Abstract
Background
Telehealth use has been increasing during the last decade. Studies have found that patients have a positive attitude toward incorporating telehealth into their health care. Substantial uncertainty remains regarding reimbursement policies that vary widely between states and by payer.
Objective
To explore the clinical, operational, and financial feasibility of a home telehealth (HTH) program in a pediatric allergy and immunology clinic.
Methods
Allergy and immunology physicians defined use cases they deemed appropriate for HTH appointments. Established patients in the allergy and immunology clinic were approached to complete an attitudes and perception survey. Patients who met the use case definitions were asked to participate in the pilot program. After their HTH appointment took place, they completed a validated satisfaction survey. Our institution’s revenue cycle management team provided reimbursement data.
Results
Patient attitudes toward HTH were generally favorable. A total of 51 HTH appointments were offered, and 46 appointments were made. Notably, 37 appointments were completed successfully among 32 unique patients. Patients were satisfied with the HTH experience. A total of 36 of 37 encounters were reimbursed by 19 different public and private payers. Payers on average reimbursed ±6% of the expected allowable for an equivalent in-person visit.
Conclusion
Patients had reservations about HTH initially but were satisfied with their experience. Private and public payers reimbursed HTH the same as in-person appointments. Here, we report that HTH is well accepted by patients and is financially viable.
Introduction
Telehealth is broadly defined as the exchange of medical information from one site to another through electronic communication.1 A variety of modalities are encompassed by the term telehealth, including store and forward, remote patient monitoring, and virtual check-ins.2 The subset of telehealth that refers to real-time communication between a medical professional and patient using audiovisual technology is sometimes referred to as telemedicine.3 All forms of telehealth have been expanding in the United States during the past decade, including in pediatrics, albeit slower than in adults.4 , 5 This trend reflects a variety of factors, including technology improvements, a health care system more embracing of innovation, and an increasing awareness of and attention to patient preference and convenience.6 For subspecialties such as allergy and immunology, there are additional drivers to rapidly adopt telehealth, such as addressing access issues for rural and other underserved communities and supplementing workforce shortages.7 On March 11, 2020, the World Health Organization declared the novel coronavirus disease 2019 (COVID-19) a global pandemic, and the need for telemedicine has never been greater.8 As part of its response, the US Department of Health and Human Services issued a notification of enforcement discretion for several regulations relating to telehealth to enable practitioners to deliver care using technology while observing social distancing.9
Nonetheless, several barriers still remain in the adoption of telehealth, including operational or logistical issues, patient trust, technology integration, and a varied and confusing patchwork of telehealth regulation and reimbursement across the country.10 Before COVID-19, the Centers for Medicare and Medicaid Services had already issued guidance for Medicare services delivered through telehealth, but pediatric patients are most often subject to Medicaid rules, which vary by state.5 Additional concerns relating to consent, privacy, and participation of the parent-child dyad have also made telehealth adoption slower in pediatrics than in adult care.11
Concerns regarding reimbursement remain a major barrier for telehealth adoption, with some states and payers reimbursing less for telehealth than in-person visits or not at all.12 The location of the patient also affects whether the visit is reimbursed. Traditionally, a patient was expected to be in a health care facility, such as an outpatient clinic (the originating site), and use telecommunications equipment there to connect to a practitioner located somewhere else (eg, an academic medical center) (the distant site). However, the telehealth reimbursement landscape has improved during the last few years. As of December 2019, 40 states have laws that require parity in reimbursed services, and an increasing number of states have passed payment parity laws.13 , 14 California passed legislation in October 2019 that required payment parity for telehealth starting January 2021.15 Home telehealth (HTH), in which the originating site is the patient’s home, is also becoming more common; 19 states have Medicaid plans that allow coverage for telehealth when the originating site is the patient’s home.13 Individual state telehealth policies can be found in eTable 1. Home telehealth may be more convenient for patients and may place less burden on the health care system to equip originating sites. During the COVID-19 pandemic, several states and payers have allowed the home to be an originating site and have offered payment parity for a variety of forms of telehealth.16 It is unclear at this time which, if any, of these changes will be rescinded after the current emergency.
To address some of these concerns, we present the results of our pilot HTH program, which was conducted before the COVID-19 pandemic in the allergy and immunology clinic at our academic medical center. We report on the attitudes and perceptions of HTH by practitioners and patients receiving care through telehealth, the clinical care delivered, and the reimbursement rates and patterns by federal, public, and private payers in California.
Methods
A prospective evaluation of HTH was piloted from April 2017 to June 2018 in the outpatient allergy and immunology clinic of a pediatric academic medical center. This study was approved by our institutional review board, and all participants gave oral consent to participate in the study.
