A novel severe acute respiratory syndrome coronavirus (SARS‐CoV‐2), a major outbreak, in China had spread to over 200 other countries by 15 May 2020, and 4 338 658 cases with 297 119 deaths (6.8% case fatality rate) had been reported by the World Health Organization (WHO). 1 Studies have shown that coagulation dysfunction is one of the main reasons causing death in coronavirus disease‐2019 (COVID‐19) patients, and 71% of dead patients achieved the diagnostic criteria of the International Society for blood clots bleeding (International Society on Thrombosis and Haemostasis [ISTH]) of disseminated intravascular coagulation (disseminated intravascular coagulation [DIC]). 2 There have been many reports of SARS‐CoV‐2 causing thrombocytopenia, but immune thrombocytopenic purpura (ITP) is rarely seen, and the latest case of COVID‐19 with ITP has been reported in a patient with autoimmune hypothyroidis, found in France. 3
In this study, a patient with immune thrombocytopenic purpura in Huoshenshan Hospital (Wuhan, China) was reported after reviewing electronic records of a total of 3 059 patients from 4 February to 30 March. This study was approved by the Medical Ethical Committee of Wuhan Huoshenshan Hospital. A written informed consent was obtained from the patient.
A 32‐year‐old woman complained of fever, cough, and fatigue without any obvious cause on 3 February 2020, and the body temperature was up to 39.4℃. After taking the medicine, the body temperature dropped to normal.
On 5 February the patient was admitted to Wuhan Hankou Hospital for chest CT examination, which showed a small amount of patchy shadows in both lungs, part of which was ground glass. Blood routine examination showed a decreased platelet count (64 × 109/L), and she received treatment with oseltamivir and Chinese medicine (Lianhua qingwen capsule) during home isolation. On 7 February, novel coronavirus nucleic acid test presented a positive result.
On 16 February, the patient was admitted to the Wuhan Fangcang Hospital, and was immediately found to have many small bleeding spots on the skin of the whole body, mainly on the lower limbs. On 19 February, the patient was admitted to the Wuhan Fifth People Hospital and diagnosed with ITP, and the rash declined gradually after treatment with glucocorticoids and intravenous injection of platelets.
On 3 March, after a 16‐day history of rash, the patient was admitted to the Wuhan Huoshenshan Hospital with moderate COVID‐19 and ITP. Physical examination: body temperature was 36.2℃, pulse was 68 times/min, respiration was 20 times/min, blood pressure was 130/77 mmHg, oxygen saturation was 98% (no oxygen), and the pulse was uneven.
Blood routine examination on 4 March showed white blood cell count was 10.6 × 109/L, percentage of eosinophil was 0.2%, absolute neutrophil count was 7.84 × 109/L, and red blood cell count was 3.78 × 1012/L. The patient's blood image was slightly higher, which was considered to be due to glucocorticoids, and continued to receive methylprednisolone treatment (two tablets per day).
Blood routine examination on 10 March showed: absolute neutrophil count was 6.41 × 109/L, and the platelet count was 119 × 109/L. Chest CT indicated that the lesion had been mostly absorbed, and there was no fever for more than 3 consecutive days. Novel coronavirus antibody IgG was single positive, and two pharyngeal swabs (sampling time >24 hours) tests for novel coronavirus nucleic acid were both negative, which met the discharge standards. Blood routine examination on 12 March showed that the platelet count was 113 × 109/L, which reached a stable level, and the discharge was processed on 14 March.
The 32‐year‐old female in our study is considered as case 1 and the 65‐year‐old female in France 3 as case 2, and the comparison of two cases are presented in Table 1, and progression of the case 1 is shown in Figure 1.
Table 1.
Comparison of two cases with immune thrombocytopenic purpura
| Characteristics | Case 1 | Case 2 |
|---|---|---|
| Gender | Female | Female |
| Age, y | 32 | 65 |
| Basic diseases | None | Hypertension, autoimmune hypothyroidism |
| COVID‐19 clinical level | Moderate | Unknown |
| Fever | Yes | Yes |
| Fatigue | Yes | Yes |
| Cough | Yes | Yes |
| Chest pain | No | No |
| Nausea | No | No |
| Abdominal discomfort | No | Yes |
| Respiratory rate (breaths per minute) | 20 | 28 |
| Oxygen saturation, % | 98 | 89 |
| Lowest platelet count | 64×109/L | 1000/mm3 |
| CT | Pneumonia | Pneumonia, subarachnoid microhemorrhage |
| Arrhythmology | Yes | No |
| Glucocorticoid therapy | Yes | Yes |
| Immunoglobulin therapy | No | Yes |
| Chinese medicine | Yes | No |
| Time from diagnosis to ITP disappearance, d | 16 | 9 |
| Time from diagnosis to throat swab SARS‐CoV‐2 nucleic acid negative, d | 32 | Unknown |
| Time from SARS‐CoV‐2 nucleic acid positive to ITP occurrence | 9 | 4 |
Case 2: Zulfiqar A‐A, Lorenzo‐Villalba N, Hassler P, Andrès E. Immune thrombocytopenic purpura in a patient with COVID‐19. New England J Med 2020:e43.
