Abstract
Introduction
The impact of COVID-19 pandemic on pediatric surgical care systems is unknown. We present an initial evaluation of self-reported pediatric surgical policy changes from hospitals across North America.
Methods
On March 30, 2020, an online open access, data gathering spreadsheet was made available to pediatric surgeons through the American Pediatric Surgical Association (APSA) website, which captured information surrounding COVID-19 related policy changes. Responses from the first month of the pandemic were collected. Open-ended responses were evaluated and categorized into themes and descriptive statistics were performed to identify areas of consensus.
Results
Responses from 38 hospitals were evaluated. Policy changes relating to three domains of program structure and care processes were identified: internal structure, clinical workflow, and COVID-19 safety/prevention. Interhospital consensus was high for reducing in-hospital staffing, limiting clinical fellow exposure, implementing telehealth for conducting outpatient clinical visits, and using universal precautions for trauma. Heterogeneity in practices existed for scheduling procedures, implementing testing protocols, and regulating use of personal protective equipment.
Conclusions
The COVID-19 pandemic has induced significant upheaval in the usual processes of pediatric surgical care. While policies evolve, additional research is needed to determine the effect of these changes on patient and healthcare delivery outcomes.
Level of evidence
III
Abbreviations: APSA, American Pediatric Surgical Association; APSTPD, Association for Pediatric Surgery Training Program Directors; ACS, American College of Surgeons; COVID-19, Corona Virus Disease-2019; ICU, Intensive Care Unit; PUI, Person Under Investigation; PPE, Personal Protective Equipment; QSC, Quality and Safety Committee
Key words: COVID-19 response, Surgical quality and safety, Pediatric surgery, Disaster management, Disaster response, Pandemic
Shortly after the arrival of SarsCov2 (also known as Corona Virus Disease-2019 [COVID-19]) to the United States, hospitals and care systems began preparing for the expected onslaught of patients progressing rapidly through mild respiratory symptoms to severe pulmonary illness [[1], [2], [3]]. Initial evidence demonstrated a higher prevalence of COVID-19 disease in the adult population, while data surrounding pediatric populations have been comparably sparse [[4], [5], [6], [7]]. Hospitals that provide healthcare for children have had to make major changes to day-to-day operations despite the fact that COVID-19 affects relatively few pediatric patients. An ideal response to the pandemic would incorporate changes to promote social distancing and minimize exposure without compromising delivery of time-sensitive healthcare for children. It is unclear how this balance can best be achieved. Furthermore, guidelines from the Center of Disease Control and Prevention (CDC) toward public, hospital, and government behaviors have been changing rapidly [8,9]. As the COVID-19 response continues to evolve, the degree to which structural changes have translated to the frontline of pediatric surgical care is unknown.
To address this knowledge gap, the American Pediatric Surgical Association (APSA) Quality and Safety Committee (QSC) created an open source online spreadsheet accessible to all pediatric surgeons designed to share hospital policy changes (https://www.pedsurglibrary.com/apsa/view/PedSurg%20Resource/1884034/all/COVID_19_for_Pediatric_Surgeons?q=covid-19) [10]. The document opened on March 31, 2020 with requests for information on hospital policies for staffing, patient care, and COVID-19 prevention and safety. In this article, we present a summary of the first month of the pandemic response across hospitals offering children's surgical care in North America.
1. Methods
An open access online document was made accessible to pediatric surgeons across North America through the American Pediatric Surgical Association (APSA) Pediatric Surgical Library: COVID-19 for Pediatric Surgeons Information page [10]. The link to the document was made publicly available on this APSA COVID-19 page, and, concurrently, responses were directly solicited from the APSA Quality and Safety Committee (QSC), the APSA Outcomes committee, and the Association for Pediatric Surgery Training Program Directors (APSTPD). Surgeons were asked to provide information reflecting policy in their local environments, update the information as policy changes occurred, and share the link with surgeons at other hospitals. Items were developed and compiled by a subcommittee of the APSA QSC to address issues related to pandemic response. At the time of evaluation, the document included 30 questions on policy changes for a variety of topics related to pediatric surgical care, as well as influences of these changes on resident and fellow training. Responses were collected from March 31, 2020 through April 16, 2020. Questions were divided into domains (Internal Structural Changes, Clinical Flow Changes, Safety and Prevention Changes, Resident and Fellow Training) based on topic of process change addressed. Hospitals were divided into freestanding children's hospitals (independent of adult academic institutions and exclusively caring for pediatric populations), affiliated children's hospitals (associated with adult healthcare system and largely caring for pediatric populations), or children's units nested within adult hospitals. Individual responses were converted from qualitative responses into a numeric coding system based on the item asked [11]. Coded responses were then compiled and analyzed in aggregate.
