Abstract
A 42-year-old man was admitted for an ST-segment elevation myocardial infarction revealing an acute thrombosis of the left anterior descending and right coronary arteries. Following this acute multivessel coronary occlusion in a young individual at low cardiovascular risk, he tested positive for severe acute respiratory syndrome-coronavirus-2 infection. (Level of Difficulty: Beginner.)
Key Words: acute coronary syndrome, arterial thrombosis, coronavirus disease-2019, myocardial infarction, SARS-CoV-2
Abbreviations and Acronyms: COVID-19, coronavirus-2019; SARS-CoV-2, severe acute respiratory syndrome-coronavirus-2; STEMI, ST-segment elevation myocardial infarction; ULN, upper limit of normal value
Graphical abstract
A 42-year-old man was admitted for an ST-segment elevation myocardial infarction revealing an acute thrombosis of the left anterior descending and right coronary arteries. F…
Presentation
A 42-year-old man without significant medical history was admitted to the catheterization laboratory for an ST-segment elevation myocardial infarction (STEMI). He felt a constrictive chest pain for the previous 4 h. He reported a single episode of fever at 38.0°C 2 weeks prior to the event, with no other symptoms. He had no signs of shock, shortness of breath, or fever. His physical examination findings were normal, with no sign of heart failure, pneumonia, or deep venous thrombosis.
Learning Objectives
-
•
ST-segment elevation myocardial infarction with a high thrombus burden can appear as the first and only onset of COVID-19 symptoms.
-
•
Plaque rupture in predisposed patients with cardiovascular risk factors can be enhanced by severe inflammation and worsened by prothrombotic characteristics of this new infectious disease.
-
•
In the course of this COVID-19 pandemic, SARS-CoV-2 infection should probably be ruled out in patients with unusual or severe thrombotic and ischemic events, even when there are no symptoms of COVID-19 disease.
Medical History
The patient reported an active lifestyle with a history of playing competitive football and had a body mass index of 27 kg/m2. He had no significant medical history except for past smoking (20 pack-years), which he had quit 2 years before. He had no family history of cardiovascular disease and was taking no medication or drugs.
Differential Diagnosis
No diagnosis other than a STEMI was possible.
Investigations
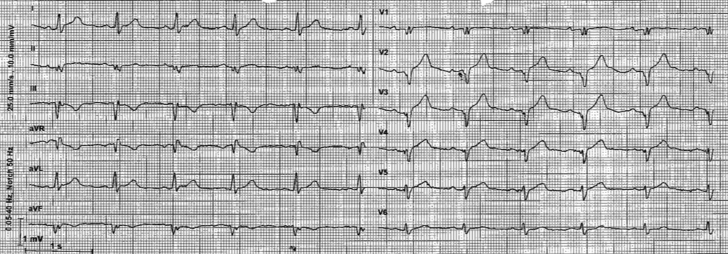
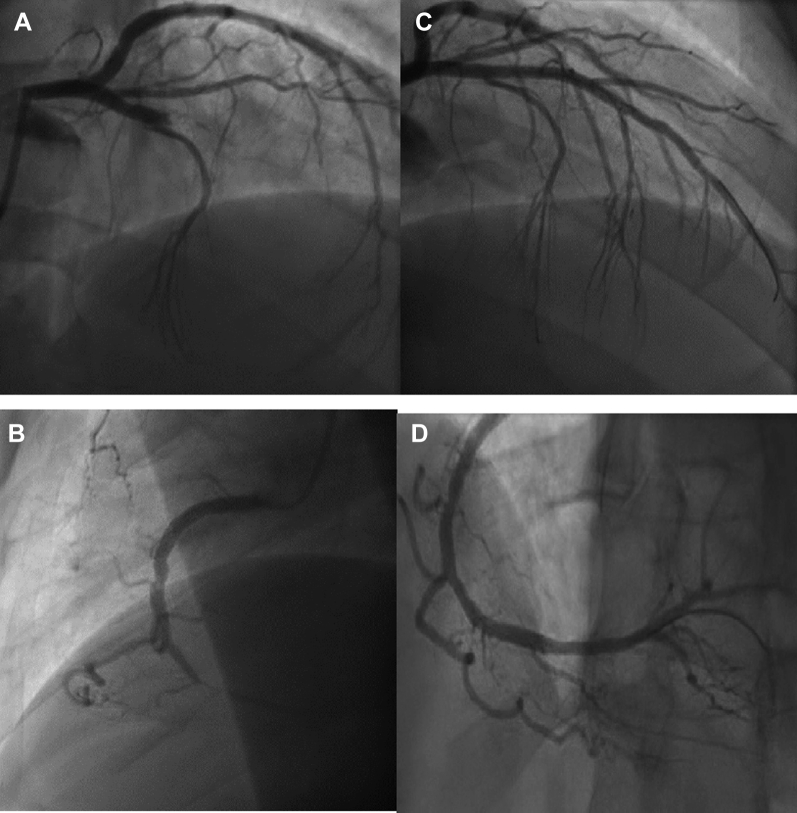
The initial electrocardiogram displayed a sinus rhythm with an anterior ST-segment elevation and Q waves with negative T waves in the inferior leads (Figure 1). Coronary angiography was immediately performed and revealed an acute thrombotic occlusion with a grade 0 thrombolysis in myocardial infarction flow in both the proximal left anterior descending and the distal right coronary arteries (Figure 2). Percutaneous coronary intervention was performed, and 2 drug-eluting stents were implanted in the left anterior descending and right coronary arteries, with an optimal result leading to the resolution of chest pain.
