Abstract
Although results of animal research show that interactions between stress and sex hormones are implicated in the development of affective disorders in women, translation of these findings to patients has been scarce. As a basic step toward advancing this field of research, we analyzed findings of studies which reported circulating cortisol levels in healthy women in the follicular vs. luteal phase of the menstrual cycle. We deemed this analysis critical not only to advance our understanding of basic physiology, but also as an important contrast to the findings of future studies evaluating stress and sex hormones in women with affective disorders. We hypothesized that cortisol levels would be lower in the follicular phase based on the proposition that changes in levels of potent GABAergic neurosteroids, including allopregnanolone, during the menstrual cycle dynamically change in the opposite direction relative to cortisol levels. Implementing strict inclusion criteria, we compiled results of high-quality studies involving 778 study participants to derive a standardized mean difference between circulating cortisol levels in the follicular vs. luteal phase of the menstrual cycle. In line with our hypothesis, our meta-analysis found that women in the follicular phase had higher cortisol levels than women in the luteal phase, with an overall Hedges' g of 0.13 (p < 0.01) for the random effects model. No significant between-study difference was detected, with the level of heterogeneity in the small range. Furthermore, there was no evidence of publication bias. As cortisol regulation is a delicate process, we review some of the basic mechanisms by which progesterone, its potent metabolites, and estradiol regulate cortisol output and circulation to contribute to the net effect of higher cortisol in the follicular phase.
Keywords: cortisol, hypothalamic-pituitary-gonadal (HPG) axis, hypothalamic-pituitary-adrenal (HPA) axis, menstrual cycle, follicular, luteal
Introduction
Women exhibit high prevalence of stress-related disorders, such as major depressive disorder (MDD) and anxiety spectrum disorder (1–9). Importantly, the increase in prevalence of these disorders is observed during periods of drastic hormonal changes, such as puberty, the pre-menstrual period, pregnancy, postpartum and menopause (10–12). These observations suggest that interactions between sex hormones, regulated by the hypothalamic-pituitary-gonadal (HPG) axis, and cortisol, a stress hormone under the control of the hypothalamic-pituitary-adrenal (HPA) axis, may be critical determinants of stress-related disorder development and progression.
Research evaluating stress effects in MDD and anxiety disorders demonstrates a blunted cortisol response to psychosocial stress in female patients compared to their respective controls [for a meta-analysis, see (13)]. However, although these research studies provide valuable information, they only examine function of the HPA axis, without evaluating how sex hormones influence it.
The number of studies evaluating interactions between the provoked HPA and the HPG axes is limited in both diseased as well as healthy participants. Results of studies comparing reactivity to psychosocial stress in healthy women suggest that cortisol output is higher in the luteal vs. follicular phase of the menstrual cycle (14, 15). However, their small sample size and opposite findings from other studies (16–19) indicate that more research needs to be completed before a conclusion can be drawn. Additional studies, implementing strict verification of menstrual cycle phase, stress manipulation and participants' healthy status, are needed.
An even more fundamental question, though, is related to the physiological relationship between the HPA and HPG axes under unprovoked, tonic conditions. However, results from human laboratory and observational studies in healthy volunteers evaluating basal cortisol levels across the menstrual cycle range broadly. Thus, we focused on the function of the HPA axis with the hypothesis that there would be a higher physiological output of cortisol during the follicular compared to the luteal phase of the menstrual cycle. Our hypothesis was based on the finding that the progesterone metabolite allopregnanolone positively modulates gamma-aminobutyric acid (GABA)A receptors via an allosteric binding site to potentiate inhibitory signaling (20) and enhance the negative feedback on the HPA axis (21, 22). Therefore, during the luteal phase, when allopregnanolone levels are high, cortisol levels would be expected to decrease relative to the follicular phase, when allopregnanolone levels are low.
Tonic levels of cortisol across the menstrual cycle have been reported as higher for example, (23, 24) or unchanged (25, 26) in the follicular vs. luteal phase. These discrepancies are rooted in marked methodological differences across studies. Hence, our analysis only included high-quality research studies implementing strict criteria and phase identification. Based on mechanistic considerations of basic research studies (reviewed in the Discussion section) that have reported the effects of neuroactive steroids on the HPA axis function, we predicted a surge in cortisol during the early/mid-follicular phase. Our meta-analysis, indeed, shows that circulating cortisol levels change dynamically as a function of menstrual cycle phase, suggesting cortisol is specifically required during the early/mid follicular phase to mediate adaptive physiological processes in response to environmental stimuli, when both estradiol and progesterone are low.
Methods
Search Strategy
We conducted a literature search in PubMed, Web of Knowledge and PsychInfo, and included eligible studies published through December 5th, 2019. Two authors (AH and KK) completed their search independently according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines (27). Any discrepancies were reconciled by reviewing the literature jointly for specific points of difference. We used the following search string: [(“Cortisol”) AND (“Menstrual” OR “Luteal” OR “Follicular”) for (DOCUMENT TYPE: (Article); LANGUAGE: English; SUBJECTS: Human)]. We compiled the results in EndNote X8.
Inclusion/Exclusion Criteria
This meta-analysis evaluated tonic peripheral cortisol levels of healthy menstruating female study participants across follicular vs. luteal phases of the menstrual cycle. Studies were considered eligible if a baseline value was provided prior to a laboratory intervention (for example, psychosocial stress procedure or exercise), if samples were collected longitudinally in a naturalistic (or a laboratory) setting across the menstrual cycle, if an experimental design evaluating a disease state included a healthy control or if an intervention included a placebo control. The exclusionary criteria implementation was carried out in a two-step approach.
In the first step, study abstracts (N = 2,225) were excluded if they were: (1) abstracts, review papers or case studies, (2) animal studies, or evaluation of cell lines, (3) male-only evaluations, (4) abstracts which only mentioned one menstrual phase (luteal or follicular) as a means of controlling for menstrual cycle phase (i.e., not as a comparison of the two phases), (5) studies evaluating a diseased population (including smokers or other substance use disorder population) or implementing a menstrual phase-specific intervention (without a placebo control). This category also included abstracts describing pregnant as well as women in the peri- or post-menstrual phases, as well as women who were on oral contraceptives. Finally, abstracts describing athletes or women who experienced early life trauma were also coded in this category. The remaining abstracts were excluded if they: (6) did not mention cortisol (blood, salivary or urinary), (7) were overlapping study participants with an already published study, and (8) if they described a procedure (such as IV fertilization, for example) which could cause changes in circulating cortisol due to anticipation.
In the second round of exclusion criteria implementation, we evaluated full articles. We excluded papers which did not evaluate groups according to menstrual cycle phases, measure cortisol, have a healthy, non-athletic control group, or report mean and/or variance and were published more than 25 years ago. Furthermore, we excluded papers which re-administered stress (as this can distort baseline cortisol levels), performed non-linear cortisol modeling, were non-original, written in languages other than English, or had overlapping participants. Given the rapid decline of cortisol in the morning, studies which collected cortisol during morning times that varied ≥2 h or did not mention what time of the day cortisol sample collection -took place were excluded, as well as studies which determined cycle phase using self-report.
Data Extraction
Information on the following variables was collected: (1) age, (2) BMI, (3) day of follicular and luteal phase of cortisol collection, (4) phase estimation method, (5) time of day of cortisol collection, and (6) physiological source of cortisol level. Regarding the length of phase variable, whereas some studies reported a range of days, others reported multiple, exact days of the cycle on which cortisol was reported. In the event that a study reported cortisol values across multiple days of the menstrual cycle, data from the day closest to the beginning of the cycle (day 1) for follicular phase, and day 21 of the luteal phase were extracted to reflect the greatest contrast of estradiol and progesterone levels across the cycle. In the event that cortisol was reported on multiple “sub-phases” (for example, early-follicular, mid-follicular), again, data from the day closest to the beginning of the cycle (day 1) for follicular phase, and day 21 of the luteal phase were extracted. If cortisol was collected across multiple menstrual cycles (for example, two menstrual cycles), values from the last cycle were reported. In the event that studies reported cortisol values at multiple times of the day (for example, morning and evening), or multiple sources (for example, salivary and plasma), the most frequently reported time (morning) and source (blood) in the remaining studies were used to extract cortisol values.
