Abstract
Background
Health care systems struggle to identify risk factors for suicide. Adverse social determinants of health (SDH) are strong predictors of suicide risk, but most electronic health records (EHR) do not include SDH data.
Objective
To determine the prevalence of SDH documentation in the EHR and how SDH are associated with suicide ideation and attempt.
Design
This cross-sectional analysis included EHR data spanning October 1, 2015–September 30, 2016, from the Veterans Integrated Service Network Region 4.
Participants
The study included all patients with at least one inpatient or outpatient visit (n = 293,872).
Main Measurements
Adverse SDH, operationalized using Veterans Health Administration (VHA) coding for services and International Statistical Classification of Diseases and Related Health Problems (ICD)-10 codes, encompassed seven types (violence, housing instability, financial/employment problems, legal problems, familial/social problems, lack of access to care/transportation, and nonspecific psychosocial needs). We defined suicide morbidity by ICD-10 codes and data from the VHA’s Suicide Prevention Applications Network. Logistic regression assessed associations of SDH with suicide morbidity, adjusting for socio-demographics and mental health diagnoses (e.g., major depression). Statistical significance was assessed with p < .01.
Key Results
Overall, 16.4% of patients had at least one adverse SDH indicator. Adverse SDH exhibited dose-response-like associations with suicidal ideation and suicide attempt: each additional adverse SDH increased odds of suicidal ideation by 67% (AOR = 1.67, 99%CI = 1.60–1.75; p < .01) and suicide attempt by 49% (AOR = 1.49, 99%CI = 1.33–1.68; p < .01). Independently, each adverse SDH had strong effect sizes, ranging from 1.86 (99%CI = 1.58–2.19; p < .01) for legal issues to 3.10 (99%CI = 2.74–3.50; p < .01) for non-specific psychosocial needs in models assessing suicidal ideation and from 1.58 (99%CI = 1.10–2.27; p < .01) for employment/financial problems to 2.90 (99%CI = 2.30–4.16; p < .01) for violence in models assessing suicide attempt.
Conclusions
SDH were strongly associated with suicidal ideation and suicide attempt even after adjusting for mental health diagnoses. Integration of SDH data in EHR could improve suicide prevention.
KEY WORDS: social determinants of health, electronic health records, suicide, attempted, suicidal ideation, Veterans
INTRODUCTION
Social factors are linked to health in various and complex ways and are critical for understanding biomedical outcomes and health care utilization.1 For example, social disruptions (e.g., relationship dissolution, financial insecurity, legal problems, exposure to childhood adversity) are well-known precipitating events to suicidal behavior.2–5 The increasing attention to and mounting evidence of social determinants’ impacts on health (and thus health care) are stark testaments that health care providers should ask about social determinants of health (SDH) and account for these factors when planning treatment, and that electronic health record (EHR) systems should include patients’ social and behavioral data.6
Documentation of SDH in EHRs has evolved slowly in the USA. For example, the National Academy of Medicine’s recommendations for collection of social and behavioral determinants of health was only issued in 2014,7 decades after several seminal studies about the roles of social determinants of population health.8, 9 Delayed uptake of SDH documentation in EHR may be attributable to health care systems’ historical focus on biological mechanisms of individual health and disease. Health care systems are challenged with broadening conceptualization of health from individual biology and health behaviors/risks to include both dynamic social forces outside clinical walls and services that may not “look” like clinical care but have major ramifications for patients. For example, Taylor and colleagues’ review of the integration of SDH into health care found that, overall, supportive housing services integrated into models of care resulted in both improved patient outcomes and lower health care costs across several patient populations (e.g., women, children, patients living with HIV).10
With over 8 million enrollees, the Veterans Health Administration (VHA) is the United States’ single largest integrated health care system, annually providing care to over 6 million patients.11 VHA is both obligated to address eligible Veterans’ medical issues and expected to acknowledge and respond to Veterans’ non-medical determinants of health.12 Correspondingly, the VHA has been amenable to addressing SDH through development and implementation of universal screens for homelessness13 and military sexual trauma (MST)14 as well as services built around vocational rehabilitation15 and supportive housing.16 These targeted screens and supportive services have resulted in valuable health services and health outcomes studies,17, 18 but there is scarce research to examine a wider array of SDH collected within VHA EHR, their co-occurrence, and how they may explain outcomes that are strongly tied to SDH, such as suicide ideation and attempt. The few extant VHA studies have focused either solely on specific phenomena (e.g., intimate partner violence,19 adverse childhood experiences,20 homelessness21) or have looked at multiple SDH in specific minority populations (e.g., transgender Veterans22).
Although the VHA has the capability to address a variety of SDH, the breadth and frequency of the attention to and documentation of SDH by frontline health care providers within the VHA is largely unknown. Because of the VHA’s adoption of SDH-related screens, large patient population, and priority for suicide prevention,23 it was an ideal setting for the purposes of this study, which were to examine the extent to which documentation of SDH occurred in EHR and how they were associated with records of suicide ideation and of suicide attempt.
METHODS
Sample
We extracted data from the VHA’s Corporate Data Warehouse (CDW), which contains administrative and EHR data.24 Detailed information about the structure and components of the CDW is available from the VA Information Resources Center.25 Data were from all Veteran Integrated Service Network Region 4 (VISN-4) patients with at least 1 inpatient or outpatient visit during the study period of fiscal year (FY) 2016 (October 1, 2015–September 30, 2016), culminating in an analytic sample of 293,872 patients after excluding 41 patients missing data on age. This research focused on VISN-4 because it was supported through a VISN-4 competitive pilot project award.
