A 59‐year‐old woman presented to Westmead Hospital, New South Wales' assigned coronavirus disease 2019 (COVID‐19) hospital, with extensive abdominal necrosis (Fig. 1) which she had been trying to manage at home for 3 weeks. This is on a background history of type 2 diabetes mellitus for which she had been on medication but ceased at her own discretion.
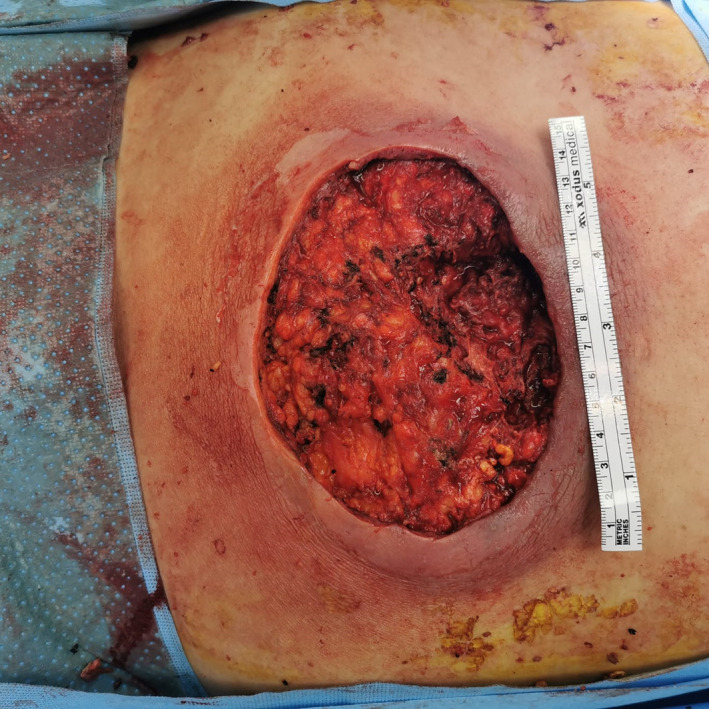
Fig. 1.

Large necrotic abdominal abscess untreated for 3 weeks. Patient delayed presentation due to fears of contracting coronavirus disease 2019.
The patient reported developing a small area of periumbilical erythema which expanded over 3 weeks. She was commenced on oral antibiotics by her general practitioner but noted over the last week the associated area of skin had become black. In particular, the patient explained she delayed presenting to the emergency department due to the COVID‐19 outbreak as she was scared of contracting the virus by coming to the hospital.
On examination, she had a large foul smelling 15‐cm fluctuant abscess with overlying necrosis. Inflammatory markers were elevated: white cell count 12.4 × 109 and C‐reactive protein 45 mg/L. Surgical debridement was booked emergently due to concerns of potential necrotizing fasciitis and was commenced on triple antibiotic therapy: meropenem, clindamycin and vancomycin. An incision and drainage was performed with 500 mL of frank pus being evacuated from the large abscess cavity, followed by debridement. The abscess involved subcutaneous fat (Fig. 2) but did not involve fascia.
Fig. 2.
Intraoperative incision and drainage: superficial abscess to subcutaneous fat with no involvement of fascia.
Negative pressure wound therapy was applied and antibiotics were rationalized in accordance with cultured susceptibilities with ongoing review by wound clinical nurse consultant and follow‐up with plastics team.
In December 2019, the province of Wuhan, China, reported clusters of patients with pneumonia of unknown cause. A novel coronavirus, 2019‐nCoV (COVID‐19), was the isolated causative organism. 1 COVID‐19 was declared a pandemic by the World Health Organization in March 2020 and healthcare systems globally have had to adapt and prepare for an unprecedented healthcare crisis. However, as people are encouraged to socially distance and isolate, and healthcare systems re‐organize themselves to increase their response, consideration must be given to the implication this has on non‐COVID patients.