Latest response dates were analyzed in relation to each representative state's projected COVID-19 surge date. Determination of the surge date was obtained from the Institute of Health Metrics Evaluation webpage [12]. Descriptive analyses were performed to describe hospital responders by type of children's hospital (freestanding or nested within adult hospital), presence of pediatric surgical fellowship, and date of last update relative to anticipated COVID-19 surge. Scatterplot of these time intervals demonstrated time interval cut-points of 10 days and 21 days, which were used to distribute respondents into three time groups (within 1–10 days, 11–20 days, and 21–31 days of predicted surge response). One-way ANOVA was performed to evaluated differences between mean number of changes reported in each policy domain (Internal Structural, Clinical Flow, and Safety/Prevention) by category of update time, relative to date of predicted COVID-19 surge. All coding, descriptive statistics, and summative evaluation were performed using Microsoft Excel (2019) and SAS Software, Version 9.4, SAS Institute Inc., Cary N.C.
2. Results
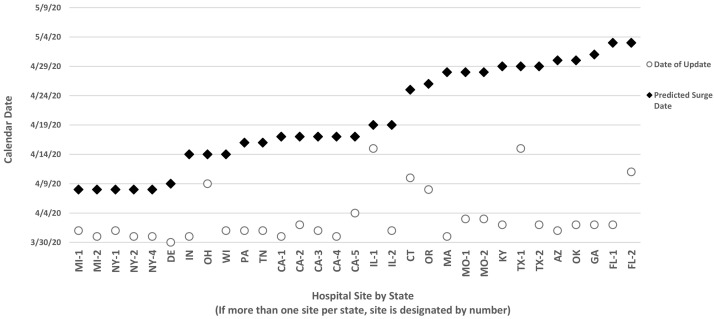
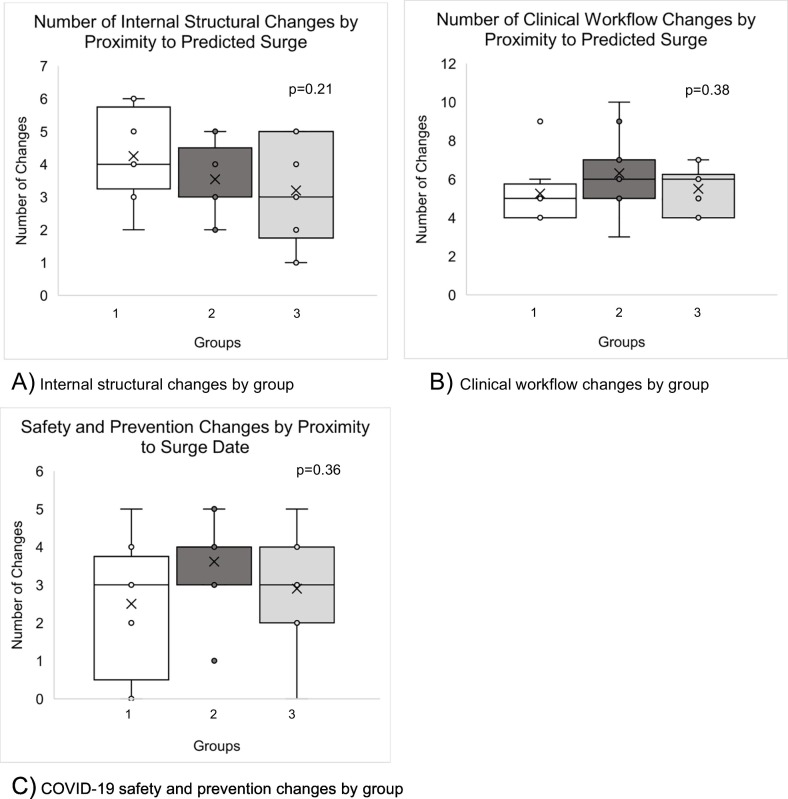
At the time of evaluation, responses from 38 hospitals across 7 regions of North America were included (Table 1 ). Hospital representation included 15 free-standing children's hospitals (40%), 23 children's hospitals affiliated with an adult hospital system (60%), and 0 (0%) unit nested within adult hospitals. Additionally, 36 hospitals (95%) represented sites with categorical pediatric surgery fellowships. Overall, hospitals reported a median of 4 changes related to Internal structure/staffing, (range 1–7 changes), 6 changes related to clinical workflow (range 1–10), and 3 changes related to Safety and COVID-19 Prevention (1–6 changes). Response dates ranged from a most recent update of March 31, 2020 to April 16, 2020. Fig. 1 depicts the variation in time between latest hospital response date (assuming multiple prior responses) and predicted surge date at the time of evaluation. Though many respondents may have contributed multiple times to the document over the access period, mean time interval between latest update and predicted surge was 17 days (mean 17 ± 8 days, range 4–31 days). On evaluation by one-way ANOVA, the mean number of policy changes reported for each domain was not found to vary significantly by number of days to predicted COVID-19 surge date (Fig. 2 ).
Table 1.
List of hospitals contributing to APSA open access data sharing spreadsheet.
| Participating hospitals | ||
|---|---|---|