Key Independent Variables
We categorized seven types of adverse SDH: experience of violence, housing instability, employment or financial problems, legal problems, social or familial problems, lack of access to care or transportation, and non-specific psychosocial needs that were documented during FY2016. Data on SDH came from three primary sources. First, we searched for International Statistical Classification of Diseases and Related Health Problems (ICD)-10 codes indicative of SDH, such as TX74.11 adult physical abuse, Z56.0 unemployment, Z59.0 homelessness, and Z65.1 imprisonment or incarceration. Second, we included any VHA code indicative of receiving services (i.e., stop codes) related to SDH, such as counseling for MST, job rehabilitation services, VHA Homeless Programs, and services for justice-involved Veterans. Third, we used selected standardized fields from a table of Health Factors data in the CDW captured through progress notes authored by master’s prepared social workers, primarily delivering social work services in Patient Aligned Care Team (PACT) settings. These standardized fields included information on “presenting issues” (e.g., abuse, housing instability, or lack of transportation) and “concerns” (e.g., concerns about housing, income, access to care, and social support). Each “concern” field could have an acuity level (1 to 4) assigned: all needs met, minor concern, major concern, or crisis, which we recoded as dichotomy of all needs met vs. minor/major concern or crisis. Although VA’s Health Factors includes various data about numerous patient indicators, there are few standardized fields. For example, to create a smoking status variable from Health Factors data, McGinnis et al. had to review over 3,800 individual Health Factor categories related to tobacco use.26 Reviewing all Health Factors data was beyond the scope of this pilot project, and the use of the social work template presented an existing standardized categorization of SDH-related indicators. Appendix Table 6 presents the ICD-10 codes, VHA stop codes, and VA Health Factors codes.
Table 6.
Prevalence of Social Determinants of Health Noted in Electronic Health Record Among VISN4 Patients (n = 293,872), by Source of Documentation, 2016
| Specific form of documentation | n | (%) |
|---|---|---|
| ICD-10 diagnostic codes | ||
| Legal issues (Z65.0 Conviction in civil and criminal proceedings without imprisonment; Z65.1 Imprisonment and other incarceration, Z65.2 Problems related to release from prison; Z65.3 Problems related to other legal circumstances; Z65.4 Victim of crime and terrorism; Y92.14 Prison as the place of occurrence of the external cause) | 3,109 | (1.1) |
| Nonspecific psychosocial needs (Z65.8 Other specified problems related to psychosocial circumstances and Z65.9 Problem related to unspecified psychosocial circumstances) | 20,145 | (6.9) |
| Exposure to violence, abuse, or maltreatment (O9A.3-5 Abuse complicating pregnancy; T74 Neglect or abandonment, confirmed; T76 Neglect or abandonment, suspected; X92 Assault by drowning and submersion; X93 Assault by handgun discharge; X94 Assault by rifle, shotgun and larger firearm discharge; X95 Assault by other and unspecified firearm and gun discharge; X96 Assault by explosive material; X97 Assault by smoke, fire and flames; X98 Assault by steam, hot vapors and hot objects; X99 Assault by sharp object; Y00 Assault by blunt object; Y01 Assault by pushing from high place; Y02 Assault by pushing or placing victim in front of moving object; Y03 Assault by crashing of motor vehicle; Y04 Assault by bodily force; Y07 Perpetrator of assault, maltreatment and neglect; Y08 Assault by other specified means; Y09 Assault by unspecified means; Y35 Legal intervention injury; Y36 Operations of war; Y37 Military operations; Y38 Terrorism; Z04.4 Encounter for examination and observation following alleged rape; Z04.7 Encounter for examination and observation following alleged physical abuse; Z04.81 Encounter for examination and observation following forced sexual exploitation; Z65.5 Exposure to disaster, war and other hostilities; Z69 Encounter for mental health services for victim and perpetrator of abuse; Z91.4 Personal history of psychological trauma) | 7,572 | (2.6) |
| Employment or financial problems (Z56 Problems related to employment/unemployment; Z59.4 Lack of adequate food and safe drinking water; Z59.5 Extreme poverty; Z59.6 Low income; Z59.7 Insufficient social insurance and welfare support; Z59.8 Other problems related to housing and economic circumstances; Z59.9 Problem related to housing and economic circumstances, unspecified) | 4,744 | (1.6) |
| Housing instability (Z59.0 Homelessness; Z59.1 Inadequate housing) | 13,459 | (4.6) |
| Social environmental problem (Z59.2 Discord with neighbors, lodgers and landlord; Z59.3 Problems related to living in residential institution; Z55 Problems related to education or literacy; Z60 Problems related to social environment) | 1,225 | (0.4) |
| Current or former family problem (Z62 Problems related to upbringing; Z63 Problems in relationship with spouse or partner | 4,325 | (1.5) |
| VHA stop codes | ||
| Work-related services (208/222/568/574 Compensated work therapy; 555 employment services; 535/574 job rehabilitation) | 3,913 | (1.3) |
| Housing-related services (504/511 Grant and per diem; 507/522/530 Department of Housing and Urban Development- Veterans Affairs Supportive Housing [HUD-VASH]; 508/528/529 Health Care for Homeless Veterans; 555/556 Homelessness/job rehabilitation) | 11,395 | (3.9) |
| Legal-related services (591 Incarcerated re-entry; 592 Veterans Justice Outreach) | 2,860 | (1.0) |
| Military sexual trauma-related services (524 Active duty sexual trauma) | 206 | (0.1) |
| VA Health Factors | ||
| Access to care concerns | 2,183 | (0.7) |
| Economic concerns | 3,010 | (1.0) |
| Income source—unemployment benefits | 76 | (.03) |
| Income source—public assistance | 71 | (.02) |
| Housing concerns | 2,162 | (0.7) |
| Living situation—shelter | 98 | (.03) |
| Social support concerns | 2,876 | (1.0) |
| Presenting issue—abuse | 718 | (0.2) |
| Presenting issue—financial | 5,761 | (2.0) |
| Presenting issue—housing | 3,701 | (1.3) |
| Presenting issue—legal | 1,252 | (0.4) |
| Presenting issue—transportation | 3,518 | (1.2) |
| Military sexual trauma screen | 939 | (0.3) |
We summarized adverse SDH as experiencing any one of the several indicators. For example, if a patient had an ICD-10 code indicating violence and a VHA stop code indicating experience of military sexual trauma, the patient was coded as “yes” for having experienced any violence. In addition to coding presence of each category of adverse SDH separately (e.g., “any violence”), we also created a variable of the number of categories of adverse SDH identified (0, 1, 2…7).