Attitudes and Perceptions
During the study period, families in the allergy and immunology clinic waiting room were approached to participate in an anonymous survey to assess telehealth attitudes and perceptions. Minimal modifications (eg, “you” was changed to “your child”) were made to a validated instrument used by Gurupur et al17 in 2016 to more appropriately address a pediatric population. The survey was available in Spanish and English and included 9 5-point Likert items about telehealth followed by 13 demographic questions, including income, education, and health insurance. A survey was considered incomplete if the participant left any question blank, except for family income (which was optional to report). An instrument was used to assess physicians’ knowledge of telehealth, their comfort with the technology, and their perception of patient experience improvement (developed by Gurupur et al, unpublished data, 2017).
Home Telehealth Visits
Allergy and immunology practitioners defined 3 clinical use cases for HTH. The first was follow-up visits after diagnostics (laboratory test or imaging) to discuss results and the plan moving forward. The second use case was for selected patients who lived far from our medical center to ease their travel burden. The third use case was a clinical assessment for ongoing high-risk food desensitization therapy. Patients are normally scheduled every 2 weeks during desensitization; if a patient felt ill between sensitization visits, a traditional in-person sick visit could be replaced by a telehealth visit.
Using these criteria, practitioners offered at their discretion HTH visits to established patients who they believed would be good candidates. Patients who agreed were consented for this study. The visits were completed using KidsDOC (Kids Doctors On Call, Los Angeles, California), a commercially available Health Insurance and Portability and Accountability Act–compliant telehealth platform. After the visit, participants completed a telehealth satisfaction survey modified (eg, “you” was changed to “your child”) from Morgan et al.18 Data regarding the visit diagnosis and patient demographics were abstracted from the electronic health record (EHR). Physicians provided brief narratives that described their experience delivering HTH.
Use and Reimbursement Patterns
To measure the effect on health care use, the number of appointments 24 months before and after the telehealth appointment as recorded in the EHR were counted. A no-show rate was also calculated. A no-show appointment was defined as a scheduled appointment that was not cancelled or rescheduled by the patient or the clinic. The institution’s revenue cycle management team provided billing and claims data for all telehealth encounters. A new telehealth encounter type was developed for this pilot so that they could be easily identified. Encounters were verified by reviewing the billing practitioner and encounter date. Payers were grouped into the following 3 categories: public, private, and federal. Public payers included California Children’s Services and Medicaid, both fee for service and managed care. Private payers included 10 different preferred provider organizations and commercial health maintenance organizations. Federal payers included Tricare, Medicare, and Federal Employee Blue Shield. Actual reimbursements were compared with the expected reimbursement rate, a value that is calculated by the revenue cycle team based on the negotiated rate with the payer and previous reimbursements for an in-person visit of the same complexity.
Statistical Analysis
Quantitative survey and claims data were summarized using descriptive statistics. Qualitative data from the practitioner narratives were analyzed using thematic content analysis. No formal codebook was developed given the overall brief nature of the narratives.
Results
Attitudes and Perceptions of Telehealth
Among all patients approached in the allergy and immunology waiting room for the attitudes and perceptions survey, 130 families initiated the survey; 20 surveys were incomplete and excluded from the analysis. Demographics are presented in Table 1 . Most respondents were female biological parents of the patients. The mean age of the respondents was 36 years. More than 40% (n = 46) of our patient population was Hispanic, 30% (n = 33) was white, 15% (n = 16) was Asian, and 4% (n = 5) was black; more than half of respondents identified as bilingual, with 76% being Spanish speakers. Almost 60% of patients received insurance through Medicaid. The mean distance traveled by families from their home to our institution was 25.4 miles.
Table 1.
Demographics of Study Participants Surveyed Regarding Parent Perceptions of Home Telehealth
| Demographic | Finding (N = 110)a |
|---|---|
| Female sex | 92 (84) |
| Age, y | 36 |
| Race or ethnicity | |
| Latino | 46 (42) |
| Asian | 16 (15) |
| White | 33 (30) |
| Black | 5 (4) |
| Other | 4 (4) |
| Mixed | 6 (5) |
| Bilingual households | 57 (52) |
| Limited English proficiency | 12 (11) |
| Medicaid | 63 (58) |
Data are presented as number (%) of study patients unless otherwise indicated.
Overall, 62% of patients thought that telehealth would reduce physician response time. Only 11% of patients believed that the idea of telehealth sounded too complicated. Patients were split on whether telemedicine would provide specialized care to their child, with 33% agreeing and 34% disagreeing. Perceptions are summarized in Table 2 .
Table 2.
