Abstract
Background
More than half of homeless adults are of age ≥ 50 years. Falls are a common cause of morbidity in older adults in the general population. Risk factors for falls in the general population include poor health, alcohol use, and exposure to unsafe environments. Homeless adults aged ≥ 50 have a high prevalence of known risk factors and face additional potential risks.
Objectives
To examine the prevalence of and risk of falling in a cohort of older homeless adults.
Design
Longitudinal cohort study with participant interviews every 6 months for 3 years; data were analyzed using generalized estimating equations (GEEs).
Participants
Three hundred fifty adults aged ≥ 50, homeless at study entry, recruited via population-based sampling.
Measures
The dependent variable is any falls in prior 6 months; independent variables include individual (i.e., illness, behaviors) and social/environmental (i.e., social support, experiencing violence, living unsheltered) factors.
Results
Over three quarters of participants were men (77.1%) and Black (79.7%). The median age was 58 (IQR 54, 61). At baseline, one third (33.7%) reported a fall in the prior 6 months. At follow-up visits, 23.1% to 31.2% of participants reported having fallen. In GEE models, individual risk factors (non-Black race, being a women, older age, functional impairment, urinary incontinence, history of stroke, and use of assistive devices, opioid, and marijuana) were associated with increased odds of falls. Environmental and social factors (spending any nights unsheltered (adjusted odds ratio (AOR) = 1.42, CI = 1.10–1.83) and experiencing physical assault (AOR = 1.67, CI = 1.18–2.37) were also associated.
Conclusions
Older homeless adults fall frequently. Likely contributors include having a high prevalence of conditions that increase the risk of falls, compounded by heightened exposure to unsafe environments. Fall prevention in this population should target those at highest risk and address modifiable environmental conditions. Providing shelter or housing and addressing substance use could reduce morbidity from falls in homeless older adults.
KEY WORDS: homelessness, vulnerable populations, falls
INTRODUCTION
In the USA, over half a million people experience homelessness each night 1. The proportion of single homeless adults over age 50 is increasing 1. Homeless adults aged 50 and over experience a higher prevalence of geriatric conditions (e.g., falls, urinary incontinence, and functional, sensory, and cognitive impairments) than adults 20 years older in the general population 2, 3.
In the general population, falls are prevalent, occurring in approximately one third of adults aged 65 or older 4, 5. Falls are associated with adverse outcomes including restricted mobility, deconditioning, and loss of independence 6, 7. In the USA, medical costs due to fatal and non-fatal falls are approximately $50 billion a year 5. Individual risk factors for falls include medical problems (e.g., stroke, depression, functional and cognitive impairment), health-related behaviors (e.g., tobacco or alcohol use) 8–11, and social factors (e.g., lack of social support). Environmental triggers are factors external to the individual that heighten the risk of slipping or tripping. These include surface- (e.g., uneven exteriors, obstructive ground-level objects), ambient- (e.g., poor lighting), and weather-related conditions 12, 13.
Falls result from an interaction between an individual’s underlying vulnerabilities and their exposure to environmental conditions 8, 14. People experiencing homelessness have a high prevalence of factors known to be associated with falls in the general population, including chronic diseases, functional impairment, and alcohol and opioid use problems 2, 15. Homeless older adults have a high prevalence of other factors that could be associated with falls, such as substance use and heightened exposure to physical violence 15, 16.
People who are homeless live in a variety of environments, including homeless shelters and unsheltered spaces that expose them to environmental hazards and violence. In each of these settings, homeless individuals have limited control over their environment, especially when living in unsheltered environments.
We examined the prevalence of and risk factors for falls in a longitudinal cohort of adults aged 50 and older who were homeless at study entry. We hypothesized that homeless adults would have a high prevalence of falls and high exposure to environmental hazards. We hypothesized that factors known to be associated with falls in the general population would be associated with falls in our cohort. We further hypothesized that several factors that are plausibly related, but have not been studied (use of marijuana and stimulants, exposure to physical assault, and uncontrolled environments), would be associated.
METHODS
Study Overview
We conducted a 3-year prospective cohort study of 350 homeless adults aged 50 and older, the Health Outcomes in People Experiencing Homelessness in Older Middle agE (HOPE HOME) study 17. We interviewed participants at baseline and every 6 months for 3 years; at each interview, trained research staff administered a structured interview and conducted clinical assessments. The institutional review board of the University of California, San Francisco approved this study. The datasets we analyzed during the current study are available from the corresponding author on request.
Study Sample
Between July 2013 and June 2014, we recruited 350 adults aged 50 or older who were homeless at study entry. We recruited from all local shelters open to older adults (n = 5), all free and low-cost meal programs that served at least three meals a week (n = 5), one recycling center, and areas where adults slept unsheltered in Oakland, California (Fig. 1). To create a sample that best represented the target population, including the high number of people living unsheltered in Oakland, we randomly selected potential participants using sampling frames that included encampment sites, recycling centers, shelters, and meal programs 18. We describe our methods in more detail elsewhere 17–19.]-->
Fig. 1.