Data Analysis
Analyses of were carried out by first calculating the Cohen's d effect size (28). In the event mean and variance values were provided for sub-groups of women in follicular and luteal phases, those were combined using the following formulas:
where, N1 = sample size group 1, N2 = sample size group 2, M1 = mean group 1, M2 = mean group 2, SD1 = standard deviation group 1, SD2 = standard deviation group 2.
We divided the mean difference between the two groups by the pooled standard deviation. Next, we used the J-correction factor to obtain the Hedges' g effect size, which corrects for small samples (29) and is considered small, medium, and large for values 0.2, 0.5, and 0.8, respectively. Within- and between-subject study designs were combined as described in Morris et al. (30). We used a random effects model to calculate the pooled effect size with an associated 95% CI and a p-value (31). We assessed source-study heterogeneity using the χ2-based Q test with its associated p-value. A statistically significant Q statistic suggests different effect sizes across studies, implying that methodological or population sample differences may be introducing variance across individual studies. We quantified heterogeneity using I2 with values 25, 50, and 75% suggestive of small, medium and large heterogeneity and calculated potential publication bias using the Classical Tests (32). We completed sub-analyses according to source (saliva vs. plasma) and time of day (morning vs. afternoon). The meta-analysis was performed using the “escalc” function, and publication bias was assessed using the “ranktest” function in “metafor” package (33) in R.
Results
Characteristics of Individual Studies
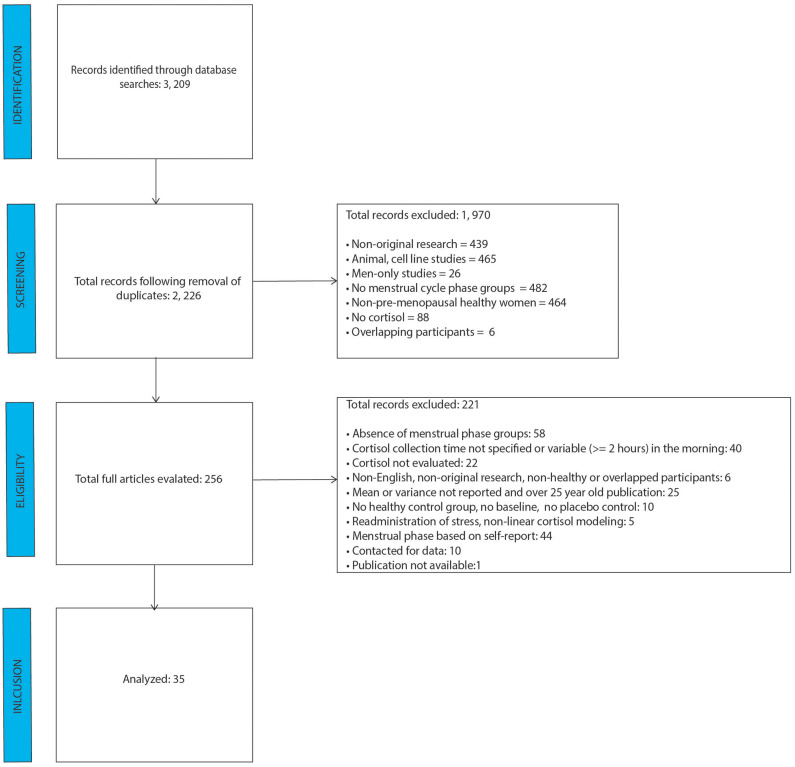
After removal of duplicate studies, literature search identified 2, 226 individual abstracts as shown in the PRISMA figure (Figure 1). Those abstracts were screened for relevance and coded for exclusion reasons. The greatest number of abstracts excluded was based on absence of menstrual cycle groups, followed by cell line/animal research studies. A total of 256 full-text articles were reviewed for relevance, of which 221 were excluded. Of the 221 studies, 44 were excluded based on the self-report nature of menstrual cycle phase determination, and 40 were excluded because they either didn't mention cortisol collection time, or the morning sample was collected at times which varied by two or more hours. The analysis included data from 35 final studies.
Figure 1.
PRISMA flow diagram.
As shown in Table 1, most of the studies included participants in their 20s, with a BMI below 25. Whereas, some studies incorporated fine-grained sub-phases of follicular and luteal phases (see Table 2), others defined the phases as day 1–14 and 15–28. Phase estimation was determined via progesterone level acquisition, LH surge measurement, basal body temperature measurement, or pelvic ultrasound. Times of cortisol collection were in the morning, afternoon/evening or over several hours, and the source was saliva, plasma or urine. Whereas, Supplementary Table 1 shows all the days/phases of menstrual cycle, time of collection and sources of cortisol across all the studies, Table 2 only shows the actual day (or range of days), time and source of cortisol which were included in the analysis. These two tables are provided in order to increase transparency of reporting, as several studies reported several values, for which we implemented the rules as specified in the Methods Section Data Extraction.
Table 1.
Participant information from individual studies.
| References | Sample size (N)* | Age [mean (SD)] | BMI [mean (SD)] | |
|---|---|---|---|---|
| Follicular Phase | Luteal Phase | |||
| Andreano et al. (34) | 20 | 24 | ___ | ___ |
| Barbarino et al. (35) | 5 | 6 | ___ | ___ |
| Beck et al. (36) | 20 | ___ | ___ | |
| Hoeger Bement et al. (37) | 20 | 20.9 (1.0) | 23.0 | |
| Bricout et al. (38) | 11 | 25.5 (7.6) | 19.9 | |
| Cannon et al. (39) | 7 | 8 | ___ | ___ |
| Carr et al. (40) | 4 | ___ | ___ | |
| Caufriez et al. (41) | 10 | 30.0 | 21.8 (0.9) | |
| Childs et al. (42) | 29 | 23 | 21.9 (0.8) | 22.3 (0.3) |
| Collins et al. (43) | 15 | 29.5 | ___ | |
| Espin et al. (14) | 30 | 30 | 19.3 (1.7) | 21.7 (4.1) |
| Genazzani et al. (44) | 5 | ___ | ___ | |
| Heitkemper et al. (45) | 25 | 33.1 (5.3) | 23.6 (4.9) | |
| Huang et al. (46) | 18 | 18 | 22.0 (2.4) | 20.0 (2.8) |
| Inoue et al. (26) | 9 | 23.7 (5.6) | ___ | |
| Judd et al. (47) | 6 | 6 | ___ | ___ |
| Kasa-Vubu et al. (48) | 10 | 14 | 29.4 (8.5) | 24.0 (4.3) |
| Kerdelhué et al. (23) | 11 | ___ | ___ | |
| Kirschbaum et al. (17) | 19 | 21 | 23.4 (3.3) | 21.7 (2.4) |
| LeRoux et al. (49) | 9 | 9 | 21.8 (2.3) | 22.5 (2.4) |
| Liu et al. (50) | 6 | ___ | ___ | |
| Lombardi et al. (51) | 20 | 26.2 | ___ | |
| Maki et al. (52) | 20 | 20 | 27.0 (5.6) | 25.0 (5.0) |
| Ohara et al. (53) | 7 | 22.3 (1.0) | 20.5 (2.1) | |
| Paoletti et al. (54) | 14 | 31.5 (2.7) | 24.2 (2.0) | |
| Parry et al. (55) | 30 | 37.2 (5.8) | ___ | |
| Rasgon et al. (56) | 5 | 27.0 (4.0) | ___ | |
| Reynolds et al. (57) | 61 | 21.7 (3.4) | ___ | |
| Roche and King (58) | 23 | 23 | 24.2 (3.9) | 23.6 (3.8) |
| Stewart et al. (59) | 4 | 24.6 (4.5) | 24.7 (2.1) | |
| Su et al. (60) | 10 | 30.8 (4.9) | ___ | |
| Timon et al. (25) | 20 | ___ | 21.3 (2.1) | |
| Tulenheimo et al. (61) | 14 | ___ | ___ | |
| Villada et al. (62) | 13 | 17 | 19.0 (1.5) | 21.3 (4.0) |
| Wolfram et al. (63) | 29 | 26.3 (3.9) | 22.1 (2.9) | |
Only one sample size (for follicular and luteal phases) is listed for within subject design studies. The total sample size is 778.