Attitudes and Perceptions of Parents Regarding Telehealth Before Home Telehealth Encounter
| Attitude and perception | No. (%) of parents |
|
|---|---|---|
| Agree or completely agree (N = 110) | Disagree or completely disagree (N = 110) | |
| The money saved in time away from work and gasoline cost would affect my decision to use telemedicine rather than traveling for a face-to-face visit with a specialist. | 58 (53) | 28 (25) |
| I am concerned about being able to understand what the doctor says through telemedicine video. | 29 (26) | 51 (46) |
| I think that the doctor will be able to understand me and my child through telemedicine video. | 71 (65) | 15 (14) |
| I would prefer to see a physician sooner through telemedicine than wait to see a physician in-person. | 64 (58) | 18 (16) |
| I feel telemedicine can improve patient feedback regarding the side effects of treatment. | 62 (56) | 14 (13) |
| I feel telemedicine can reduce physician response time. | 68 (62) | 19 (17) |
| The idea of telemedicine sounds too complicated. | 12 (11) | 76 (69) |
| If a specialist were not available in my local area, I would prefer to see a specialist via telemedicine rather than travel a long distance. | 80 (73) | 18 (16) |
| The use of telemedicine would provide my child specialized care that I would not otherwise have access to. | 36 (33) | 37 (34) |
All 4 practitioners completed a validated assessment of attitudes and perceptions. All the practitioners believed that telehealth would improve care delivery to otherwise isolated rural areas. Practitioners indicated that they believed telehealth would be an additional burden for their practice. Most practitioners thought that a patient’s personal health information would be respected with telehealth platforms. Other practitioner responses are given in Table 3 .
Table 3.
Practitioner Attitudes and Perceptions Toward the Use of Telehealth
| Attitude or perception | Mean scorea (n = 4) |
|---|---|
| The use of telemedicine technology can allow for a more timely diagnosis and treatment of my patients. | 2.8 |
| Telemedicine will be an added burden in my practice, creating more work and training for my staff and me. | 3.3 |
| Telemedicine provides access to specialized care that otherwise would be unavailable to rural patients in a timely fashion. | 4.0 |
| I am knowledgeable about the uses of telemedicine technology. | 3.5 |
| I have used telemedicine technology in my practice. | 2.8 |
| I feel that the personal health information of my patients is respected through the use of telemedicine. | 3.8 |
| I am able to communicate with my patients as effectively through telemedicine as in face-to-face visits in my office. | 2.5 |
| Telemedicine equipment is relatively easy to use and maintain. | 3.5 |
| Telemedicine technology offers a more cost-effective way for me to treat my patients. | 2.5 |
| I feel that patients receive the same level of care in a telemedicine setting. | 2.8 |
| I am concerned that learning how to setup and use the telemedicine equipment will be difficult. | 2.3 |
| The telemedicine technology is reliable. | 3.0 |
| The technological costs associated with telemedicine are prohibitive. | 2.3 |
| Patients are more likely to be compliant if they are cared for using both telemedicine and face-to-face interactions. | 3.3 |
| I am comfortable referring a patient for evaluation via telemedicine. | 3.3 |
| I am concerned that patients will not travel to see a physician in person. | 3.0 |
| The physician can effectively communicate with the patient through telemedicine. | 2.8 |
| Telemedicine is a needed service. | 3.5 |
| Adequate telemedicine training is available. | 3.5 |
| I am aware of telemedicine vendors in my area. | 2.0 |
| I am familiar with the rules and regulations concerning telemedicine. | 2.8 |
Scores range from 1, indicating disagree, to 4, indicating strongly agree.
Home Telehealth Visits
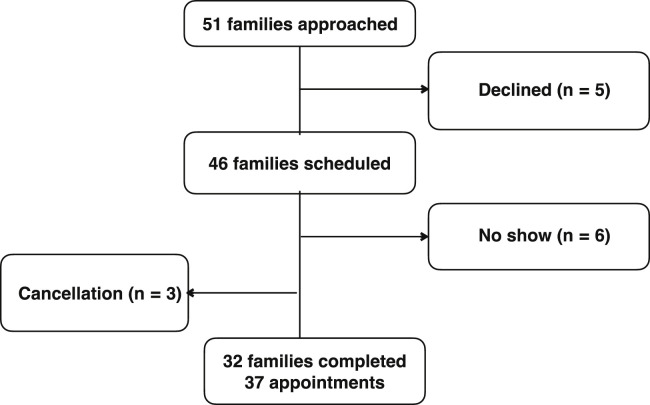
A total of 51 patients were approached for the feasibility pilot, and 46 agreed to make an appointment. These 51 patients were a separate cohort from the waiting room cohort of 110 patients and were selected because they fit 1 of the clinical use cases. To the best of our knowledge, there was no overlap between the waiting room cohort and the pilot cohort. Although 3 patients cancelled and 6 patients did not show up to their appointments, 37 appointments were completed successfully among 32 unique patients (Fig 1 ). Of those 37 appointments; 30 were for continuity of care; 6 were for food challenge follow-ups, including 3 sick visits that were deemed appropriate to conduct through telehealth; and 1 was for laboratory test results review. Some common visit diagnosis for the HTH visits included food allergies (n = 10), asthma (n = 8), and urticaria (n = 3). The full list of visit diagnoses is given in Table 4 . Among families who had HTH visits, the mean age of patients was 11.9 years, and 35% were female. Data on race and ethnicity were taken from the electronic health system. A total of 35% (n = 13) of our patient population was white, 22% (n = 8) was Hispanic, 5% (n = 2) was Asian, 8% (n = 3) was other, and 30% (n = 11) was unknown. Patient satisfaction with HTH visits is summarized in Table 5 . Almost 80% had never used telehealth before, but all respondents had used video communication (eg, Skype or FaceTime) in their personal life. Despite being telehealth naive, patient experiences were overall positive (>90%), with 100% indicating they would use telehealth again and would recommend it to others. All the patients thought that their privacy was respected, and 96% were satisfied with the amount of time with their practitioner.