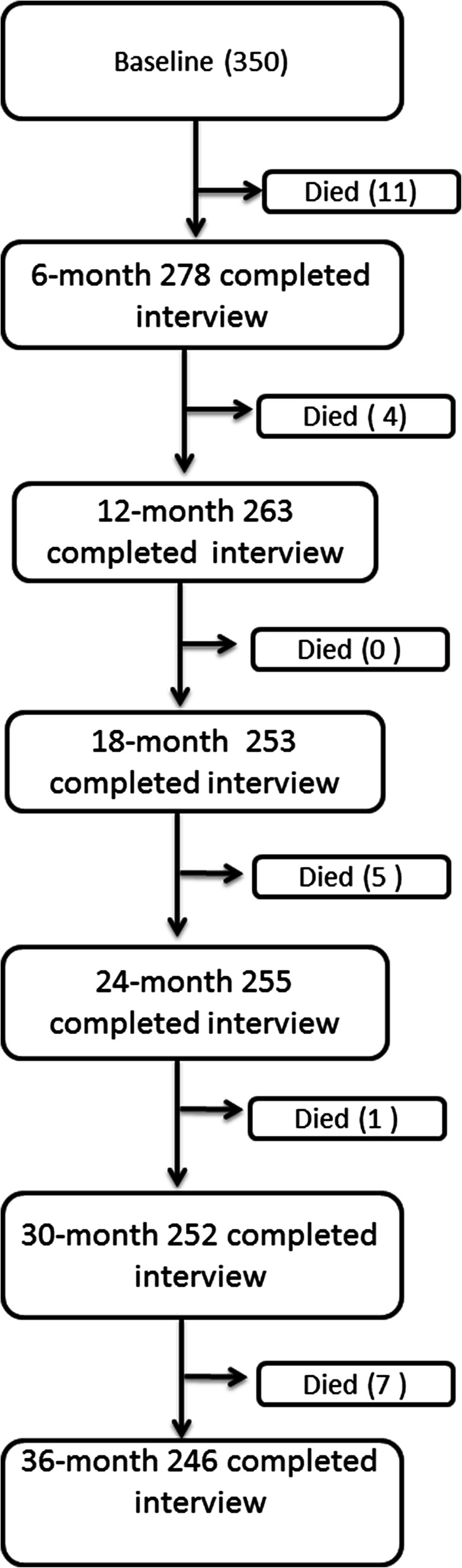
HOPE HOME sample recruitment and follow-up sample sizes. The number of individuals enrolled at baseline and followed at 6-month intervals over the 36-month follow-up is shown. Deaths between each follow-up are noted.
Eligibility criteria included the following: (1) homeless according to the Homeless Emergency Assistance and Rapid Transition to Housing (HEARTH) Act definition that includes any person living unsheltered, staying in an emergency shelter, or facing eviction in the next 14 days; (2) age of 50 years or older; (3) English-speaking; and (4) able to provide informed consent as determined by a teach-back mechanism 20. Participants received $25 for the screening and enrollment interview, $5 for monthly check-ins, and $15 for follow-up interviews.
Measures
Outcome Variable
Our primary outcome was self-reported falls in the prior 6 months, assessed at each study interview. We defined falling as “a sudden, unintentional change in position from an upright posture coming to rest on the floor or ground.” For descriptive purposes, among participants who reported a fall, we asked how many times the participant fell and whether they sought medical treatment for their fall.
Independent Variables
Individual Risk Factors
We identified demographic risk factors as time-constant (assessed once at baseline) and other risk factors, health status, and health-related behaviors as time-varying (assessed at each visit).
We assessed age, gender, and race/ethnicity 21. In our analyses, we dichotomized race as Black versus non-Black. Participants reported their highest educational attainment. We classified participants as having graduated from high school or earned a General Educational Development (GED) certificate versus no high school diploma/GED.
Health Status
Using modified questions from the National Health and Nutrition Examination Survey (NHANES), we asked participants whether a healthcare provider told them they had myocardial infarction, congestive heart failure, stroke, arthritis, diabetes, or chronic lung disease (chronic obstructive pulmonary disease or asthma); we included these as separate variables 22. If a participant reported a medical condition at any time point, we considered them to have that condition in subsequent visits.
We assessed visual impairment using the Snellen test and defined visual impairment as corrected visual acuity < 20/100 23. We defined hearing impairment as self-reported difficulty hearing 24. To evaluate cognitive impairment, we used the Modified Mini-Mental State Examination (3MS). Those who scored below the 7th percentile (1.5 standard deviations below a reference cohort mean) or were unable to complete the assessment were defined as cognitively impaired 25.
We asked participants about their ability to complete activities of daily living (ADLs). We defined an ADL impairment as reporting difficulty with bathing, transferring, toileting, dressing, or eating 26. We assessed lower extremity function with the Short Physical Performance Battery (SPPB) test and classified those who scored ≤ 10 as having reduced physical performance 27. We assessed urinary incontinence in the past 6 months by asking participants whether they had “leaked urine, even a small amount.” 28
We measured height and weight and calculated body mass index (BMI), classifying a BMI ≥ 18 to < 25 as normal weight, 25 to < 30 as overweight, and ≥ 30 as obese. We used the Center for Epidemiologic Studies Depression Scale (CES-D) to assess depressive symptoms; we considered scores ≥ 22 as indicating depressive symptoms 29. We assessed pain by asking participants to score their average pain in the past week using a 10-point Likert scale. We categorized pain as mild (0–4), moderate (5–7), and severe (8–10) 30. We assessed whether participants used an assistive device—such as a cane, crutches, walker, wheelchair, or scooter—in the past 6 months.
Health-Related Behaviors
We classified smoking status using the California Tobacco Survey, categorizing participants as never, current, or former smokers 31. We asked participants to report how much alcohol they drank and considered those who drank ≥ 6 drinks on one occasion monthly as heavy drinkers 32. To assess illicit drug use (cocaine, amphetamines, opioids, and marijuana) in the last 6 months, we used the World Health Organization (WHO)’s Alcohol, Smoking and Substance Involvement Screening Test (ASSIST). We considered a score of ≥ 4 as indicative of moderate-to-severe use 33.
Social and Environmental Risk Factors
Social Support
We used a validated measure of social support, counting the number of people in whom the participant could confide (0, 1–5, or ≥ 6) 34–36.
