1.15) | 3.3 (1.59) | 2.8 (1.81) |
Note: S-STB+AGG= Severe Suicidal Thoughts/Behavior + Aggression; S-STB= Severe Suicidal Thoughts/Behavior; STB= Suicidal Thoughts/Behavior; HX-STB+AGG= History of Suicidal Thoughts/Behavior + Aggression; HX-STB= History of Suicidal Thoughts/Behavior.
Youth reported lifetime suicide attempt on the Columbia-Suicide Severity Rating Scale (C-SSRS) and/or the Ask Suicide-Screening Questions (ASQ).
Youth endorsed past month suicide attempt on C-SSRS.
The likelihood of a suicide attempt prior to 6-month follow-up was 14.3% (151/1054) for the youth who met the study’s “high suicide risk” criteria at baseline in comparison to 0.8% (10/1205) for the remaining ED-STARS Study One subjects who participated in follow-up interviews (OR=19.98; 95% CI, 10.48 – 38.12; p < 0.001). Table 3 reports the likelihood of a suicide attempt prior to follow-up for each of the five high suicide risk profiles, comparing this to the likelihood of a suicide attempt for adolescents designated as low/moderate risk at baseline. Each of the five high suicide risk profiles was associated with a significantly increased likelihood of suicide attempt. This likelihood was highest for the two groups in classes with severe STB at baseline. Specifically, the suicide attempt rates were 28.0% (23/82) for the S-STB+AGG group, with an unadjusted odds ratio of 46.6 (CI: 21.2, 102.3), and 26.1% (62/238) for the S-STB group, with an unadjusted odds ratio of 42.1 (CI: 21.2, 83.6). The profile with the lowest suicide attempt rate (6.6%, 31/469) was the HX-STB profile.
Table 3.
Adolescents in High Suicide Risk Classes Versus Low/Moderate Risk Group at Baseline: The Likelihood of Suicide Attempt by 6-Months
| Group | Attempt | No Attempt | Odds Ratio (95% CI) | p |
|---|---|---|---|---|
| Six Months | <.001 | |||
| High: S-STB+AGG | 23/82 (28.0%) | 59/82 (72.0%) | 46.58 (21.20, 102.34) | |
| High: S-STB | 62/238 (26.1%) | 176/238 (73.9%) | 42.10 (21.19, 83.63) | |
| High: STB | 22/160 (13.8%) | 138/160 (86.2%) | 19.05 (8.84, 41.06) | |
| High: HX-STB+AGG | 13/105 (12.4%) | 92/105 (87.6%) | 16.89 (7.21, 39.56) | |
| High: HX-STB | 31/469 (6.6%) | 438/469 (93.4%) | 8.46 (4.11, 17.40) | |
| Low/Moderate | 10/1205 (0.8%) | 1195/1205 (99.2%) | (reference) |
Adolescent demographics in relation to the five latent classes are displayed in Table S2 (Online Supplement). Adolescents were differentially distributed across latent classes by race and paternal education. White youth (25%) and youth whose fathers had completed college (29%) were more likely to be described by the S-STB profile than Black youth (13%) and youth whose fathers had completed some college or less (18%). A higher proportion of Black (65%) versus White youth (50%) was described by HX-STB+AGG and HX-STB profiles.
Mental Health Service Utilization
Each type of mental health service utilization (psychiatric hospitalization, outpatient psychotherapy, medication, ED visit with psychiatric chief complaint) varied by latent class (p-values < 0.01; Table 4; See Table S3 in online Supplement for past month MHSU). Relative to adolescents characterized by the HX-STB profile, adolescents characterized by S-STB+AGG, S-STB, and HX-STB+AGG profiles had higher odds of psychiatric hospitalization; adolescents characterized by S-STB+AGG, S-STB, STB, and HX-STB+AGG profiles had higher odds of medication use; and those characterized by S-STB+AGG and S-STB had higher odds of a lifetime history of outpatient psychotherapy.