The impact of COVID‐19 on delayed presentations of non‐COVID pathologies is being experienced worldwide. During March, Italy saw a significant reduction in paediatric emergency presentations by 73–88%. 2 Lazzerini et al. presented a 12 patient case series of delayed paediatric emergency presentations in which the parents of all cases reported avoiding the hospital due to fears of contracting COVID‐19. Half of the children were admitted to intensive care unit and four died. 2 New York has experienced a significant decline in acute coronary syndrome presentations. 3 Similarly, delays in referral to surgical teams result from awaiting COVID‐19 clearance as testing is performed on patients presenting with gastrointestinal symptoms as these symptoms have been associated with COVID‐19 infection.4, 5
Similar effects were seen during the severe acute respiratory syndrome (SARS) outbreak at the beginning of the millennium. At the peak of the SARS epidemic, Taiwan saw a significant reduction in ambulatory care, inpatient care and dental care patients. 6 Fear of contracting SARS influenced people's willingness and choice to seek adequate medical care. 6 These concerns were reflected in cancer patients at the Taipei Veterans General Hospital, Taiwan, as 63.8% were afraid of visiting hospital during the SARS infective period and 36.2% felt SARS was more severe and fatal than their underlying cancer. 7
Locally, the impact of COVID‐19 has led to significant changes in surgical practice. Non‐emergency surgeries (category 2 – within 90 days and category 3 – within 365 days) have been suspended, protocols regarding intubation and extubation have been developed and the risk of viral exposure from surgical smoke in laparoscopic surgeries continues to be an issue of growing debate. 8 Acute surgical pathologies, such as appendicitis, usually treated by surgical intervention have been reconsidered towards medical management. 8
The COVID‐19 pandemic has drastically changed medical practice worldwide and as focus remains on control of the virus, there are concerns over the toll on non‐COVID patients. 3 Fear of contracting the virus will undoubtedly impact non‐COVID patients seeking adequate and timely medical care. As face‐to‐face consults are exchanged for alternate reviews, such as teleconferencing, healthcare workers must consider its implication on adequate clinical assessment. The challenge lies in continuing to deliver optimum care to patients, when patients themselves are too scared to seek assistance in fear of contracting, what they perceive as a more serious illness. From the surgeons' perspective, bacterial sepsis left unchecked will result in death or require intensive care support, in a higher proportion than what has currently been seen with COVID‐19 within Australasia. This message needs to reach the community, such that late presentations as described within this article are avoided.
References
- 1. Zhu N, Zhang D, Wang W et al. A novel coronavirus from patients with pneumonia in China, 2019. N. Engl. J. Med. 2020; 382: 727–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Lazzerini M, Barbi E, Apicella A, Marchetti F, Cardinale F, Trobia G. Delayed access or provision of care in Italy resulting from fear of COVID‐19. Lancet Child Adolesc. Health 2020; 4: e10–1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Rosenbaum L. The Untold Toll — The Pandemic’s Effects on Patients without Covid‐19. New England Journal of Medicine. 2020; 10.1056/nejmms2009984. [DOI] [PubMed] [Google Scholar]
- 4. Slim K, Veziant J. Urgent digestive surgery, a collateral victim of the COVID‐19 crisis?. Journal of Visceral Surgery. 2020; 10.1016/j.jviscsurg.2020.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Wong SH, Lui RN, Sung JJ. Covid‐19 and the digestive system. J. Gastroenterol. Hepatol. 2020; 35: 744–8. [DOI] [PubMed] [Google Scholar]
- 6. Chang HJ, Huang N, Lee CH, Hsu YJ, Hsieh CJ, Chou YJ. The impact of the SARS epidemic on the utilization of medical services: SARS and the fear of SARS. Am. J. Public Health 2004; 94: 562–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Chen YM, Perng RP, Chu H, Tsai CM, Whang‐Peng J. Impact of severe acute respiratory syndrome on the status of lung cancer chemotherapy patients and a correlation of the signs and symptoms. Lung Cancer 2004; 45: 39–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. McBride KE, Brown KGM, Fisher OM, Steffens D, Yeo DA, Koh CE. Impact of the COVID‐19 pandemic on surgical services: early experiences at a nominated COVID‐19 centre. ANZ J. Surg. 2020; 90: 663–5. [DOI] [PMC free article] [PubMed] [Google Scholar]


