Editor
Since the beginning of the COVID‐19 pandemic, different types of cutaneous manifestations have been reported. In Spain, there were reports in the first weeks of April 2020 of an increase in purpuric acral lesions similar to perniosis on the hands and especially the feet of children and young adults. These patients do not normally present with clinical manifestations linked to COVID‐19, and their PCR and serological tests are usually negative for specific IgM and IgG. 1 , 2
These acral lesions manifest in two clinical forms and can present in an isolated or concomitant manner. The first type of lesions is located on the fingers and toes as a type of erythematous‐purpuric perniosis, which can evolve into vesicles, blisters and crusts. The second type of lesions is found on the palms of the hand, soles of the feet or on the heels with macular or papular purpura characteristics that are similar to vasculitis or to erythema multiforme, being generally asymptomatic or pruriginous. This clinical and histopathological study reports on the second type of clinical presentation, associated with a thrombotic vasculopathy in the histological study, a finding that has not been reported in asymptomatic patients during the COVID‐19 pandemic. 2
A 12‐year‐old boy who, during the period of COVID‐19 lockdown, presented with a pruriginous, haemorrhagic purpuric eruption and vesicular blisters on the heels of both feet, which had developed over a period of 4 days (Fig. 1) The patient had not taken any new medications and neither he nor his family presented with respiratory symptoms. The tests, which included biochemical, hepatic and renal tests, hemogram, coagulation test and urinalysis, showed no alterations. Nasopharyngeal swabs were taken for a specific PCR for COVID‐19 and for an IgM and IgG rapid test, both of which were negative. A nasopharyngeal swab was also taken to carry out tests for influenza and other respiratory viruses, which were also negative. Serological tests were carried out for Epstein–Barr virus, cytomegalovirus, parvovirus B19, Mycoplasma pneumoniae, herpes simplex virus, measles, rubella, parotitis, HIV and hepatitis B and C, all of which were negative. PCRs of blood samples and of the cutaneous lesions were also carried out for enterovirus, which were also negative.
Figure 1.

Clinical image. Purpuric lesions and vesicles located on the soles and ankles of the feet.
The serological tests were repeated 15 days after the symptoms started, and a test for SARS‐Cov‐2‐specific IgM and IgG was also added, all of which were negative.
The histopathological study of a cutaneous biopsy revealed partial epidermal necrosis and perivascular lymphoid infiltrate in superficial and deep dermis. In addition, some capillaries in papillary dermis showed images of microthrombi, with extravasation of red blood cells. Vasculitic changes were present in relation to the lymphoid component but not in the thrombotic one (Fig. 2).
Figure 2.
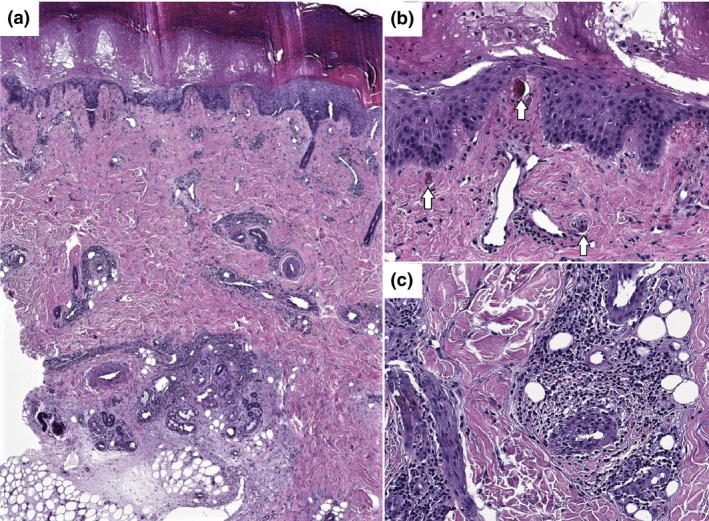
Histopathological findings (a). At low power view, a perivascular lymphoid infiltrate is present in dermis, both superficial and deep. (H&E, 2×). (b) Epidermal necrosis is identified. Focal images of microthrombi are observed in capillaries of the papillary dermis accompanied by extravasation of red blood cells. (White arrows) (H&E, 10×). (c). Vasculitic changes can be seen, with thickening of the vessel wall and activation of the endothelium with nuclear enlargement. In addition, lymphocytes are observed permeating the vessel wall (H&E, 20×).
In cases or series of cases of perniotic acral lesions, the histopathological findings have been unspecific. Dermal oedema, vacuolar alteration of the basal layer, necrotic keratinocytes and mixed infiltrate with a mainly perivascular and perieccrine distribution in the superficial and deep dermis and the hypodermis have been notified. 2 , 3 , 4
However, our histological findings are reminiscent of the pauci‐inflammatory thrombogenic vasculopathy that occurs seriously ill hospitalized COVID‐19 patients with COVID‐19. This thrombogenic vasculopathy is due to activation of the complement pathways and an associated procoagulant state. 5 , 6 However, no cases of thrombotic vasculopathy have been reported to date in asymptomatic children or young adults with acral lesions.
In conclusion, the histological findings of purpura‐erythema multiforme appearing on soles and heels reveal thrombogenic vasculopathy similar to that found in COVID‐19 patients with severe forms of the disease, which suggests that these acral lesions may be related to SARS‐COV‐2 or its etiopathogenesis.
Conflicts of interest
The authors declare that they have no conflict of interest.
Funding sources
This research received no specific grant from any funding agency in the public, commercial or not‐for‐profit sectors.
References
- 1. Fernandez‐Nieto D, Jimenez‐Cauhe J, Suarez‐Valle A et al. Characterization of acute acro‐ischemic lesions in non‐hospitalized patients: a case series of 132 patients during the COVID‐19 outbreak. J Am Acad Dermatol 2020; S0190‐9622(20)30709‐X. 10.1016/j.jaad.2020.04.093 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Romaní J, Baselga E, Mitjà O et al. Chilblain and acral purpuric lesions in Spain during COVID confinement: retrospective analysis of 12 cases. Actas Dermosifiliogr 2020; S0001‐7310(20)30087‐9. 10.1016/j.ad.2020.04.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Kolivras A, Dehavay F, Delplace D et al. Coronavirus (COVID‐19) infection‐induced chilblains: a case report with histopathological findings. JAAD Case Rep 2020. 10.1016/j.jdcr.2020.04.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Recalcati S, Barbagallo T, Frasin LA et al. Acral cutaneous lesions in the time of COVID‐19. J Eur Acad Dermatol Venereol 2020. 10.1111/jdv.16533 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Magro C, Mulvey JJ, Berlin D et al. Complement associated microvascular injury and thrombosis in the pathogenesis of severe COVID‐19 infection: a report of five cases. Transl Res 2020; S1931‐5244(20)30070‐0. 10.1016/j.trsl.2020.04.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Zhang Y, Cao W, Xiao M et al. Clinical and coagulation characteristics of 7 patients with critical COVID‐2019 pneumonia and acro‐ischemia. Zhonghua Xue Ye Xue Za Zhi 2020; 41: E006. [DOI] [PubMed] [Google Scholar]
Acknowledgement
The patients in this manuscript have given written informed consent to publication of their case details. We gratefully acknowledge the multidisciplinary team that contributed to the patient's medical care, especially Dr. Carmen Boldova Aguar.