Table 4.
Lifetime Mental Health Service Utilization and Reason for Emergency Department (ED) Visit in Relation to Demographics and Latent Classes (Adjusted Odds Ratios [OR])
| Psychiatric Hospitalization | Psychiatric Medication | Outpatient Therapy | ED Visit – Psychiatric Complaint | |||||
|---|---|---|---|---|---|---|---|---|
| OR | p | OR | p | OR | p | OR | p | |
| Age in years | 0.98 (0.91, 1.07) | 0.70 | 1.04 (0.96, 1.12) | 0.30 | 1.05 (0.97, 1.14) | 0.27 | 0.92 (0.84, 1.00) | 0.049 |
| Sex | 0.06 | 0.49 | 0.63 | 0.054 | ||||
| Male Participants | (reference) | (reference) | (reference) | (reference) | ||||
| Female Participants | 1.33 (0.99, 1.78) | 0.91 (0.70, 1.18) | 0.93 (0.70, 1.24) | 0.74 (0.55, 1.00) | ||||
| Race | 0.08 | <.001 | <.001 | 0.09 | ||||
| White | (reference) | (reference) | (reference) | (reference) | ||||
| Black | 0.69 (0.50, 0.95) | 0.33 (0.25, 0.45) | 0.30 (0.22, 0.41) | 0.73 (0.52, 1.02) | ||||
| Other/Unknown | 0.87 (0.59, 1.27) | 0.70 (0.50, 0.99) | 0.83 (0.57, 1.21) | 0.74 (0.50, 1.09) | ||||
| Ethnicity | 0.12 | <.001 | <.001 | 0.08 | ||||
| Not Hispanic/Latino | (reference) | (reference) | (reference) | (reference) | ||||
| Hispanic or Latino | 0.68 (0.47, 0.98) | 0.52 (0.38, 0.71) | 0.44 (0.31, 0.61) | 0.69 (0.48, 1.00) | ||||
| Unknown | 0.96 (0.55, 1.66) | 1.01 (0.61, 1.67) | 0.75 (0.44, 1.25) | 1.22 (0.72, 2.07) | ||||
| Latent Classes | <.001 | <.001 | 0.003 | <.001 | ||||
| HX-STB | (reference) | (reference) | (reference) | (reference) | ||||
| HX-STB+AGG | 1.70 (1.11, 2.58) | 1.94 (1.30, 2.88) | 1.50 (0.98, 2.32) | 2.50 (1.62, 3.88) | ||||
| STB | 0.99 (0.66, 1.47) | 1.53 (1.09, 2.15) | 1.25 (0.87, 1.81) | 7.43 (5.21, 10.61) | ||||
| S-STB | 1.76 (1.28, 2.43) | 1.92 (1.42, 2.59) | 1.71 (1.21, 2.41) | 29.30 (20.23, 42.44) | ||||
| S-STB+AGG | 2.60 (1.70, 3.97) | 3.22 (2.06, 5.03) | 2.15 (1.29, 3.60) | 23.43 (14.38, 38.17) | ||||
Note: 95% Confidence intervals provided for odds ratios. S-STB+AGG= Severe Suicidal Thoughts/Behavior + Aggression; S-STB= Severe Suicidal Thoughts/Behavior; STB= Suicidal Thoughts/Behavior; HX-STB+AGG= History of Suicidal Thoughts/Behavior + Aggression; HX-STB= History of Suicidal Thoughts/Behavior.