Physical Assault
To assess physical assault, we asked participants: “in the past six months, have you experienced physical violence by another person using an object like a gun or a knife, or did anyone ever slap, hit, punch, kick, choke, or burn you?” 37
Residential Status
To assess exposure to environmental hazards at each visit, we used a residential follow-back calendar in which we asked participants to report each place they had stayed and the number of nights in each setting during the prior 6 months 38. We considered being unsheltered as indicative of the highest environmental exposure. We defined an unsheltered environment as sleeping outdoors or any place not meant for human habitation (e.g., transit terminal, abandoned building). We categorized participants as having spent any nights versus no nights in unsheltered settings 16. In preliminary analyses, we evaluated nights unsheltered as a 3-level variable (0, 1–119, and 12–180 nights) and as a 6-level variable (0, 1–7, 8–30, 31–90, 91–120, and 121–180 nights). Neither alternative exhibited a dose-response effect. Therefore, we used a dichotomous measure of any nights unsheltered in our analysis.
Statistical Analyses
To identify risk factors for falls, we chose independent variables based on our hypotheses. We assessed bivariate associations between a priori independent variables and recent falls (i.e., one or more falls in the past 6 months) using generalized estimating equations (GEEs).
We built our multivariable model by including variables with bivariate type 1 p values < 0.20. If a categorical variable had more than two levels, we included all levels in our multivariable model if any type 1 p value was < 0.20. We reduced the model using backward elimination retaining variables with p values < 0.05 in our final multivariable model. We conducted our analysis in SAS 9.4 using complete case analysis and robust confidence intervals (SAS Institute Inc., Cary, NC, USA, 2017).
In a sensitivity analysis, we assessed whether we had underestimated the probability of falls due to incomplete follow-up or mortality. We examined the prevalence of falls among those (1) with complete follow-up, (2) who had died during follow-up, or (3) who had not died but had missed any study visits over the 36-month study period. We used GEE to examine whether those who had died or missed visits were more likely to have experienced a fall in the past 6 months than those with complete follow-up.
We included participants with a minimum of two visits. We used weighted linear regression with a second-order polynomial and zero intercept term to plot a trend line.
RESULTS
Participant Characteristics at Baseline
The median age was 58.0 (IQR 54.0, 61.0). Of the 350 participants, the majority were men (77.1%) and Black (79.7%). More than a quarter had less than a high school education (25.7%; Table 1). Over one quarter was obese (26.6%). The majority of participants reported current tobacco use (65.4%), and 11.2% reported heavy drinking. Almost one fifth was cognitively impaired (18.3%). The most prevalent substances with problematic use were cocaine (43.1%), marijuana (39.1%), and opioids (12.9%). Approximately one third of the cohort (32.5%) reported not having any confidants; 10.1% experienced physical assault, and 81.7% had spent a night unsheltered.
Table 1.
Characteristics of Homeless Adults Aged 50 and Older With and Without Falls in the Past 6 Months at Baseline Interview (N = 350)
| Characteristics | Total (N = 350) | Experienced falls in past 6 months (N = 118) | No falls in past 6 months (N = 232) | p values |
|---|---|---|---|---|
| Individual risk factors | ||||
| Age (years), median (interquartile range) | 58.0 (54.0, 61.0) | 58.0 (54.0, 62.0) | 57.5 (54.0, 61.0) | 0.57 |
| Men, N (%) | 270 (77.1) | 87 (73.7) | 183 (78.9) | 0.28 |
| Race/ethnicity, N (%) | ||||
| Black | 279 (79.7) | 86 (72.9) | 193 (83.2) | 0.11 |
| White | 38 (10.9) | 18 (15.3) | 20 (8.6) | |
| Hispanic | 16 (4.6) | 8 (6.8) | 8 (3.4) | |
| Other | 17 (4.9) | 6 (5.1) | 11 (4.7) | |
| Less than high school diploma/General Education Development (GED), N (%) | 90 (25.7) | 37 (31.4) | 53 (22.8) | 0.09 |
| Health status | ||||
| Myocardial infarction | 32 (9.1) | 15 (12.7) | 17 (7.3) | 0.10 |
| Congestive heart failure | 25 (7.1) | 8 (6.8) | 17 (7.3) | 0.85 |
| Stroke | 39 (11.2) | 25 (21.4) | 14 (6.0) | < 0.0001 |
| Arthritis | 156 (44.6) | 59 (50.0) | 97 (41.8) | 0.15 |
| Diabetes | 50 (14.3) | 18 (15.3) | 32 (13.9) | 0.72 |
| Chronic lung disease | 94 (26.9) | 39 (33.1) | 55 (23.7) | 0.06 |
| Visual impairment* | 53 (15.9) | 19 (17.1) | 34 (15.2) | 0.66 |