Covariates
We extracted data on several covariates, such as socio-demographic information on race, ethnicity, sex, marital status, and age. Because transgender Veterans have high risk for suicide morbidity and mortality and prevalent SDH-related issues (e.g., housing instability),22, 27 we included transgender status using methodology in previous VHA-based research using ICD codes (e.g., gender identity disorder). We included patients’ locale, which was defined by VHA’s Planning Systems Support Group (PSSG) data source that identifies a patient as living in an urban, rural, or highly rural area.28 Patients who had different entries for their locale during the study period or were missing were recoded to a category of “unknown” locales. Lastly, because of their strong relations with suicidal ideation and attempt, we extracted the following diagnoses for patients during the study period: major depressive disorder, alcohol use disorder, drug use disorder, anxiety disorder, posttraumatic stress disorder, schizophrenia, and bipolar disorder.
Dependent Variables
The two key outcomes of suicidal ideation and suicide attempt were coded using two forms of data. First, we used presence of any ICD-10 code for suicidal ideation or for suicide attempt during FY2016. Second, the VHA has a unique registry of patients who have experienced suicidal ideation, attempt, death, or non-suicidal self-harm, known collectively as the Suicide Prevention Applications Network (SPAN) and input by a national network of VA Suicide Prevention Coordinators (see Hoffmire et al.).29 We coded any patient that had either a SPAN record or an ICD code indicating suicidal ideation or attempt during the study period as having the outcomes of interest; patients without either notations during the study period were considered not to have the outcomes of interest. Suicide ideation and attempt are related—but distinct—phenomena,30 and we elected to analyze them separately rather than as a combined outcome.
Analyses
We summarized the frequencies and point prevalence estimates of all socio-demographic characteristics and adverse SDH. We generated a co-prevalence matrix illustrating the co-occurrence between any two adverse SDH; a correlational analysis (i.e., tetrachoric) was not plausible because one could not assume the adverse SDH variables had underlying normally distributed continuous structures. To assess the association of the count of adverse SDH with suicidal ideation and with suicide attempt, we used multiple logistic regression to adjust for socio-demographic and mental disorder diagnoses. We also conducted a series of separate multiple logistic regression analyses to determine the independent association of each adverse SDH with suicidal ideation and with suicide attempt. For multivariable models, we top-coded the count of adverse SDH to > 4 because of the relatively scant frequency of patients in the categories of having indicators of 5, 6, or all 7 adverse SDH. Missing values in socio-demographic variables were recoded to “unknown” to preserve the observations from list-wise deletion in multivariable analyses. Because of the large sample size, statistical significance was assessed at the p < .01 level, and all adjusted odds ratios (aOR) included 99% confidence intervals (CI). All analyses were conducted using Stata/MP Version 15.31 This study was approved by the VA Pittsburgh Healthcare Systemp institutional review board.
RESULTS
Similar to the profile of the general United States Veteran population,32 the VISN-4 patient population primarily comprised men (91.7%), individuals who were White (79.7%), and approximately 70% were aged 60 years or older (Table 1). Just under 1% of patients had an ICD code of suicidal ideation and approximately 0.1% had an ICD code of suicide attempt.
Table 1.
Socio-demographic Characteristics and Prevalence of Suicide Morbidity Among VISN4 Patients (n = 293,872), FY2016
| n | (%) | |
|---|---|---|
| Sex | ||
| Male | 269,562 | (91.7) |
| Female | 24,310 | (8.3) |
| Race | ||
| White | 234,351 | (79.7) |
| Black/African American | 37,941 | (12.9) |
| Other racial identity | 2,669 | (0.9) |
| Unknown | 18,911 | (6.4) |
| Ethnicity | ||
| Non-Hispanic | 288,517 | (98.2) |
| Hispanic | 5,355 | (1.8) |
| Transgender | 107 | (0.04) |
| Marital status | ||
| Married | 160,263 | (54.5) |
| Formerly married | 84,214 | (28.6) |
| Single/never married | 39,054 | (13.3) |
| Unknown | 10,341 | (3.5) |
| Age | ||
| 18–29 | 7,386 | (2.5) |
| 30–39 | 22,275 | (7.6) |
| 40–49 | 20,174 | (6.9) |
| 50–59 | 35,484 | (12.1) |
| 60–69 | 67,532 | (23.0) |
| 70–79 | 75,633 | (25.7) |
| > 80 | 65,356 | (22.2) |
| Locale | ||
| Urban | 186,223 | (63.5) |
| Rural | 88,854 | (30.2) |
| Unknown | 18,795 | (6.4) |
| Mental health disorders | ||
| Alcohol use disorder | 19,959 | (6.8) |
| Drug use disorder | 12,523 | (4.3) |
| Schizophrenia | 3,655 | (1.2) |
| Major depressive disorder | 45,391 | (15.4) |
| Bipolar disorder | 6,843 | (2.3) |
| Posttraumatic stress disorder | 34,051 | (11.6) |
| Anxiety | 25,193 | (8.6) |
| Suicidal ideation | 2,999 | (1.0) |
| Suicide attempt | 1,035 | (0.3) |
Percentages may not sum to 100% due to missing data
Approximately 16.4% of patients had at least one adverse SDH in their EHR during 2016, and over 16,000 patients had > 2 adverse SDH (Table 2). The category of non-specific psychosocial needs was the most prevalent adverse SDH (6.9%), followed by housing instability (6.0%) and employment/financial problems (3.5%). Suicide ideation and attempt were significantly more prevalent among patients with adverse SDH than patients without adverse SDH. In terms of co-occurrence, 57.6% of patients with employment/financial problems also had an indicator of housing instability (Table 3). Among patients with housing instability, over 1/3 had employment/financial issues and over 1/3 had legal problems. Violence had the lowest co-prevalence; of patients who had an indicator of violence, 8.3% also had an indicator of social/familial problems and 8.5% experienced lack of access to care/transportation.