Sixty percent of this study’s sample of 1,609 youth at high risk for suicide (n = 959) did not present to the ED with a psychiatric chief complaint, and the likelihood of presenting with such a complaint differed substantially across latent classes: S-STB+AGG, 79% (95% CI, 71%−85%); S-STB, 81% (95% CI, 76%−85%); STB, 52% (95% CI, 46%−59%); HX-STB+AGG, 28% (95% CI, 21%−36%); HX-STB, 13% (95% CI, 10%−15%). Adolescents characterized by HX-STB were the least likely to present to the ED with a psychiatric chief complaint. Relative to this class, the odds ratios for presenting with a psychiatric chief complaint for other classes were: HX-STB+AGG (OR=2.50; 95% CI, 1.62–3.88), STB (OR=7.43; 95% CI, 5.21–10.61), S-STB+AGG (OR=23.4; 95% CI, 14.4–38.2), and S-STB (OR=29.3; 95% CI, 20.2–42.4). The confidence intervals for these odds ratios are non-overlapping for all classes except S-STB+AGG and S-STB, which both had a very high likelihood of presenting with a psychiatric chief complaint.
Discussion
In keeping with our first study objective, we identified five distinct profiles of suicide risk among adolescents presenting to pediatric EDs with elevated risk for suicide. These profiles were based on differing patterns of eight suicide risk factors: suicidal ideation, history of multiple suicide attempts, depression, impulsive-aggression, alcohol and drug use, and history of sexual and physical abuse. To our knowledge, this is the first study to use LCA to systematically address the heterogeneity of adolescent clinical presentations associated with elevated suicide risk. Moreover, in comparison to adolescents who were not designated as “high risk” at baseline, each “high risk” profile was associated with an increased likelihood of a suicide attempt within six months of the ED visit, supporting the validity of the “high risk” designation used to define this study’s sample. In keeping with our second study objective, we examined the association of these profiles with history of mental health service use (MHSU). Results indicated that the likelihood of MHSU varied across risk profiles, suggesting that subgroups of adolescents at risk may either require proactive screening for suicide risk recognition or more proactive facilitation of engagement with MH services following recognition.
Lifetime MHSU was the lowest, across types of services, for adolescents characterized by the HX-STB profile. Because 64% (459/722) of these adolescents reported a history of suicide attempt and all of them met one or more criteria for high suicide risk at the time of their ED visit, this low rate of lifetime MHSU is concerning. It could be due to a perceived stigma associated with sharing past MH services as well as inadequate assessment and mental health linkage procedures in EDs currently, which has been documented.35 Other potential reasons for the low rate of lifetime MHSU include barriers associated with poverty;36 the shortage of child and adolescent psychiatrists;37 lack of parental awareness of youth mental health symptoms;38 and other family-related factors.39
The majority of adolescents in this study (60%), all of whom screened positive for suicide risk, did not present to the ED with a psychiatric chief complaint. Moreover, the adolescents who matched profiles characterized by little or no current suicidal thoughts and no recent suicidal attempt (HX-STB+AGG and HX-STB) were the least likely to present to the ED with a psychiatric complaint. This is despite the fact that the majority of these adolescents reported a previous suicide attempt, many (34% and 42% of adolescents with HX-STB and HX-STB+AGG profiles, respectively) reported a history of multiple suicide attempts, and nearly all (82%) reported a lifetime history of suicidal thoughts. Among adolescents characterized by the HX-STB+AGG profile, the co-occurrence of other suicide risk factors such as cannabis use, aggressive outbursts, sexual abuse was not uncommon.5 This is concerning and suggest the possible value of universal suicide risk screening. Given that approximately 19% of adolescents, ages 12 to 17 years, visit a hospital ED for services in a one-year period,40 the ED setting has substantial potential as a site for suicide risk screening and linkage to mental health services. Support for screening includes favorable feasibility studies,41,42 favorable attitudes by parents and adolescents toward suicide risk screening in general EDs,43 and the potential to identify adolescents with previously unrecognized suicide risk who are receiving no MH services.42
Although suicidal ideation is a well-established suicide risk factor,5 study findings suggest that screening questions about current suicidal ideation or a recent suicide attempt are insufficient if used as the sole triage or “go-no go” questions for determining whether or not a youth may be at risk for suicide. As seen in this study and others, not all individuals who make suicide attempts report current suicidal ideation.9 Furthermore, suicidal ideation is only a modest predictor of suicide attempts within clinical samples of adolescents and has failed to predict suicide attempts among adolescent males in the year following their psychiatric hospitalization.44 A computerized adaptive screen, which is under development in the ED-STARS study,21 may be more effective in identifying the full range of youth at risk for suicidal behavior. Further research is also recommended to examine the longitudinal trajectories of youth who report a past history of suicide risk only. They may represent a subgroup that denies current problems for fear of intervention, being stigmatized by self or others, or a loss of freedom if hospitalized.