| Hearing impairment | 124 (35.6) | 49 (41.9) | 75 (32.5) | 0.08 |
| Cognitive impairment (3MS)† | 64 (18.3) | 20 (17.1) | 44 (19.0) | 0.67 |
| ≥ 1 ADL impairments | 136 (38.9) | 66 (55.9) | 70 (30.2) | < 0.0001 |
| Physical performance (SPPB test score ≤ 10) | 201 (58.4) | 84 (73.0) | 117 (51.1) | < 0.0001 |
| Urinary incontinence | 167 (48.0) | 71 (61.2) | 96 (41.4) | 0.0005 |
| Body mass index, N (%) | ||||
| < 25 | 149 (43.6) | 52 (47.3) | 97 (41.8) | 0.56 |
| 25 to < 30 | 102 (29.8) | 29 (26.4) | 73 (31.5) | |
| ≥ 30 | 91 (26.6) | 29 (26.4) | 62 (26.7) | |
| Depressive symptoms; CES-D score ≥ 22, N (%) | 133 (38.3) | 55 (46.6) | 78 (34.1) | 0.02 |
| Pain severity | ||||
| Mild | 151 (43.4) | 43 (36.8) | 108 (46.8) | 0.11 |
| Moderate | 60 (17.2) | 19 (16.2) | 41 (17.7) | |
| Severe | 137 (39.4) | 55 (47.0) | 82 (35.5) | |
| Assistive device | 102 (29.1) | 50 (42.4) | 52 (22.4) | 0.0001 |
| Health-related behaviors | ||||
| Smoking status, N (%) | ||||
| Non-smoker | 78 (22.3) | 59 (25.4) | 19 (16.1) | 0.10 |
| Current smoker | 229 (65.4) | 148 (63.8) | 81 (68.6) | |
| Former smoker | 43 (12.3) | 25 (10.8) | 18 (15.3) | |
| Heavy drinking‡ | 39 (11.2) | 13 (11.1) | 26 (11.3) | 0.97 |
| Cocaine§ | 151 (43.1) | 57 (48.3) | 94 (40.5) | 0.16 |
| Amphetamines | 28 (8.0) | 10 (8.5) | 18 (7.8) | 0.82 |
| Opioids | 45 (12.9) | 22 (18.6) | 23 (9.9) | 0.02 |
| Marijuana | 137 (39.1) | 58 (49.2) | 79 (34.1) | 0.006 |
| Environmental risk factors, N (%) | ||||
| Social support, N (%) | ||||
| 0 confidants | 113 (32.5) | 38 (32.8) | 75 (32.3) | 0.02 |
| 1–5 confidants | 205 (58.9) | 75 (64.7) | 130 (56.0) | |
| 6+ confidants | 30 (8.6) | 3 (2.6) | 27 (11.6) | |
| Physical assault, past 6 months | 35 (10.1) | 19 (16.2) | 16 (7.0) | 0.007 |
| Any nights spent in unsheltered settings, past 6 months | 286 (81.7) | 101 (85.6) | 185 (79.7) | 0.18 |
ADL Activities of Daily Living, SPPB Short Physical Performance Battery, CES-D Center for Epidemiologic Studies Depression Scale
*Visual acuity < 20/100 using the Snellen test
†Cognitive impairment defined as a Modified Mini-Mental State Examination score < 7th percentile (i.e., 1.5 standard deviations below the demographically adjusted cohort mean)
‡Greater than or equal to 6 drinks on one occasion ≥ once monthly
§Moderate-to-severe illicit drug use for the past 6 months defined as a World Health Organization’s Alcohol, Smoking and Substance Involvement Screening Test score for cocaine, amphetamines, opioids, and marijuana with a score of ≥ 4
Fall Prevalence and Seeking Care for Falls
At baseline, over one third (33.7%) reported one or more falls in the past 6 months (Table 1). Of the 118 participants who reported falling at baseline, 28.0% reported 4 or more falls, 35.6% two to three falls, and 36.4% one fall. One third (33.1%) of participants who fell required medical treatment due to a fall.
During the 36-month study, 28 participants died. Of those who survived, 183 completed all six follow-up interviews; 72 completed 4–5 interviews, 32 completed 2–3 interviews, and 21 completed one follow-up interview. We found a higher mean number of falls at baseline among those who died during follow-up (mean 0.42; standard deviation (SD) 0.50) and those who had not died but had missed visits (mean 0.38; SD 0.49) than among those who completed follow-up (mean 0.30; SD 0.46).
Of the 350 participants, 218 (62.3%) reported one or more falls in at least one study visit, 107 (30.6%) reported falls in at least half of the visits, and 34 (9.7%) reported falls at all visits.
Factors Associated with Falls
Those who reported falls at baseline had a higher prevalence of known risk factors for falls than those who had not fallen (Table 1). People with falls were significantly more likely to have less than a high school education, a history of stroke, difficulty with ADLs, mobility impairment, use of assistive device, increased urinary incontinence, and depressive symptoms. We found that those who fell were more likely to have moderate-to-high risk opioid and marijuana use, fewer social confidants, have spent at least one night unsheltered, or experienced physical assault.
In models adjusted for key covariates, individual risk factors associated with significantly higher odds of falls included older age (adjusted odds ratio (AOR) 1.03, confidence interval (CI) 1.00–1.06), being a woman (AOR 1.45, 95% CI 1.02–2.04), having non-Black race (AOR 1.65, 95% CI 1.12–2.43), having a history of stroke (AOR 2.17, 95% CI 1.42–3.32), reporting an ADL impairment (AOR 1.99, 95% CI 1.51–2.63), urinary incontinence (AOR 1.40, 95% CI 1.07–1.81), and use of an assistive device (AOR 1.86, 95% CI 1.39–2.50) (Table 2).
Table 2.