Table 2.
Menstrual cycle and outcome measure information from individual studies.
| References | Menstrual cycle | Cortisol | |||
|---|---|---|---|---|---|
| Follicular phase | Luteal phase | Phase estimation | Time | Source | |
| Andreano et al. (34) | 1–7 | 18–24 | Estradiol and progesterone | Afternoon | Saliva |
| Barbarino et al. (35) | 4–8 | 20–24 | Estradiol and progesterone | Morning | Plasma |
| Beck et al. (36) | 10 | 24 | LH surge | Morning | Plasma |
| Hoeger Bement et al. (37) | “Mid-follicular” | “Mid-luteal” | LH surge | Afternoon | Saliva |
| Bricout et al. (38) | “Mid-follicular” | “Mid-luteal” | Estradiol and progesterone | 24-h | Urine |
| Cannon et al. (39) | 1–14 | 15–28 | Progesterone | 24-h | Urine |
| Carr et al. (40) | 1 | 21 | LH surge | Morning | Plasma |
| Caufriez et al. (41) | 3–8 | 23–28 | Basal body temperature | 24-h | Urine |
| Childs et al. (42) | 3–10 | 16–24 | LH ovulation test | Morning | Plasma |
| Collins et al. (43) | 5–7 | 22–25 | Basal body temperature | Morning | Plasma |
| Espin et al. (14) | 5–8 | 20–24 | Basal body temperature | Afternoon | Saliva |
| Genazzani et al. (44) | 1 | 21 | LH surge | Morning | Plasma |
| Heitkemper et al. (45) | 1 | 22 | LH ovulation test | Morning | Urine |
| Huang et al. (46) | 1–4 | 24–28 | Estradiol and progesterone | Afternoon | Saliva |
| Inoue et al. (26) | 1–14 | 21–28 | Estradiol and progesterone | Morning | Plasma |
| Judd et al. (47) | 3–5 | 20–24 | LH ovulation test | 10-h | Serum |
| Kasa-Vubu et al. (48) | 1–14 | 15–28 | LH and progesterone | 24-h | Plasma |
| Kerdelhué et al. (23) | 1 | 21 | LH surge | Morning | Serum |
| Kirschbaum et al. (17) | 4–7 | 21–25 | Estradiol and progesterone | Afternoon | Plasma |
| LeRoux et al. (49) | 8–10 | 20–22 | Estradiol and progesterone | Morning | Saliva |
| Liu et al. (50) | 1–5 | 20–22 | Pelvic Ultrasound | Morning | Plasma |
| Lombardi et al. (51) | 5–7 | 22–26 | LH surge and progesterone | Morning | Serum |
| Maki et al. (52) | 2–4 | 22–24 | LH ovulation test | Afternoon | Saliva |
| Ohara et al. (53) | 1–14 | 15–28 | LH ovulation test | Morning | Saliva |
| Paoletti et al. (54) | 5–8 | 21–24 | Basal body temperature | Morning | Serum |
| Parry et al. (55) | 6–8 | 26–28 | LH ovulation test | Morning | Plasma |
| Rasgon et al. (56) | 2–9 | 7–14 | LH ovulation test | Morning | Plasma |
| Reynolds et al. (57) | 7–10 | 20–23 | LH ovulation test | Afternoon | Saliva |
| Roche and King (58) | 1–14 | 15to 28 | Estradiol and progesterone | Morning | Plasma |
| Stewart et al. (59) | 7 | 21 | Progesterone | 12-h | Plasma |
| Su et al. (60) | 3–7 days after the end of menses | 21 | Progesterone | Morning | Plasma |
| Timon et al. (25) | 1–2 | 21–22 | Basal body temperature | Morning | Urine |
| Tulenheimo et al. (61) | 6–9 | 21–24 | Progesterone | Morning | Plasma |
| Villada et al. (62) | 5–8 | 20–24 | Basal body temperature | Afternoon | Saliva |
| Wolfram et al. (63) | 2–6 | 21–24 | LH ovulation test | CAR | Saliva |
CAR, Cortisol Awakening Response.
Evaluation of Standardized Mean Difference in Cortisol Levels Across Menstrual Cycle
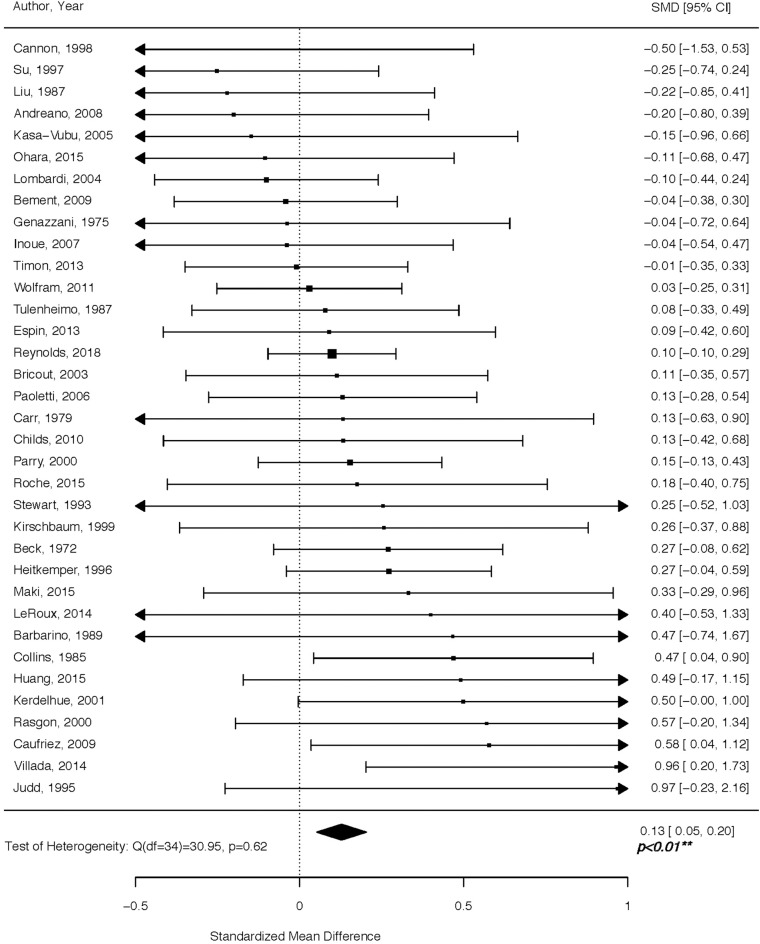
Women in the follicular phase had higher cortisol levels than women in the luteal phase, with an overall Hedges' g of 0.13 (p < 0.01) for the random effects model (Figure 2). The confidence interval range was between 0.05 and 0.20. No significant between-study difference was detected (tau2 =0; H = 1.0), with the level of heterogeneity in the small range (I2 = 0%, Q = 30.69; p = 0.63). The Rank Correlation Test for Funnel Plot Asymmetry resulted in Kendall's tau = 0.14 (p = 0.23), indicating absence of small study effects.
Figure 2.
Forest plot of cortisol levels across the menstrual cycle. Positive standardized mean difference (SMD) means that cortisol levels were higher in the follicular vs. luteal phase.
Sub-analysis of Cortisol Levels According to Source and Time of Day
Sub-analysis according to the biospecimen source showed a significant effect of plasma (p = 0.036) and marginally significant effect of saliva (p = 0.055). The time of day sub-analysis showed a significant effect of morning (p = 0.005), but not afternoon (p = 0.177). Table 3 displays all relevant sub-analyses statistics, including standardized mean difference, standard error, z and p-values, confidence intervals, degrees of freedom, Q statistic and its associated p-value.
Table 3.