Our study sample was comprised entirely of adolescents who were known to be at elevated risk for suicide based on previously identified risk factors. Nevertheless, the fact that 46% of the sample reported a history of multiple suicide attempts is striking. The rate varied from a low of 34% for the HX-STB profile to a high of 71% for the S-STB+AGG profile. The overall high rate for this sample is consistent with that documented by a recent study that sampled psychiatrically hospitalized adolescents and reported a similar multiple attempt rate of 53%.45 It is also notable that sexual and physical abuse characterized a significant minority of adolescents who fit each of the five identified profiles, which is consistent with results from a recent meta-analysis of the association between childhood maltreatment and suicide risk.15 These findings suggest that, although profile characteristics varied, all youth in our sample were at elevated risk, pointing to the importance of better understanding issues of mental health service utilization.
In this study, race was differentially distributed across latent classes. There were small proportions of Black adolescents in S-STB+AGG and S-STB classes, which were the classes most likely to have a history of MHSU and to present to the ED with a psychiatric chief complaint. Thus, the difference in MHSU by race parallels the difference in the distribution of latent class profiles for MHSU. The disparities in MHSU for minority groups have been well documented.16 It is important to understand the factors that influence clinicians’ and caregivers’ decisions on the need to use mental health care for their patients and children, and barriers to access these services.
This study had multiple strengths including its large sample size; the recruitment of adolescents from 13 pediatric EDs in PECARN, which were characterized by geographic, racial/ethnic, and economic diversity; and the broad range of risk factors available for LCA. Findings should be considered, however, within the context of study limitations. This study was conducted in the pediatric EDs of large academic health systems, which are not representative of all medical EDs, including those of smaller community hospitals. In addition, because we were assessing a broad range of risk factors and working within the time and space constraints of EDs, with a consideration of patient burden, many risk factors were assessed with brief, adapted scales. In addition, the choices we made in limiting variables for the LCA may differ from those of other investigators, as it is possible to examine multiple iterations. Although more than half of the adolescents who screened positive for suicide risk did not present to the ED with a psychiatric chief complaint, it is possible that some of them had another chief complaint yet did receive psychiatric help. Also, if we only rely on lifetime MHSU, it is not possible to know if these services occurred before or after the STB. We also do not have information about diagnosed psychiatric disorders, which could be expected to impact MHSU. Finally, our LCA profile descriptors use simple summaries to capture multidimensional concepts and do not perfectly characterize each individual within those groups. For example, a non-negligible proportion of adolescents in the HX-STB class had multiple suicide attempts.