Figure 1.
CONSORT-style flow diagram of patients participating in the home telehealth pilot study. CONSORT, consolidated standards of reporting trials.
Table 4.
Visit Diagnoses
| Diagnosis | No. of visits |
|---|---|
| Atopy | 21 |
| Asthma | 8 |
| Allergic rhinitis | 8 |
| Eczema or atopic dermatitis | 5 |
| Food allergies | 10 |
| Immunodeficiencies | 9 |
| DiGeorge syndrome | 2 |
| Common variable immune deficiency | 2 |
| Chronic granulomatous disease | 1 |
| IgG2 subclass deficiency | 1 |
| Hypogammaglobulinemia | 1 |
| Immunodeficiency NOS | 1 |
| Emmanuel syndrome | 1 |
| Chronic urticaria | 3 |
| Eosinophilic gastrointestinal disease | 1 |
| Chronic sinusitis | 2 |
| Addison disease | 1 |
| Hemolytic anemia | 1 |
| Total | 48 |
Abbreviations: IgG2, immunoglobulin G2; NOS, not otherwise specificed.
Table 5.
Participant Satisfaction With Home Telehealth Encounter
| Question | Satisfied or completely satisfied or response of yes, No. (%) |
|---|---|
| How satisfied were you with . . . | |
| The audio and video quality? | 28 (87) |
| Personal comfort using the telehealth platform? | 31 (96) |
| The length of time with the A/I provider? | 31 (96) |
| The explanation of your treatment by the A/I provider? | 29 (91) |
| The thoroughness, carefulness and skillfulness of the A/I provider? | 31 (96) |
| The courtesy, respect, sensitivity, and friendliness of the A/I provider? | 31 (96) |
| How well your privacy was respected? | 32 (100) |
| Your overall treatment experience with telehealth? | 29 (91) |
| Would you use telehealth again? | 32 (100) |
| Would you recommend telehealth to another person | 32 (100) |
| Have you ever used telehealth or telemedicine before today? | 7 (21.7) |
| Have you ever used video call technology before, like Skype or FaceTime? | 32 (100) |
| How often do you use video call technology? | |
| Everyday | 3 (8.7) |
| A few times a week | 1 (4.3) |
| A few times a month | 13 (39.1) |
| A few times a year | 15 (47.8) |
Abbreviation: A/I, allergy/immunology.
In addition, 3 of 4 physicians provided narrative descriptions of their experiences with telehealth and were also generally positive. Common themes that emerged included patients being timely and comfortable in their own house. Specifically, one special needs patient benefited greatly from not undergoing the stress of coming to the hospital for his checkup and remaining in the comfort of his own home. Physicians did report that issues with internet connectivity and unfamiliarity with a new workflow occasionally hindered the appointment.
Use and Reimbursement Patterns
Patients had a mean of 5 in-person appointments with a no-show rate of 25% before the telehealth appointment. After their appointment, patients scheduled 4 in-person appointments with a no-show rate of 24%. The no-show rate for HTH visits was 14%.
Private, public, and federal payers generally covered HTH visits, with 36 of 37 visits being reimbursed (Table 6 ). Only 1 visit (evaluation and management code 99214) was not reimbursed by a local commercial independent physician association. Mean reimbursement ranged from 94% to 107% of the expected rate, suggesting no difference between in-person and HTH visit reimbursement.
Table 6.