Results of sub-analyses according to the biospecimen source and time of day.
| Factor | SMD | Q | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Value | SE | Z value | p-value | CI.LB | CI.UB | df | Value | p-value | |
| Source | |||||||||
| Plasma | 0.12 | 0.0583 | 2.0907 | 0.0366 | 0.0076 | 0.2361 | 18 | 13.2214 | 0.7783 |
| Saliva | 0.1179 | 0.0615 | 1.9182 | 0.0551 | −0.0026 | 0.2384 | 8 | 7.872 | 0.446 |
| Time of day | |||||||||
| Morning | 0.1363 | 0.0485 | 2.8088 | 0.005 | 0.0412 | 0.2314 | 21 | 16.6924 | 0.7296 |
| Afternoon | 0.0966 | 0.0716 | 1.348 | 0.1777 | −0.0438 | 0.237 | 7 | 9.1638 | 0.2411 |
Discussion
For decades, literature on cortisol has yielded mixed results with respect to its concentration in the follicular vs. luteal phase of the menstrual cycle. Implementing a comprehensive search of high-quality studies spanning a period of almost 50 years of research, we show that circulating cortisol levels are higher in the follicular vs. luteal phase. Cortisol regulation is a delicate process of extensive physiological processes working in concert to adjust responses to environmental stimuli. Below, we review mechanisms driving circulating cortisol levels to both increase and decrease across various menstrual cycle time-points, while noting that the net effect of these, or other, still unidentified processes, is a higher circulating cortisol during the follicular compared to the luteal phase, as reported in our analysis (Figure 2).
The paraventricular nucleus (PVN) of the hypothalamus integrates numerous circadian and environmental inputs to funnel information through neurons expressing corticotropin-releasing hormone (CRH). The release of CRH into the hypophyseal portal vasostructure enhances the synthesis and release of adrenocorticotropic hormone (ACTH) from the anterior pituitary, which, in turn, stimulates adrenal glands to synthesize and release cortisol to adapt metabolic processes and behavioral responses.
Intriguingly, PVN neurons express high levels of estrogen receptor beta (ER-β) and low levels of estrogen receptor alpha (ER-α) (64–66). Several research studies have demonstrated that estradiol, through its near equivalent affinity for the two estrogen receptor subtypes, can selectively decrease or increase HPA axis function. A high number of ER-β-expressing cells in the PVN are oxytocin and vasopressin immunoreactive (67–69), which complement the CRH neurons that also express ER-β (64). Stimulation of ER-β in the PVN results in a reduction of cortisol levels. In accord, both centrally- and peripherally-delivered ER-β selective agonists inhibit the HPA function (70). ER-α occupancy, on the other hand, has an indirect, trans-synaptic activation in the PVN. The peri-PVN region contains ER-α neurons, and their activation can impair glucocorticoid-mediated negative feedback regulation of the HPA axis (71). These opposing actions of estradiol—with ER-α amplifying, and ER-β reducing HPA function—are in agreement with laboratory observations that estradiol both enhances (72, 73) and inhibits (74, 75) HPA function. Hence, in the luteal phase, when estradiol levels are higher compared to the early/mid follicular phase, theoretically, depending on the extent of ER-β or ER-α expression and activation in or near the PVN, estradiol can either decrease or increase circulating cortisol levels.
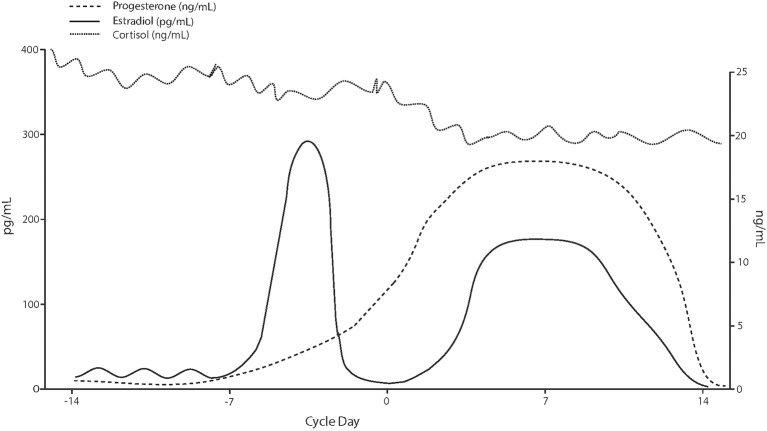
The activity of CRH neurons in the PVN is tightly regulated by inhibitory GABAergic interneuron populations (76). Allopregnanolone, a progesterone derivative resulting from conversion by 5α-reductase type I and 3α-hydroxysteroid dehydrogenase, is an endogenous neurosteroid and a potent, positive, allosteric modulator of the action of the inhibitory neurotransmitter GABA at GABAA receptor. Studies in rodents show an inhibitory effect of allopregnanolone on the function of the HPA axis (77–79). This effect of allopregnanolone seems to be exerted through its action at GABAA receptors, and subsequent inhibition on PVN neurons (80) under both basal and stressful conditions (81). In support of these findings, in addition to allopregnanolone, another potent GABAA receptor modulator and deoxycorticosterone-derived steroid, tetrahydrodeoxycorticosterone (TH-DOC), also attenuates the HPA axis function (77, 82, 83). Therefore, in the luteal phase, under the physiological milieu of higher circulating progesterone levels and, most importantly, of its potent GABAA receptor-modulating metabolite, allopregnanolone, lower circulating cortisol levels can be expected relative to the follicular phase. Not surprisingly, our meta-analysis has confirmed this expectation (Figure 3).
Figure 3.
Hypothetical cortisol levels across the menstrual cycle based on values reported in the analyzed studies.
Once released in the blood flow, ~80% of circulatory cortisol is bound to corticosteroid-binding globulin (CBG), leaving ~5% of cortisol in the free form (84). CBG is primarily synthesized by the liver and secreted into the bloodstream, where it binds and provides a pool of circulating cortisol. It enhances the availability of cortisol to be released on demand both systemically and at a tissue level. Whereas plasma cortisol reflects total cortisol (i.e., bound and unbound), the salivary levels only reflect unbound/free cortisol. Changes in circulating CBG have a significant impact on total, but not free, cortisol concentrations (85, 86). The CBG is under a tight regulation by estradiol, with women expressing greater CBG basal concentrations than men (87). Interestingly, ethinyl estradiol, found in oral contraceptives (OC), dose-dependently increases CBG serum levels (88). Ethynyl estradiol is also a potent ER modulator, with 194 and 151% of the affinity of estradiol for the ER-α and ER-β, respectively (89). It is, however, unclear whether changes in estradiol across the menstrual cycles can alter CBG. Nenke et al. (90) report that total CBG concentration reaches ~1,000 nmol/L in pregnancy as well as during the active phase of pill cycle containing ethinyl estradiol. These expression levels are substantially higher than the CBG levels of ~500 nmol/L determined in non-pregnant, non-OC taking individuals (90). Unfortunately, this study did not account for menstrual cycle phase, which would have provided valuable information regarding CBG changes, if any, across the menstrual cycle. The question of potential CBG changes across the menstrual cycle due to changes in estradiol concentrations should be evaluated in future studies by carefully examining the potential anti-estrogenic and blunting effect of luteal progesterone on estradiol-induced increase in CBG (91).
There are several limitations to consider in the present meta-analysis. First, our sub-analyses may have been underpowered to detect effects of time variations. For example, the “time of day” sub-analysis showed a significant effect of morning, but not afternoon menstrual phase cortisol (Table 3). However, degrees of freedom for morning vs. afternoon sub-analyses were 21 and 7, respectively, with the afternoon sample possibly underpowered to detect a significant effect. Importantly, our sub-analysis of “source” (plasma vs. serum) was consistent with our main study results, showing higher follicular cortisol in both the free and total form. Furthermore, given that the overall sample was fairly homogenous, with most women in the same age range (20–29 years old) and a normal BMI (Table 1), we were unable to perform a meta-regression, which would have provided meaningful information related to the direction of future mechanistic studies.