Odds of Experiencing Falls in the Past 6 Months over 3 Years in the GEE Model Among Adults Aged ≥ 50 Years Who Were Homeless at Baseline 2013–2014
| Variables | Unadjusted odds ratio (OR) (95% CI)* | Adjusted odds ratio (AOR) (95% CI) |
|---|---|---|
| Individual risk factors | ||
| Age (continuous years) | 1.03 (1.00–1.05) | 1.03 (1.00–1.06) |
| Women | 1.59 (1.11–2.27) | 1.45 (1.02–2.04) |
| Non-Black | 1.68 (1.15–2.45) | 1.65 (1.12–2.43) |
| < High school diploma/GED | 1.37 (0.94–2.01) | – |
| Health status | ||
| Myocardial infarction | 2.15 (1.30–3.57) | – |
| Congestive heart failure | 1.70 (0.98–2.94) | – |
| Stroke | 3.36 (2.07–5.47) | 2.17 (1.42–3.32) |
| Arthritis | 1.44 (1.04–2.00) | – |
| Diabetes | 0.74 (0.49–1.10) | – |
| Chronic lung disease | 1.61 (1.16–2.24) | – |
| Hearing impairment | 1.49 (1.07–2.08) | – |
| ≥ 1 ADL impairments | 3.06 (2.34–3.99) | 1.99 (1.51–2.63) |
| Physical performance (SPPB test score ≤ 10) | 1.82 (1.29–2.56) | – |
| Urinary incontinence | 2.23 (1.71–2.91) | 1.40 (1.07–1.81) |
| Depressive symptoms (CES-D score ≥ 22) | 1.73 (1.31–2.28) | – |
| Pain severity | ||
| Moderate | 1.74 (1.26–2.40) | |
| Severe | 2.51 (1.83–3.44) | |
| Assistive device | 2.81 (2.11–3.75) | 1.86 (1.39–2.50) |
| Health-related behaviors | ||
| Current smoker | 1.30 (0.96–1.77) | |
| Heavy drinking† | 1.63 (1.08–2.47) | – |
| Cocaine‡ | 1.36 (1.00–1.86) | – |
| Opioids | 2.13 (1.35–3.36) | 1.64 (1.02–2.65) |
| Marijuana | 1.85 (1.40–2.42) | 1.93 (1.47–2.55) |
| Environmental risk factors | ||
| Social support | ||
| 1–5 confidants | 1.11 (0.84–1.46) | – |
| ≥ 6 confidants | 0.65 (0.36–1.15) | – |
| Physical assault, past 6 months | 2.28 (1.65–3.17) | 1.67 (1.18–2.37) |
| Any nights spent in unsheltered settings, past 6 months | 1.49 (1.16–1.91) | 1.42 (1.10–1.83) |
GED General Education Development, ADL Activities of Daily Living, SPPB Short Physical Performance Battery, CES-D Center for Epidemiologic Studies Depression Scale
*Only bivariate variables with any type 1 p values < 0.20 are shown, and these were entered in the starting multivariate model
†Greater than or equal to 6 drinks on one occasion ≥ once monthly
‡Moderate-to-severe illicit drug use for the past 6 months defined as a World Health Organization’s Alcohol, Smoking and Substance Involvement Screening Test score for cocaine, amphetamines, opioids, and marijuana with a score of ≥ 4
Moderate-to-severe marijuana use (AOR 1.93, 95% CI 1.47–2.55) and moderate-to-severe opioid use (AOR 1.64, 95% CI 1.02–2.65) were associated with increased odds of falling. Experiencing physical assault (AOR 1.67, 95% CI 1.18–2.37) and spending any night unsheltered (AOR 1.42, 95% CI 1.10–1.83) in the last 6 months were as well.
In a sensitivity analysis, we found that those who had died during study follow-up (AOR 1.35, 95% CI 0.56–3.28) or who survived to study follow-up but had missed visits (AOR 1.24, 95% CI 0.89–1.72) were more likely to experience falls.
DISCUSSION
In this longitudinal study of adults aged 50 and older who were homeless at study enrollment, we found a high prevalence of falls. Despite a median age of 58 years, study participants reported a prevalence of falls higher than older adults with a mean age of 78 in the general population 3. Many participants fell repeatedly throughout the 3-year study period; over a third of the cohort reported falls in at least half of their study visits. We found an association between falls and several factors known to increase fall risk within the general population, including older age, gender, functional impairment, urinary incontinence, use of an assistive device, and stroke.
Our findings indicate that the increased risk of falls in homeless older adults results, in part, from a high prevalence of geriatric conditions (e.g., functional and urinary impairment) and substance use (e.g., problematic opioid use) known to increase fall risk 2. Some of these risk factors may be modifiable via physical and occupational therapy, although it is more difficult to intervene while someone is experiencing homelessness. As the average age of the homeless population continues to increase, the population will have increasing prevalence of geriatric risk factors 39.
We identified the following novel risk factors: using marijuana, experiencing physical assault, and spending time unsheltered that contributed to the high fall prevalence in our population. Both opioid use and marijuana use were associated with increased odds of falling. Opioid use is associated with increased fall risk among older adults in the general population 40, 41. However, despite research on marijuana use and injuries in community-dwelling older adults, little is known about how marijuana use impacts falls 42–44. Marijuana—like opioids—may increase falls by affecting the sensorium, inducing dizziness, confusion, and drowsiness 42, 45. We found a high prevalence of marijuana use among study participants. People born in the study’s age cohort have had high prevalence of marijuana use their whole lives, including in older adulthood 46–48. As marijuana use among older adults increases, due to changes in legal status and cohort effects, there may be increased falls associated with its use.
Experiencing physical assault is common among older adults who are homeless 16. Physical assault can increase fall risk directly (as a complication of assault), or indirectly, by causing injuries that enhance underlying individual vulnerabilities associated with falls 16. Future research should evaluate the role of marijuana use and physical assault in falls among housed older adults to determine whether these risk factors are unique to older adults experiencing homelessness.
People who are unsheltered have increased exposure to unsafe environments, with minimal control. They may stay in isolated locations with uneven surfaces and physical barriers, such as abandoned buildings, under bridges, or along highways. Unsheltered environments lack lighting or protection against environmental hazards. Avoiding falls requires intact executive function and physical agility to be able to process external stimuli and modify movements to remain upright 49. For older adults with vulnerabilities—such as those common among homeless older adults—small external triggers (e.g., rain, sidewalk debris, or uneven surfaces) may precipitate falls. Housed older adults are able to modify their behaviors to avoid high-risk environmental exposures that predispose them to falls. For example, they can decrease how often they walk outside on uneven surfaces or minimize their public transit use. In contrast, adults living in unsheltered settings have less ability to avoid high-risk environmental exposures 50.
Our finding that non-Black race was associated with increased falls is consistent with research in housed adults 51, 52. Homelessness is caused by an interaction between structural factors and individual risk factors. Because Black Americans face structural racism, Black Americans with less individual vulnerability (such as substance use and mental health disabilities) are at risk of homelessness. While we adjusted for these conditions, there may be unmeasured confounders that we were unable to account for 1, 53.