Reimbursement of Billed Home Telehealth Encounters
| Category | No. of encounters (n = 37) | No. of encounters reimbursed (n = 36) | Expected allowable %, (range) |
|---|---|---|---|
| By E&M code | |||
| 99213 | 21 | 21 | 98 (72-128) |
| 99214 | 10 | 9 | 96 (89-118) |
| 99215 | 6 | 6 | 98 (90-100) |
| By payer | |||
| Private | 25 | 24 | 94 (72-100) |
| Public | 8 | 8 | 107 (97-128) |
| Federal | 4 | 4 | 100 (100-100) |
Abbreviaton: E&M, evaluation and management.
Discussion
Our pilot study found that HTH is technically and economically feasible in addition to being well received by patients and practitioners in an outpatient pediatric allergy and immunology clinic, as evidenced by patient and practitioner satisfaction measures and billing outcomes. The socioeconomically diverse patient population that participated suggests broad acceptability.
Historically, telemedicine has been considered a viable alternative for patients in medically underserved areas, such as rural communities.19 Ray et al20 found that children from rural areas or more than 90 miles from a subspecialist were more likely to schedule a telemedicine visit. A total of 6% of the participants surveyed lived more than 90 miles away from our clinic. However, the disadvantaged populations in urban settings also experience difficulties accessing specialty care.20 Our data indicated that 28% of our patients surveyed earned less than $50,000, and almost 60% received insurance though Medi-Cal (California’s Medicaid program). Barnett et al21 found that the wait time to see certain specialists in Los Angeles County could be up to 9 months. The authors describe the development of an electronic consultation system in which requests for specialist appointments were reviewed electronically within 1 day by a separate screener to determine whether the case could be electronically resolved or required a specialist appointment. The median wait time to see a specialist decreased by 17.4%. For comparison, the mean wait time at our clinic can be up to 16 weeks. In states such as South Carolina, with significant rural and economically disadvantaged communities, telehealth has become the critical technical infrastructure on which hub-and-spoke models are built for subspecialty care delivery.22 Our institution’s catchment area is predominantly urban but includes large rural areas, with some patients traveling more than 100 miles for their appointments. Implementing telehealth could help improve appointment availability and care delivery to a diverse population by adding health care capacity without an increase in physical space and overhead.
A recent systematic review and narrative analysis found that telemedicine decreases missed appointments and readmissions in addition to improving communication with practitioners and decreasing travel time to the hospital.23 This finding is supported by our study because the practitioners thought that patients using HTH were more timely and relaxed during their appointments. Lin et al24 conducted a telemedicine intervention program for children with asthma that improved medication adherence and hospitalization outcomes. Their study found that parents were satisfied with the telehealth visits and believed it to be as helpful as in-person visits. Many of our patients did not have strong opinions on telehealth in the intake survey, with only 65% agreeing that the physician would understand them through telemedicine and 33% believing that telemedicine would provide access to specialized care. After the appointment, 100% of our patients expressed that they would use telehealth again, and more than 90% were satisfied or completely satisfied with the visit. For institutions concerned about patient adoption, our study found that patients were comfortable with the new technology and model of care.
Only 1 private independent physician association did not reimburse the HTH visit, but public and federal plans reimbursed at 100% of the expected rate. Interestingly, this pattern occurred before California passed a private insurance payment parity law that requires that practitioners be reimbursed at the same rate for in-person and telehealth visits. This law will be effective January 1, 2021.15 As of March 6, 2020, Medicare has also relaxed its guidelines, allowing the home to qualify as an originating site and paying physicians under the same fee schedule for in-person appointments under Medicare Part B.16 Our results, with similar reimbursement for in-person and HTH care before the implementation of parity laws, suggest that the industry may be receptive to this new care delivery modality. This finding should alleviate the concerns that some practitioners may have about starting telehealth programs.
Finally, although outside the scope of this study, the actual planning and implementation of a telehealth program is critical to its success. Several professional organizations have published manuals, including the American Medical Association,25 the American Telemedicine Association,26 the American Academy of Pediatrics,27 and the Telehealth Resource Centers.28 A few authors have specifically addressed critical telehealth issues for pediatric subspecialists, including referral barriers, patient scheduling, and supporting culture change.20 , 29
There are several limitations to this study. The small sample size and lack of randomization mean that statistical significance and potential for bias cannot be excluded. We conducted our study in only 1 geographic region and insurance marketplace, which limits the generalizability of our findings to other states or regions that may have a different insurance or regulatory environment because telehealth regulations are fractured across the United States. 13 The demographics of the sample of patients who completed the waiting room attitudes and perceptions survey are similar, but not identical, to the demographics of patients who participated in the HTH pilot (eg, 40% vs 22% Hispanic, 30% vs 35% white, and 15% vs 5% Asian). This finding could be attributable to a genuine difference between the 2 populations, bias in the convenience sample of patients selected for the pilot study by treating physicians, or the different methodos used to collect the data. For the survey, patients self-reported demographic data, and no demographic fields were left blank. For the pilot participants, demographic data were taken from the EHR, which can be inaccurate or missing (eg, 30% of pilot participants had no race or ethnicity indicated in the EHR). With that, African Americans were not well represented in either patient population compared with regional demographics.