Table 2.
Prevalence and Accumulation of Adverse Social Determinants of Health and Prevalence of Suicidal Ideation and Attempt Within Social Determinant Categories, VISN4 2016
| Overall | Suicidal | Suicide | ||||
|---|---|---|---|---|---|---|
| (n = 293,872) | Ideation* | Attempt* | ||||
| n | (%) | n | (%) | n | (%) | |
| Individual types of adverse social determinants of health | ||||||
| Violence | 9,646 | (3.3) | 494 | (5.1) | 80 | (0.8) |
| Housing instability | 17,738 | (6.0) | 1,493 | (8.4) | 155 | (0.9) |
| Employment/financial | 10,353 | (3.5) | 1,026 | (9.9) | 104 | (1.0) |
| Legal issues | 4,561 | (1.5) | 579 | (12.7) | 68 | (1.5) |
| Social/familial problems | 7,954 | (2.7) | 640 | (8.1) | 84 | (1.1) |
| Lack access to care/transportation | 5,443 | (1.9) | 406 | (7.5) | 41 | (0.7) |
| Non-specific psychosocial needs | 20,145 | (6.9) | 1,155 | (5.7) | 117 | (0.6) |
| Number of types of adverse social determinants of health | ||||||
| 0 | 245,793 | (83.6) | 528 | (0.2) | 86 | (0.03) |
| 1 | 31,717 | (10.8) | 516 | (1.6) | 92 | (0.3) |
| 2 | 9,546 | (3.3) | 521 | (5.5) | 57 | (0.6) |
| 3 | 3,914 | (1.3) | 402 | (10.3) | 40 | (1.0) |
| 4 | 1,722 | (0.6) | 279 | (16.2) | 34 | (2.0) |
| 5 | 777 | (0.3) | 188 | (24.2) | 12 | (1.5) |
| 6 | 305 | (0.1) | 98 | (32.1) | 13 | (4.3) |
| 7 | 98 | (0.03) | 55 | (56.1) | 7 | (7.1) |
*All comparisons are significant at p < .01; comparator for individual types of adverse social determinants is the group of patients without the adverse social determinants
Table 3.
Co-occurrence of Adverse Social Determinants of Health Noted in Electronic Health Record, VISN4 2016
| Violence | Housing instability | Employment/financial | Legal issues | Social/familial problems | Lack access to care/transportation | Nonspecific psychosocial needs | |
|---|---|---|---|---|---|---|---|
| % | % | % | % | % | % | % | |
| Violence (n = 9,646) | – | 19.0 | 13.9 | 9.4 | 8.3 | 8.4 | 16.4 |
| Housing instability (n = 17,738) | 10.3 | – | 33.6 | 17.0 | 17.1 | 15.9 | 28.0 |
| Employment/financial (n = 10,353) | 12.9 | 57.6 | – | 19.2 | 14.8 | 22.2 | 34.6 |
| Legal issues (n = 4,561) | 19.8 | 66.1 | 43.6 | – | 16.1 | 19.1 | 30.2 |
| Social/familial problems (n = 7,954) | 10.1 | 38.2 | 19.2 | 9.2 | – | 23.3 | 30.3 |
| Lack access to care/transportation (n = 5,443) | 14.9 | 51.8 | 42.2 | 16.0 | 34.0 | – | 42.6 |
| Nonspecific psychosocial needs (n = 20,145) | 7.8 | 24.6 | 17.8 | 6.8 | 12.0 | 11.5 | – |
After adjusting for numerous socio-demographic factors and mental disorder diagnoses, adverse SDH showed robust and graded associations with both measures of suicide morbidity (Table 4; Figs. 1 and 2). For example, compared with patients who had no adverse SDH, patients with one adverse SDH had nearly 2.5 the odds of suicidal ideation (aOR = 2.45, 99% CI = 2.07–2.92), two adverse SDH had over four times the odds (aOR = 4.20, 99%CI = 3.49–5.05), three adverse SDH had nearly five times the odds (aOR = 4.95, 99%CI = 4.01–6.13), and > 4 adverse SDH had over 8 times the odds (aOR = 8.60, 99%CI = 7.01–10.54). Likelihood ratio tests comparing nested models with and without the adverse SDH revealed that inclusion of this variable significantly improved model fit for suicidal ideation (χ2 = 871.4, p < .001) and suicide attempt (χ2 = 104.3, p < .001).
Table 4.