Figure 1.
Initial Electrocardiogram
Figure 2.
Coronary Angiography
(A) Thrombotic occlusion of proximal left anterior descending artery. (B) Left anterior descending artery after percutaneous coronary intervention. (C) Thrombotic occlusion of distal right coronary artery. (D) Right coronary artery after percutaneous coronary intervention.
Laboratory tests indicated increased troponin concentration of 6,269 ng/l (ULN <14 ng/l), an N-terminal pro–B-type natriuretic peptide concentration of 1,012 ng/l (ULN <250 ng/l), D-dimers under 240 ng/ml, an inflammatory syndrome with a white blood count of 10 g/l, and a fibrinogen concentration of 5.5 g/l. The low-density lipoprotein cholesterol level was measured at 94 mg/dl, the apolipoprotein I concentration was 94 mg/dl, high-density lipoprotein cholesterol concentration was 27 mg/dl, and serum triglyceride concentration was 139 mg/dl.
Because of the severe presentation in this low-risk young adult patient, a nasopharyngeal swab sample was taken and tested using reverse transcriptase-polymerase chain reaction and was found positive for severe acute respiratory syndrome-coronavirus-2 (SARS-CoV-2) infection.
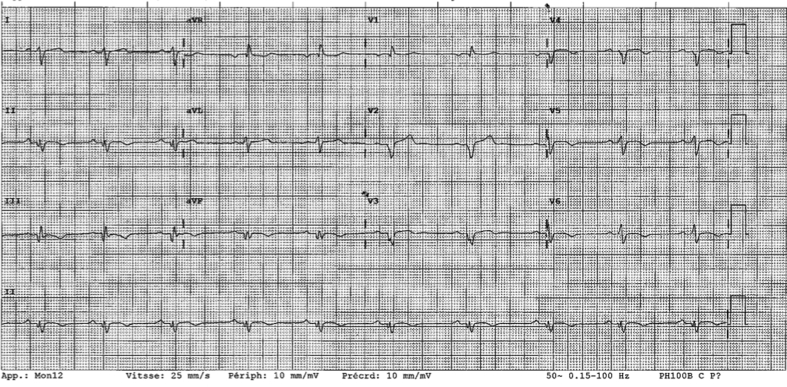
The initial echocardiography showed a large anterior apical and inferior sequela with a reduced left ventricular ejection fraction of 40%, without right ventricular dysfunction. The contrast echocardiography ruled out a patent foramen ovale. The chest radiograph result was normal. Leiden V mutation as well as protein S and C deficits and antiphospholipid syndrome were ruled out. Toxicological screening in urine showed no recent toxic consumption. The patient did not present any arrhythmic episode during the 4-day hospital stay. The electrocardiogram at discharge is displayed in Figure 3.
Figure 3.
Electrocardiogram at Discharge
Management
A dual-antiplatelet therapy with aspirin and ticagrelor was initiated prior to hospital admission, as well as enoxaparin, which was prolonged during the hospital stay. A glycoprotein IIb/IIIa inhibitor was prescribed during the procedure. The patient was discharged with a prescription for dual-antiplatelet therapy and was provided with protective measures to prevent any transmission of coronavirus-2019 (COVID-19) before discharge.
Discussion
Myocardial infarction in young adults is an increasing public health issue. The typical profile of these individuals involves active smoking, high low-density lipoprotein cholesterol levels, or a premature family history of coronary artery disease. Conventionally, this profile features a single-vessel disease with a localized thrombotic occlusion, whereas other arteries display a normal angiographic aspect (1). Nonetheless, this individual with a low cardiovascular risk presented with 2 simultaneous acute occlusions of 2 coronary arteries of thrombotic and not embolic angiographic aspect. This suggests a significant thrombus burden that could have been triggered by COVID-19 disease.