The timing of this pilot study is also a limitation. All the HTH visits were conducted in 2017, and billing data collection was completed in 2018, therefore our outcomes may not be representative of the current regulatory environment, which is rapidly evolving in California and across the United States.11 However, given the trend toward more coverage of HTH and the lasting effects of the COVID-19 pandemic, the effect of this limitation may not be significant. There were no Medicare patients in our study, so it would be difficult to extrapolate our results to that patient population. The study population was comprised of young urban families who may be more comfortable with technology than the typical patient. These study limitations are in addition to the inherent limitations of telehealth, such as the inability to perform a complete physical examination. Telehealth visits may also be complicated by unexpected patient complaints or concerns that are not amenable to being addressed virtually and require an additional in-person visit. Specific to the allergy and immunology clinic, telehealth visits cannot replicate in-office procedures, such as skin prick testing or pulmonary function tests (ie, spirometry). Moreover, high-risk procedures, such as food or drug challenges, are difficult to replicate safely in a virtual environment.
In conclusion, patients had some reservations about HTH initially but were satisfied with their experience afterward. Private and public payers reimbursed for HTH the same as in-person appointments. Home telehealth is well accepted by patients and is financially viable. The ongoing COVID-19 pandemic has accelerated the timeline to incorporate telehealth into the national guidelines and define national regulations and funding for telehealth. Further studies are needed to understand the effects of HTH on clinical outcomes, workflows and productivity, and overall financial impact.
Footnotes
Disclosures: The authors have no conflicts of interest to report.
Funding: The authors have no funding sources to report.
Supplementary data related to this article can be found at https://doi.org/10.1016/j.anai.2020.06.003.
Supplementary Data
eTable 1.
Summary of State Telehealth Policiesa
| State | Medicaid reimbursement |
Private payer law |
Professional requirements |
|||||
|---|---|---|---|---|---|---|---|---|
| Live video | Store and forward | RPM | HTH | Law exists | Payment parity | Licensing compact | Consent requirement | |
| Alabama | ✔ | ✔ | IMLC, NLC | ✔ | ||||
| Alaska | ✔ | ✔ | ✔ | ✔ | ✔ | |||
| Arizona | ✔ | ✔ | ✔ | ✔ | ✔ | NLC, PSYPACT, PTC | ✔ | |
| Arkansas | ✔ | ✔ | ✔ | ✔ | NLC, PTC | ✔ | ||
| California | ✔ | ✔ | ✔ | ✔ | ✔ | |||
| Colorado | ✔ | ✔ | ✔ | ✔ | IMLC, NLC, PTC, PSYPACT | ✔ | ||
| Connecticut | ✔ | ✔ | ✔ | |||||
| District of Columbia | ✔ | ✔ | ✔ | IMLC | ✔ | |||
| Delaware | ✔ | ✔ | ✔ | ✔ | NLC, PTC, PSYPACT | ✔ | ||
| Florida | ✔ | ✔ | NLC | ✔ | ||||
| Georgia | ✔ | ✔ | ✔ | ✔ | IMLC, NLC, PTC, PSYPACT | ✔ | ||
| Hawaii | ✔ | ✔ | ✔ | ✔ | ||||
| Idaho | ✔ | IMLC, NLC | ✔ | |||||
| Illinois | ✔ | ✔ | ✔ | IMLC, PSYPACT | ||||
| Indiana | ✔ | ✔ | ✔ | NLC | ✔ | |||
| Iowa | ✔ | ✔ | IMLC, NLC, PTC | |||||
| Kansas | ✔ | ✔ | ✔ | ✔ | IMLC, NLC | ✔ | ||
| Kentucky | ✔ | ✔ | ✔ | ✔ | IMLC, NLC, PTC | ✔ | ||
| Louisiana | ✔ | ✔ | ✔ | NLC, PTC | ✔ | |||
| Maine | ✔ | ✔ | ✔ | IMLC, NLC | ✔ | |||
| Maryland | ✔ | ✔ | ✔ | ✔ | IMLC, NLC, PTC | ✔ | ||
| Massachusetts | ✔ | ✔ | ||||||
| Michigan | ✔ | ✔ | ✔ | IMLC | ✔ | |||
| Minnesota | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | IMLC | ✔ |
| Mississippi | ✔ | ✔ | ✔ | IMLC, NLC, PTC | ✔ | |||
| Missouri | ✔ | ✔ | ✔ | ✔ | NLC, PTC, PSYPACT | ✔ | ||
| Montana | ✔ | ✔ | IMLC, NLC, PTC | |||||
| Nebraska | ✔ | ✔ | ✔ | ✔ | IMLC, NLC, PTC, PSYPACT | ✔ | ||
| Nevada | ✔ | ✔ | ✔ | ✔ | IMLC, PSYPACT | |||