As the research evaluating interacting effects between HPA and HPG axes unfolds, there are several issues to consider. Perhaps the greatest pitfall of menstrual cycle research is the inadequate assessment of the menstrual cycle phase. In the full-article evaluation step of our meta-analysis, we excluded findings from 44 studies because menstrual cycle phase was estimated based on self-report. Retrospective reports of menstrual cycle “start” and “duration” are plagued by profound phase misinformation (92) and prospective measures confirming both ovulation and luteal phase status are essential. Menstrual cycle phase determination was also based on self-report in approximately half of the studies evaluating the HPA reactivity in the follicular vs. luteal phase (16, 18, 19), contributing to the inability to make meaningful conclusions regarding the direction of effect.
HPA axis dysfunction is strongly implicated in the etiopathology of affective disorders (93–95) with women at an increased risk (96, 97). Yet, basic questions related to the function of the HPA axis throughout stages of the menstrual cycle under acute or prolonged stress conditions remain largely unanswered. Whereas, our meta-analysis reflects a single time point in the cortisol diurnal cycle, it is still unknown whether there are phase-specific effects on the shape of the diurnal curve. This assessment could be easily implemented given the availability of the salivary (unbound) cortisol assay, and would provide a comprehensive picture of daily cortisol trajectory and its potential mean, amplitude and/or phase shift as the hormonal milieu changes across the menstrual cycle. In this case, the awakening and morning cortisol should be taken more frequently than the late afternoon/evening samples.
It is strongly recommended that future studies employ a fine-grained approach (i.e., evaluating early/mid follicular, ovulatory, early, mid and late luteal phases) to advance women's mental health research, rather than broadly defining phases as “follicular” vs. “luteal.”
In summary, the aim of our meta-analysis was to summarize findings of a period spanning over 50 years of research and test whether circulating cortisol levels change as a function of menstrual phase. With respect to this objective, we showed higher cortisol levels in the follicular vs. luteal phase of the menstrual cycle. By completing this aim, our hope is to simultaneously increase awareness of the poor state of women's neuroendocrine science research. Experimental protocols designed to study effects that influence the HPA and HGA axis function need to be specifically designed to account for women's physiological requirements. The joint protocols previously designed for both sexes rarely apply to studies involving women. Whereas, participant recruitment, evaluation and analysis are more rapid in many research scenarios involving men, given the dynamic nature of the menstrual cycle and the need for prospective data collection, the same parameters should not be applied to research involving women. Resources and completion expectations need to be adjusted as such. Once implemented, these changes will contribute meaningful information to progress our understanding of rhythmic hormonal changes, which are crucial for understanding the now well-established sex difference in affective disorder development and progression.
Data Availability Statement
The datasets generated for this study are available on request to the corresponding author.
Author Contributions
AH, KK, SC, and TE-M conceptualized the question, completed literature search and data gathering. AH and FS completed statistical analysis. AH and GP wrote the manuscript.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
The authors would like to thank Dr. Ann Caufriez (Laboratoire de Physiologie et Pharmacologie, Université libre de Bruxelles, Brussels, Belgium) for sending a complete dataset and Dr. Scott Morris (Department of Psychology Illinois Institute of Technology. Chicago, Illinois, USA) for statistical consultation.
The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Footnotes
Funding. Research reported in this publication was supported by the National Institute of Mental Health of the National Institutes of Health under Award Number R21MH119642.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fendo.2020.00311/full#supplementary-material
References
- 1.Albert PR. Why is depression more prevalent in women? J Psychiatry Neurosci. (2015) 40:219–21. 10.1503/jpn.150205 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Angst J, Gamma A, Gastpar M, Lepine JP, Mendlewicz J, Tylee A, et al. Gender differences in depression. Epidemiological findings from the European DEPRES I and II studies. Eur Arch Psychiatry Clin Neurosci. (2002) 252:201–9. 10.1007/s00406-002-0381-6 [DOI] [PubMed] [Google Scholar]
- 3.Barnes VA, Treiber FA, Ludwig DA. African-American adolescents' stress responses after the 9/11/01 terrorist attacks. J Adolesc Health. (2005) 36:201–7. 10.1016/j.jadohealth.2004.02.035 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Breslau N, Schultz L, Peterson E. Sex differences in depression: a role for preexisting anxiety. Psychiatr Res. (1995) 58:1–12. 10.1016/0165-1781(95)02765-O [DOI] [PubMed] [Google Scholar]
- 5.Cahill L. Why sex matters for neuroscience. Nat Rev Neurosci. (2006) 7:477–84. 10.1038/nrn1909 [DOI] [PubMed] [Google Scholar]
- 6.Kessler RC, McGonagle KA, Nelson CB, Hughes M, Swartz M, Blazer DG. Sex and depression in the National Comorbidity Survey. II: Cohort effects. J Affect Disord. (1994) 30:15–26. 10.1016/0165-0327(94)90147-3 [DOI] [PubMed] [Google Scholar]
- 7.McLean CP, Asnaani A, Litz BT, Hofmann SG. Gender differences in anxiety disorders: prevalence, course of illness, comorbidity and burden of illness. J Psychiatr Res. (2011) 45:1027–35. 10.1016/j.jpsychires.2011.03.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Olff M. Sex and gender differences in post-traumatic stress disorder: an update. Eur J Psychotraumatol. (2017) 8:1351204 10.1080/20008198.2017.1351204 [DOI] [Google Scholar]
- 9.Seeman MV. Psychopathology in women and men: focus on female hormones. Am J Psychiatry. (1997) 154:1641–7. 10.1176/ajp.154.12.1641 [DOI] [PubMed] [Google Scholar]
- 10.Beddig T, Kuhner C. Current aspects of premenstrual dysphoric disorder - a review. Psychother Psychosom Med Psychol. (2017) 67:504–13. 10.1055/s-0043-113816 [DOI] [PubMed] [Google Scholar]
- 11.Biaggi A, Conroy S, Pawlby S, Pariante CM. Identifying the women at risk of antenatal anxiety and depression: A systematic review. J Affect Disord. (2016) 191:62–77. 10.1016/j.jad.2015.11.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Birkhauser M. Depression, menopause and estrogens: is there a correlation? Maturitas. (2002) 41:S3–8. 10.1016/S0378-5122(02)00009-9 [DOI] [PubMed] [Google Scholar]
- 13.Zorn JV, Schur RR, Boks MP, Kahn RS, Joels M, Vinkers CH. Cortisol stress reactivity across psychiatric disorders: a systematic review and meta-analysis. Psychoneuroendocrinology. (2017) 77:25–36. 10.1016/j.psyneuen.2016.11.036 [DOI] [PubMed] [Google Scholar]