Limitations
Our study has several limitations. We rely on 6-month recall of falls. Other studies of falls in older adults use timeframes that range from monthly to biennial 54, 55. Participants without complete study follow-up had a higher prevalence of falls, indicating that our model may have underestimated the odds of experiencing falls. We did not ask about prescribed medications and could not report on the role of polypharmacy. We conducted the study in the San Francisco Bay Area, where 67% of people experiencing homelessness live unsheltered, compared to 5% in both New York and Boston 56. Studies in cities with lower proportions of unsheltered homelessness may report lower rates of falls. Among individuals who are unsheltered, there are a wide variety of environments that may affect fall risk. We did not have detailed data on the variety of environments in which unsheltered homeless people stayed and cannot assess the risk of these different exposures.
CONCLUSION
Older homeless adults have a high rate of falls, similar to those of adults 20 years older. The increased risk is due to a high prevalence of individual risk factors and environmental exposures. Identifying people at high risk of falls could allow targeted interventions, such as providing shelter, low-height accessible beds, counseling on marijuana and opioid use, and physical therapy. For older adults who live unsheltered, there are nascent efforts to have occupational therapists visit unsheltered settings to reduce fall risk by employing reflective tape and anchoring unstable environmental elements 57, 58. Finally, reducing unsheltered homelessness—via either increased shelters or, ideally, increased long-term housing—could decrease the number of falls in this high-risk population.
Acknowledgments
Contributors
We gratefully acknowledge our colleagues Claudia Ponath, Pamela Olsen, John Weeks, Stephen King, and Kenneth Perez for their invaluable contributions to the HOPE HOME study. The authors also thank the staff at St. Mary’s Center and the HOPE HOME Community Advisory Board for their guidance and partnership.
Funding Information
This study was funded by grants from the National Institute on Aging at the National Institutes of Health (R01AG041860, K24AG046372, K23AG045290, K76AG057016) and the American Federation for Aging Research (K76AG057016). These funding sources had no role in the preparation, review, or approval of the manuscript.
Compliance with Ethical Standards
Conflict of Interest
The authors declare that they do not have a conflict of interest.
Disclaimer/Disclosures
The views expressed here/in this manuscript are those of the authors and do not necessarily represent the views of the National Institute on Aging at the National Institutes of Health or the American Federation for Aging Research.
Footnotes
Prior Presentations
This study was presented at the Society of General Internal Medicine Annual Meeting, May 2019.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Henry M, Watt R, Rosenthal L, Shivji A. The 2017 Annual Homeless Assessment Report (AHAR) to Congress. Washington: DC: The U.S. Department of Housing and Urban Development: Office of Community Planning and Development;2017.
- 2.Brown RT, Hemati K, Riley ED, et al. Geriatric Conditions in a Population-Based Sample of Older Homeless Adults. Gerontologist. 2017;57(4):757–766. doi: 10.1093/geront/gnw011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Brown RT, Kiely DK, Bharel M, Mitchell SL. Geriatric syndromes in older homeless adults. J Gen Intern Med. 2012;27(1):16–22. doi: 10.1007/s11606-011-1848-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Cigolle CT, Ha J, Min LC, et al. The epidemiologic data on falls, 1998-2010: more older Americans report falling. JAMA Intern Med. 2015;175(3):443–445. doi: 10.1001/jamainternmed.2014.7533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Florence CS, Bergen G, Atherly A, Burns E, Stevens J, Drake C. Medical Costs of Fatal and Nonfatal Falls in Older Adults. J Am Geriatr Soc. 2018;66(4):693–698. doi: 10.1111/jgs.15304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Friedman SM, Munoz B, West SK, Rubin GS, Fried LP. Falls and fear of falling: which comes first? A longitudinal prediction model suggests strategies for primary and secondary prevention. J Am Geriatr Soc. 2002;50(8):1329–1335. doi: 10.1046/j.1532-5415.2002.50352.x. [DOI] [PubMed] [Google Scholar]
- 7.King MB, Tinetti ME. Falls in community-dwelling older persons. J Am Geriatr Soc. 1995;43(10):1146–1154. doi: 10.1111/j.1532-5415.1995.tb07017.x. [DOI] [PubMed] [Google Scholar]
- 8.Tinetti ME, Inouye SK, Gill TM, Doucette JT. Shared risk factors for falls, incontinence, and functional dependence. Unifying the approach to geriatric syndromes. JAMA. 1995;273(17):1348–1353. [PubMed] [Google Scholar]
- 9.Tinetti ME. Preventing Falls in Elderly Persons. N Engl J Med. 2003;348(1):42–49. doi: 10.1056/NEJMcp020719. [DOI] [PubMed] [Google Scholar]
- 10.Tinetti ME, Baker DI, McAvay G, et al. A multifactorial intervention to reduce the risk of falling among elderly people living in the community. N Engl J Med. 1994;331(13):821–827. doi: 10.1056/NEJM199409293311301. [DOI] [PubMed] [Google Scholar]