COVID-19 infection comes with various clinical presentations. In addition to the influenza-like and gastrointestinal symptoms, COVID-19 is now well described as a prothrombotic disease with a high prevalence of thromboembolic venous complications, as well as acute arterial ischemic events. Myocardial infarction related to COVID-19 disease seems to be common, as suggested by a recently published series (2). The inflammatory state induced by SARS-CoV-2 is indeed described as associated with a higher local immune response and more frequent atherosclerotic plaque erosions or ruptures causing type 1 myocardial infarction. Adjunctive factors such as hypoxemia and endothelial injury induced by the cytokine storm could play an important part in the process. Of note, other respiratory viruses, such as influenza viruses, are associated with more frequent myocardial infarction (3). Indeed, local inflammation inside the plaques can boost the production of collagenase by macrophages, thereby degrading and weakening the fibrous cap, which can induce plaque rupture and thrombotic acute coronary syndrome. Nevertheless, myocardial infarction in such infectious settings is not always tied to severe clinical or biological signs of sepsis. In fact, an observational study of 2,287 patients presenting with myocardial infarction during pneumonia found that 16% of the patients had no sign of sepsis (4). In the present case, the patient presented with negative D-dimers but a high level of fibrinogen. Moreover, the concomitant occlusion of 2 coronary arteries is a good illustration of the prothrombotic state likely induced by COVID-19 disease. The hypothesis of the thrombotic role of COVID-19 is reinforced by the exclusion of other diagnoses such as multiple emboli associated with atrial fibrillation or a patent foramen ovale. Similarly, no thrombophilia was detected.
Interestingly, this patient featured almost no COVID-19 symptoms prior to myocardial infarction, except for a transient feverish episode, spontaneously regressive within a few hours. The recent series by Stefanini et al. (5) showed that 85.7% of Lombard patients infected with COVID-19 with cardiovascular risk factors presenting for ST-segment elevation myocardial infarction did not show any infectious symptom before myocardial infarction. These observations suggest that ischemic events jeopardize patients infected with SARS-CoV-2, even when they have asymptomatic forms and are at low cardiovascular risk.
Follow-Up
The patient did not develop heart failure, or heart rhythm disturbances, or other complications of myocardial infarction. Furthermore, he remained free of COVID-19 disease symptoms.
Conclusions
In the context of the COVID-19 pandemic, unusual myocardial infarction presentations, such as in young individuals at low cardiovascular risk, should lead to testing for SARS-CoV-2 infection, even in asymptomatic patients. Because of the prothrombotic and inflammatory status enhanced by viral infection, COVID-19 disease is associated with a multitude of ischemic events, among which ST-segment elevation myocardial infarction remains common.
Footnotes
This study was led by the ACTION Study Group at the Institute of Cardiology of Pitié-Salpêtrière Hospital. Dr. Zeitouni has received research grants from Institut Servier and Fédération Française de Cardiologie and BMS/Pfizer. Dr. Silvain has received research grants from Amed, Amgen, Algorythm, AstraZeneca, Bayer, Daiichi-Sankyo, Eli Lilly, Fondation de France, Gilead Science, Iroko Cardio, Sanofi-Aventis, and St. Jude Medical. Dr. Montalescot has received research grants from Abbott, Amgen, Actelion, AstraZeneca, Bayer, Boehringer Ingelheim, Boston-Scientific, Bristol-Myers Squibb, Beth Israel Deaconess Medical, Brigham Women’s Hospital, Cardiovascular Research Foundation, Daiichi-Sankyo, Idorsia, Lilly, Europa, Elsevier, Fédération Française de Cardiologie, ICAN, Medtronic, Journal of the American College of Cardiology, Lead-Up, Menarini, Merck Sharp & Dohme, Novo-Nordisk, Pfizer, Sanofi, Servier, The Mount Sinai School, TIMI Study Group, and WebMD. All other authors have reported that they have no relationships relevant to the contents of this paper to disclose.
The authors attest they are in compliance with human studies committees and animal welfare regulations of the authors’ institutions and Food and Drug Administration guidelines, including patient consent where appropriate. For more information, visit the JACC: Case Reportsauthor instructions page.
References
- 1.Collet J.-P., Zeitouni M., Procopi N., Hulot J.-S., Silvain J., Kerneis M. Long-term evolution of premature coronary artery disease. J Am Coll Cardiol. 2019;74:1868–1878. doi: 10.1016/j.jacc.2019.08.1002. [DOI] [PubMed] [Google Scholar]
- 2.Bangalore S., Sharma A., Slotwiner A., Yatskar L., Harari R., Shah B. ST-segment elevation in patients with covid-19—a case series. N Engl J Med. 2020;382:2478–2480. doi: 10.1056/NEJMc2009020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Musher D.M., Abers M.S., Corrales-Medina V.F. Acute infection and myocardial infarction. N Engl J Med. 2019;380:171–176. doi: 10.1056/NEJMra1808137. [DOI] [PubMed] [Google Scholar]
- 4.Corrales-Medina V.F., Musher D.M., Wells G.A., Chirinos J.A., Chen L., Fine M.J. Cardiac complications in patients with community-acquired pneumonia: incidence, timing, risk factors, and association with short-term mortality. Circulation. 2012;125:773–781. doi: 10.1161/CIRCULATIONAHA.111.040766. [DOI] [PubMed] [Google Scholar]
- 5.Stefanini G.G., Montorfano M., Trabattoni D., Andreini D., Ferrante G., Ancona M. ST-elevation myocardial infarction in patients with COVID-19: clinical and angiographic outcomes. Circulation. 2020;141:2113–2116. doi: 10.1161/CIRCULATIONAHA.120.047525. [DOI] [PMC free article] [PubMed] [Google Scholar]