| Children's Hospital of Richmond at VCU Cohen Children's Medical Center/ Northwell Connecticut Children's Medical Center Nemours-AI duPont Hospital for Children Oishei Children's/Univ at Buffalo Penn State Children's Hospital Stony Brook Children's Hospital Strong Memorial Hospital at University of Rochester Texas Children's Hospital UCSF Benioff Children's Hospital SF UCSF Benioff Children's Hospital Oakland |
Boston Children's Hospital Children's Hospital of Alabama Children's Healthcare of Atlanta Johns Hopkins All Children's Hospital Le Bonheur Children's Hospital Norton Children's Hospital University of Florida-Pediatrics Children's Hospital at Providence-Anchorage Doernbecher Children's Hospital-OHSU Children's Memorial Hermann Hospital (Houston) Lucile Packard Children's Hospital-Stanford Rady Children's Hospital San Diego Arkansas Children's Hospital |
Children's Hospital of Michigan Children's Mercy Hospitals and Clinics Children's Hospital of Wisconsin Ann & Robert H. Lurie Children's Hospital of Chicago University of Chicago-Comer Children's C. S. Mott Children's Hospital Nationwide Children's Hospital Oklahoma Children's Hospital Phoenix Children's Hospital Riley Children's Hospital St. Louis Children's Hospital Alberta Children's Hospital IWK Health Centre-Dalhousie University |
Fig. 1.
Variance in date of site update and date of state's predicted surge.
*Predicted surge date source (accessed 4/16/20): https://covid19.healthdata.org/united-states-of-america.
Responses from 38 programs regarding changes in hospital guidelines and procedures related to care of pediatric surgical patients in the COVID-19 pandemic. The relationship of dates of last update for the open access document relative to the respective state's predicted date of COVID-19 surge are shown.
Fig. 2.
(A–C) Number of changes by days until predicted COVID-19 surge.
Group 1 hospitals updated results within 10 days of predicted surge date, Group 2 updated within 11–20 days of predicted surge, and Group 3 updated within 21–30 days of predicted surge date.
2.1. Internal structural changes
Most hospitals reported significant staffing changes to minimize exposure of healthcare workers. Ninety-five percent (36 hospitals) reported decreasing staff coverage, and 37 hospitals (97%) reported also reducing clinical fellow coverage. Twenty-one (55%) hospitals converted to a weekend schedule with skeleton crew and one rounding team, while 12 (30%) hospitals reported converting to a Team A/Team B structure. Nineteen (50%) hospitals restricted the work duties of surgeons older than 65 years, surgeons with underlying medical conditions, and/or surgeons who were pregnant.