Addressing the heterogeneity of clinical presentations among adolescents at elevated risk for suicide attempts, we identified five profiles of adolescents at risk with differing patterns of risk factors. MHSU was relatively common among adolescents characterized by the profiles with recent and severe suicidal thoughts and behavior, with or without aggression. However, MHSU was much less common among adolescents who only reported a history of suicidal thoughts and behavior, despite the fact that many of these youth had a lifetime history of multiple suicide attempts and/or other known suicide risk factors. MHSU was also lower among adolescents from racial and ethnic minority groups. In addition to implementing effective strategies for the recognition of suicide risk, this suggests the importance of facilitating treatment engagement and retention. Some of the strategies found to be helpful include the incorporation of motivational interviewing principles and attention to family stress, family coping, and broader family system issues.46 Care navigators47 and matching the race and ethnicity of clinical providers and families may also be helpful.48 Finally, a recent review of 50 randomized controlled trials examining the effectiveness of treatment engagement interventions for child mental health services (conducted 1974 – 2016) concluded that specific interventions can improve engagement and work across youth with varying racial and ethnic identifications, and mental health problems.49
Summary
This study identified five distinct profiles of suicide risk among adolescents that were associated with differing patterns of MHSU. Lifetime MHSU was the lowest for adolescents identified at high risk for suicide who did not report current suicidal ideation or a recent suicide attempt, and for adolescents from racial and ethnic minority groups. Because adolescents who engage in suicidal behavior are highly heterogeneous, this identification of profiles or subgroups of youth at risk may enable us to develop more effective treatment engagement and retention strategies for subgroups with low levels of mental health service utilization.
Supplementary Material
Acknowledgments
This study was supported by a grant from the National Institute of Mental Health (NIMH), “Emergency Department Screen for Teens at Risk for Suicide” (ED-STARS, U01 MH104311). It was also supported in part by the Health Resources and Services Administration (HRSA), the Maternal and Child Health Bureau (MCHB), the Emergency Medical Services for Children (EMSC) Network Development Demonstration Program under cooperative agreements U03MC00008, U03MC00001, U03MC00003, U03MC00006, U03MC00007, U03MC22684, U03MC28845, H3MC26201, and U03MC22685. The information or content and conclusions in this manuscript are those of the authors and should not be construed as the official position or policy of, nor should any endorsements be inferred by the NIMH, HRSA, the US Department of Health and Human Services, or the US Government.
Dr. Casper served as the statistical expert for this research.
Pediatric Emergency Care Applied Research Network (PECARN): http://www.pecarn.org/pecarnNetwork/index.html
The authors thank the PECARN Data Coordinating Center staff at the University of Utah, including Marie Kay, BA, and Michelle Robinson, BS, for project management, and Casey Evans, BS, for contributions to data programming and management. They also thank Rebecca Lindsay, MPH, and Kristin Aho, MS, of the University of Michigan, for project assistance, as well as the youth and families who participated in the ED-STARS study.
Disclosure: Dr. King has received support from the NIMH, the American Foundation for Suicide Prevention (AFSP), the National Institute of Child Health and Human Development (NICHD), and the Centers for Disease Control and Prevention. Dr. Brent has received research support from NIMH, AFSP, the Once Upon a Time Foundation, and the Beckwith Foundation; has received royalties from Guilford Press, from the electronic self-rated version of the C-SSRS from eRT, Inc., and from performing duties as an UptoDate Psychiatry Section Editor; and has received consulting fees from Healthwise. Dr. Mahabee-Gittens has received funding from the Ohio Department of Health/AAP and the National Institutes of Health (NIH). Dr. Chernick has received support from the National Center for Advancing Translational Sciences, the NIH, and the NICHD. Drs. Grupp-Phelan, Shenoi, Melzer-Lange, Rea, Littlefield, and Casper, Mr. Page, and Ms. McGuire report no biomedical financial interests or potential conflicts of interest.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Cheryl A. King, University of Michigan, Ann Arbor.
David Brent, University of Pittsburgh, PA.
Jacqueline Grupp-Phelan, University of California San Francisco.
Rohit Shenoi, Baylor College of Medicine, Houston, TX.
Kent Page, University of Utah School of Medicine, Salt Lake City, UT.
E. Melinda Matabele-Gittens, University of Cincinnati, OH.
Lauren S. Chernick, Columbia University Medical Center, New York, NY.
Marlene Melzer-Lange, Medical College of Wisconsin, Milwaukee.
Margaret Rea, University of California, Davis.
Taylor C. McGuire, University of Michigan, Ann Arbor.
Andrew Littlefield, Texas Tech University, Lubbock.