Association of the Count of Adverse Social Determinants of Health With Suicide Ideation and Suicide Attempt, VISN-4 FY2016
| Suicidal ideation | Suicide attempt | |||
|---|---|---|---|---|
| (n = 293,831) | (n = 293,831) | |||
| AOR | (99%CI) | AOR | (99%CI) | |
| Age group | ||||
| 18–29 | Ref | Ref | ||
| 30–39 | 0.82 | (0.60–1.11) | 0.87 | (0.47–1.62) |
| 40–49 | 0.81 | (0.59–1.12) | 0.56 | (0.28–1.11) |
| 50–59 | 0.83 | (0.61–1.11) | 0.65 | (0.34–1.23) |
| 60–69 | 0.70* | (0.52–0.95) | 0.41* | (0.21–0.79) |
| 70–79 | 0.58* | (0.41–0.81) | 0.37* | (0.18–0.78) |
| >80 | 0.44* | (0.28–0.70) | 0.15* | (0.04–0.51) |
| Marital status | ||||
| Married | Ref | Ref | ||
| Formerly married | 1.16 | (1.00–1.35) | 1.59* | (1.12–2.28) |
| Single/never married | 1.07 | (0.90–1.27) | 1.03 | (0.67–1.59) |
| Unknown | 0.67 | (0.32–1.43) | 0.76 | (0.11–5.27) |
| Hispanic ethnicity | ||||
| No | Ref | Ref | ||
| Yes | 1.19 | (0.87–1.62) | 0.61 | (0.24–1.58) |
| Race | ||||
| White | Ref | Ref | ||
| Black/African American | 0.94 | (0.81–1.09) | 0.36* | (0.22–0.59) |
| Other racial identity | 0.96 | (0.56–1.64) | 0.81 | (0.24–2.74) |
| Unknown | 1.26 | (0.90–1.78) | 0.55 | (0.18–1.69) |
| Sex | ||||
| Male | Ref | Ref | ||
| Female | 0.74* | (0.61–0.91) | 0.87 | (0.56–1.36) |
| Transgender | ||||
| No | Ref | Ref | ||
| Yes | 1.89 | (0.51–7.03) | 1.94 | (0.13–28.35) |
| Locale | ||||
| Urban | Ref | Ref | ||
| Rural | 0.88 | (0.75–1.03) | 1.72* | (1.23–2.40) |
| Unknown | 1.64* | (1.35–2.00) | 1.84* | (1.19–2.84) |
| Mental health disorders | ||||
| Alcohol use disorder | 2.23* | (1.94–2.56) | 1.98* | (1.40–2.81) |
| Drug use disorder | 2.90* | (2.51–3.35) | 1.36 | (0.93–1.98) |
| Schizophrenia | 4.67* | (3.73–5.85) | 3.12* | (1.79–5.42) |
| Major depressive disorder | 13.69* | (11.32–16.55) | 8.45* | (5.42–13.16) |
| Bipolar disorder | 3.30* | (2.84–3.84) | 2.55* | (1.79–3.63) |
| Posttraumatic stress disorder | 1.89* | (1.67–2.14) | 1.88* | (1.37–2.56) |
| Anxiety | 1.30* | (1.15–1.48) | 1.40* | (1.03–1.91) |
| Number of social determinant of health indicators | ||||
| 0 | Ref | Ref | ||
| 1 | 2.45* | (2.07–2.92) | 3.29* | (2.20–4.93) |
| 2 | 4.20* | (3.49–5.05) | 3.68* | (2.27–5.95) |
| 3 | 4.95* | (4.01–6.13) | 3.71* | (2.11–6.53) |
| >4 | 8.60* | (7.01–10.54) | 6.19* | (3.68–10.44) |
*p < .01
Figure 1.
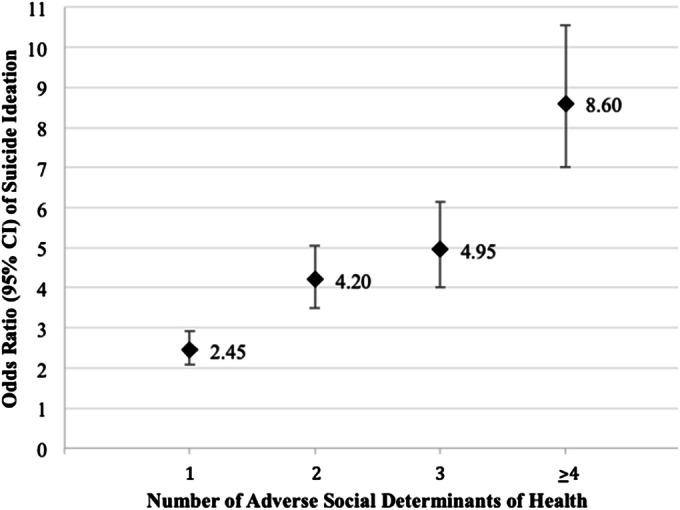
Associations of the count of adverse social determinants of health with suicidal ideation. All odds ratios are adjusted for age group, marital status, race, ethnicity, sex, transgender status, locale, alcohol abuse disorder, drug use disorders, schizophrenia, major depressive disorder, bipolar disorder, posttraumatic stress disorder, and anxiety disorder.
Figure 2.
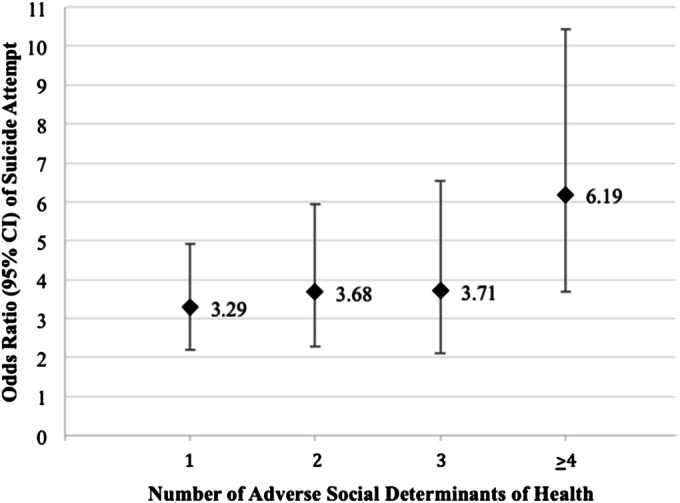
Associations of the count of adverse social determinants of health with suicide attempt. All odds ratios are adjusted for age group, marital status, race, ethnicity, sex, transgender status, locale, alcohol abuse disorder, drug use disorders, schizophrenia, major depressive disorder, bipolar disorder, posttraumatic stress disorder, and anxiety disorder.
Post hoc tests for trend of SDH showed a significant linear relation for suicidal ideation (AOR = 1.67, 99%CI = 1.60–1.75) and suicide attempt (AOR = 1.49, 99%CI = 1.33–1.68) (data not shown). For example, for each unit increase in the number of SDH identified, the odds of suicidal ideation increased by 67%. Diagnostics indicated low collinearity (mean variance inflation factor = 2.3). Multivariate outliers did not affect estimates of the model for suicidal ideation, but estimates for the model for suicide attempt may be sensitive to 1,996 observations indicated as potential outliers (i.e., standardized residuals > 3). Estimates in the model of suicide attempt should be interpreted with caution. Individual adverse SDH had significant independent associations with suicide morbidity after adjusting for covariates (Table 5).