One in five hospitals (22%) reported that their hospital was sharing equipment with neighboring adult facilities. The most common equipment shared include ventilators from pediatric operating rooms and intensive care units (ICUs), followed by attending staff sharing duties with the adult facilities. A small minority (10%) of hospitals reported that their surgeons were covering adult services, including the Acute Care Surgical service and Surgical ICUs. Five hospitals (13%) reported that they were actively accepting adult patients, and 13 hospitals (34%) reported that plans were in place to do so in the case of decreased local adult capacity during a COVID-19 surge. Among these 18 sites, 4 (22%) reported willingness or active acceptance of COVID-19 positive adults, while the majority were planning to accept only adult patients who were COVID-19 negative, or not considered to be persons under investigation (PUIs).
2.2. Clinical flow changes
2.2.1. Patient transfers and consultations
Given the potential for redistribution of pediatric patients to free up space for adult patients, we asked respondents about pediatric patient transfers within their systems. Thirty (80%) pediatric surgical hospitals reported that they were not needing to transfer pediatric patients away from their centers for general or trauma care, in order to cohort and care for COVID-19 positive patients. Four (10%) hospitals specifically reported that they were receiving more pediatric patients from neighboring regional or community hospitals, as those centers were working to limit patient exposure to COVID-19 positive adult patients.
The approach to management of trauma patients poses a particular challenge during COVID-19, since there is often no time to screen for symptoms or determine likelihood of infection, and many of these patients might need to undergo aerosolizing procedures urgently, such as intubation. Most (87%) of hospitals reported using universal PPE when caring for trauma patients. Twenty-two hospitals (57%) reported that they considered all trauma patients to be COVID-19 PUIs, and required use of N95 and safety goggles or face shields during trauma assessments. Only 6% of hospitals reported selective use of N95 for symptomatic patients or those undergoing active COVID-19 positive screening, level 1 traumas, or patients needing airway management.
2.2.2. Operative scheduling and workflow processes
In the wake of the changes listed above, and following the mandate of the American College of Surgeons (ACS) [8], 38 (100%) of hospitals reported canceling elective operations. The approach to operative case scheduling for nonelective cases was found to vary among reporting hospitals. Approximately 1/3 of hospitals exclusively used American College of Surgeons (ACS) guidelines [8] to determine whether cases should be rescheduled, 1/3 of hospitals used ACS guidelines and evaluated inclusion on a case-by-case basis, and 1/3 of hospitals were requiring hospital or division leadership to sign off approval for proceeding with a submitted case before it could be scheduled.
All hospitals reported that anesthesiology teams were required to wear full PPE with N95 and safety goggles for intubation of COVID-19 positive or PUI in the operating room. At the time of evaluation, one third of hospitals were routinely performing COVID-19 testing preoperatively. Of these, 11 hospitals (83%) were testing all semi-urgent patients before their operative procedure, while the rest only reported ability to test eligible PUIs before surgery.
Risk of COVID-19 transmission has also influenced hospitals to consider reducing use of laparoscopy for operations, and in some cases, to restructure management of pediatric appendicitis. Overall, 27 (71%) hospitals reported changing their guidelines and practices around use of laparoscopy. Twenty-two (64%) hospitals reported using filtration during laparoscopy for all patients, and five (23%) of these hospitals reported minimizing use of laparoscopy to reduce potential healthcare worker exposure to COVID-19. An additional 15% of hospitals reported that they had not yet made changes, but were considering limiting laparoscopy to reduce spread. Half of surgeons (47%) reported not changing usual pathways of care for managing appendicitis, but 10% (four hospitals) reported that they were considering a change. Of the remaining 19 respondents, three (13%) reported that their hospitals were uniformly treating acute appendicitis nonoperatively (a change from prior practice), and nine (25%) hospitals were (newly) making decisions for nonoperative appendicitis on a case-by-case basis.
2.2.3. Implementation of telehealth
The COVID-19 pandemic has led to a marked increase in telehealth across nearly all hospitals. Thirty-six (95%) hospitals reported early conversion to telehealth for outpatient clinic visits. Of these participating in telehealth, 28 hospitals (78%) reported that their providers were able to conduct clinic visits from home. Finally, 10 hospitals (26%) reported use of telehealth for inpatient consults and transfer evaluations, further limiting in-person physical exams and presurgical evaluations.