- 14.Espin L, Almela M, Hidalgo V, Villada C, Salvador A, Gomez-Amor J. Acute pre-learning stress and declarative memory: impact of sex, cortisol response and menstrual cycle phase. Horm Behav. (2013) 63:759–65. 10.1016/j.yhbeh.2013.03.013 [DOI] [PubMed] [Google Scholar]
- 15.Villada C, Hidalgo V, Almela M, Salvador A. Assessing performance on an evaluated speaking task. J Psychophysiol. (2018) 32:64–74. 10.1027/0269-8803/a000185 [DOI] [Google Scholar]
- 16.Montero-Lopez E, Santos-Ruiz A, Garcia-Rios MC, Rodriguez-Blazquez M, Rogers HL, Peralta-Ramirez MI. The relationship between the menstrual cycle and cortisol secretion: Daily and stress-invoked cortisol patterns. Int J Psychophysiol. (2018) 131:67–72. 10.1016/j.ijpsycho.2018.03.021 [DOI] [PubMed] [Google Scholar]
- 17.Kirschbaum C, Kudielka BM, Gaab J, Schommer NC, Hellhammer DH. Impact of gender, menstrual cycle phase, and oral contraceptives on the activity of the hypothalamus-pituitary-adrenal axis. Psychosom Med. (1999) 61:154–62. 10.1097/00006842-199903000-00006 [DOI] [PubMed] [Google Scholar]
- 18.Duchesne A, Tessera E, Dedovic K, Engert V, Pruessner JC. Effects of panel sex composition on the physiological stress responses to psychosocial stress in healthy young men and women. Biol Psychol. (2012) 89:99–106. 10.1016/j.biopsycho.2011.09.009 [DOI] [PubMed] [Google Scholar]
- 19.Duchesne A, Pruessner JC. Association between subjective and cortisol stress response depends on the menstrual cycle phase. Psychoneuroendocrinology. (2013) 38:3155–9. 10.1016/j.psyneuen.2013.08.009 [DOI] [PubMed] [Google Scholar]
- 20.Girdler SS, Klatzkin R. Neurosteroids in the context of stress: implications for depressive disorders. Pharmacol Ther. (2007) 116:125–39. 10.1016/j.pharmthera.2007.05.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Brunton PJ. Neuroactive steroids and stress axis regulation: Pregnancy and beyond. J Steroid Biochem Mol Biol. (2016) 160:160–8. 10.1016/j.jsbmb.2015.08.003 [DOI] [PubMed] [Google Scholar]
- 22.Gunn BG, Cunningham SG, Mitchell JD, Swinny JJ, Lambert D, Belellie D. GABAA receptor-acting neurosteroids: a role in the development and regulation of the stress response. Front Neuroendocrinol. (2015) 35:28–48. 10.1016/j.yfrne.2014.06.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kerdelhué B, Brown S, Lenoir V, Queenan JT, Jones GS, Scholler R, et al. Timing of Initiation of the preovulatory luteinizing hormone surge and its relationship with the circadian cortisol rhythm in the human. Neuroendocrinology. (2002) 75:158–63. 10.1159/000048233 [DOI] [PubMed] [Google Scholar]
- 24.Villada C, Hidalgo V, Almela M, Mastorci F, Sgoifo A, Salvador A. Coping with an acute psychosocial challenge: behavioral and physiological responses in young women. PLoS ONE. (2014) 9:e114640. 10.1371/journal.pone.0114640 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Timon R, Corvillo M, Brazo J, Robles MC, Maynar M. Strength training effects on urinary steroid profile across the menstrual cycle in healthy women. Eur J Appl Physiol. (2013) 113:1469–75. 10.1007/s00421-012-2575-6 [DOI] [PubMed] [Google Scholar]
- 26.Inoue Y, Terao T, Iwata N, Okamoto K, Kojima H, Okamoto T, et al. Fluctuating serotonergic function in premenstrual dysphoric disorder and premenstrual syndrome: findings from neuroendocrine challenge tests. Psychopharmacology. (2007) 190:213–9. 10.1007/s00213-006-0607-9 [DOI] [PubMed] [Google Scholar]
- 27.Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gotzsche PC, Ioannidis JP, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. PLoS Med. (2009) 6:e1000100. 10.1371/journal.pmed.1000100 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Cohen J. Statistical Power Analysis for the Behavioral Sciences. New York, NY: Routledge Academic; (1988). [Google Scholar]
- 29.Hedges L, Olkin I. Statistical Methods for Meta-Analysis. San Diego, CA: Academic Press; (1985). [Google Scholar]
- 30.Morris SB, DeShon RP. Combining effect size estimates in meta-analysis with repeated measures and independent-groups designs. Psychol Methods. (2002) 7:105–25. 10.1037/1082-989x.7.1.105 [DOI] [PubMed] [Google Scholar]
- 31.Borenstein M. Effect sizes for continuous data. In: Cooper H, Hedges L, Valentine J. editors. The Handbook of Research Synthesis and Meta Analysis. New York, NY: Russell Sage Foundation; (2009). [Google Scholar]
- 32.Egger M, Smith G, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. Br Med J. (1997) 315:629–34. 10.1136/bmj.315.7109.629 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Schwarzer G, Antes G, Schumacher M. A test for publication bias in meta-analysis with sparse binary data. Stat Med. (2007) 26:721–33. 10.1002/sim.2588 [DOI] [PubMed] [Google Scholar]
- 34.Andreano JM, Arjomandi H, Cahill L. Menstrual cycle modulation of the relationship between cortisol and long-term memory. Psychoneuroendocrinology. (2008) 33:874–82. 10.1016/j.psyneuen.2008.03.009 [DOI] [PubMed] [Google Scholar]
- 35.Barbarino A, De Marinis L, Folli G, Tofani A, Della Casa S, D'Amico C, et al. Corticotropin-releasing hormone inhibition of gonadotropin secretion during the menstrual cycle. Metabolism. (1989) 38:504–6. 10.1016/0026-0495(89)90208-4 [DOI] [PubMed] [Google Scholar]
- 36.Beck RP, Morcos F, Fawcett D, Watanabe M. Adrenocortical function studies during the normal menstrual cycle and in women receiving norethindrone with and without mestranol. Am J Obstet Gynecol. (1972) 112:364–8. 10.1016/0002-9378(72)90478-4 [DOI] [PubMed] [Google Scholar]
- 37.Hoeger Bement MK, Rasiarmos RL, DiCapo JM, Lewis A, Keller ML, Harkins AL, et al. The role of the menstrual cycle phase in pain perception before and after an isometric fatiguing contraction. Eur J Appl Physiol. (2009) 106:105–12. 10.1007/s00421-009-0995-8 [DOI] [PubMed] [Google Scholar]
- 38.Bricout VA, Wright F, Lagoguey M. Urinary profile of androgen metabolites in a population of sportswomen during the menstrual cycle. Int J Sports Med. (2003) 24:197–202. 10.1055/s-2003-39090 [DOI] [PubMed] [Google Scholar]
- 39.Cannon JG, Angel JB, Abad LW, O'Grady J, Lundgren N, Fagioli L, et al. Hormonal influences on stress-induced neutrophil mobilization in health and chronic fatigue syndrome. J Clin Immunol. (1998) 18:291–8. 10.1023/A:1027389907780 [DOI] [PubMed] [Google Scholar]
- 40.Carr BR, Parker CR, Madden JD, MacDonald PC, Porter JC. Plasma levels of adrenocorticotropin and cortisol in women receiving oral contraceptive steroid treatment. J Clin Endocrinol Metab. (1979). 49:346–9. 10.1210/jcem-49-3-346 [DOI] [PubMed] [Google Scholar]
- 41.Caufriez A, Leproult R, L'Hermite-Baleriaux M, Moreno-Reyes R, Copinschi G. A potential role of endogenous progesterone in modulation of GH, prolactin and thyrotrophin secretion during normal menstrual cycle. Clin Endocrinol. (2009) 71:535–42. 10.1111/j.1365-2265.2009.03539.x [DOI] [PubMed] [Google Scholar]
- 42.Childs E, Dlugos A, De Wit H. Cardiovascular, hormonal, and emotional responses to the TSST in relation to sex and menstrual cycle phase. Psychophysiology. (2010) 47:550–9. 10.1111/j.1469-8986.2009.00961.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Collins A, Eneroth P, Landgren BM. Psychoneuroendocrine stress responses and mood as related to the menstrual cycle. Psychosom Med. (1985) 47:512–27. 10.1097/00006842-198511000-00002 [DOI] [PubMed] [Google Scholar]