Table 5.
Independent associations of individual adverse social determinants of health with suicide ideation and suicide attempt, VISN-4 FY2016
| Type of adverse social determinant of health | Suicidal ideation | Suicide attempt | ||
|---|---|---|---|---|
| AOR | (99%CI) | AOR | (99%CI) | |
| Violence | 2.26* | (1.91–2.67) | 2.90* | (2.03–4.16) |
| Housing instability | 3.09* | (2.71–3.53) | 2.18* | (1.53–3.09) |
| Employment/financial | 2.28* | (1.99–2.62) | 1.58* | (1.10–2.27) |
| Legal issues | 1.86* | (1.58–2.19) | 1.57* | (1.05–2.36) |
| Social/familial problems | 2.37* | (2.05–2.75) | 2.31* | (1.63–3.29) |
| Lack access to care/transportation | 2.26* | (1.88–2.71) | 1.71* | (1.07–2.72) |
| Non-specific psychosocial needs | 3.10* | (2.74–3.50) | 1.86* | (1.35–2.57) |
Models adjusted for age group, marital status, race, ethnicity, sex, transgender status, locale, alcohol abuse disorder, drug use disorders, schizophrenia, major depressive disorder, bipolar disorder, posttraumatic stress, disorder, and anxiety disorder
*p < .01
DISCUSSION
To our knowledge, this is one of the largest epidemiologic studies of adverse SDH using EHR data in the USA. Consistent with prior survey research, adverse SDH identified via EHR were robustly associated with suicide morbidity.2–5 However, in novel and important findings, adverse SDH—both in individual analyses and as a count—remained associated with suicide morbidity even after adjusting for mental health diagnoses that strongly predict suicide morbidity. Moreover, many of the effect sizes for SDH were medium-to-large33 and stronger than some mental health diagnoses.
The results underscore that adverse SDH are as relevant as medical factors (e.g., depression) for suicide prevention and treatment. Suicide is an insidiously complex phenomenon due to its dynamic etiology. For example, although most people who die by suicide likely had some mental illness (regardless of formal diagnosis), the majority of people living with mental illness do not attempt to kill themselves.34 The lack of specificity around mental illness to adequately predict suicide ultimately has called into question its utility as a meaningful—typically requisite—predictor for suicide research.35 In a health care system, the emphasis on mental illness may create a myopia on biological conditions, which then orients toward biomedical treatments (e.g., pharmacotherapies). For instance, despite increasing prescriptions of antidepressants in the USA since 1999,36 the rate of suicide has not decreased over that same time period.37 Seemingly obscured are important social factors associated with suicidal crisis such as relationship failure, legal problems, and financial stressors, which often require more intensive, coordinated case management. However, best practices for health care systems to collect SDH data (e.g., conducting self-report surveys vs. provider-administered conversations, determining which SDH to prioritize) are largely unknown.38 Furthermore, it is unclear which clinical strategies could be employed to address adverse SDH as part of a comprehensive approach to suicide prevention. Consequently, research is necessary to determine how health care systems can better create or refer patients to services equipped to assist with SDH needs of patients in addition to medical treatment for mental illness.
Because social workers are best trained and positioned to address social factors that impact health, the role of social work in health care may be a key avenue of future research and quality improvement initiatives that integrate community and social services into “traditional” health care delivery for patients who experience suicidal crisis. In the VHA, social workers provide care as a member of the patient-aligned care team (PACT, VHA’s patient-centered medical home); however, there are shortages of social workers in the VHA system, despite being directly involved in suicide prevention.39 Demand for the social work profession in health care is projected to grow faster than other occupations in the next decade.40 Full deployment of the Social Work Case Management Model in PACT and utilization of standardized documentation of social work interventions in treating at-risk patients, with other mental and behavioral health professionals, could be a key strategy for suicide prevention. Increasing access to master’s level social workers will assist with proactively addressing patients’ SDH (e.g., social workers conduct assessments of patients upon initial contact and through ongoing monitoring of the treatment plan). Furthermore, social work integration fully into PACT environments underscores the unique contribution of SDH on disease and treatment, including suicide. If providers are not documenting these contributions, then social workers who are trained to identify and mitigate the risks of SDH can assist in the documentation of these determinants.
We note several limitations. First, causality between adverse SDH and suicide morbidity could not be assessed because of the observational study design. A strength of this study was VHA’s implementation of direct clinical screens for housing instability and for military sexual trauma, which is likely to increase the ability to get patients’ self-report of SDH. However, reliance on ICD coding indicative of adverse SDH likely underestimated the phenomena. Moreover, ICD coding is generally used for billing purposes; however, the VHA system is federally subsidized, so it is unknown how the use of ICD codes in VHA may differ from non-federal health care systems’ use of ICD codes. Additionally, our search for adverse SDH may have excluded relevant coding (e.g., general social work consults) or experiences that were noted outside of our study period, so our seven categories of adverse SDH were not exhaustive. Our reliance on the standardized social work template in VA’s Health Factors data table, though likely highly valid for indicating adverse SDH, did not include SDH that could have been input by other providers (e.g., primary care physicians). Additionally, we were unable to capture other potentially relevant SDH, such as patients’ income or aspects of patients’ built environment (e.g., environmental exposures). Because the VHA population differs systematically from the general US population, the results may not generalize to other patient populations. The focus on one geographic region (i.e., VISN4 includes most of Pennsylvania, all of Delaware, and small portions of West Virginia, Ohio, New York, and New Jersey) further limits generalizability. Finally, it is unknown whether providers have inattention to SDH or have difficulty in documenting them.