2.3. Policies around COVID-19 safety and prevention
By far, the most common guidelines in this domain centered around universal masking policies, patient visitation, COVID-19 testing, and mechanisms of preserving N95 masks. Twenty-five hospitals (67%) reported implementation of universal masking policies in their hospitals. Eight (33%) required staff and healthcare workers alone to wear masks, compared with 14 (55%) extending this regulation to include staff and families. Thirty-two of the hospitals (84%) were restricting patient visitors to one or zero caregivers. Among hospitals allowing visitors, the most common policy indicated that the list of allowable visitors was established at the time of admission, and was not permitted to change over the course of the patient's stay. Additionally, 22 hospitals (57%) reported that they were cohorting PUIs with true COVID-19 positive patients. Importantly, hospitals reported persistently long wait times for COVID-19 results, with 75% of hospitals reporting wait times of 12 h or longer (IQR 4–72 h).
Finally, 75% of hospitals reported sterilizing or reusing N95 masks. The most common policy reported among hospitals was reuse of masks until soiled or dirty, with most policies allowing reuse up to 10 days. Among the 6 hospitals who reported sterilizing N95 masks, 4 reported using ultraviolet light sterilization, and 2 reported using hydrogen peroxide sterilization techniques.
2.4. Impact on resident and fellow training
Within each of these domains, hospitals specifically reported on several changes impacting resident and fellow duties and training. Nearly every hospital associated with a clinical fellowship reported decreasing fellow presence on service and in the operating room. The most common policies included separating clinical fellows from one another, alternating their weeks on-service (95% of hospitals) and limiting fellow presence in cases with PUI or COVID-19 positive patients (42% of hospitals). Clinical education and training for surgical residents were also described as restrictive in favor of social distancing practices. Thirteen percent of hospitals reported excluding surgical residents entirely from operations with COVID-19 positive patients. Hospitals also report having surgical residents stay outside of PUI or COVID-19 positive exam rooms for rounds, traumas, or consultations in order to limit the number of physicians exposed (30%). Additionally, 44% of hospitals reported that rotating surgical residents were being pulled away from their pediatric surgical rotation to help with coverage of COVID-19 patients in their home (adult) hospitals. Finally, 97% of hospitals reported that they had transitioned didactics to remote or online sessions only, with only 1 hospital having to cancel didactics entirely in light of the pandemic.
3. Discussion
Optimal guidance around appropriate or expected COVID-19 response for pediatric surgical hospitals has been limited and mostly extrapolated from adult practices. In this report, we demonstrate that the number and type of changes occurring among and within hospitals have been significant, and continually dynamic. We did not find that hospitals at dates closer to the state's predicted surge data implemented more changes than those hospitals who were further away from surge date at the time of evaluation. This is likely related to the fact that local policy change is likely to be driven by local response to the pandemic, which does not necessarily correlate with surge proximity. There are many factors affecting the number and types of changes occurring in institutions including local government restrictions such as shelter-in-place orders, governor mandates calling for cancellation of all elective surgery, and others.
Nonetheless, while there is tremendous variability in the challenges faced by pediatric institutions throughout the country, hospitals independently developed similar approaches to both care for patients and protect their teams. The most immediate and common changes included implementing protocols to reduce healthcare worker presence in the hospital (including residents and “vulnerable” surgeons), reducing inpatient volume to conserve resources, and modifying guidelines for operations (including laparoscopic operations and management of appendicitis) to minimize frequency of aerosol-generating procedures. We also observed that variability existed across hospitals in their abilities to provide essential prevention and safety measures during the initial response. For example, only 2/3 of hospitals reported universal masking procedures in place, and only 1/3 of hospitals were found to offer preoperative COVID-19 testing for patients. In addition, rates of at-home telemedicine for physicians and capacity for rapid COVID-19 testing of inpatients were lower than expected. These findings suggest that increasing technical support across pediatric surgical hospitals may be necessary for improving response [13].