| New Hampshire | ✔ | ✔ | ✔ | IMLC, NLC, PTC, PSYPACT | ||||
| New Jersey | ✔ | ✔ | NLC, PTC | ✔ | ||||
| New Mexico | ✔ | ✔ | ✔ | ✔ | NLC | ✔ | ||
| New York | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ||
| North Carolina | ✔ | PTC, NLC | ||||||
| North Dakota | ✔ | ✔ | IMLC, NLC, PTC | ✔ | ||||
| Ohio | ✔ | ✔ | ✔ | ✔ | ||||
| Oklahoma | ✔ | ✔ | IMLC, NLC, PTC, PSYPACT | ✔ | ||||
| Oregon | ✔ | ✔ | ✔ | ✔ | PTC | ✔ | ||
| Pennsylvania | ✔ | IMLC | ✔ | |||||
| Rhode Island | ✔ | ✔ | ✔ | |||||
| South Carolina | ✔ | ✔ | NLC, PTC | ✔ | ||||
| South Dakota | ✔ | ✔ | IMLC, NLC, PTC | |||||
| Tennessee | ✔ | ✔ | ✔ | IMLC, NLC, PTC | ✔ | |||
| Texas | ✔ | ✔ | ✔ | ✔ | ✔ | NLC, PTC, PSYCPACT | ✔ | |
| Utah | ✔ | ✔ | ✔ | IMLC, NLC, PTC, PSYPACT | ||||
| Vermont | ✔ | ✔ | ✔ | ✔ | IMLC | ✔ | ||
| Virginia | ✔ | ✔ | ✔ | ✔ | NLC, PTC | ✔ | ||
| Washington | ✔ | ✔ | ✔ | ✔ | ✔ | IMLC, PTC | ✔ | |
| West Virginia | ✔ | IMLC, NLC, PTC | ✔ | |||||
| Wisconsin | ✔ | NLC, PTC | ✔ | |||||
| Wyoming | ✔ | ✔ | IMLC, NLC | ✔ | ||||
Abbreviations: HTH, home telehealth; IMLC, Interstate Medical Licensure Compact; NLC: Nurses Licensure Compact; PTC, Physical Therapy Compact; PSYPACT, Psychology Interjurisdictional Compact; RPM, remote patient monitoring.
Adapted from Center for Connected Health Policy.13
References
- 1.Mechanic O.J., Kimball A.B. Telehealth systems. StatPearls. NCBI bookshelf. https://www.ncbi.nlm.nih.gov/books/NBK459384/ Available at: [PubMed]
- 2.Trout K.E., Rampa S., Wilson F.A., Stimpson J.P. Legal mapping analysis of state telehealth reimbursement policies. Telemed J E Health. 2017;23(10):805–814. doi: 10.1089/tmj.2017.0016. [DOI] [PubMed] [Google Scholar]
- 3.Marcoux R.M., Vogenberg F.R. Telehealth: applications from a legal and regulatory perspective. P T. 2016;41(9):567–570. [PMC free article] [PubMed] [Google Scholar]
- 4.Barnett M.L., Ray K.N., Souza J., Mehrotra A. Trends in telemedicine use in a large commercially insured population, 2005-2017. JAMA. 2018;320(20):2147–2149. doi: 10.1001/jama.2018.12354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Olson C.A., McSwain S.D., Curfman A.L., Chuo J. The current pediatric telehealth landscape. Pediatrics. 2018;141(3) doi: 10.1542/peds.2017-2334. [DOI] [PubMed] [Google Scholar]
- 6.Tuckson R.V., Edmunds M., Hodgkins M.L. Telehealth. N Engl J Med. 2017;377(16):1585–1592. doi: 10.1056/NEJMsr1503323. [DOI] [PubMed] [Google Scholar]
- 7.Marcin JP, Rimsza ME, Moskowitz WB, WB Moskowitz. The use of telemedicine to address access and physician workforce shortages. Pediatrics. 2015;136(1):202–209. [DOI] [PubMed]
- 8.World Health Organization WHO Director-General’s opening remarks at the media briefing on COVID-19 – 11 March 2020. https://www.who.int/dg/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19---11-march-2020 Available at:
- 9.US Department of Health and Human Services Notification of enforcement discretion for telehealth remote communications during the COVID-19 nationwide public health emergency. https://www.hhs.gov/hipaa/for-professionals/special-topics/emergency-preparedness/notification-enforcement-discretion-telehealth/index.html Available at:
- 10.Scott Kruse C., Karem P., Shifflett K., Vegi L., Ravi K., Brooks M. Evaluating barriers to adopting telemedicine worldwide: a systematic review. J Telemed Telecare. 2018;24(1):4–12. doi: 10.1177/1357633X16674087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Verma R., Krishnamurti T., Ray K.N. Parent perspectives on family-centered pediatric electronic consultations: qualitative study. J Med Internet Res. 2020;22(4) doi: 10.2196/16954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wilson F.A., Rampa S., Trout K.E., Stimpson J.P. Reimbursements for telehealth services are likely to be lower than non-telehealth services in the United States. J Telemed Telecare. 2016;23(4):497–500. doi: 10.1177/1357633X16652288. [DOI] [PubMed] [Google Scholar]