CONCLUSIONS
Because SDH are germane for nearly all health outcomes, they likely impact other medical conditions and health care metrics (e.g., patient compliance, missed appointments, utilization patterns). Additionally, asking patients about SDH behooves health care systems to offer services, resources, or referrals to the patients. Questions remain about how best to collect data about SDH from patients, and until best practices are promulgated, health services researchers may be able to use existing methods outlined in this report. However, avenues of future research include understanding the context of existing SDH documentation, including where documentation occurs (e.g., facility-level effects) and who inputs documentation (e.g., provider-level effects). There is also a need for further research to investigate whether interventions that address patients’ adverse SDH may have concomitant benefits of preventing suicide; for example, permanent supportive housing manages an immediate problem of homelessness, but it also may have managed a patient’s thoughts of suicide. Lastly, adverse SDH are complex problems that require complex solutions, and best practice models of how health care systems partner with community agencies are largely uncharted and the nuances of those partnerships unexplored (e.g., interagency data sharing to enrich health services research).
Acknowledgments
The authors thank John Cashy, PhD, for his assistance in data management, Ada Youk, PhD, for her assistance in analysis, and Tayler Boyer, MPH, for their assistance in creating the figures.
Appendix
Funders
This work was supported by a VISN-4 pilot award to JRB. This work was also partially supported by a VA Health Services Research and Development (HSR&D) Career Development Award to JRB (CDA-14-408) and a VA HSR&D Merit Award to AEM (IIR-13-334).
Compliance with Ethical Standards
Conflict of Interest
The authors declare that they do not have a conflict of interest.
Disclaimer
The views or opinions expressed in this work are those of the authors and do not necessarily reflect those of the funders, institutions, the Department of Veterans Affairs, or The United States Government.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Braveman P, Egerter S, Williams DR. The social determinants of health: coming of age. Annual review of public health. 2011;32:381–398. doi: 10.1146/annurev-publhealth-031210-101218. [DOI] [PubMed] [Google Scholar]
- 2.King CA, Merchant CR. Social and interpersonal factors relating to adolescent suicidality: A review of the literature. Archives of Suicide Research. 2008;12(3):181–196. doi: 10.1080/13811110802101203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kposowa AJ. Unemployment and suicide: a cohort analysis of social factors predicting suicide in the US National Longitudinal Mortality Study. Psychological medicine. 2001;31(01):127–138. doi: 10.1017/S0033291799002925. [DOI] [PubMed] [Google Scholar]
- 4.Nock MK, Borges G, Bromet EJ, Cha CB, Kessler RC, Lee S. Suicide and suicidal behavior. Epidemiologic reviews. 2008;30(1):133–154. doi: 10.1093/epirev/mxn002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Dube SR, Anda RF, Felitti VJ, Chapman DP, Williamson DF, Giles WH. Childhood abuse, household dysfunction, and the risk of attempted suicide throughout the life span: findings from the Adverse Childhood Experiences Study. Jama. 2001;286(24):3089–3096. doi: 10.1001/jama.286.24.3089. [DOI] [PubMed] [Google Scholar]
- 6.Gottlieb L, Sandel M, Adler NE. Collecting and applying data on social determinants of health in health care settings. JAMA internal medicine. 2013;173(11):1017–1020. doi: 10.1001/jamainternmed.2013.560. [DOI] [PubMed] [Google Scholar]
- 7.Institute of Medicine. Capturing social and behavioral domains in electronic health records. Washington, DC2014. [PubMed]
- 8.Marmot MG, Stansfeld S, Patel C, et al. Health inequalities among British civil servants: the Whitehall II study. The Lancet. 1991;337(8754):1387–1393. doi: 10.1016/0140-6736(91)93068-K. [DOI] [PubMed] [Google Scholar]
- 9.Pappas G, Queen S, Hadden W, Fisher G. The increasing disparity in mortality between socioeconomic groups in the United States, 1960 and 1986. New England journal of medicine. 1993;329(2):103–109. doi: 10.1056/NEJM199307083290207. [DOI] [PubMed] [Google Scholar]
- 10.Taylor LA, Tan AX, Coyle CE, et al. Leveraging the social determinants of health: What works? PLOS-ONE. 2016;11(8):e0160217. doi: 10.1371/journal.pone.0160217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.U.S. Department of Veterans Affairs, National Center for Veterans Analysis and Statistics. VA utilization profile FY2016. 2017; https://www.va.gov/vetdata/docs/QuickFacts/VA_Utilization_Profile.PDF. Accessed February 5, 2019.
- 12.U.S. Department of Veterans Affairs. Department of Veterans Affairs FY2018-2024 Strategic Plan. Washington, DC2018.