While this report provides a glimpse into the activity surrounding COVID-19 response for pediatric surgical hospitals, many unanswered questions remain. First and foremost, we do not yet know the effect of these clinical workflow and internal structural changes on patient outcomes. For example, the 26% of hospitals that are conducting inpatient consults and transfer evaluations remotely using telehealth have introduced a dramatic change in the dynamics of patient–provider communication. Even prior to the pandemic, clinicians have held significant apprehension using telemedicine to evaluate pediatric physical exams [14], and applications of telehealth to surgical care have been ongoing areas of investigation [15]. Nonetheless, despite unknowns or apprehension around the service, introduction of a greater need to preserve workforce and maintain social distancing has pushed hospitals to adopt these systems rapidly. Further, we do not yet know the effect of delaying seemingly “elective” cases, including hernia repairs or enterostomy reversals [8], may have for children's health. Concerns about unintended consequences have been raised for adult patients [13] and the risk/benefit ratio for pediatric patients may be even less favorable, since the risk of pediatric morbidity from COVID-19 appears to be comparably low [4,7]. Tracking the short- and long-term outcomes of the unique cohort of pediatric patients treated within surgical centers through the pandemic will be incredibly valuable and informative for future innovations and policies implemented in healthcare.
Second, hospital practices to increase healthcare worker social distancing, and limit exposure of trainees to clinical units, have held significant implications for trainee education. We observed that 95% of hospitals participating in the document support pediatric surgical fellowships. Though most hospitals reported continuing education virtually, the loss of clinical learning associated with limited in-person consultations and evaluations cannot be overstated. Further, efforts to limit fellow coverage in the operating room may have a potentially deleterious effect on graduating fellow case volumes, which has not yet been quantified. The significance of this phenomenon is underscored by the fact that the American Board of Surgery has published hardship modifications to pediatric surgery training requirements including reductions in required time on service and minimum case volumes [16]. These concerns extend to resident trainees as well, whose exposure to pediatric surgery is likely to be compromised if they are pulled back to their home programs or have schedules truncated in a team A/team B fashion. The importance of increasing healthcare worker safety by implementation of social distancing measures is not disputed; however, the effects of these measures on training of future generations have yet to be determined.
An inherent limitation of the data presented in this report is the dynamic nature and rapidly evolving environment of COVID-19 response. Hospital policies and guidelines are changing daily. These data represent a self-reported snapshot in time and do not fully describe the fluctuation of change occurring at the hospital level. These data also represent a convenience sampling of voluntary reporting that may have inherent biases in terms of hospitals that elected to participate. Nonetheless, a sampling of 38 hospitals from geographically diverse locations and practice types provides a unique glimpse of contemporary practices that may be generalizable. The importance of this work lies in its ability to capture a sense of priority, importance, and relevance, among pediatric hospitals, for policies guiding the balance of maintaining high quality of care and also healthcare worker safety. Leveraging the technical prowess, skill, and readiness of pediatric surgeons to combat and serve in a national pandemic with the existing responsibility of providing care for children is not easy, nor previously prescribed.
Because of the variability across the country (both in demand and response capability), it is not possible or ethical to establish a universal standard on many of the issues presented here. Therefore, the demonstration of these practices is hoped to serve as guidance of community-established “best practice” examples, which can be utilized by other hospitals in the absence of a universal standard. Certainly, further study is needed to examine effects of these changes, develop evidence-based practices, and guide future practice. Nonetheless, the information shared through this document reveals valuable themes for present and future investigation. We will continue to evaluate these changes iteratively in the weeks and months to come. Ultimately, we hope that these summative reports will help inform future policies and guidelines around pandemic response and pediatric surgical best practices.
4. Conclusion
Pediatric surgical response within the first month of the pandemic has been rapid, dynamic, and significantly directed toward protecting healthcare workers from contracting the virus, while innovating methods to provide high quality care to pediatric patients. The situation is dynamic, and the full impact of these changes on patient outcomes is still unknown.
Footnotes
Acknowledgments: The authors would like to acknowledge Dr. Jon Ting, Dr. Ellen Reibling, Dr. Dustin Smith, and the APSA Quality and Safety Committee for assistance in providing question content and helping shape the open access database. The authors would also like to acknowledge all of the hospitals who have contributed to the database, and appreciate their input to generate the body of work presented in this article.