Figure 1.
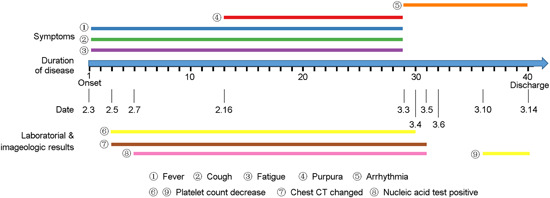
Immune thrombocytopenic purpura progression in the patient. The axis represents the days after hospital onset. The significant points are shown in the figure, including fever, cough, fatigue, purpura, arrtythmia, platelet count decrease, chest CT changes, and nucleic acid test positive
In most COVID‐19 with thrombocytopenia cases, the platelet count did not decrease to a level at which bleeding occurs. Although the mechanism of thrombocytopenia in COVID‐19 is still unclear, researchers indicated the possible mechanisms of thrombocytopenia in COVID‐19 patients, similar to SARS, 4 including decreased primary platelet production caused by cytokine storm and direct infection of hematopoietic and bone marrow stromal cells, increased platelet destruction caused by increase of antibodies and immune complexes, declined circulating platelet caused by lung injury. 5 Use of antibiotics, antivirals, heparin, and other commonly used agents as treatment for hemodialysis and extracorporeal membrane oxygenation (ECMO) may trigger the mechanism. Some studies suggested that the lower the platelet count, the higher is the mortality, and the possibility of adverse effects caused by polypharmacy should also be carefully considered in severe thrombocytopenia.
In this study, the course of ITP was within the course of COVID‐19, same as case 2; however, whether SARS‐CoV‐2 can cause ITP is hard to confirm, in the presence of a pre‐existing autoimmune disease, without testing the patient. This case suggests to be vigilant for complications associated with COVID‐19; and the mechanism of ITP, secondary to COVID‐19, needs further study.
CONFLICT OF INTERESTS
The authors declare that there are no conflict of interests.
AUTHOR CONTRIBUTIONS
XX and JZ had full access to all the data in this study and took responsibility for its integrity and accuracy during analysis. Concept and design: XX and YT. Data collection, analysis, and interpretation: JW. Drafting of the manuscript: YY and JZ.
ACKNOWLEDGMENTS
This study was financially supported by grants from the Key Foundation of Wuhan Huoshenshan Hospital ([2020[18]), Key Research & Development Program of Jiangsu Province (BE2018713), Medical Innovation Project of Logistics Service (18JS005).
Funding Information Medical Innovation Project of Logistics Service, Grant/Award Number: 18JS005; Key Research & Development Program of Jiangsu Province, Grant Award Number: BE2018713; Key Foundation of Wuhan Huoshenshan Hospital, Grant/Award Number: 2020[18]
Yang Yang and Jun Zhao contributed equally to this study.
Contributor Information
Yi Teng, Email: 502769485@qq.com.
Xinyi Xia, Email: xiaxynju@163.com.
REFERENCES
- 1. Organization WH . Coronavirus disease (COVID‐19) situation dashboard. https://whosprinklr.com. Accessed 15 May 2020.
- 2. Tang N, Li D, Wang X, Sun Z. Abnormal coagulation parameters are associated with poor prognosis in patients with novel coronavirus pneumonia. J Thromb Haemostasis. 2020;18:844‐847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Zulfiqar A‐A, Lorenzo‐Villalba N, Hassler P, Andrès E. Immune thrombocytopenic purpura in a patient with COVID‐19. N Engl J Med. 2020;382:e43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Yang M, Li C, Li K, et al. Hematological findings in SARS patients and possible mechanisms. Int J Mol Med. 2004;14(2):311‐315. [PubMed] [Google Scholar]
- 5. Yang X, Yang Q, Wang Y, et al. Thrombocytopenia and its association with mortality in patients with COVID‐19. J Thromb Haemostasis. 2020:14848. [DOI] [PMC free article] [PubMed] [Google Scholar]