- 13.Center for Connected Health Policy State Telehealth Laws and Reimbursement Policies report. https://www.cchpca.org/telehealth-policy/state-telehealth-laws-and-reimbursement-policies-report Available at:
- 14.Center for Connected Health Policy Telehealth Private Payer Laws: Impact and Issues. https://www.milbank.org/publications/telehealth-private-payer-laws-impact-issues/
- 15.California Legislative Information AB-744: Health Care Coverage: Telehealth. Assembly Bill 744: Chapter 867. https://leginfo.legislature.ca.gov/faces/billTextClient.xhtml?bill_id=201920200AB744 Available at:
- 16.Center for Medicare & Medicaid Services Medicare telemedicine health care provider fact sheet. https://www.cms.gov/newsroom/fact-sheets/medicare-telemedicine-health-care-provider-fact-sheet
- 17.Gurupur V., Shettian K., Xu P. Identifying the readiness of patients in implementing telemedicine in northern Louisiana for an oncology practice. Health Inform J. 2016;23(3):181–196. doi: 10.1177/1460458216639740. [DOI] [PubMed] [Google Scholar]
- 18.Morgan D.G., Kosteniuk J., Stewart N., O’Connell M.E., Karunanayake C., Beever R. The telehealth satisfaction scale: reliability, validity, and satisfaction with telehealth in a rural memory clinic population. Telemed J e-Health. 2014;20(11):997–1003. doi: 10.1089/tmj.2014.0002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Shah T.K., Tariq T., Phillips R. Health care for all: effective, community supported, healthcare with innovative use of telemedicine technology. J Pharm Policy Pract. 2018;11(1):3. doi: 10.1186/s40545-018-0130-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ray K.N., Mehrotra A., Yabes J., Kahn J.M. Telemedicine and outpatient subspecialty visits among pediatric Medicaid beneficiaries [e-pub ahead of print]. Acad Pediatr. [DOI] [PMC free article] [PubMed]
- 21.Barnett M.L., Yee H.F.J., Mehrotra A., Giboney P. Los Angeles Safety-Net Program eConsult System was rapidly adopted and decreased wait times to see specialists. Health Aff (Millwood) 2017;36(3):492–499. doi: 10.1377/hlthaff.2016.1283. [DOI] [PubMed] [Google Scholar]
- 22.Lesher A.P., Fakhry S.M., DuBose-Morris R. Development and evolution of a statewide outpatient consultation service: leveraging telemedicine to improve access to specialty care. Popul Health Manag. 2020;23(1):20–28. doi: 10.1089/pop.2018.0212. [DOI] [PubMed] [Google Scholar]
- 23.Kruse C.S., Krowski N., Rodriguez B., Tran L., Vela J., Brooks M. Telehealth and patient satisfaction: a systematic review and narrative analysis. BMJ Open. 2017;7(8) doi: 10.1136/bmjopen-2017-016242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Lin N.Y., Ramsey R.R., Miller J.L. Telehealth delivery of adherence and medication management system improves outcomes in inner-city children with asthma. Pediatr Pulmonol. 2020;55:1–8. doi: 10.1002/ppul.24623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.American Medical Association Telehealth Implementation Playbook. https://www.ama-assn.org/terms-use Available at:
- 26.American Telemedicine Association ATA state telemedicine toolkit. https://www.americantelemed.org/resource_categories/practice-guidelines/ Available at:
- 27.American Academy of Pediatrics Getting Started in Telehealth. https://www.aap.org/en-us/professional-resources/practice-transformation/telehealth/Pages/Getting-Started-in-Telehealth.aspx Available at:
- 28.National Consortium of Telehealth Resource Centers Telehealth Policy Issues. https://www.telehealthresourcecenter.org/ Available at:
- 29.Crossen S., Raymond J., Neinstein A.B. Top ten tips for successfully implementing a diabetes telehealth program [e-pub ahead of print]. Diabetes Technol Ther. https://doi.org/10.1089/dia.2020.0042 [DOI] [PMC free article] [PubMed]