- 44.Genazzani AR, Lemarchand-Béraud T, Aubert ML, Felber JP. Pattern of plasma ACTH, hGH, and cortisol during menstrual cycle. J Clin Endocrinol Metab. (1975) 41:431–7. 10.1210/jcem-41-3-431 [DOI] [PubMed] [Google Scholar]
- 45.Heitkemper M, Jarrett M, Cain K, Shaver J, Bond E, Woods NF, et al. Increased urine catecholamines and cortisol in women with irritable bowel syndrome. Am J Gastroenterol. (1996) 91:906–13. [PubMed] [Google Scholar]
- 46.Huang Y, Zhou R, Wu M, Wang Q, Zhao Y. Premenstrual syndrome is associated with blunted cortisol reactivity to the TSST. Stress. (2015) 18:160–8. 10.3109/10253890.2014.999234 [DOI] [PubMed] [Google Scholar]
- 47.Judd SJ, Wong J, Saloniklis S, Maiden M, Yeap B, Filmer S, et al. The effect of alprazolam on serum cortisol and luteinizing hormone pulsatility in normal women and in women with stress-related anovulation. J Clin Endocrinol Metab. (1995) 80:818–23. 10.1210/jcem.80.3.7883836 [DOI] [PubMed] [Google Scholar]
- 48.Kasa-Vubu JZ, Dimaraki EV, Young EA. The pattern of growth hormone secretion during the menstrual cycle in normal and depressed women. Clin Endocrinol. (2005) 62:656–60. 10.1111/j.1365-2265.2005.02274.x [DOI] [PubMed] [Google Scholar]
- 49.LeRoux A, Wright L, Perrot T, Rusak B. Impact of menstrual cycle phase on endocrine effects of partial sleep restriction in healthy women. Psychoneuroendocrinology. (2014) 49:34–46. 10.1016/j.psyneuen.2014.06.002 [DOI] [PubMed] [Google Scholar]
- 50.Liu JH, Rasmussen DD, Rivier J, Vale W, Yen SS. Pituitary responses to synthetic corticotropin-releasing hormone: absence of modulatory effects by estrogen and progestin. Am J Obstet Gynecol. (1987) 157:1387–91. 10.1016/S0002-9378(87)80229-6 [DOI] [PubMed] [Google Scholar]
- 51.Lombardi I, Luisi S, Quirici B, Monteleone P, Bernardi F, Liut M, et al. Adrenal response to adrenocorticotropic hormone stimulation in patients with premenstrual syndrome. Gynecol Endocrinol. (2004) 18:79–87. 10.1080/09513590310001652955 [DOI] [PubMed] [Google Scholar]
- 52.Maki PM, Mordecai KL, Rubin LH, Sundermann E, Savarese A, Eatough E, et al. Menstrual cycle effects on cortisol responsivity and emotional retrieval following a psychosocial stressor. Horm Behav. (2015) 74:201–8. 10.1016/j.yhbeh.2015.06.023 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Ohara K, Okita Y, Kouda K, Mase T, Miyawaki C, Nakamura H. Cardiovascular response to short-term fasting in menstrual phases in young women: an observational study. BMC Womens Health. (2015) 15:67. 10.1186/s12905-015-0224-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Paoletti AM, Romagnino S, Contu R, Orru MM, Marotto MF, Zedda P, et al. Observational study on the stability of the psychological status during normal pregnancy and increased blood levels of neuroactive steroids with GABA-A receptor agonist activity. Psychoneuroendocrinology. (2006) 31:485–92. 10.1016/j.psyneuen.2005.11.006 [DOI] [PubMed] [Google Scholar]
- 55.Parry BL, Javeed S, Laughlin GA, Hauger R, Clopton P. Cortisol circadian rhythms during the menstrual cycle and with sleep deprivation in premenstrual dysphoric disorder and normal control subjects. Biol Psychiatry. (2000) 48:920–31. 10.1016/S0006-3223(00)00876-3 [DOI] [PubMed] [Google Scholar]
- 56.Rasgon N, McGuire M, Tanavoli S, Fairbanks L, Rapkin A. Neuroendocrine response to an intravenous L-tryptophan challenge in women with premenstrual syndrome. Fertil Steril. (2000) 73:144–9. 10.1016/S0015-0282(99)00452-5 [DOI] [PubMed] [Google Scholar]
- 57.Reynolds TA, Makhanova A, Marcinkowska UM, Jasienska G, McNulty JK, Eckel LA, et al. Progesterone and women's anxiety across the menstrual cycle. Horm Behav. (2018) 102:34–40. 10.1016/j.yhbeh.2018.04.008 [DOI] [PubMed] [Google Scholar]
- 58.Roche DJ, King AC. Sex differences in acute hormonal and subjective response to naltrexone: the impact of menstrual cycle phase. Psychoneuroendocrinology. (2015) 52:59–71. 10.1016/j.psyneuen.2014.10.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Stewart PM, Penn R, Holder R, Parton A, Ratcliffe JG, London DR. The hypothalamo-pituitary-adrenal axis across the normal menstrual cycle and in polycystic ovary syndrome. Clin Endocrinol. (1993) 38:387–91. 10.1111/j.1365-2265.1993.tb00519.x [DOI] [PubMed] [Google Scholar]
- 60.Su TP, Schmidt PJ, Danaceau M, Murphy DL, Rubinow DR. Effect of menstrual cycle phase on neuroendocrine and behavioral responses to the serotonin agonist M-chlorophenylpiperazine in women with premenstrual syndrome and controls. J Clin Endocrinol Metab. (1997) 82:1220–8. 10.1210/jc.82.4.1220 [DOI] [PubMed] [Google Scholar]
- 61.Tulenheimo A, Laatikainen T, Salminen K. Plasma Beta-Endorphin Immunoreactivity in Premenstrual Tension. Br J Obstet Gynaecol. (1987) 94:26–9. 10.1111/j.1471-0528.1987.tb02247.x [DOI] [PubMed] [Google Scholar]
- 62.Villada C, Espin L, Hidalgo V, Rubagotti S, Sgoifo A, Salvador A. The influence of coping strategies and behavior on the physiological response to social stress in women: the role of age and menstrual cycle phase. Physiol Behav. (2017) 170:37–46. 10.1016/j.physbeh.2016.12.011 [DOI] [PubMed] [Google Scholar]
- 63.Wolfram M, Bellingrath S, Kudielka BM. The cortisol awakening response (CAR) across the female menstrual cycle. Psychoneuroendocrinology. (2011) 36:905–12. 10.1016/j.psyneuen.2010.12.006 [DOI] [PubMed] [Google Scholar]
- 64.Suzuki S, Handa RJ. Estrogen receptor-beta, but not estrogen receptor-alpha, is expressed in prolactin neurons of the female rat paraventricular and supraoptic nuclei: comparison with other neuropeptides. J Comp Neurol. (2005) 484:28–42. 10.1002/cne.20457 [DOI] [PubMed] [Google Scholar]
- 65.Simerly RB, Chang C, Muramatsu M, Swanson LW. Distribution of androgen and estrogen receptor mRNA-containing cells in the rat brain: an in situ hybridization study. J Comp Neurol. (1990) 294:76–95. 10.1002/cne.902940107 [DOI] [PubMed] [Google Scholar]
- 66.Estacio MA, Tsukamura H, Yamada S, Tsukahara S, Hirunagi K, Maeda K. Vagus nerve mediates the increase in estrogen receptors in the hypothalamic paraventricular nucleus and nucleus of the solitary tract during fasting in ovariectomized rats. Neurosci Lett. (1996) 208:25–8. 10.1016/0304-3940(96)12534-9 [DOI] [PubMed] [Google Scholar]
- 67.Somponpun SJ, Sladek CD. Osmotic regulation of estrogen receptor-beta in rat vasopressin and oxytocin neurons. J Neurosci. (2003) 23:4261–9. 10.1523/JNEUROSCI.23-10-04261.2003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Hrabovszky E, Kalló I, Hajszán T, Shughrue PJ, Merchenthaler I, Liposits Z. Expression of estrogen receptor-beta messenger ribonucleic acid in oxytocin and vasopressin neurons of the rat supraoptic and paraventricular nuclei. Endocrinology. (1998) 139:2600–4. 10.1210/endo.139.5.6024 [DOI] [PubMed] [Google Scholar]