- 11.Paliwal Y, Slattum PW, Ratliff SM. Chronic Health Conditions as a Risk Factor for Falls among the Community-Dwelling US Older Adults: A Zero-Inflated Regression Modeling Approach. Biomed Res Int. 2017;2017:5146378. doi: 10.1155/2017/5146378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Li W, Keegan TH, Sternfeld B, Sidney S, Quesenberry CP, Jr, Kelsey JL. Outdoor falls among middle-aged and older adults: a neglected public health problem. Am J Public Health. 2006;96(7):1192–1200. doi: 10.2105/AJPH.2005.083055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kelsey JL, Berry SD, Procter-Gray E, et al. Indoor and outdoor falls in older adults are different: the maintenance of balance, independent living, intellect, and Zest in the Elderly of Boston Study. J Am Geriatr Soc. 2010;58(11):2135–2141. doi: 10.1111/j.1532-5415.2010.03062.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Inouye SK, Studenski S, Tinetti ME, Kuchel GA. Geriatric syndromes: clinical, research, and policy implications of a core geriatric concept. J Am Geriatr Soc. 2007;55(5):780–791. doi: 10.1111/j.1532-5415.2007.01156.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Spinelli MA, Ponath C, Tieu L, Hurstak EE, Guzman D, Kushel M. Factors associated with substance use in older homeless adults: Results from the HOPE HOME study. Subst Abus. 2017;38(1):88–94. doi: 10.1080/08897077.2016.1264534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Tong MS, Kaplan LM, Guzman D, Ponath C, Kushel MB. Persistent Homelessness and Violent Victimization Among Older Adults in the HOPE HOME Study. J Interpers Violence. 2019:886260519850532. [DOI] [PMC free article] [PubMed]
- 17.Lee CT, Guzman D, Ponath C, Tieu L, Riley E, Kushel M. Residential patterns in older homeless adults: Results of a cluster analysis. Soc Sci Med. 2016;153:131–140. doi: 10.1016/j.socscimed.2016.02.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Burnam MA, Koegel P. Methodology for obtaining a representative sample of homeless persons: The Los-Angeles skid row study. Eval Rev. 1988;12(2):117–152. [Google Scholar]
- 19.Brown RT, Goodman L, Guzman D, Tieu L, Ponath C, Kushel MB. Pathways to Homelessness among Older Homeless Adults: Results from the HOPE HOME Study. PLOS ONE. 2016;11(5):e0155065. doi: 10.1371/journal.pone.0155065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Dunn LB, Jeste DV. Enhancing informed consent for research and treatment. Neuropsychopharmacology. 2001;24(6):595–607. doi: 10.1016/S0893-133X(00)00218-9. [DOI] [PubMed] [Google Scholar]
- 21.U.S. Census Bureau. 2010 Census of Population Housing. Available at: https://www.census.gov/programs-surveys/decennial-census/decade.2010.html. Accesssed August 27th 2019.
- 22.Teno JM, Licks S, Lynn J, et al. Do advance directives provide instructions that direct care? SUPPORT Investigators. Study to Understand Prognoses and Preferences for Outcomes and Risks of Treatment. J Am Geriatr Soc. 1997;45(4):508–512. doi: 10.1111/j.1532-5415.1997.tb05179.x. [DOI] [PubMed] [Google Scholar]
- 23.U.S. Preventive Services Task Force (USPSTF) Siu AL, Bibbins-Domingo K, et al. Screening for impaired visual acuity in older adults: U.S. Preventive Services Task Force recommendation statement. Ann Intern Med. 2009;151(1):37–43. doi: 10.7326/0003-4819-151-1-200907070-00007. [DOI] [PubMed] [Google Scholar]
- 24.Moyer VA. Screening for hearing loss in older adults: U.S. Preventive Services Task Force recommendation statement. Ann Intern Med. 2012;157(9):655–661. doi: 10.7326/0003-4819-157-9-201211060-00526. [DOI] [PubMed] [Google Scholar]
- 25.Bland RC, Newman SC. Mild dementia or cognitive impairment: the Modified Mini-Mental State examination (3MS) as a screen for dementia. Can J Psychiatry. 2001;46(6):506–510. doi: 10.1177/070674370104600604. [DOI] [PubMed] [Google Scholar]
- 26.Katz S. Assessing self-maintenance: activities of daily living, mobility, and instrumental activities of daily living. J Am Geriatr Soc. 1983;31(12):721–727. doi: 10.1111/j.1532-5415.1983.tb03391.x. [DOI] [PubMed] [Google Scholar]
- 27.Guralnik JM, Simonsick EM, Ferrucci L, et al. A short physical performance battery assessing lower extremity function: association with self-reported disability and prediction of mortality and nursing home admission. J Gerontol. 1994;49(2):M85–94. doi: 10.1093/geronj/49.2.m85. [DOI] [PubMed] [Google Scholar]
- 28.Brown JS, Bradley CS, Subak LL, et al. The sensitivity and specificity of a simple test to distinguish between urge and stress urinary incontinence. Ann Intern Med. 2006;144(10):715–723. doi: 10.7326/0003-4819-144-10-200605160-00005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Radloff LS. The CES-D Scale: A self-report depression scale for research in the general population. Applied Psychological Measurement. 1977;1(3):385–401. [Google Scholar]
- 30.Cleeland CS, Ryan KM. Pain assessment: global use of the Brief Pain Inventory. Ann Acad Med Singapore. 1994;23(2):129–138. [PubMed] [Google Scholar]
- 31.Al-Delaimy, WK; Edland, S; Pierce, JP; et al. California Tobacco Survey (CTS) 2008. Available at: 10.6075/J0KW5CX7. Accessed August 27th 2019.
- 32.Babor TF, Higgins-Biddle JC, Saunders JB, Monteiro MG. The Alcohol Use Disorders Identification Test: Guidelines for Use in Primary Care. World Health Organization;2001.