Funding Sources: Research reported in this publication was supported, in part, by the National Institutes of Health's National Center for Advancing Translational Sciences, Grant Number TL1TR001423 (author MI). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
References
- 1.CDC Coronavirus disease 2019 (COVID-19): healthcare professionals. 2020. https://www.cdc.gov/coronavirus/2019-nCoV/hcp/index.html [accessed April 26 2020.2020]
- 2.Pagano Monica, Hess John, Tsang Hamilton. Prepare to adapt: blood supply and transfusion support during the first 2 weeks of novel coronavirus (COVID-19) pandemic affecting Washington State. Transfusion. 2020;60(5):908–911. doi: 10.1111/trf.15789. [DOI] [PubMed] [Google Scholar]
- 3.Antommaria Armand, Gibb Tyler, McGuire Amy. Ventilator triage policies during the COVID-19 pandemic at US hospitals associated with members of the association of bioethics program directors. Ann Intern Med. 2020;(M20-1738) doi: 10.7326/M20-1738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ludvigsson Jonas. Systematic review of COVID-19 in children shows milder cases and a better progrnosis than in adults. Acta Paediatr. 2020;109(6):1088–1095. doi: 10.1111/apa.15270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Zeng Lingkong, Xia Shiwen, Yuan Wenhao. Neonatal early-onset infection with SARS-CoV-2 in 33 neonates born to mothers with COVID-19 in Wuhan, China. JAMA Pediatr. 2020;(e200878) doi: 10.1001/jamapediatrics.2020.0878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Rasmussen Sonja, Thompson Lindsay. Coronavirus disease 2019 and children: what pediatric health care clinicians need to know. JAMA Pediatr. 2020 doi: 10.1001/jamapediatrics.2020.1224. [DOI] [PubMed] [Google Scholar]
- 7.CDC Coronavirus disease 2019 in children—United States. 2020. https://www.cdc.gov/mmwr/Novel_Coronavirus_Reports.html [DOI] [PMC free article] [PubMed]
- 8.COVID-19: elective case triage guidelines for surgical care. 2020. https://www.cdc.gov/coronavirus/2019-nCoV/hcp/index.html [accessed April 26 2020.2020]
- 9.Create a surgical review committee for COVID-19 related surgical triage decision-making. 2020. https://www.facs.org/covid-19/clinical-guidance/review-committee [2020]
- 10.Berman L., Newton C., Powell D. APSA Quality and Safety Committee COVID-19 data sharing database. 2020. https://www.pedsurglibrary.com/apsa/view/PedSurg%20Resource/1884034/all/COVID_19_for_Pediatric_Surgeons#2 [accessed April 16 2020.2020]
- 11.O'Brien B., Harris I., Beckman T. Standards for reporting qualitative research: a synthesis of recommendations. Acad Med. 2014;89(9):1245–1251. doi: 10.1097/ACM.0000000000000388. [DOI] [PubMed] [Google Scholar]
- 12.COVID-19 projections. 2020. https://covid19.healthdata.org/united-states-of-america [accessed April 16 2020.2020]
- 13.Rosenbaum Lisa. The untold toll—the pandemic’s effects on patients without Covid-19. N Engl J Med. 2020;382(24):2368–2371. doi: 10.1056/NEJMms2009984. [DOI] [PubMed] [Google Scholar]
- 14.Haimi M., Brammli-Greenberg S., Waisman Y. Physicians' experiences, attitudes, and challenges in a pediatric telemedicine service. Pediatr Res. 2018;84:650–656. doi: 10.1038/s41390-018-0117-6. [DOI] [PubMed] [Google Scholar]
- 15.Harting M., Wheeler A., Ponsky T. Telemedicine in pediatric surgery. J Pediatr Surg. 2019;54(3):587–594. doi: 10.1016/j.jpedsurg.2018.04.038. [DOI] [PubMed] [Google Scholar]
- 16.COVID-19 FAQs: hardship modifications to pediatric surgery training requirements. 2020. http://www.absurgery.org/default.jsp?faq_pshardship [accessed April 28 2020.2020]