T. Charles Casper, University of Utah School of Medicine, Salt Lake City, UT.
References
- 1.Centers for Disease Control and Prevention. Web-based Injury Statistics Query and Reporting System (WISQARS). 2019; https://webappa.cdc.gov/sasweb/ncipc/leadcause.html Accessed 18 April, 2019.
- 2.Kann L, McManus T, Harris WA, et al. Youth Risk Behavior Surveillance — United States, 2017. MMWR CDC Surveill Summ. 2018;67(No. SS-8):1–114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Miron O, Yu K-H, Wilf-Miron R, Kohane IS. Suicide rates among adolescents and young adults in the United States, 2000–2017. JAMA. 2019;321(23):2362–2364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Mercado MC, Holland K, Leemis RW, Stone DM, Wang J. Trends in emergency department visits for nonfatal self-inflicted injuries among youth aged 10 to 24 years in the United States, 2001–2015. JAMA. 2017;318(19):1931–1933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.King CA, Ewell Foster C, Rogalski KM. Teen suicide risk: A practitioner guide to screening, assessment, and management. New York, NY: Guilford Press; 2013. [Google Scholar]
- 6.Brent DA, Perper JA, Goldstein CE, et al. Risk factors for adolescent suicide: A comparison of adolescent suicide victims with suicidal inpatients. Arch Gen Psychiatry. 1988;45(6):581–588. [DOI] [PubMed] [Google Scholar]
- 7.Brent DA, Perper JA, Moritz G, et al. Psychiatric risk factors for adolescent suicide: A case-control study. J Am Acad Child Adolesc Psychiatry. 1993;32(3):521–529. [DOI] [PubMed] [Google Scholar]
- 8.Esposito-Smythers C, Spirito A. Adolescent substance use and suicidal behavior: A review with implications for treatment research. Alcoholism: Clinical and Experimental Research. 2004;28:77S–88S. [DOI] [PubMed] [Google Scholar]
- 9.Nock MK, Green JG, Hwang I, et al. Prevalence, correlates, and treatment of lifetime suicidal behavior among adolescents: Results from the National Comorbidity Survey Replication Adolescent Supplement. JAMA Psychiatry. 2013;70(3):300–310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Beautrais AL, Joyce PR, Mulder RT, Fergusson DM. Prevalence and comorbidity of mental disorders in persons making serious suicide attempts: A case-control study. Am J Psychiatry. 1996;153(8):1009–1014. [DOI] [PubMed] [Google Scholar]
- 11.Goldston DB, Daniel SS, Reboussin DM, Reboussin BA, Kelley AE, Frazier PH. Psychiatric diagnoses of previous suicide attempters, first-time attempters, and repeat attempters on an adolescent inpatient psychiatry unit. J Am Acad Child Adolesc Psychiatry. 1998;37(9):924–932. [DOI] [PubMed] [Google Scholar]
- 12.Brent DA, Perper JA, Moritz G, Baugher M. Stressful life events, psychopathology, and adolescent suicide: A case control study. Suicide Life Threat Behav. 1993;23(3):179–187. [PubMed] [Google Scholar]
- 13.Hallfors DD, Waller MW, Ford CA, Halpern CT, Brodish PH, Iritani B. Adolescent depression and suicide risk: Association with sex and drug behavior. Am J Prev Med. 2004;27(3):224–230. [DOI] [PubMed] [Google Scholar]