- 13.Montgomery AE, Fargo JD, Byrne TH, Kane VR, Culhane DP. Universal Screening for Homelessness and Risk for Homelessness in the Veterans Health Administration. Am J Public Health. 2013;103(S2):S210–S211. doi: 10.2105/AJPH.2013.301398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kimerling R, Gima K, Smith MW, Street A, Frayne S. The Veterans Health Administration and military sexual trauma. American Journal of Public Health. 2007;97(12):2160–2166. doi: 10.2105/AJPH.2006.092999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Rosenheck RA. Posttraumatic stress disorder and employment in veterans participating in Veterans Health Administration Compensated Work Therapy. Journal of rehabilitation research and development. 2008;45(3):427. doi: 10.1682/JRRD.2007.06.0093. [DOI] [PubMed] [Google Scholar]
- 16.Gabrielian S, Yuan AH, Andersen RM, Rubenstein LV, Gelberg L. VA Health Service Utilization for Homeless and Low-income Veterans: A Spotlight on the VA Supportive Housing (VASH) Program in Greater Los Angeles. Medical care. 2015;52(5):454–461. doi: 10.1097/MLR.0000000000000112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Davis LL, Kyriakides TC, Suris AM, et al. Effect of evidence-based supported employment vs transitional work on achieving steady work among veterans with posttraumatic stress disorder: a randomized clinical trial. JAMA psychiatry. 2018;75(4):316–324. doi: 10.1001/jamapsychiatry.2017.4472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Montgomery AE, Dichter ME, Thomasson AM, Roberts CB. Services receipt following Veteran outpatients’ positive screen for homelessness. American journal of preventive medicine. 2016;50(3):336–343. doi: 10.1016/j.amepre.2015.06.035. [DOI] [PubMed] [Google Scholar]
- 19.Dichter ME, True G, Marcus SC, Gerlock AA, Yano EM. Documentation of intimate partner violence in women veterans' medical records: An in-depth analysis. Military Behavioral Health. 2013;1(2):114–120. doi: 10.1080/21635781.2013.830063. [DOI] [Google Scholar]
- 20.Hammond KW, Ben-Ari AY, Laundry RJ, Boyko EJ, Samore MH. The Feasibility of Using Large-Scale Text Mining to Detect Adverse Childhood Experiences in a VA-Treated Population. Journal of traumatic stress. 2015;28(6):505–514. doi: 10.1002/jts.22058. [DOI] [PubMed] [Google Scholar]
- 21.Gundlapalli AV, Carter ME, Palmer M, et al. Using natural language processing on the free text of clinical documents to screen for evidence of homelessness among US veterans. Paper presented at: AMIA Annual Symposium Proceedings2013. [PMC free article] [PubMed]
- 22.Blosnich JR, Marsiglio MC. Dichter ME, et al. American Journal of Preventive Medicine: Impact of Social Determinants of Health on Medical Conditions Among Transgender Veterans; 2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.U.S. Department of Veterans Affairs. National strategy for preventing veteran suicide 2018-2028. 2018; https://www.mentalhealth.va.gov/suicide_prevention/docs/Office-of-Mental-Health-and-Suicide-Prevention-National-Strategy-for-Preventing-Veterans-Suicide.pdf. Accessed January 20, 2019.
- 24.Fihn SD, Francis J, Clancy C, et al. Insights from advanced analytics at the Veterans Health Administration. Health Affairs. 2014;33(7):1203–1211. doi: 10.1377/hlthaff.2014.0054. [DOI] [PubMed] [Google Scholar]
- 25.Souden M. Overview of VA data, information systems, national databases and research uses. 2017. [Google Scholar]
- 26.McGinnis KA, Brandt CA, Skanderson M, et al. Validating smoking data from the Veteran’s Affairs Health Factors dataset, an electronic data source. Nicotine & Tobacco Research. 2011;13(12):1233–1239. doi: 10.1093/ntr/ntr206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Blosnich JR, Brown GR, Shipherd P, Jillian C, Kauth M, Piegari RI, Bossarte RM. Prevalence of gender identity disorder and suicide risk among transgender veterans utilizing Veterans Health Administration care. American Journal of Public Health. 2013;103(10):e27–e32. doi: 10.2105/AJPH.2013.301507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.West AN, Lee RE, Shambaugh-Miller MD, et al. Defining “rural” for veterans’ health care planning. The Journal of Rural Health. 2010;26(4):301–309. doi: 10.1111/j.1748-0361.2010.00298.x. [DOI] [PubMed] [Google Scholar]
- 29.Hoffmire C, Stephens B, Morley S. al. e. VA Suicide Prevention Applications Network: A National Health Care System–Based Suicide Event Tracking System. Public Health Rep. 2016;131(6):816–821. doi: 10.1177/0033354916670133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Crosby AE, Ortega L, Melanson C. Self-directed violence surveillance: Uniform definitions and recommended data elements, Version 1.0. Atlanta, GA: Centers for Disease Control and Prevention,National Center for Injury Prevention and Control;2011.
- 31.Stata Statistical Software: Release 15 [computer program]. College Station, TX: StataCorp LLC; 2017.
- 32.U.S. Department of Veterans Affairs, National Center for Veterans Analysis and Statistics. Profile of Veterans: 2016, data from the American Community Survey. 2018; https://www.va.gov/vetdata/docs/SpecialReports/Profile_of_Veterans_2016.pdf. Accessed February 5, 2019.
- 33.Chen H, Cohen P, Chen S. How big is a big odds ratio? Interpreting the magnitudes of odds ratios in epidemiological studies. Communications in Statistics—Simulation and Computation®. 2010;39(4):860–864. doi: 10.1080/03610911003650383. [DOI] [Google Scholar]
- 34.Brown GK, Beck AT, Steer RA, Grisham JR. Risk factors for suicide in psychiatric outpatients: a 20-year prospective study. Journal of consulting and clinical psychology. 2000;68(3):371. doi: 10.1037/0022-006X.68.3.371. [DOI] [PubMed] [Google Scholar]
- 35.Nock MK, Ramirez F, Rankin O. Advancing our understanding of the who, when, and why of suicide risk. JAMA psychiatry. 2019;76(1):11–12. doi: 10.1001/jamapsychiatry.2018.3164. [DOI] [PubMed] [Google Scholar]
- 36.Pratt LA, Brody DJ, Gu Q. Antidepressant use among persons aged 12 and over: United States, 2011-2014. NCHS data brief, no. 283. Hyattsville, MD: National Center for Health Statistics;2017. [PubMed]
- 37.Curtin SC, Warner M, Hedegaard H. Increase in suicide in the United States, 1999-2014. NCHA data brief, no. 241. Hyattsville, MD2016. [PubMed]
- 38.Gottlieb L, Tirozzi KJ, Manchanda R, Burns AR, Sandel MT. Moving electronic medical records upstread: Incorporating social determinants of health. American journal of preventive medicine. 2015;48(2):215–218. doi: 10.1016/j.amepre.2014.07.009. [DOI] [PubMed] [Google Scholar]
- 39.National Academies of Sciences E, and Medicine,. Evaluation of the Department of Veterans Affairs Mental Health Services. Washington, DC: The National Academies Press;2018. [PubMed]
- 40.Bureau of Labor Statistics, U.S. Department of Labor. Occupational outlook handbood, social workers. 2019; https://www.bls.gov/ooh/community-and-social-service/social-workers.htm. Accessed February 18, 2019.