- 33.Humeniuk R, Henry-Edwards S, Ali R, Poznyak V, Monteiro M. The Alcohol, Smoking and Substance Involvement Screening Test (ASSIST): Manual for use in primary care. Geneva: World Health Organization; 2010. [Google Scholar]
- 34.Gielen AC, O'Campo PJ, Faden RR, Kass NE, Xue X. Interpersonal conflict and physical violence during the childbearing year. Soc Sci Med. 1994;39(6):781–787. doi: 10.1016/0277-9536(94)90039-6. [DOI] [PubMed] [Google Scholar]
- 35.Gielen AC, McDonnell KA, Wu AW, O'Campo P, Faden R. Quality of life among women living with HIV: the importance violence, social support, and self care behaviors. Soc Sci Med. 2001;52(2):315–322. doi: 10.1016/s0277-9536(00)00135-0. [DOI] [PubMed] [Google Scholar]
- 36.Riley ED, Cohen J, Knight KR, Decker A, Marson K, Shumway M. Recent violence in a community-based sample of homeless and unstably housed women with high levels of psychiatric comorbidity. Am J Public Health. 2014;104(9):1657–1663. doi: 10.2105/AJPH.2014.301958. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Straus MA, Hamby SL, Boney-McCoy SUE, Sugarman DB. The Revised Conflict Tactics Scales (CTS2): Development and Preliminary Psychometric Data. J Fam Issues. 1996;17(3):283–316. [Google Scholar]
- 38.Tsemberis S, McHugo G, Williams V, Hanrahan P, Stefancic A. Measuring homelessness and residential stability: The residential time-line follow-back inventory. J Community Psychol. 2006;35(1):29–42. [Google Scholar]
- 39.Culhane DP, Treglia D, Byrne T, et al. The Emerging Crisis of Aged Homelessness: A Multi-Site Research Project: Could Housing Solutions Be Funded by Avoidance of Excess Shelter, Hospital, and Nursing Home Costs? 2019. Available at: https://www.aisp.upenn.edu/wp-content/uploads/2019/01/Emerging-Crisis-of-Aged-Homelessness-1.pdf. Accessed August 27th 2019.
- 40.Daoust R, Paquet J, Moore L, et al. Recent opioid use and fall-related injury among older patients with trauma. CMAJ. 2018;190(16):E500–e506. doi: 10.1503/cmaj.171286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Rolita L, Spegman A, Tang X, Cronstein BN. Greater number of narcotic analgesic prescriptions for osteoarthritis is associated with falls and fractures in elderly adults. J Am Geriatr Soc. 2013;61(3):335–340. doi: 10.1111/jgs.12148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Abuhasira R, Schleider LB, Mechoulam R, Novack V. Epidemiological characteristics, safety and efficacy of medical cannabis in the elderly. Eur J Intern Med. 2018;49:44–50. doi: 10.1016/j.ejim.2018.01.019. [DOI] [PubMed] [Google Scholar]
- 43.Choi NG, Marti CN, DiNitto DM, Choi BY. Older adults' marijuana use, injuries, and emergency department visits. Am J Drug Alcohol Abuse. 2018;44(2):215–223. doi: 10.1080/00952990.2017.1318891. [DOI] [PubMed] [Google Scholar]
- 44.Barrio G, Jiménez-Mejías E, Pulido J, Lardelli-Claret P, Bravo MJ, de la Fuente L. Association between cannabis use and non-traffic injuries. Accident Analysis & Prevention. 2012;47:172–176. doi: 10.1016/j.aap.2012.01.002. [DOI] [PubMed] [Google Scholar]
- 45.Briscoe J, Casarett D. Medical Marijuana Use in Older Adults. J Am Geriatr Soc. 2018;66(5):859–863. doi: 10.1111/jgs.15346. [DOI] [PubMed] [Google Scholar]
- 46.Lloyd SL, Striley CW. Marijuana Use Among Adults 50 Years or Older in the 21st Century. Gerontology and Geriatric Medicine. 2018;4:2333721418781668. doi: 10.1177/2333721418781668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Dinitto DM, Choi NG. Marijuana use among older adults in the U.S.A.: user characteristics, patterns of use, and implications for intervention. Int Psychogeriatr. 2011;23(5):732–741. doi: 10.1017/S1041610210002176. [DOI] [PubMed] [Google Scholar]
- 48.Johnson PB, Sung H-E. Substance Abuse among Aging Baby Boomers: Health and Treatment Implications. J Addict Nurs. 2009;20(3):124–126. [Google Scholar]
- 49.Nowak A, Hubbard RE. Falls and frailty: lessons from complex systems. J R Soc Med. 2009;102(3):98–102. doi: 10.1258/jrsm.2009.080274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Clemson L, Cusick A, Fozzard C. Managing risk and exerting control: determining follow through with falls prevention. Disabil Rehabil. 1999;21(12):531–541. doi: 10.1080/096382899297189. [DOI] [PubMed] [Google Scholar]
- 51.Sun DQ, Huang J, Varadhan R, Agrawal Y. Race and fall risk: data from the National Health and Aging Trends Study (NHATS) Age Ageing. 2016;45(1):120–127. doi: 10.1093/ageing/afv173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Hanlon JT, Landerman LR, Fillenbaum GG, Studenski S. Falls in African American and White Community-Dwelling Elderly Residents. The Journals of Gerontology: Series A. 2002;57(7):M473–M478. doi: 10.1093/gerona/57.7.m473. [DOI] [PubMed] [Google Scholar]
- 53.Gee GC, Ford CL. STRUCTURAL RACISM AND HEALTH INEQUITIES: Old Issues, New Directions. Du Bois Rev. 2011;8(1):115–132. doi: 10.1017/S1742058X11000130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Blackwood J. Cognitive Function and Falls in Older Adults With Type 2 Diabetes Mellitus. J Geriatr Phys Ther. [DOI] [PubMed]
- 55.Leveille SG, Kiel DP, Jones RN, et al. The MOBILIZE Boston Study: design and methods of a prospective cohort study of novel risk factors for falls in an older population. BMC Geriatr. 2008;8:16. doi: 10.1186/1471-2318-8-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Bay Area Council Economic Institute. Bay Area Homelessness: A Regional View of A Regional Crisis. 2019. Available at: http://www.bayareaeconomy.org/files/pdf/BayAreaHomelessnessReport.pdf. Accessed August 27th 2019.
- 57.Los Angeles County Department of Health Services (DHS). Housing for Health. 2019. Available at: http://dhs.lacounty.gov/wps/portal/dhs/housingforhealth. Accessed Nov 8th 2019.
- 58.Henwood B. Piloting the CAPABLE model in Permanent Supportive Housing. 2019. Available at: https://sc-ctsi.org/funding/awardees/benjamin-henwood-1. Accessed Nov 8th 2019.