- 69.Alves SE, Lopez V, McEweb BS, Weiland NG. Differential colocalization of estrogen receptor b (ER b) with oxytocin and vasopressin in the paraventricular and supraoptic nuclei of the female rat brain: An immunocytochemical study. Proc Natl Acad Sci USA. (1998) 95:3281–6. 10.1073/pnas.95.6.3281 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Lund TD, Hinds LR, Handa RJ. The androgen 5alpha-dihydrotestosterone and its metabolite 5alpha-androstan-3beta, 17beta-diol inhibit the hypothalamo-pituitary-adrenal response to stress by acting through estrogen receptor beta-expressing neurons in the hypothalamus. J Neurosci. (2006) 26:1448–56. 10.1523/JNEUROSCI.3777-05.2006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Weiser MJ, Handa RJ. Estrogen impairs glucocorticoid dependent negative feedback on the hypothalamic-pituitary-adrenal axis via estrogen receptor alpha within the hypothalamus. Neuroscience. (2009) 159:883–95. 10.1016/j.neuroscience.2008.12.058 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Gaskin JH, Kitay JI. Adrenocortical function in the hamster. Sex differences and effects of gonadal hormones. Endocrinology. (1970) 87:779–86. 10.1210/endo-87-4-779 [DOI] [PubMed] [Google Scholar]
- 73.Burgess LH, Handa RJ. Chronic estrogen-induced alterations in adrenocorticotropin and corticosterone secretion, and glucocorticoid receptor-mediated functions in female rats. Endocrinology. (1992) 131:1261–9. 10.1210/endo.131.3.1324155 [DOI] [PubMed] [Google Scholar]
- 74.Ochedalski T, Subburaju S, Wynn PC, Aguilera G. Interaction between oestrogen and oxytocin on hypothalamic-pituitary-adrenal axis activity. J Neuroendocrinol. (2007) 19:189–97. 10.1111/j.1365-2826.2006.01525.x [DOI] [PubMed] [Google Scholar]
- 75.Ter Horst GJ, Wichmann R, Gerrits M, Westenbroek C, Lin Y. Sex differences in stress responses: focus on ovarian hormones. Physiol Behav. (2009) 97:239–49. 10.1016/j.physbeh.2009.02.036 [DOI] [PubMed] [Google Scholar]
- 76.Boudaba C, Szabo K, Tasker JG. Physiological mapping of local inhibitory inputs to the hypothalamic paraventricular nucleus. J Neurosci. (1996) 16:7151–60. 10.1523/JNEUROSCI.16-22-07151.1996 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Brunton PJ, McKay AJ, Ochedalski T, Piastowska A, Rebas E, Lachowicz A, et al. Central opioid inhibition of neuroendocrine stress responses in pregnancy in the rat is induced by the neurosteroid allopregnanolone. J Neurosci. (2009) 29:6449–60. 10.1523/JNEUROSCI.0708-09.2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Gunn BG, Cunningham L, Cooper MA, Corteen NL, Seifi M, Swinny JD, et al. Dysfunctional astrocytic and synaptic regulation of hypothalamic glutamatergic transmission in a mouse model of early-life adversity: relevance to neurosteroids and programming of the stress response. J Neurosci. (2013) 33:19534–54. 10.1523/JNEUROSCI.1337-13.2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Biggio G, Pisu MG, Biggio F, Serra M. Allopregnanolone modulation of HPA axis function in the adult rat. Psychopharmacology. (2014) 231:3437–44. 10.1007/s00213-014-3521-6 [DOI] [PubMed] [Google Scholar]
- 80.Sarkar J, Wakefield S, MacKenzie G, Moss SJ, Maguire J. Neurosteroidogenesis is required for the physiological response to stress: role of neurosteroid-sensitive GABAA receptors. J Neurosci. (2011) 31:18198–210. 10.1523/JNEUROSCI.2560-11.2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Misztal T, Mlotkowska P, Marciniak E, Misztal A. Allopregnanolone reduces neuroendocrine response to acute stressful stimuli in sheep. J Endocrinol. (2020) 244:201–11. 10.1530/JOE-19-0376 [DOI] [PubMed] [Google Scholar]
- 82.Owens MJ, Ritchie JC, Nemeroff CB. 5a-Pregnane-3a,21-diol-20-one (THDOC) attenuates mild stress-induced increases in plasma corticosterone via a non-glucocorticoid mechanism: comparison with alprazolam. Brain Res. (1992) 573:353–5. 10.1016/0006-8993(92)90788-B [DOI] [PubMed] [Google Scholar]
- 83.Patchev VK, Hassan AH, Holsboer DF, Almeida OF. The neurosteroid tetrahydroprogesterone attenuates the endocrine response to stress and exerts glucocorticoid-like effects on vasopressin gene transcription in the rat hypothalamus. Neuropsychopharmacology. (1996) 15:533–40. 10.1016/S0893-133X(96)00096-6 [DOI] [PubMed] [Google Scholar]
- 84.Siiteri PK, Murai JT, Hammond GL, Nisker JA, Raymoure WJ, Kuhn RW. The serum transport of steroid hormones. Recent Prog Horm Res. (1982) 38:457–510. 10.1016/B978-0-12-571138-8.50016-0 [DOI] [PubMed] [Google Scholar]
- 85.Coolens JL, Van Baelen H, Heyns W. Clinical use of unbound plasma cortisol as calculated from total cortisol and corticosteroid-binding globulin. J Steroid Biochem. (1987) 26:197–202. 10.1016/0022-4731(87)90071-9 [DOI] [PubMed] [Google Scholar]
- 86.Vinning RF, McGinley RA, Maksvytis J, Ho KY. Salivary cortisol: a better measure ofadrenal cortical function than serum cortisol. Ann Clin Biochem. (1983) 20:329–35. 10.1177/000456328302000601 [DOI] [PubMed] [Google Scholar]
- 87.Westphal U. Steroid-protein interactions. Monogr Endocrinol. (1971) 4:1–567. 10.1007/978-3-642-46262-7_1 [DOI] [PubMed] [Google Scholar]
- 88.Moore DE, Kawagoe S, Davajan V, Nakamura RM, Mishell DR. An in vivo system in man for quantitation of estrogenicity. II Pharmacologic changes in binding capacity of serum corticosteroid-binding globulin induced by conjugated estrogens, mestranol, and ethinyl estradiol. Am J Obstet Gynecol. (1978) 130:482–6. 10.1016/0002-9378(78)90294-6 [DOI] [PubMed] [Google Scholar]
- 89.Jeyakumar M, Carlson KE, Gunther JR, Katzenellenbogen JA. Exploration of dimensions of estrogen potency: parsing ligand binding and coactivator binding affinities. J Biol Chem. (2011) 286:12971–82. 10.1074/jbc.M110.205112 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Nenke MA, Zeng A, Meyer EJ, Lewis JG, Rankin W, Johnston J, et al. Differential effects of estrogen on corticosteroid-binding globulin forms suggests reduced cleavage in pregnancy. J Endocr Soc. (2017) 1:202–10. 10.1210/js.2016-1094 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Herrera AY, Faude S, Nielsen SE, Locke M, Mather M. Effects of hormonal contraceptive phase and progestin generation on stress-induced cortisol and progesterone release. Neurobiol Stress. (2019) 10:100151. 10.1016/j.ynstr.2019.100151 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Hampson E. A brief guide to the menstrual cycle and oral contraceptive use for researchers in behavioral endocrinology. Horm Behav. (2019) 119:104655. 10.1016/j.yhbeh.2019.104655 [DOI] [PubMed] [Google Scholar]
- 93.Daskalakis NP, Cohen H, Nievergelt CM, Baker DG, Buxbaum JD, Russo SJ, et al. New translational perspectives for blood-based biomarkers of PTSD: From glucocorticoid to immune mediators of stress susceptibility. Exp Neurol. (2016) 284:133–40. 10.1016/j.expneurol.2016.07.024 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Plotsky PM, Owens MJ, Nemeroff CB. Psychoneuroendocrinology of depression. Hypothalamic-pituitary-adrenal axis. Psychiatr Clin North Am. (1998) 21:293–307. 10.1016/S0193-953X(05)70006-X [DOI] [PubMed] [Google Scholar]
- 95.Sze Y, Brunton PJ. Sex, stress and steroids. Eur J Neurosci. (2019). [Epub ahead of print]. 10.1111/ejn.14615. [DOI] [PubMed] [Google Scholar]
- 96.Altemus M, Sarvaiya N, Neill Epperson C. Sex differences in anxiety and depression clinical perspectives. Front Neuroendocrinol. (2014) 35:320–30. 10.1016/j.yfrne.2014.05.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Bangasser DA, Valentino RJ. Sex differences in stress-related psychiatric disorders: neurobiological perspectives. Front Neuroendocrinol. (2014) 35:303–19. 10.1016/j.yfrne.2014.03.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The datasets generated for this study are available on request to the corresponding author.