- 14.Pena JB, Matthieu MM, Zayas LH, Masyn KE, Caine ED. Co-occurring risk behaviors among White, Black, and Hispanic US high school adolescents with suicide attempts requiring medical attention, 1999–2007: Implications for future prevention initiatives. Soc Psychiatry Psychiatr Epidemiol. 2012;47(1):29–42. [DOI] [PubMed] [Google Scholar]
- 15.Zatti C, Rosa V, Barros A, et al. Childhood trauma and suicide attempt: A meta-analysis of longitudinal studies from the last decade. Psychiatry Res. 2017;256:353–358. [DOI] [PubMed] [Google Scholar]
- 16.Merikangas KR, He J-P, Burstein M, et al. Service utilization for lifetime mental disorders in U.S. Adolescents: Results of the National Comorbidity Survey-Adolescent Supplement (NCSA). J Am Acad Child Adolesc Psychiatry. 2011;50(1):32–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Diamond GS, Herres JL, Krauthamer Ewing ES, et al. Comprehensive screening for suicide risk in primary care. Am J Prev Med. 2017;53(1):48–54. [DOI] [PubMed] [Google Scholar]
- 18.Jiang Y, Perry DK, Hesser JE. Suicide patterns and association with predictors among Rhode Island public high school students: A latent class analysis. Am J Public Health. 2010;100(9):1701–1707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Shaffer D, Gould MS, Fisher PW, et al. Psychiatric diagnosis in child and adolescent suicide. Arch Gen Psychiatry. 1996;53(4):339–348. [DOI] [PubMed] [Google Scholar]
- 20.Brent DA, Baugher M, Bridge J, Chen T, Chiappetta L. Age- and sex-related risk factors for adolescent suicide. J Am Acad Child Adolesc Psychiatry. 1999;38(12):1497–1505. [DOI] [PubMed] [Google Scholar]
- 21.King CA, Grupp-Phelan J, Brent D, et al. Predicting 3-month risk for adolescent suicide attempts among pediatric emergency department patients. Journal of Child Psychology and Psychiatry 2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Czyz EK, King CA. Longitudinal trajectories of suicidal ideation and subsequent suicide attempts among adolescent inpatients. J Clin Child Adolesc Psychol. 2015;44(1):181–193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Victor SE, Klonsky ED. Correlates of suicide attempts among self-injurers: A meta-analysis. Clin Psychol Rev. 2014;34(4):282–297. [DOI] [PubMed] [Google Scholar]
- 24.Posner K, Brent D, Lucas C, et al. Columbia-Suicide Severity Rating Scale (C-SSRS). 2007; http://www.fda.gov/ohrms/dockets/ac/07/slides/2007-4306s1-01-CU-Posner_files/frame.htm#slide0708.htm Accessed January 27, 2009.
- 25.Horowitz LM, Bridge JA, Teach SJ, et al. Ask Suicide-Screening Questions (ASQ): A brief instrument for the pediatric emergency department. Arch Pediatr Adolesc Med. 2012;166(12):1170–1176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kroenke K, Spitzer RL, Williams JBW. The PHQ-9: Validity of a brief depression severity measure. J Gen Intern Med. 2001;16(9):606–613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Saunders JB, Aasland OG, Babor TF, De La Fuente JR, Grant M. Development of the Alcohol Use Disorders Identification Test (AUDIT): WHO collaborative project on early detection of persons with harmful alcohol consumption--II. Addiction. 1993;88(6):791–804. [DOI] [PubMed] [Google Scholar]
- 28.National Institute for Drug Abuse. NIDA-Modified Assist. 2013; https://www.drugabuse.gov/sites/default/files/pdf/nmassist.pdf Accessed October 11, 2015.
- 29.Stanford MS, Greve KW, Dickens TJ. Irritability and impulsiveness: Relationship to self-reported impulsive aggression. Personality and Individual Differences. 1995;19(5):757–760. [Google Scholar]
- 30.Bernstein DP, Stein JA, Newcomb MD, et al. Development and validation of a brief screening version of the Childhood Trauma Questionnaire. Child Abuse Negl. 2003;27(2):169–190. [DOI] [PubMed] [Google Scholar]
- 31.Muthén LK, Muthén BO. Mplus user’s guide. Los Angeles, CA: Muthén & Muthén;1998–2017. [Google Scholar]
- 32.R: A language and environment for statistical computing. [computer program]. Vienna, Austria: R Foundation for Statistical Computing; 2016. [Google Scholar]
- 33.SAS Software [computer program]. Version 9.4. Cary, NC: SAS Institute Inc; 2013. [Google Scholar]
- 34.Celeux G, Soromenho G. An entropy criterion for assessing the number of clusters in a mixture model. Journal of Classification. 1996;13(2):195–212. [Google Scholar]
- 35.Bridge JA, Olfson M, Fontanella CA, Marcus SC. Emergency department recognition of mental disorders and short-term risk of repeat self-harm among young people enrolled in-Medicaid. Suicide and Life-Threatening Behavior. 2018;48(6):652–660. [DOI] [PubMed] [Google Scholar]
- 36.Hodgkinson S, Godoy L, Beers LS, Lewin A. Improving mental health access for low-income children and families in the primary care setting. Pediatrics. 2017;139(1):e20151175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Hoffman L A proposal to address the workforce shortage in child and adolescent psychiatry. J Am Acad Child Adolesc Psychiatry. 2018;57(12):977–978. [DOI] [PubMed] [Google Scholar]
- 38.Logan DE, King CA. Parental identification of depression and mental health service use among depressed adolescents. J Am Acad Child Adolesc Psychiatry. 2002;41(3):296–304. [DOI] [PubMed] [Google Scholar]
- 39.Ryan SM, Jorm AF, Toumbourou JW, Lubman DI. Parent and family factors associated with service use by young people with mental health problems: a systematic review. Early Interv Psychiatry. 2015;9(6):433–446. [DOI] [PubMed] [Google Scholar]
- 40.U.S. Department of Health and Human Services, Health Resources and Services Administration, Maternal and Child Health Bureau. Child Health USA 2012. Emergency department utilization. Rockville, Maryland: U.S. Department of Health and Human Services; 2013:60. [Google Scholar]
- 41.Horowitz L, Ballard E, Teach S, J., et al. Feasibility of screening patients with nonpsychiatric complaints for suicide risk in pedicatric emergency department. Pediatr Emerg Care. 2010;26(11):787–792. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.King CA, O’Mara RM, Hayward CN, Cunningham RM. Adolescent suicide risk screening in the emergency department. Acad Emerg Med. 2009;16(11):1234–1241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.O’Mara RM, Hill RM, Cunningham RM, King CA. Adolescent and parent attitudes toward screening for suicide risk and mental health problems in the pediatric emergency department. Pediatr Emerg Care. 2012;28(7):626–632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.King CA, Jiang Q, Czyz EK, Kerr DC. Suicidal ideation of psychiatrically hospitalized adolescents has one-year predictive validity for suicide attempts in girls only. J Abnorm Child Psychol. 2014;42(3):467–477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Defayette AB, Adams LM, Whitmyre ED, Williams CA, Esposito-Smythers C. Characteristics of a first suicide attempt that distinguish between adolescents who make single versus multiple attempts. Archives of Suicide Research. 2019:1–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Ingoldsby EM. Review of interventions to improve family engagement and retention in parent and child mental health programs. Journal of Child and Family Studies. 2010;19(5):629–645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Godoy L, Hodgkinson S, Robertson HA, et al. Increasing mental health engagement from primary care: The potential role of family navigation. Pediatrics. 2019;143(4):e20182418. [DOI] [PubMed] [Google Scholar]
- 48.Halliday-Boykins CA, Schoenwald SK, Letourneau EJ. Caregiver-therapist ethnic similarity predicts youth outcomes from an empirically based treatment. J Consult Clin Psychol. 2005;73(5):808–818. [DOI] [PubMed] [Google Scholar]
- 49.Becker KD, Boustani M, Gellatly R, Chorpita BF. Forty years of engagement research in children’s mental health services: Multidimensional measurement and practice elements. Journal of Clinical Child & Adolescent Psychology. 2018;47(1):1–23. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.